Research Article Open Access
End-of-Life Decision Making in Pediatric Oncology and Intensive Care in Germany Results of a Multi-professional Questionnaire Study
Nennhaus M and Classen CF*Children’s Hospital, University Medicine Rostock, Ernst-Heydemann-Str. 8, D-18057 Rostock, Germany
- *Corresponding Author:
- Carl Friedrich Classen, MD, PhD
Children’s Hospital, University Medicine Rostock
Ernst-Heydemann-Str. 8, D-18057 Rostock, Germany
Tel: +49 381 494 7262
Fax: +49 381 494 7261
E-mail: carl-friedrich.classen@med.uni-rostock.de
Received date: February 07, 2016 Accepted date: March 08, 2016 Published date: March 12, 2016
Citation: Nennhaus M, Classen CF (2016) End-of-Life Decision Making in Pediatric Oncology and Intensive Care in Germany – Results of a Multi-professional Questionnaire Study. J Palliat Care Med 6:251. doi:10.4172/2165-7386.1000251
Copyright: © 2016 Nennhaus M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: In modern medicine, not all possible treatments are in the best interest of a patient. Decisions to withhold or withdraw therapies should be based on the patient’s or guardian's wishes and on the medical indication. To define the latter medical teams have to find decisions themselves, which involves not only physicians, but in particular nurses and psychologists – and in case of disagreements emotional conflicts may result. Methods: We asked how end-of-life decisions are made in German pediatric oncology and intensive care units, and what problems were observed. An online questionnaire was sent to team members of 42 hospitals, covering 32 items, including personal data, the process of decision-making talks itself, and finally, whether they were a burden for teams or led to conflicts within them. Data were studied by a descriptive analysis. Results: From 282 questionnaires, we received 77 answers (27.30%; i.e. 59 physicians, 6 nurses, 10 psychologists/others). In most cases, 4-5 participants were involved in end-of-life decision talks, always including physicians, often nurses or other professional groups. A standard procedure was used only by a minority, in particular in intensive care units, as were cooperation with a clinical ethics committee or with a neutral observer. Many respondents reported moderately burdening talks, and conflicts in decision making were a burden to the teams. These conflicts took place on all levels. The feeling of being ignored or neglected in an end-of-life decision talk was described by some respondents. Conclusion: We conclude that standard operation procedures may be of some help; particularly regarding the participation of nurses, there still is some room for improvement. Whether ethical committees or external experts are helpful remains open. However, as conclusion, our impression is that the status quo is not too bad.
Keywords
End-of-life; Pediatric palliative care; Decision-finding
Abbreviations
TAN: Transaction number
Background
In modern medicine, not all medical measures that are possible are in the best interest of a patient. Limitations of therapy may include the switch from a curative to a palliative intent, as well as giving up lifeprolonging measures, by withholding a possible escalation of intensive treatment or even by withdrawal of on-going treatments. Usually, such decisions should be based on two pillars: the patient’s wish – either declared or presumed – and the medical indication [1-5]. Sometimes, an adolescent may declare his or her own wishes, however, in pediatrics, typically the guardians representing the child – in most cases the parents – will have to make such decisions. Medical teams, treating the children, learning about their medical and psychological conditions, have to assist them. It is their obligation to give the best possible advice, both, to prevent the children from harm, and the guardians from feelings of guilt. They will have to live the rest of their lives remembering this situation. Not only to be with one’s own dying child is one of the most unbearable situation imaginable - it may also be unendurable to feel solely responsible for the right decisions to be taken in this process.
Thus, both to define the medical indication, and to counsel the guardians, the medical teams have to shape their own attitudes – and therefore, they have to make decisions themselves [6,7].
Such decision making is an every-day component of modern medicine. In 2000, the EURONIC study group found that among neonatologists of seven European countries including Germany, more than 90% had already practised therapy limitations [8]. A study of 1997 from the Netherlands found that in 299 deaths of children below one year of age, 57% were in advance discussed in a process of decision making [9].
If severely ill children are cared for by a medical team, not only physicians but also nurses, and often psychologists, physiotherapists and other specialists are involved. Being involved does also include one’s own feelings and conscience – which often is in particular true for the nurses. Thus, all professions have to bear such decisions – and it is not an uncommon observation that disagreements in this field may be the cause of emotional conflicts within a team [6].
Therefore, the right way of decision making does not only aim at the patient’s best, it is also relevant for the social functioning of a medical team. Thus, three questions are of particular interest: Who is usually involved in the decision making process - is it a multiprofessional procedure, are clinical ethics committees or other external specialists involved? Are standard procedures used? Is decision-finding a burden to the team members, or even a cause of conflicts?
Such questions have already been studied by several working groups.
In the ETHICUS study, data of 4248 deceased adult intensive care patients from 17 European countries were studied, including 3086 cases (72%), in which a decision for therapy limitation was made. Here, in 70% the physicians declared that nurses were involved in decision making discussions [10,11]. In contrast, a questionnaire study performed in Munich showed that, in a majority of cases, nurses were not involved, leading to some discontent [12,13]. In a study by Graw et al. performed at an adult surgical intensive care unit, in 69% of 226 deceased patients, a limitation of therapy was documented. Here, it was found that the nurses were the more often involved, the longer the patient was in the hospital [13]. In a French study covering numerous adult intensive care units, 50% of the physicians declared that nurses were involved, however, this was confirmed by only 27% of the nurses [14].
