Research Article Open Access
End of Life Decisions: Using Lectures, Small Groups and Standardized Patients to Develop Communication Skills
Scott De La Cruz*, Kelly White, Dan Johnson and Eva AagaardDepartment of internal medicine, University of Colorado School of Medicine, 7025 E. 21st Ave., Denver, CO 80207, USA
- *Corresponding Author:
- Dr. Scott De La Cruz
Department of internal medicine
University of Colorado, 7025 E. 21st Ave
Denver, CO 80207, USA
Tel: 720-941- 8076
Fax: 720-848-9502
E-mail: scott.delacruz@ucdenver.edu
Received date: December 07, 2011; Accepted date: January 04, 2012; Published date: January 10, 2012
Citation: De La Cruz S, White K, Johnson D, Aagaard E (2012) End of Life Decisions: Using Lectures, Small Groups and Standardized Patients to Develop Communication Skills. J Palliative Care Med 2:104. doi:10.4172/2165-7386.1000104
Copyright: ©2012 De La Cruz S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Study Background: Teaching communication skills to medical students is necessary and challenging. Our aim was to enhance student confidence in and ability to communicate with patients and families, particularly in difficult and complex medical situations.
Methods: Interactive didactics given to 146 third year medical students at the University of Colorado School of Medicine provided content and context for developing advanced communication skills. Students practiced these skills during standardized patient (SP) interactions involving 1) breaking bad news and 2) a family meeting to address goals of care. The course was assessed using: 1) student self-assessment, 2) SP assessment of student’s performance, and 3) results of the medical school graduation questionnaire.
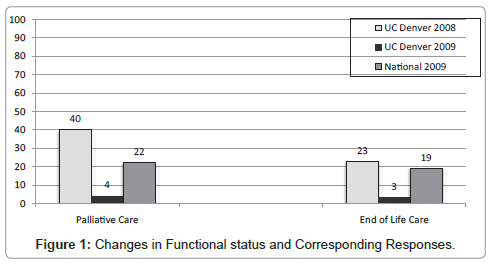
Results: Students felt better prepared to deliver bad news (93.9% either agreed or strongly agreed with this statement), manage family meetings (95.3% agreed or strongly agreed) and communicate with patients and families (95.3% agreed or strongly agreed). More than 80% of students consistently demonstrated key skills during SP encounters including: eliciting understanding, responding to emotion, and avoiding false reassurances. Four percent and 3% of students who completed this curriculum reported that they received inadequate palliative or end of life care instruction compared with 22% and 19% of all students nationally (respectively).
Conclusion: A multimodal medical student curriculum in advanced communication skills is feasible and effectively teaches these skills.
Keywords
Palliative care; Medical education; Communication; End of life; Breaking bad news
Abbreviations
EOL: End of Life; SP: Standardized Patient
Introduction
As the population of the United States ages and people are living longer with terminal diseases, palliative care is becoming increasingly important. In 2006, in recognition of the inadequacy of end-of-life (EOL) education, the Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Medical Specialties (ABMS) designated palliative care as an official medical subspecialty. Since then, medical schools and residency programs have been charged with incorporating EOL care into the curriculum [1]. However, EOL education remains limited in quantity and inadequate in scope [2-5]. Many of the existing programs consist of lectures and seminars in the various aspects of palliative care, but offer little or no opportunity to gain clinical experience. A survey of family medicine residents revealed that practice is specifically needed in the areas of delivering bad news, reflective listening, providing patient-centered empathetic care, and addressing patients’ and families’ conflicting wishes and emotional and spiritual needs [6].
Effective communication between doctor and patient has been described as a central clinical function and poor communication between physicians and patients can leave patients with uncertainties about their diagnosis or prognosis and confusion about test results and treatment plans [7,8]. In 1999, the ACGME and ABMS stated that “interpersonal and communication skills that result in effective information exchange and teaming with patients, their families, and other health professionals” is a core area of competency required of all physicians [9]. Our aim was to develop a curriculum on advanced communication skills and EOL care to enhance students’ confidence in and abilities to deliver bad news, conduct patient/family meetings, recognize and accommodate common reactions (especially emotions) to difficult news, and identify cues that may suggest a lack of patient or family understanding.
