Research Article Open Access
End-of-Life Care for Aged Care Residents Presenting to Emergency Departments
Jo-Anne Wilkinson1*, Maryann Street2,3, Sonia Fullerton1 and Patricia M Livingston2,3
1Eastern Health251 Mountain Highway, Wantirna 3152, Australia
2Faculty of Health, Deakin University, 221 Burwood Highway, Burwood Victoria 3125, Australia
3Eastern Health, 251 Mountain Highway, Wantirna 3152, Australia
4Faculty of Health, Deakin University, 221 Burwood Highway, Burwood Victoria 3125, Australia
- *Corresponding Author:
- Jo-Anne Wilkinson
RN, Grad Dip Nat, Eastern Health, 251 Mountain Highway
Wantirna 3152, Australia
Tel: 040061894
Fax: 613-9955- 1384
E-mail: Jo-anne.wilkinson@easternhealth.org.au
Received date March 27, 2012; Accepted date June 21, 2012; Published date June 25, 2012
Citation: Wilkinson JA, Maryann, Fullerton S, Livingston PM (2012) End-of-Life Care for Aged Care Residents Presenting to Emergency Departments. J Palliative Care Med 2:121. doi:10.4172/2165-7386.1000121
Copyright: © 2012 Wilkinson JA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: The number of patients from Aged Care presenting to acute care is increasing, many of whom have a life limiting illness.
Aims: To identify differences in relation to Aged Care Residents presenting to Emergency departments who died during a hospital admission compared to those who were referred to the hospital based palliative care. Methods: Review of a stratified random sample of 90 Aged Care residents transferred to acute care who died during admission in 2009; half the sample received palliative care. Comparisons were made with regard to age; gender; co-morbidities; symptoms, investigations and active treatment; prior admissions and costs. Results: The median age of patients was 87.5 years, 61% were female and 38% had three or more admissions in the year prior to death. Patients with a length of stay of four or more days were 2.98 times (CI, 95%:1.11-8.03) and patients with agitation were 3.08 (CI 95%:1.10- 8.64) times more likely to be referred to palliative care. Patients who received palliative care had significantly fewer investigations or active treatment in the 24 hours prior to their death (p< 0.01) and palliated patients had significantly lower average costs per day of admission ($1022, SD=$441) compared to those who were not palliated ($ 831; SD= $ 1041) (p< 0.001). Discussion: Our study indicates there is a difference between dying patients who received palliative care compared to those who did not in an acute care setting. Further research into the outcomes of patients discharged back to Aged Care facilities for palliative care warrants investigation.
Keywords
Aged care facilities; Emergency departments; Palliative care; End of life care
Introduction
In 2010, there were over 166,000 residents in Australian residential aged care services. More than half were aged 85 years or over and 71% required high care [1]. This is predicted to increase exponentially with the ageing of the population. Australia’s population will increase significantly over the next 50 years, with approximately one in four Australians being 65 years or older by 2056. Moreover, people aged 85 years or over will account for up to 7% of the Australian population [2].
The number of people from Aged Care facilities presenting to Emergency Departments (EDs) is increasing, many of whom may be at the end stage of a life threatening illness [3,4]. Older patients occupy a disproportionate number of public hospital bed days and are more likely to have co-morbidities and chronic conditions resulting in complex care requirements [4]. Older patients are often admitted into the acute hospital system when in theory more appropriate strategies could be in place where the patient could return to their residential care facility and familiar surroundings, for end of life care [5].
Palliative care focuses on improving the quality of life for patients with advanced illness through pain and symptom management, communication and support for medical decisions which reflects goals of care, with the assurance of a safe transition between acute and subacute care settings [6]. Hospital Based Palliative Care Consultation Teams (HBPCCT) have been shown to improve care for adults with life threatening illnesses while providing significant hospital cost savings [7]. Referral to HBPCCT can occur for many reasons i.e. symptom management, support of EOLC, discussions around goals of care and discharge planning. Referral has usually been agreed upon by the treating medical team after discussion with patient and or family that active medical treatments will no longer restore health. An assessment is then carried out by the HBPCT and a plan put in place.
In 2004, the Commonwealth Government’s Department of Health and Ageing developed Guidelines for Palliative Care in Residential Aged Care [8], to assist with palliation and End-of-Life Care (EOLC) in Aged Care. Despite the introduction of these Guidelines, there appears to be a lack of understanding among clinical staff and families concerning the ability for staff in Aged Care facilities to appropriately palliate their dying residents. Failure to do so can result in poor outcomes for the residents, as well as poor health system outcomes when dying residents are inappropriately transferred to emergency departments [3,5].
The aims of this study were to describe the clinical profile, outcomes and costs associated with an episode of care among patients presenting to emergency departments from Aged Care facilities across one health service in Victoria and compare dying patients who received palliative care to those who did not.