A South African study described problems in the interprofessional interaction in this field, however, it also showed that decision making involving both physicians and nurses is helpful [15]. In a work analyzing interprofessional cooperation in intensive care units, end-oflife decision making was even described as one main source of conflicts, in particular in case of lacking psychological team support [16].
Similar results were found by the CONFLICUS study of 2009. Here, 32 % of nurses from 24 European countries declared always or regularly to be involved in decision-finding. Conflicts between physicians and nurses were described in 32.6% [17]. In a study analyzing 31 pediatric intensive care units in the USA in 2000, 92 % of the physicians declared that decision making was well organized, however only 59 % of the nurses confirmed this view [18]. In an interview study in 2012, 13 physiscians and nurses were questioned, and again the process of end-of-life decision making was described as a relevant cause of conflicts in the teams [19].
A recent study involving interviews with 51 intensive care nurses of 5 nations showed that nurses often have an important role mediating between physicians and parents of severely ill children [20]. This was also described in a German analysis [6].
A study from the Netherlands involving pediatric intensive care units showed that about one quarter used some guidelines for decision making, and 40% wished the establishment of national guidelines for such processes [21]. As a summary of a conference on medical ethics in Durban 2014 [22], interprofessional strategies of decision making were recommended in general.
The so called Einbeck Recommendations of German neonatologists from 1986 and 1992 contain detailed recommendations to include all persons involved in the care for a baby in the decision making, in order to find the best possible answers [23].
In the USA, the Hastings Center in 2013 published a national guidance including similar recommendations in pediatric intensive care [24]. Another guidance developed in Munich for adults was based on an algorithm for decision making that was judged in a positive way by 90% of those using it [25].
Thus, many studies confirm the relevance of such decision processes for the functioning of a team. However, firm conclusions still seem to be lacking.
The aim of our study was to analyse end-of-life decision processes, focusing on pediatric oncological and intensive care units in Germany. Thus, a questionnaire was designed and sent to physicians, nurses, and psychosocial care workers, covering the main questions regarding decision-finding, as described above, to learn about the pathways of end-of-life decision making currently practiced in German pediatric oncology and intensive care units.
Materials and Methods
Based on a detailed literature search [7,12,13,17,26-28], an online questionnaire was developed using the program VividFormsEditor, a browser, and web based software provided by the EvaSys platform. The questionnaire was sent to pediatric oncology and intensive care units throughout Germany, selected by a clinical oncology study group (SIOP CNS GCT II) including 42 German hospitals. The heads of the units were asked to give the permit to distribute the questionnaire to their co-workers. Finally, 32 hospitals were included, the questionnaires were sent in October 2013, and after a recall in December, data acquisition was terminated in February 2014. The questioning was anonymous, and by generation of a TAN (transaction number), double responses were prevented.
The attached letter contained all relevant information, and the respondents agreed in written form to participate in the questioning. Since all involved people were professionals, and no minors or mentally handicapped persons were involved in accordance with the Declaration of Helsinki (1964), an additional ethical committee vote was not applied for.
The attached letter contained all relevant information, and the respondents agreed in written form to participate in the questioning. Since all involved people were professionals, and no minors or mentally handicapped persons were involved in accordance with the Declaration of Helsinki (1964), an additional ethical committee vote was not applied for.
The next part of the questionnaire included the following aspects: was there a standard procedure for such decision making, and, if not, did the person believe that such would be useful; how was the discussion was organized; was a neutral observer or a clinical ethics committee involved, etc. Most of such questions could be answered by “never ”, “rarely ”, “occasionally ”, “often ” or “always ”.
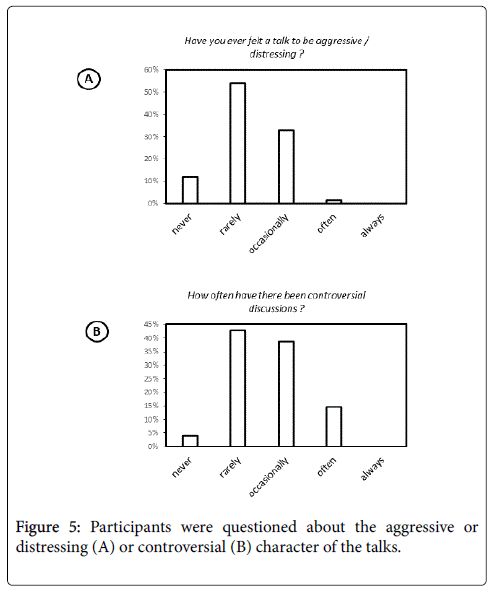
In the final part of the questionnaire, questions were asked concerning the burdens and conflicts of end-of-life decisions. We asked whether all participants got the chance to express their opinion, whether these talks were regarded as distressing, and whether participants felt to be ignored or denied the chance to express their opinion. We also asked whether there had ever been controversial or aggressive discussions. In particular, we wanted to know whether conflicts occurred rather between different hierarchical levels or different professional groups. At the end of the questionnaire, there was free space for individual comments.
The statistic data analysis was done using the program IBM SPSS Statistics 20. Incidence tables, cross table and Chi square tests as well as bivariate correlation analyses were used. Each variable was tested for normal distribution. P = 0.05 was defined as level of significance.