Materials and Methods
In December of 2007 (Graduating Class of 2009), we introduced a weeklong curriculum to 149 third year students, just after the fourth core clinical clerkship (see online appendix 1 for the pertinent syllabus). During their first and second year, these students received 16 hours of classroom based instruction to build knowledge of core principles of EOL care (introduction to hospice and palliative medicine, EOL ethics, physiology and psychology of dying, pain pharmacology, spirituality, and self-care). In addition, approximately two-thirds of the students had received additional exposure to EOL care through a required oneday, community-based hospice experience (during their ambulatory medicine rotation), and a 5-hour, required interactive didactic session on pain management, shared decision making and discussing resuscitation status (during their inpatient medicine rotation). With the exception of the new weeklong 3rd year curriculum, the 1st, 2nd and 3rd year curricula were the same for the classes of 2008 and 2009.
Bruner’s Constructivist Theory was used to develop this curriculum and the overall EOL and advanced communication curriculum taught at our institution. This theory emphasizes that learning is an active process in which learners base new ideas and concepts on prior knowledge [11]. The cognitive structures formed (schema, mental models, etc.) provide meaning and organization to experiences. Two key principles of Bruner’s Constructivist Theory are that instruction must be concerned with the experiences and contexts that make the student willing/able to learn and that instruction is best structured spirally, building on itself sequentially over time.
During the new weeklong curriculum, students participated in a series of interactive lectures, small group exercises, movies and standardized patient (SP) exercises designed to enhance their knowledge, build confidence and encourage skill building in EOL care. The course was implemented after the mid-point of 3rd year when many students will have encountered death and participated in or observed EOL care discussions. These experiences underscore the challenges faced in these situations, thereby creating motivational discomfort to learn the material. The curriculum we created reinforced key EOL instruction that was provided during the 1st two years, and built upon it, creating the spiral organization emphasized in Constructivist Theory.
Throughout the week of curriculum, lectures and discussions were led by local experts, patients and caregivers on topics such as Breaking Bad News, Practical Tools for Cultural Conversations, The Financial and Emotional Costs of Chronic Care, Assessing and Managing Symptoms in Advanced Illness, and Conducting the Family Meeting. Small Groups allowed students to discuss related ethical topics such as withdrawal of life-sustaining treatment and physician-assisted suicide and provided an opportunity for students to reflect on their feelings and experiences around these issues. Reflective writing encouraged students to discuss how their personal experiences with death and other challenging patient care experiences have changed their views of medicine and themselves. Movies and non-clinical readings portraying different cultural and spiritual experiences with disease and dying provided students with foundational knowledge and prompted discussion of challenging topics. The various teaching formats were selected to appeal to different learning styles in an attempt to maximize student participation and engagement with the material [10,12].
In order to practice the concepts being taught, students worked in pairs to complete two standardized patient (SP) interactions (“Breaking Bad News” and “The Family Meeting”) designed to simulate a series of challenging patient/family interactions (see appendix 2 for detailed description). The initial visit lasted 30 minutes and focused on informing a patient and her husband that her recent memory changes were likely due to Alzheimer’s disease. The subsequent 60-minute visit involved the same patient, 7 years into her illness after being admitted for recurrent aspiration pneumonia, and asked the students to lead a family meeting regarding goals of care and EOL issues. Students were carefully matched to the same SPs throughout their series of visits. SPs provided directive formative feedback immediately following each of the encounters. Debriefing sessions comprised of 15-20 students and 1-2 faculty facilitators followed each SP encounter and focused on the similarities and differences in the various student experiences, and spiritual and cultural issues in EOL decision-making.