Methods
A retrospective audit was conducted of all people transferred from Aged Care facilities to any of the three acute care hospital sites within one metropolitan health service from 1st January to 31st December 2009.
The health service is the second largest of Victoria’s 18 Public Health Services, which supports the health care needs of the eastern metropolitan Melbourne population and covers a geographical catchment of approximately 2,800 square kilometres. Services are delivered from a range of acute, sub-acute, residential and community based facilities, providing a combined total of 915 acute inpatient beds and 158 sub acute beds. There are approximately 9,500 Residential Care places (high and low level care) in the catchment area of this health service.
Data were integrated from three sources: patient medical records, Eastern Health Information Service cost-weight data set and the Victorian Emergency Minimum Dataset (VEMD). The VEMD comprises demographic, administrative and clinical data detailing ED presentations at Victorian public hospitals.
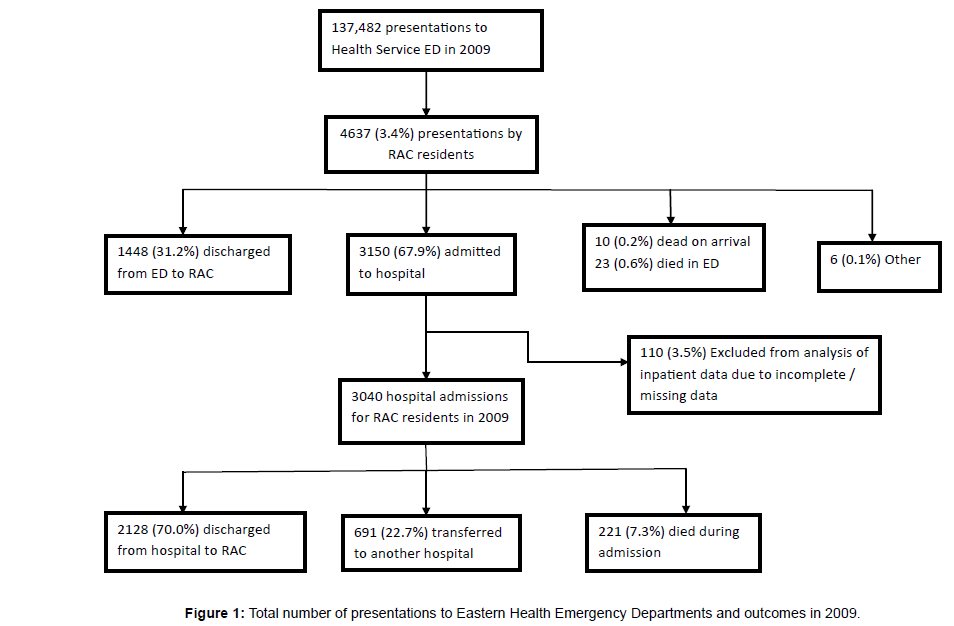
In 2009, there were 137,482 total patient presentations to the health service EDs. Of these presentations 4,737 (3.4%) were from Aged Care facilities resulting in 3,150 admissions (67.9%). Overall, 10 clients were pronounced dead on arrival to ED, 23 died in ED, 221 patients died in hospital; 54% of those patients who died in hospital were referred to palliative care. A random sample of 90 patients was selected from the 221 patients who died during the hospital admission. The sample was stratified by referral to the HBPCCT, such that half the sample received palliative care and half did not receive palliative care prior to death (Figure 1).
Data comprised demographic (age and gender), administrative (level of care at residential accommodation, admitting hospital, number of admissions in year prior to death), clinical data (diagnoses at admission, triage category, length of stay in ED, admission details, co-morbidities, symptoms, investigations and interventions during admission and in the 24 hours prior to death, complications, and length of hospital admission), documented advance care plans, family meetings and Limitation of Treatment orders and inpatient cost data. Comparisons were made between those patients referred to palliative care and those who did not receive palliative care during their final admission.
The study received ethical approval from the Health Service Research and Ethics Review Panel and Deakin University Human Research Ethics Committee.
Statistical analysis
Descriptive statistics(frequencies, percentages, measures of central tendency) were used to explore the patient characteristics (age) and outcome measures (length of stay in ED, length of hospital admission, number of co-morbidities, number of symptoms, number of investigations or interventions and number of previous admissions in the year prior to death). Frequency distributions were reported for categorical variables (gender, level of care at residential accommodation, Australian Triage Scale (ATS) category, presence or absence of symptoms, co-morbidities and complications, care plan variables and investigations or interventions during admission and in 24 hours prior to death).