Results
Study population
300 questionnaires were distributed, however, 18 email addresses turned out to be unfunctional. From 282 questionnaires, we received 77 answers (27.30%); i.e. from 216 physicians we received 59 answers (27.31%), from 27 nurses 6 answers (22.22%), from 39 psychologists/ other therapists we received 10 answers (25.64%).
53.2% of the participants were male; the age distribution was as follows: 30 - 39 years: 22 (28.6%), 40 - 49 years: 34 (44.2%), 50 - 59 years: 18 (23.4%), 60 - 69 years: 3 (3.9%). Median age was 45, average age 44 years. 6.5% had <5 years of professional experience, 14.3 % 5- <10 years, 45.5 % 10-<20 years and 33.8 % >20 years. The hospital types were as follows: university hospitals 59 (76.6%) , community hospitals 7 (9.1%), private hospitals 6 (7.8%), church hospitals 4 (5.2%), no information 1 (1.3%).
The department types were: intensive care unit 18 (23.4%), oncology unit 53 (68.8%), others (like bone marrow transplant unit) or unknown 6 (7.8%). Most participants were physicians (76%, including 11% heads of department, 51 % other senior physicians, 4% other physicians). 6 nurses and 7 psychologists / schoolteachers were involved, three called themselves "others“. There was no female heads involved, and only one male nurse, one male psychologist. Most respondents (88%) had already taken part in more than 10 end-of-life decision talks, only 10% in less. 71 % respondents told that a supervision was available at their institution.
End-of-life talks: structural aspects
We first asked about the number of participants in end-of-life decision talks. 19,5% of respondents said it were 2-3 people, 47 % said it were 4-5, and 34 % it was >5.
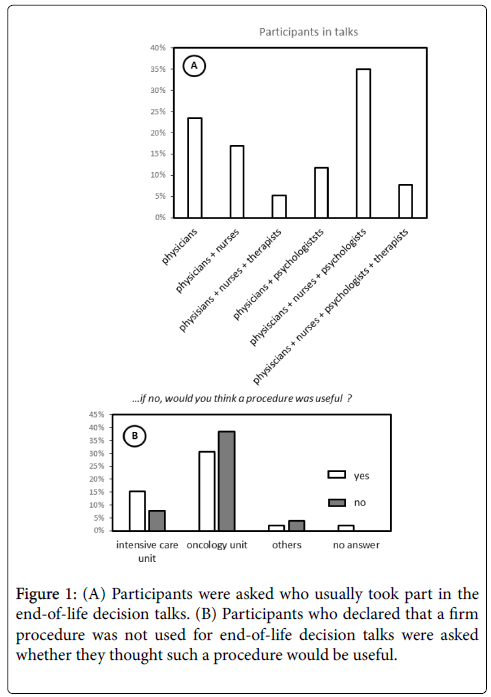
The pattern of professions that were involved was very heterogeneous (Figure 1A). The largest group declared that physicians, nurses, and psychologists participated (35%).
Concerning the mode of decision making, most participants answered that the clinical team first made up its opinion and then approached the parents; only one participant declared that always the parents were asked first. 20 % said that both modes were common. A protocol was written in 81%.
Only about one third of the respondents declared that a firm procedure was used for such talks, and in those who did not use one, only one third believed that it might be useful. Here, we saw a marked difference between the types of medical units: in intensive care units, the majority wished to have a firm procedure, while this was less marked in oncology units (Figure 1B).
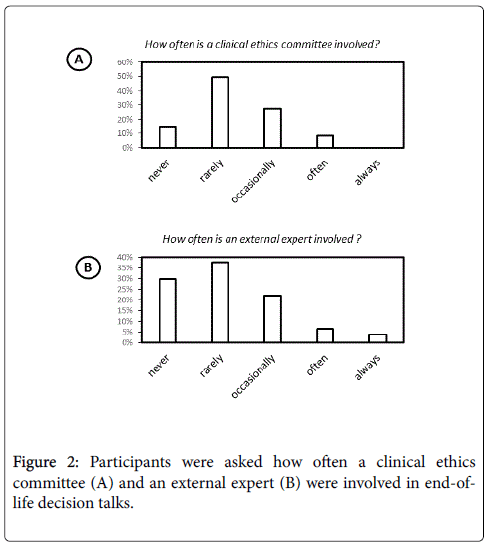
Both cooperation with a clinical ethics committee or with a neutral observer was performed only rarely (Figure 2). Also, an advance directive from the patient or the guardians was only available in a small number of cases (38 % said “never”, 48% “rarely”, 13 % “occasionally”).
The talks were usually led by a senior physician or by the head of the department (76%), usually the specialist was responsible (56%), followed by the head (41%). Majority votes were described by 12% (often/always).
Burdens and conflicts in end-of-life talks
Now we wanted to know more about possible burdens and conflicts associated with end-of-life talks.