Achievement of course objectives was evaluated using 3 sources: 1) student self-assessment of their achievement of course objectives, 2) SP assessment of student’s performance after each encounter, and 3) results of the medical school graduation questionnaire. Students (n=149, response rate 100%) evaluated their perceived achievement of course objectives via a required online survey using a 4-point scale (1=Strongly Disagree, 2=Disagree, 3=Agree and 4=Strongly Agree). SPs evaluated specific communication and interpersonal behaviors of students following each interaction using a scaled checklist (1=did not complete the task or designated behavior, 2=minimally completed the task or rarely demonstrated designated behavior, 3=mostly completed the task or sometimes demonstrated designated behavior, 4=fully completed the task or consistently demonstrated designated behavior). Students were surveyed upon graduation from medical school as part of the national graduation questionnaire (GQ) administered annually by the Liaison Committee for Medical Education. They were asked about their perception of the adequacy of the instruction they received in various topics including palliative and EOL care with the question: “Do you believe that your instruction in the following areas was inadequate, appropriate, or excessive?” GQ data from the class of 2009 was analyzed and compared to results from the class of 2008 (prior to implementation of the EOL curriculum) and the national sample of graduating students in 2009.
Results
Students felt they gained knowledge and skills during this course that [made them] better prepared for future clinical rotations (96% either agreed or strongly agreed with this statement), to practice in their chosen specialties (93.2% agreed or strongly agreed), and to better communicate with patients and their families (95.3% agreed or strongly agreed). Students felt better prepared to deliver bad news to patients (93.9% agreed or strongly agreed) and manage family meetings (95.3% agreed or strongly agreed). They felt they had a better understanding of the emotional and physical costs to the caregiver (98% agreed or strongly agreed) and of the challenges associated with advance directives and EOL planning (97.4% agreed or strongly agreed). Finally, students felt that they could better analyze the ethical issues that they will likely encounter in clinical practice (89.2% agreed or strongly agreed). The percentages of the student responses are presented in Table 1.
| % Students responding: | ||||
|---|---|---|---|---|
| Strongly Agree | Agree | Disagree | Strongly Disagree | |
| I feel better prepared for future clinical rotations |
46.0% | 50.0% | 4.0% | 0% |
| I feel better prepared to practice in my chosen specialty | 40.2% | 53.0% | 6.8% | 0% |
| I feel better prepared to communicate with patients and their families. | 55.0% | 40.3% | 4.7% | 0% |
| I feel better prepared to deliver bad news to patients | 42.2% | 51.7% | 6.1% | 0% |
| I feel better prepared to manage family meetings. | 37.6% | 57.7% | 4.7% | 0% |
| I feel I have a better understanding of the emotional and physical costs to the caregiver | 37.6% | 60.4% | 2.0% | 0% |
| I feel I have a better understanding of the challenges associated with advance directives and end of life planning | 33.6% | 63.8% | 2.0% | 0.6% |
| I feel I can better analyze the ethical issues that they will likely encounter in clinical practice | 26.8% | 62.4% | 10.8% | 0% |
Table 1: StudentâÂ?Â?s reported level of agreement with the following statements.
There were 76 SP/student encounters during the first SP session- “Breaking Bad News” and 75 during the second session- “The Family Meeting”. This reflects that students worked through the SP encounters in pairs, rather than individually. The discordance in number of encounters for session 1 vs. session 2 represents students who were unable to attend the second session due to acute illness or family emergency. Table 2 describes student performance on the communication behaviors assessed by the SPs in areas such as nonverbal communication, listening, and concise verbal communication.