Kolmogorov-Smirnov and Shapiro_Wilks tests were used to assess the normality of the data. Where data were not normally distributed (indicated by p < 0.05 in either test), medians and Inter Quartile Ranges (IQR) are presented. For comparison of outcome measures between those patients who received palliative care and those who did not, chisquare tests were used for categorical data (triage category, number of admissions in year prior to death, co-morbidities and symptoms) and Mann-Whittney rank sum tests for non-parametric continuous data (age, length of stay in ED, length of admission, days from admission to Not for Resuscitation orders, days from admission to palliative care referral, days from palliative care referral to death, cost per day of admission, total inpatient costs, number of co-morbidities, number of symptoms, number of investigations and interventions).
Logistic regression (using the hierarchical stepwise method of model building) was used to explore the relationship between symptoms, comorbidities and referral to palliative care, based on the following predictors: age, gender, number and type of symptoms, number and type of interventions or investigations.
Two tailed tests were used and a level of significance was set at p < 0.05 with 95% confidence limits. Data were analysed using SPSS version 17; (SPSS, Inc. Chicago, IL).
Results
The median age of patients included in the sample was 87.5 years, and 61% were female. Overall, 50% were from high level care, 40% were from low level care and 10% were transferred to ED from transitional care.
Patient outcomes
The median length of stay in ED for Aged Care residents was 7.8 hours (IQR: 5.8-11.9) and the median hospital admission was 4.3 days (IQR 1.7-8.2). Patients referred to the HBPCCT had a longer median hospital admission (six days) compared to those who did not receive palliative care (two days) (Mann Whitney U = 630.5, n=90, p= 0.002). For those patients referred to palliative care services, the median number of days from admission to referral was four days, with a range of 1-7 days (Table 1).
| Length of Stay (n=90) | Median (IQR) | Range |
|---|---|---|
| Emergency Department | 7.8 hrs (5.8-11.9) | 2-29 hrs |
| Hospital Admission | 4.3 days (1.7-8.2) | <1-47 days |
| No Palliative Care (n=45) | 2 days (1- 7.5) | 1-48 days |
| Palliative Care (n=45) | 6 days (3.4-10) | 1-35 days |
| Days from Admission to: | ||
| Limitation of treatment orders (n=73) | 0 days (0-1) | 0-16 days |
| Palliative Care Referral (n=45) | 4 days (1-7) | 0-31 days |
| Days from Palliative Care: | ||
| To death (n=45) | 2 days (1-4) | 0-16 days |
Table 1: Patient outcomes from Aged Care Residents presentating to Emergency Department.
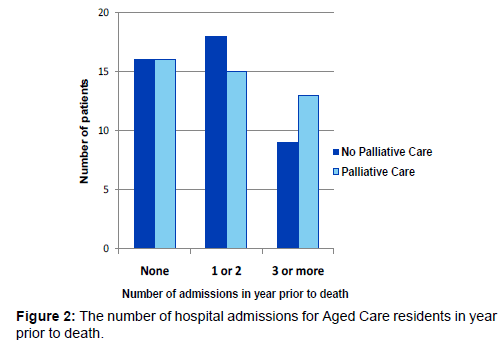
The number of prior admissions did not predict whether a patient was referred to palliative care services (χ2 = 0.989, df= 2,p= 0.61) (Figure 2).
Two-thirds of patients had an admission to acute care in the previous year (range: 1- 8). A total of 34 (38%) patients had three or more prior admissions in the previous year, however, this did not predict whether a patient received a palliative care referral or Advance Care Planning (ACP). Although 30% of patients in the sample had three or more admissions and 17% had five or more admissions in the previous year, only 12 (13%) received ACP documentation. Where ACPs were documented, compliance with these orders did not occur in 3 (25%) patients.
Patients referred to the HBPCCT were more likely to have symptoms of restlessness (p< 0.01); agitation (p< 0.01) or fitting (p< 0.05). In contrast, there was no significant difference in referral to palliative care based on symptoms of pain, nausea/ vomiting, respiratory secretions, shortness of breath oranxiety. Similarly, co-morbidities of cancer, congestive cardiac failure, chronic obstructive airway disease, renal failure, cerebrovascular accident or dementia were not associated with referral to palliative care. The number of symptoms and the number of co-morbidities was not associated with referral to the HBPCCT.
A logistic regression demonstrated a significant relationship between agitation and delirium (p= 0.002), agitation and restlessness (p= 0.001) and fitting and restlessness (p= 0.005). Patients with a length of stay of four or more days were 2.98 times (CI, 95%:1.11- 8.03) and patients with agitation were 3.08 (CI 95%:1.10- 8.64) times more likely to be referred to palliative care.
Patients who received palliative care had significantly fewer investigations or active treatment in the 24 hours prior to death (p< 0.01), in particular intravenous (IV) antibiotics, IV fluids or radiology.