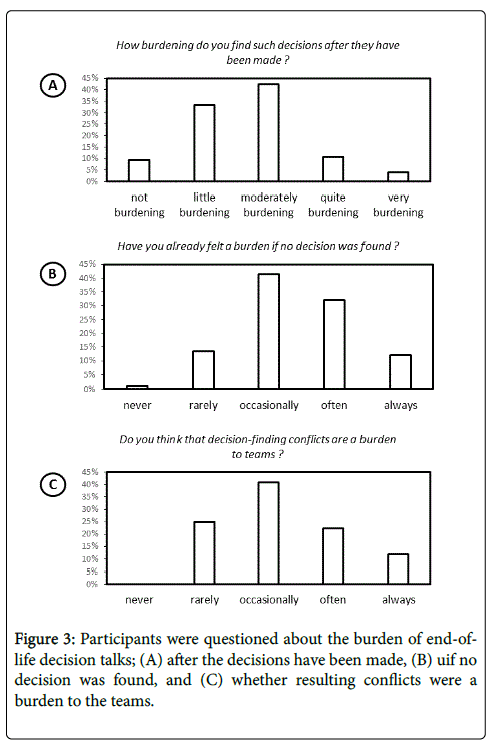
Regarding the question whether they felt that such decisions were a burden, 42 % said they were ‘moderately burdening’ . Most of the participants said that talks were burdening if no clear decision was found (Figure 3A and 3B).
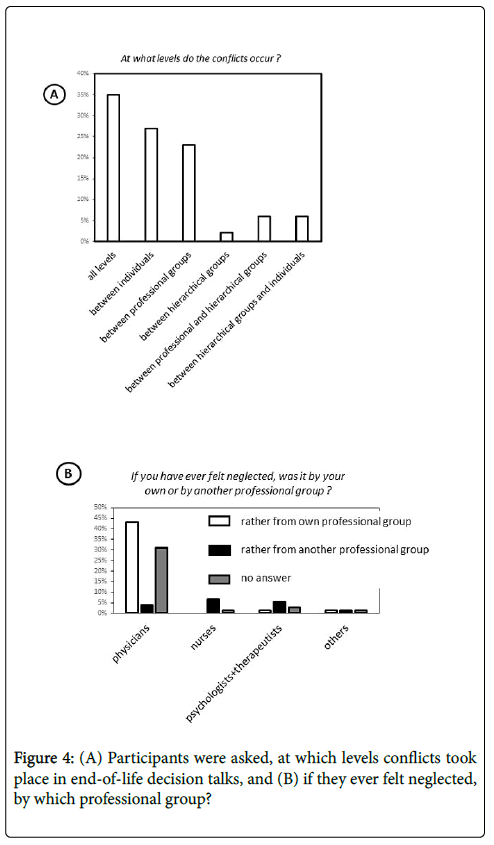
More than a third of the responders declared that conflicts in decision making were a burden to the teams (Figure 3C). We had further asked at which levels the conflicts occurred – whether rather between professional groups, within the hierarchy, or at individual levels.
It was possible to give more than one answer. 35 % responded that conflicts took place on all levels, and 27 % said it was mainly a question of individuals (Figure 4A).
The feeling of being ignored or neglected in an end-of-life decision talk may be a reason for conflicts within a team.
In our study, nearly all people told that all participants of such talks were allowed to talk (96%).
Also, the majority of respondents had “never ” (35%) or “rarely ” (42%) made the experience of being ignored or neglected, only 14 % declared that this was “occasionally ” the case. However, these numbers might also be related to the type of profession.
The physicians who had felt ignored blamed their own profession; the non-physicians said they were suppressed by another profession than their own (Figure 4B).
However, the number of non-physician respondents had been rather low.
For more than half of the respondents, talks only “rarely ” had an aggressive or irritated character, for a third “occasionally ”. Controversial discussions, however, were described by 50 as occurring “occasionally ” or even “often ” (Figure 5A and 5B).
Further data analysis regarding subgroups
For the further data analysis, first the variables were tested for normal distribution. Since no variable showed normal distribution, non-parametric tests like the Chi square test, U test, and nonparametric correlation analyses were performed.
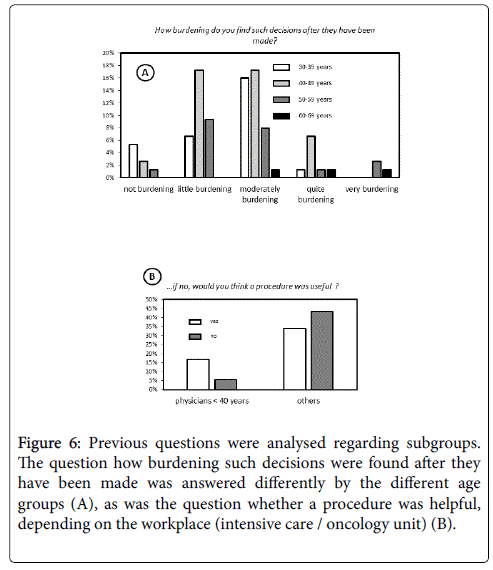
First we tested whether there was a correlation between age and feeling of burden by decision talks. We found that there was no clear trend (Figure 6A).
The same was tested for the sexes; here, using the U-Test, we found a significance of .038, indicating that women felt a higher burden than men.
Physicians younger than 40 years of age significantly more often wished to have a defined standard procedure for end-of-life decision talks (Figure 6B).
Figure 6: Previous questions were analysed regarding subgroups. The question how burdening such decisions were found after they have been made was answered differently by the different age groups (A), as was the question whether a procedure was helpful, depending on the workplace (intensive care / oncology unit) (B).