| % SP responding: | ||||
|---|---|---|---|---|
| “4” | “3” | “2” | “1” | |
| Provided information using simple, jargon-free language | 59.2% | 38.2% | 2.6% | 0% |
| Tolerated silence/listened without interruption | 75.0% | 19.7% | 5.3% | 0% |
| Responded to emotion | 48.7% | 47.3% | 4.0% | 0% |
| Conveyed genuine caring | 73.7% | 26.3% | 0% | 0% |
| Facilitated introductions | 77.0% | 23.0% | 0% | 0% |
| Clarified purpose/goal for the meeting | 70.3% | 25.7% | 4.0% | 0% |
| Invited conversation with an open body position | 82.9% | 17.1% | 0% | 0% |
| Makes and maintains appropriate eye contact | 92.1% | 7.9% | 0% | 0% |
| Avoids giving false reassurances or misleading information | 69.7% | 27.6% | 2.7% | 0% |
| Summarized medical issues and clarified key decisions | 56.8% | 36.5% | 6.8% | 0% |
| Ensured adequate time without interruption | 64.5% | 32.9% | 2.6% | 0% |
| Explored what the patient would want under the circumstances | 90.5% | 8.1% | 1.4% | 0% |
| Elicited family members’ hopes/fears/preferences | 75.7% | 23.0% | 1.3% | 0% |
| Identified and communicated shared goals | 50.0% | 44.6% | 5.4% | 0% |
| Communicates personal availability and ongoing attention | 77.6% | 17.1% | 4.0% | 1.3% |
Table 2: Communication Behaviors Demonstrated By Students During SP Encounters*.
Medical school graduation questionnaire data is presented in Figure 1. Only 4% and 3% of students who completed this curriculum reported that they received inadequate palliative or end of life care instruction respectively compared with 40% and 23% in the year prior to implementation and 22% and 19% of students nationally.
Discussion
This weeklong curriculum on advanced communication and EOL care was well received by medical students and associated with high student self-perceived knowledge of and skills in EOL care, as well as excellent SP-assessed performance during challenging communication encounters. Even after graduation, students perceived their education in these skills to be adequate at much higher rates than students from University of Colorado School of Medicine prior to curriculum implementation and as compared to students nationally.
This curriculum utilizes didactics, interactive lectures, films, small group learning environments, and SP practice sessions. Incorporating different teaching modalities appeals to different learning styles and allows students to construct new ideas and concepts based on current or past knowledge, theoretically providing an optimal learning environment [10,11]. Other programs that have been developed to teach palliative care and communication skills in the medical school setting have also incorporated multiple modalities, including small group sessions, didactics, and standardized patient encounters, and their results are also generally positive [13-15].
Traditionally, evaluation of advanced communication curricula has been limited to assessing the clinical knowledge acquired during the course [6,16]. Few studies have assessed the impact of an educational program in palliative care on interpersonal and communication abilities [17,15]. Our study addresses both issues by asking SPs to evaluate the students’ performance in the practice sessions in addition to asking students to complete the overall course evaluation. We also demonstrate a lasting impact of the curriculum on student perception of their learning through the results of the graduation questionnaire.
There are some limitations to this curriculum and its evaluation. Although proven to be very effective at teaching clinical skills to medical students, SP encounters are time consuming and financially expensive [18-20]. Also, the reliability and validity of the use of 2 SP assessments remains unknown. We incorporated SP evaluations to be used primarily as feedback mechanisms rather than as reliable evaluations of clinical skills. Assessing individual medical student performance is difficult as students were paired in an attempt to balance encounter time and patient simulation costs. Several different skill sets are needed to lead successful EOL discussions (clinical knowledge, cultural competency, advanced communication, etc.), making it challenging to assess each skill individually. Furthermore, it is difficult to assess the specific effects of the individual components of the weeklong curriculum on overall skills, thus, it is unclear whether all components are necessary to achieve similar results. Finally, it is unclear how evaluations and self-reported efficacy at this early point in medical students’ careers will translate to actual practice in the clinical environment, either now or in the future.
In conclusion, a teaching approach that targets several different learning styles via a series of lectures, discussions, films and small groups and then reinforces its objectives with serial SP interactions leads to improved perception of knowledge and skills in EOL care and suggests development of skills as documented by SPs. Development of a comparable, multimodal curriculum for implementation in the graduate medical education setting could further address ACGME competencies in advanced communication and palliative care. Further studies are needed to assess the impact of such a curriculum on actual practice and patient care outcomes.