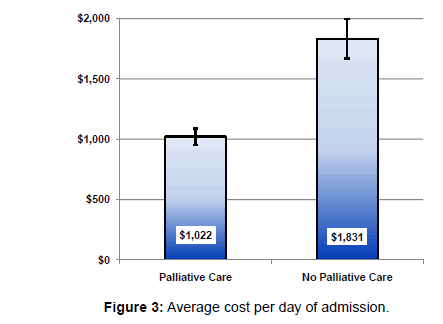
The total cost of hospital admission for patients in the sample ranged from $ 720 to $ 48, 210, with a mean (SD) of $ 7,287 ($ 7,658). Patients referred to the HBPCCT had a 44% lower average cost per day of admission ($ 1,022) compared to those who were not referred ($ 1,831; p< 0.001) (Figure 3).
Discussion
This study provides important information on presentation patterns and potential gaps in relation to Aged Care residents presenting to EDs who may require end of life care. Moreover, the study highlights the potential cost saving associated with presentation to ED and hospital admission for Aged Care residents who were referred to palliative care services. Finally, the findings of this study improve our understanding of the clinical characteristics of dying Aged Care residents who present to ED.
The results highlighted that ACP was suboptimal for patients who had multiple hospital admissions in the year prior to death and adherence to ACPs was substandard with 25% of cases not complying with ACP documentation. This result identifies the need for further research and program initiatives to improve compliance with individualised ACP for Aged Care residents requiring end of life care.
The current study demonstrated a reduction in bed day cost of 44% for patients seen by the HBPCCT, compared with dying patients who were not seen by the palliative care team, although the total inpatient costs were similar for the two groups. Patients who were seen by the palliative care team had significantly fewer interventions in the last day of life, and hence reduced costs. HBPCCT has been shown to improve physical and psychological symptom management, caregiver well-being, and family satisfaction [9]. Previous research [7] has demonstrated a reduction in total cost per hospital admission of US$ 4900 for a dying patient seen by the HBPCCT.
Triggers for a referral to a palliative care service often relate to symptom management [6]. The triggers for a referral to the palliative care consultation service in this study appeared to be less directed at symptoms distressing to the patient (pain, delirium, nausea) and more at those features distressing to staff or family (agitation and fitting) and the health service (length of stay). For patients included in this study, the delay in referral to palliative care was evident, in that the average time from admission to referral was twice as long as the time from referral to death. Late referrals and non referrals to palliative care have been associated with fear by medical practitioners of losing management of the patient in the end of life care. The transition from cure to comfort is difficult for healthcare providers, patients and their families [10]. There are currently no standardized criteria to determine when a referral to a palliative service should be triggered [11].
The results of this study must be assessed in light of its limitations. The study did not include patients who were discharged back to Aged Care facilities to die with a Palliative Care plan in place. Therefore the results may reflect a conservative estimate of the cost saving associated with palliative care referral. The sample size for this study was small, however, the results demonstrated significant differences between the two patient groups. Despite these limitations, further research into the outcomes of patients discharged back to Aged Care facilities for palliative care is worth investigation.
Author Disclosure Statement
This study was undertaken by the authors without external funding. No author has competing financial interests through receipt of payment or services from a third party for any aspect of this study. There are no real or perceived.
References
- Australian Institute of Health & Welfare (AIHW) (2011) Residential aged care in Australia 2009-10: a statistical overview. Aged care statistics series no. 35. Cat. no. AGE 66. Canberra, Australia.
- 3222.0- Population Projections, Australia, 2006-2101 (2008) Australian Bureau of Statistics Australia, ABS, Canberra, Australia.
- Arendts G, Dickson C, Howard K, Quine S (2012) Transfer from residential aged care to emergency departments: an analysis of patient outcomes. Intern Med J 42: 75-82.
- Arendts G, Howard K (2010) The interface between residential aged care and the emergency department: a systematic review. Age Ageing 39: 306-312.
- Reymond L, Israel FJ, Charles MA (2011) A residential aged care end-of-life care pathway (RAC EoLCP) for Australian aged care facilities. Aust Health Rev 35: 350-356.
- Morrison RS, Meier DE (2004) Clinical practice. Palliative care. N Engl J Med 350: 2582-2590.
- Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, et al. (2008) Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 168: 1783-1790.
- National Health and Medical Research Council (2006) Guidelines for a palliative approach in residential aged care, Canberra, Australia.
- Hearn J, Higginson IJ (1998) Do specialist palliative care teams improve outcomes for cancer patients? A systematic literature review. Palliat Med 12: 317-332.
- Melvin CS, Oldham L (2009) When to refer patients to palliative care: Triggers, traps, and timely referrals. J Hosp Palliat Nurs 11: 291-301.
- Bestall JC, Ahmed N, Ahmedzai SH, Payne SA, Noble B, et al. (2004) Access and referral to specialist palliative care: patients’ and professionals’ experiences. Int J Palliat Nurs 10: 381-389.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 6562
- [From(publication date):
September-2012 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 2028
- PDF downloads : 4534