Asking whether there was a strong wish for a procedure, we found that a large proportion of those using a procedure also said that it was helpful, the majority of respondents however did not use one and did not wish one or was non-respondent for this question.
Further we found that those centers cooperating with an ethics committee often had a high level of structure, e.g. using protocols and summaries when organizing the talks.
Comparing age and feeling of burden, we found that the three participants >60 years of age felt a higher burden by such decisions (P=0,03).
And younger physicians preferred to have a standard procedure (P=0,05). Other correlations to sociodemographic parameters of the participants were not significant.
Our finding that in most cases decisions were first discussed within the team, than with parents (80%), is in concordance with published data from the Netherlands – here even all decisions were first discussed within the team.
Comparing Northern and Southern European pediatric intensive care units, Devictor et al. found that in Northern Europe 85%, in Southern Europe 68% of the parents were involved in shared decision making.
Free text statements
Some of the free text statements the respondents could make gave some insight into factors or attitudes that are relevant for the professionals working in this field.
The double-edged sword of shared decision between physicians and parents - and the burden of painful decisions - was described by a respondent who wrote: “the parents are involved but the responsibility for a decision remains with the treating physicians, in order to save the parents from feelings of guilt”. However, making decisions in the terminal phase of life does not only mean a burden, it may also help – as a nurse put it in our study: “thus it often becomes easier to deal with the patients, once they know for sure what is going on, and are no more in a state of suspense.”
Regarding our proposal of firm procedures or protocols for decision-making talks, one physician wrote in the freetext “- the talks are very individual and should be so. Thus, attempts to regulate them are not necessary ”.
Conditions for calm decision finding sometimes are difficult, as some respondents put it: “Limited resources of personnel or lack of time may hamper sufficient and satisfying discussions in some cases”
Discussion
Our study was intended to give a general answer on current practice and perceptions in pediatric end-of-life decision making in Germany. Further, we wanted to know whether these procedures could be optimized, both in order to find the best possible solutions for the children and their families, and to prevent team conflicts that might result from such situations.
Of course, the response rate of our questionnaire was relatively low, in particular in the non-physician group. However, this certainly is a common problem in comparable studies [26-28]. It may also be asked whether a questionnaire is the right method, since recently, a trend for qualitative studies in such fields of research has become common [19,20,29,30]. In our work, in addition to the questionnaire itself, we received some valuable qualitative information from the free textsections of the questionnaire. However, since we focussed on a quantitative analysis of the status-quo, our questionnaire method appeared to give the most solid data.
Most respondents declared that usually physicians, nurses and psychologists were involved in the end-of-life talks (35%), however, the second most answer was physicians alone (23%), which was more usual in oncology than in intensive care. Several studies stress the role of nurses for pediatric end-of-life decisions [7,12,14,20,31-33]: The nurses – next to the families - usually have the closest contact to the children, and often may act as a mediator [20]. Thus there is some space for improvement. However, it should be clear in advance whether they want to be involved; in a Netherland study from 2014 two thirds of 587 nurses - from all areas of care - declared that they had already participated in an end-of-life-decision talk, however, only 75 % of the nurses wished to be involved [31].
While involvement of nursing staff is subject to several published studies, the role of other non-physician professions is only occasionally discussed. Psychologists or teachers may also be able to give a significant contribution. A meta-analysis from 2006 [34] analyzed 12 studies showing a significant benefit in stress reduction for parents and their attitude towards the disease by psychosocial interventions. As we found, about 48% of all participants declared that other professional groups were involved. However, only few members of other professions participated in our study, and the responses were very heterogenous, making further firm conclusions impossible.
As we found, regular cooperation with clinical ethics committees is not a common standard. In a British study it was found that most clinical ethics committees had no more than 3 cases per year [35], and in a recent letter to the German Physicians‘ Journal, two ethicists declared that the ethical committees in Germany were not of much use, and clinicians should better improve their own capacity for ethical judgment [36]. In a German questionnaire, in 2004, only 28% of 36 head administrators of hospitals or nursery staff declared to involve clinical ethics committees on a regular basis [37], a finding in concordance with our observation. However, in our study several responders declared in the individual free text commentaries to have experienced significant benefit from clinical ethics committees. Thus, in conflict situations, involvement of an ethics committee is recommended by several authors [38]. This may also help to improve the structure of end-of-life decision talks [37]. From our study, however, the role of clinical ethics committees in pediatrics still remains a bit open.
Our finding that in most cases decisions were first discussed within the team, than with parents (80%), is in concordance with published data from the Netherlands – here even all decisions were first discussed within the team [21]. Comparing Northern and Southern European pediatric intensive care units, Devictor et al. found that in Northern Europe 85%, in Southern Europe 68% of the parents were involved in shared decision making [39].
Since legally, the parents bear the full responsibility for the decisions, this procedure might seem questionable. However – on the one hand, medical facts should be analyzed first, in order to assess medical indication separately from the patient’s or guardians’ wish. Besides, some physicians might intend to relieve the burden of a painful decision from the parents, as a respondent put it in the above mentioned free text of our questionnaire. In a meta-analysis from 2015, the needs of parents who had lost their children had been analyzed retrospectively [40]. Here, many respondents stressed the relevance of sufficient information – both for the decision making process and for the process of coping after the death of the child. Other aspects that were named were honesty and sensitivity in the communication. Thus, the success of shared decision making probably rather depends on such soft skills than on a well-defined procedure.