Acknowledgements
Contribution: The authors wish to thank Dr. Paritosh Kaul and course coordinator Christy Linsenmaier.
References
- von Gunten CF, Ferris FD, Emanuel LL (2000) The patient-physician relationship.Ensuring competency in end-of-life care: communication and relational skills. JAMA 284: 3051-3057.
- Martini CJM, Grenholm G (1993) Institutional responsibility in graduate medical education and highlights of historical data. JAMA 270: 1053-1060.
- Plumb JD, Segraves M (1992) Terminal care in primary care postgraduate medical education programs: A national survey. Am J Hosp Palliat Care 9: 32-35.
- Goldberg R, Guadagnoli E, LaFarge S (1987) A survey of house staff attitudes towards terminal care education. J Cancer Educ 2: 159-163.
- Barzansky B, Veloski JJ, Miller R, Jonas HS (1999) Education in end-of-life care during medical school and residency training. Acad Med 74: l02-104.
- Burge F, McIntyre, P, Kaufman D, Cummings I, Frager, G, et al. (2000) Family medicine residents knowledge and attitudes about end-of-life care. J Palliat Care 16: 5-12.
- Simpson M, Buckman R, Stewart M, Maquire P, Lipkin M, et al. (1991) Doctorpatient communication: the Toronto consensus statement. BMJ 303: 1385- 1387.
- Bruera E, Sweeney C, Calder K, Palmer L, Benisch-Tolley S (2001) Patient preferences versus physician perceptions of treatment decisions in cancer care. J Clin Oncol 19: 2883-2885.
- http://www.acgme.org/acWebsite/home/home.asp
- Newble DI, Entwistle NJ (1986) Learning styles and approaches: Implications for medical education. Med Educ 20: 162-175.
- Bruner JS (1990) Acts of meaning. Cambridge: Harvard University Press, Cambridge, Massachusetts, USA.
- Shaughnessy AF, Slawson DC (1999) Are we providing doctors with the training and tools for lifelong learning?. Interview by Abi Berger. BMJ 319:1280.
- Deveugele M, Derese A, De Maesschalck S, Willems S, Van Driel M, et al. (2005) Teaching communication skills to medical students, a challenge in the curriculum? Patient educ Couns 58: 265-270.
- van Dalen J, Zuidweg J, Collet J (1989) The curriculum of communication skills teaching at Masstricht medical school. Med Educ 23: 55-61.
- Yedidia M, Gillespie C, Kachur E, Schwartz MD, Ockene J, et al. (2003) Effect of communications training on medical student performance. JAMA 290: 1157- 65
- Rawlinson F and Finlay I (2002) Assessing education in palliative medicine: Development of a tool based on the Association of Palliative Medicine core curriculum. Palliat Med 16: 5-51.
- Lloyd-Williams M, MacLeod RD (2004) A systematic review of teaching and learning in palliative care within the medical undergraduate curriculum. Med Teach 26: 683-690.
- Hodges B, Hanson M, McNaughton N, Regehr G (2002) Creating, monitoring, and improving a psychiatry OSCE: a guide for faculty. Acad Psychiatry 26: 134-61.
- Wallace J, Rao R, Haslam R (2002) Simulated patients and objective structured clinical examinations: review of their use in medical education. Advances in Psychiatric Treatment 8: 342-348.
- Bokken L, Rethans JJ, van Heurn L, Duvivier R, Scherpbier A, et al. (2009) Students' views on the use of real patients and simulated patients in undergraduate medical education. Acad Med 84: 958-63.
Tables and Figures at a glance
| Table 1 | Table 2 |
Figures at a glance
 |
| Figure 1 |
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 13971
- [From(publication date):
January-2012 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 9404
- PDF downloads : 4567