Several authors, however, advocate the establishment of guidelines for end-of-life decision making e.g., the European Council in 2014 published a “European Guide on the decision-making process regarding medical treatment in end of life situations”, written both for patients and medical personnel, giving an advice for shared decision making by patients, physicians and nurses. Still, there is the question whether a written guidance really can help. Many of the respondents in our study left the question whether a standard procedure would be helpful for end-of-life decisions unanswered (24/77). Or, as one physician put it in the above mentioned free text, talks might have a too individualized character to be standardized. Interestingly, among the physicians younger than 40 years, the majority preferred a procedure. This is in line with an observation from Munich indicating that physicians profit the more from a guidance the younger they are [41]. Apparently, legal uncertainties are reduced by guidance. This was also found by a study performed in 2008 at a pediatric hospital in Melbourne [42]. The importance of learning in this field is stressed by many authors [43,44].
We next attempted to analyze the burden of end-of-life decisions. Of course, seeing a patient suffer for whom no curative treatment is available, is very distressing both, for physicians and nurses. However, it is also painful to see a child receive never-ending invasive therapies, especially experimental therapies, which do not change the final outcome of the disease [45]. While some publications stressed the burden of end-of-life decisions in pediatric oncology [46], others described the satisfying aspects of end-of-life care [47]. Thus, making decisions in the terminal phase of life does not only mean a burden, it may also help by releaving the state of suspense, as a nurse put it in a free text in our study.
The question “How stressful is decision making for you?” was answered by most respondents as "moderately” in our study (46%). This is similar to the finding of Müller et al. who studied German intensive care units [48].
In the literature, the role of professional communication is stressed by several authors. By interviews with physicians, nurses, and psychosocial team members of a pediatric intensive care unit, Lee and Dupree could show that communication was a very relevant point, and well-organized discussion groups helped both to prevent patients and guardians, and the teams from conflicts [49]. Another US study showed heterogeneous perceptions of communication: while about 92% of the physicians believed that cases were discussed appropriately, only 59% of the nurses said so [18].
This hints to possible reasons for misunderstandings. In the study by Müller et al. involvement of nurses in decision making was described as protective factor for burn-out [48] similar conclusions were drawn in several Portuguese studies [26,29]. In our questionnaire, at least as a trend, the non-physicians felt stronger distressed by endof- life discussions than physicians, and women stronger than men. One third of the respondents also declared that team conflict regarding decision were “often ” or even “always ” a burden for the team. Another 40% said “occasionally ”. When we asked at which levels conflicts were observed, 35% answered that such conflicts occurred at all levels, i.e. within the professional hierarchy, between professional groups or individuals. Further 23% declared that conflicts occurred mainly between professional groups. In the CONFLICUS study this was even said by 32%. In this study, end-of-life decisions were even found to be one of the main reasons for conflicts in general [17].
In an interview study of 2009, the conflict between physician and nurses was described as the most relevant [44]. Similar observations were made in the study by Müller et al. [48]. In our study, 53% of the respondents told that “controversies and disagreements in the talks” occurred “occasionally ” or “often ”.
Thus, a high quality of end-of-life decision talks certainly plays an important role in the functioning of medical teams.
In this context, it is very important whether all participants of such talks feel taken serious and respectfully treated. When we asked if participants were ignored in the talks, 23 out of 59 physicians did not give any answer. Moreover, in the non-physician group, the majority of respondents declared to be ignored by another professional group (P=0,00), however, this was based on a small number.
In a Corean study, modes of conflict management were analyzed. The majority of physicians preferred to just wait and observe, while nurses most preferred to find a solution by discussions, in particular with the heads of the ward. [33]. Conflicts resulting from difficulties in decision making were also described in a Swiss study, and supervision was recommended [50]. In our study, supervision was provided the majority of respondents (71%). Some studies describe possible negative implications of conflicts even for the patients [17,27]. In intensive care units, misunderstandings might lead to medical mistreatment. This is, of course, in particular the case in conditions of much workload, as some respondents put it in the free text in our study: “Some rituals – a calm room, no beeper, enough time – are very important, yet not always present in daily practice…”
Conclusion
As a conclusion of our study, our impression in general is that the status quo in pediatrics is not too bad.
It is inevitable that every pathway to decision is a difficult one. Certainly standard operation procedures may be of some help, however it is the individual, practical communication that counts. It is quite encouraging that nearly 80% of the respondents confirmed that the medical decisions are made by interprofessional teams.
It should be standard that every participant's point of view can be articulated and is respected. Here, particularly regarding the involvement and participation of nurses in decision-finding, there still might be some room for improvement. Other professions, i.e. psychologists, teachers, or other therapists, may also be beneficial in decision making talks, however, unfortunately, our study is unable to contribute much in this field.
Whether ethical committees or external experts are helpful may be open, but besides helping to find the right answer, they may also help to limit internal team conflicts.
Thus, working on a better culture of end-of-life decision making in daily medical care still is an important task in modern pediatrics. Or, as a pediatric oncology nurse put it in our questionnaire- “I think it is very important to discuss this subject, since the acceptance of medical limits often is lost, and the patient’s benefit is not considered – I believe, the pro and cons of intensive therapies should more often be discussed – although in children’s medicine the standard certainly is a better one than in adults-”
Competing interests
All authors declare that they have no financial competing interests or non-financial competing interests that would cause them embarrassment were they to become public after the publication of the manuscript.
Authors' contributions
MN has made substantial contributions to conception and design, has acquired, analysed and interpreted the data; she has been involved in drafting the manuscript (first in German) and revising it critically for important intellectual content; she has given final approval of the version to be published; and she agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
CFC has made substantial contributions to conception and design, has supervised acquisition, analysis and interpretation of the data; he has been involved in drafting the manuscript (in English) and revising it critically for important intellectual content; he has given final approval of the version to be published; and he agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgements
The authors wish to acknowledge the superb help from all respondents to the questionnaire without which the study would not have been possible.
References
- Becker G, Sarhatlic R, Olschewski M, Xander C, Momm F, et al. (2007) End-of-life care in hospital: current practice and potentials for improvement.J Pain Symptom Manage 33: 711-719.
- Janssens U, Burchardi H, Duttge G, Erchinger R, Gretenkort P, et al. (2013) Therapeutic change and stop treatment in intensive care . Anesthetist 62: 47-52.
- Sjökvist P, Nilstun T, Svantesson M, Berggren L (1999) Withdrawal of life support--who should decide? Differences in attitudes among the general public, nurses and physicians. Intensive Care Med 25:949-954.
- Gillis J (2008) "We want everything done".Arch Dis Child 93: 192-193.
- Lorenz C (2012) End-of-life decisions - what is important for our routine duties in critical care medicine? AnasthesiolIntensivmedNotfallmedSchmerzther 47: 144-149.
- Führer M, Duroux A, Jox RJ,Borasio GD (2009) End of life decisions in pediatric palliative care . MonatsschrKinderheilkd157: 18-25.
- McMillen RE (2008) End of life decisions: nurses perceptions, feelings and experiences. Intensive Crit Care Nurs 24: 251-259.
- Cuttini M, Nadai M, Kaminski M, Hansen G, de Leeuw R, et al. (2000) End-of-life decisions in neonatal intensive care: physicians' self-reported practices in seven European countries. EURONIC Study Group. Lancet 355: 2112-2118.
- van der Heide A, van der Maas PJ, van der Wal G, de Graaff CL, Kester JG, et al. (1997) Medical end-of-life decisions made for neonates and infants in the Netherlands. Lancet 350: 251-255.
- Cohen S, Sprung C, Sjökvist P, Lippert A, Ricou B, et al.(2005) Communication of end-of-life decisions in European intensive care units. Intensive Care Med 31:1215–1221.
- Benbenishty J, Ganz FD, Lippert A, Bulow HH, Wennberg E, et al. (2006) Nurse involvement in end-of-life decision making: the ETHICUS Study. Intensive Care Med 32: 129-132.
- Jox RJ, Krebs M, Fegg M, Reiter-Theil S, Frey L, et al. (2010) Limiting life-sustaining treatment in German intensive care units: a multiprofessional survey. J Crit Care 25: 413-419.
- Graw JA, Spies CD, Kork F, Wernecke KD, Braun JP (2015) End-of-life decisions in intensive care medicine-shared decision-making and intensive care unit length of stay. World J Surg 39: 644-651.
- Ferrand E, Lemaire F, Regnier B, Kuteifan K, Badet M, et al. (2003) Discrepancies between perceptions by physicians and nursing staff of intensive care unit end-of-life decisions. Am J RespirCrit Care Med 167: 1310-1315.
- Vivian L, Marais A, McLaughlin S, Falkenstein S, Argent A (2009) Relationships, trust, decision-making and quality of care in a paediatric intensive care unit. Intensive Care Med 35: 1593-1598.
- Riessen R, Tränkle P,Schwabbauer N, Wolf K, Haap M (2011) Profession -border cooperation in the ICU . Intensivmed 48:389-395.
- Azoulay E, Timsit JF, Sprung CL, Soares M, Rusinová K, et al. (2009) Prevalence and factors of intensive care unit conflicts: the conflicus study. Am J RespirCrit Care Med 180: 853-860.
- Burns JP, Mitchell C, Griffith JL, Truog RD (2001) End-of-life care in the pediatric intensive care unit: attitudes and practices of pediatric critical care physicians and nurses. Crit Care Med 29: 658-664.
- Coombs MA, Addington-Hall J, Long-Sutehall T (2012) Challenges in transition from intervention to end of life care in intensive care: a qualitative study. Int J Nurs Stud 49: 519-527.
- Gallagher A, Bousso RS, McCarthy J, Kohlen H, et al. (2015) Negotiated reorienting: a grounded theory of nurses' end-of-life decision-making in the intensive care unit. Int J Nurs Stud 52: 794-803.
- de Vos MA, van der Heide A, Maurice-Stam H, Brouwer OF, Plötz FB, et al. (2011) The process of end-of-life decision-making in pediatrics: a national survey in the Netherlands. Pediatrics 127: e1004-1012.
- Joynt GM, Lipman J, Hartog C,Guidet B, Paruk F, et al. (2015) The Durban World Congress Ethics Round Table IV: health care professional end-of-life decision making. J Crit Care 30: 224-230.
- Einbecker recommendations of the German Society for Medical Law (DGMR) to the limits of medical treatment obligation in the most critically injured newborns. MedR1992:206
- Berlinger N, Barfield R, Fleischman AR (2013) Facing persistent challenges in pediatric decision-making: new Hastings Center guidelines. Pediatrics 132: 789-791.
- Winkler EC, Borasio GD, Jacobs P, Weber J, Jox RJ (2012) Munich Guideline on end of life decisions. ethics Med 24: 221-234.
- Cardoso T, Fonseca T, Pereira S, Lencastre L (2003) Life-sustaining treatment decisions in Portuguese intensive care units: a national survey of intensive care physicians.Crit Care 7: R167-175.
- Fassier T, Azoulay E (2010) Conflicts and communication gaps in the intensive care unit.CurrOpinCrit Care 16: 654-665.
- van der Heide A, Deliens L, Faisst K, Nilstun T, Norup M, et al. (2003) End-of-life decision-making in six European countries: descriptive study. Lancet 362: 345-350.
- Hernández-Marrero P, Pereira SM, Carvalho AS (2015) Ethical Decisions in Palliative Care: Interprofessional Relations as a Burnout Protective Factor? Results From a Mixed-Methods Multicenter Study in Portugal. Am J HospPalliat Care.
- Svantesson M,Sjökvist P, Thorsén H (2003) End-of-life decisions in Swedish ICUs. How do physicians from the admitting department reason? Intensive Crit Care Nurs 19: 241-251.
- Albers G, Francke AL, de Veer AJ, Bilsen J, Onwuteaka-Philipsen BD (2014) Attitudes of nursing staff towards involvement in medical end-of-life decisions: a national survey study. Patient EducCouns 94: 4-9.
- Bilgen H, Topuzoğlu A, Kuşçu K, Altuncu E, Ozek E (2009) End-of-life decisions in the newborn period: attitudes and practices of doctors and nurses. Turk J Pediatr 51: 248-256.
- Lee YH, Ahn D, Moon J, Han K (2014) Perception of interprofessional conflicts and interprofessional education by doctors and nurses. Korean J Med Educ 26: 257-264.
- Pai AL, Kazak AE (2006) Pediatric medical traumatic stress in pediatric oncology: family systems interventions.CurrOpinPediatr 18: 558-562.
- Whitehead JM, Sokol DK, Bowman D, Sedgwick P (2009) Consultation activities of clinical ethics committees in the United Kingdom: an empirical study and wake-up call. Postgrad Med J 85: 451-454.
- Strätling MWM, Sedemud-Adib B (2011) Ethics Consultation: Ethical core competencies in medicine retrieve DtschArztebl 110:A 825-828.
- Vollmann J, Burchardi N, Weidtmann A (2004) Health care ethics committees in German university clinics. A survey of all medical directors and directors of nursing]. Dtsch Medical Weekly 129: 1237-1242.
- Thompson BT, Cox PN, Antonelli M, Carlet JM, Cassell J, et al. (2004) Challenges in end-of-life care in the ICU: statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, Crit Care Med 32: 1781-1784.
- Devictor DJ, Nguyen DT (2004) Forgoing life-sustaining treatments in children: a comparison between Northern and Southern European pediatric intensive care units.PediatrCrit Care Med 5: 211-215.
- Xafis V, Wilkinson D, Sullivan J (2015) What information do parents need when facing end-of-life decisions for their child? A meta-synthesis of parental feedback. BMC Palliat Care 14: 19.
- Jox RJ, Winkler EC, Borasio GD (2012) Changing the treatment goal at the end of life: effects of a guideline at a hospital. Dtsch Medical Weekly 137: 829-833.
- Forbes T, Goeman E, Stark Z, Hynson J, Forrester M (2008) Discussing withdrawing and withholding of life-sustaining medical treatment in a tertiary paediatric hospital: A survey of clinician attitudes and practices. J Paediatr Child Health 44: 392-398.
- Solomon MZ, Sellers DE, Heller KS, Dokken DL, Levetown M, et al. (2005) New and lingering controversies in pediatric end-of-life care. Pediatrics 116: 872-883.
- Danjoux Meth N, Lawless B, Hawryluck L (2009) Conflicts in the ICU: perspectives of administrators and clinicians. Intensive Care Med 35: 2068-2077.
- Oberle K, Hughes D (2001) Doctors' and nurses' perceptions of ethical problems in end-of-life decisions. J AdvNurs 33: 707-715.
- Granek L, Bartels U, Scheinemann K, Labrecque M, Barrera M (2015) Grief reactions and impact of patient death on pediatric oncologists. Pediatr Blood Cancer 62: 134-142.
- Klassen A, Gulati S, Dix D (2012) Health care providers' perspectives about working with parents of children with cancer: a qualitative study. J PediatrOncolNurs 29: 92-97.
- Müller M, Pfister D, Markett S, Jaspers B (2009) [How many patient deaths can a team cope with?: A nationwide survey of palliative care units in Germany]. Schmerz 23: 600-608.
- Lee KJ, Dupree CY (2008) Staff experiences with end-of-life care in the pediatric intensive care unit. J Palliat Med 11: 986-990.
- Mpinga EK, Chastonay P, Pellissier F, Rapin CH (2006) [End of life conflicts: perceptions of health professionals in French speaking Valais].RechSoins Infirmpp: 96-107.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 12331
- [From(publication date):
March-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 11447
- PDF downloads : 884