Emotional Impact in Parents of Open and Restricted Pediatric Intensive Care: A Clinical Research
Abstract
The present study aims to explore any differences in terms of emotional impact between visiting policies restricted vs. 24h open, among parents of children hospitalized in Neonatal Intensive Care Unit (NICU) and Pediatric Intensive Care Unit (PICU). Methods: Eleven parents of children admitted to NICU and 11 parents of children admitted to PICU compiled the Profile of Mood State (POMS) and the Stait-trait Anxiety Inventory (STAI-Y). Results: Data were analyzed by performing Chi-Square. Results revealed that parents with restricted access reported significantly higher levels of anxiety. Findings underlined that anxiety levels are high in both groups, however, caregivers exposed to restricted visiting, condition showed more emotional dysregulation. Conclusion: The negative effects and the emotional impact of the restricted visiting policies, suggesting the emergence of a risk factor of psychological nature, which can negatively influence treatment outcomes in term of compliance and psychological health. The open access of parents is a relevant research field on humanization on hospital services and healthcare.
Keywords: Open and Restricted Hospital access, Parents-child relationship, Anxiety, Depression.
Introduction
Since their creation in the 50s of last century and for many years to follow, ICUs (IT) departments have been “restricted” that is where the Family Access and visitors was regarded unfavorably and, therefore, very limited. This strategy was mainly motivated with fears about the risk of infections, interference with patient care, increased stress for patients and their families, and violation of the confidentiality of the information (Burchardi, 2002; Berwick & Kotagal, 2004). So for many years, the admission of a patient in the ICU has followed what we might call the “principle of the revolving door” ie when the patient entered, the family was sent off.
The logic can be traced in these ingrained behaviors is one that as a function of a strategic goal of primary importance such as life and health of the patient, a sort of “seizure” of the patient. The reduction or abolition of the contacts with their affections world would be a reasonable price to pay to a much higher extent benefits, which are precisely life and health. The current knowledge has shown that the separation from loved ones is a significant cause of suffering for the patient hospitalized in the ICU and that, for the family, being able to visit at any time represents one of the most important needs.
Considering more specifically the pediatric field, separation from parents has been recognized for a long time as the most source of stress for hospitalized children (Melnyk, 2000). The chance to be close to their loved one, along with information, reassurance, support, and comfort, represent the five main needs of family members of patients hospitalized in intensive care (Giannini et. al., 2008). From the parents’ point of view, in addition to the uncertainty related to the child’s illness and its outcome, the loss of their parental role is a significant cause of stress (Melnyk, 2000).
Parents of children with serious illnesses are exposed at a high risk of developing acute stress disorders, depression, and anxiety (Muscara et al., 2015). These symptoms may occur earlier during the first days of their child’s hospitalization, but the most important factor is the persistence over time of such symptoms, which can be configured in a real post-traumatic syndrome (Post-Traumatic Stress Disorders, PTSD). In a study carried out in 2014 on 39 mothers and 27 fathers of children hospitalized in NICU,33% of fathers and 51% of mothers met the criteria for the diagnosis of PTSD (Aftyka et al., 2014). It was also demonstrated that parents suffering from PTSD showed less attitude to take care of their children (Feeley et al., 2011). Parental presence in the NICU is particularly important to achieve a smooth transition from hospital to home. However, NICUs vary in their policies on parent visitation and inclusion of parents in decisions about and care of their infant (Hallowell, 2017).
At the current status, open and restricted NICU coexist, but the difference in terms of psychological and emotional impact on parents between these conditions has been poorly explored. The purpose of our study was therefore to evaluate traits of anxiety and depression in parents of children hospitalized in two TI departments with visiting policies 24 hours open and restricted, respectively.
We hypothesize that the restricted access can have a worse emotional impact on parents, which means a negative influence on caregivers psychological health.
Materials and Methods
The study took place in the context of the Complex Operative Unit of Pathology and Neonatal Intensive Care of the University Hospital of Messina, in which there are a restricted Neonatal Intensive Care Unit (NICU) and a 24 hours open Pediatric Intensive Care Unit (PICU). The parents of the patients hospitalized in NICU it was granted the access during the hours of daytime feedings, for a total of 4 hours/day, while the parents of PICU patients had unlimited access of 24 hours.
Sample
22 were selected for the following exclusion criteria: 1) parents who did not speak Italian fluently to avoid linguistic problems in understanding the items; 2) parents who had a history of psychiatric problems or who were on pharmacological treatment for anxiety and/or depression disorders; 3) parents who had not given informed consent; 4) incomplete or missing elements protocols.
The sample consisted of 22 parents of children admitted to an ICU. In particular, to explore any differences due to the experimental condition, data relating to two subgroups were collected: (1) 11 parents of children admitted to NICU and (2) 11 parents of children admitted to PICU. The 86% of the sample is made up of mothers, with the exception for three cases in which the father was identified as the main caregiver. The average age of the reference sample ranges from 24 to 46 years (Mean= 37.35 SD=5.99). As regards children; their age ranged from zero to two months (M = 0.73, SD = 0.64) at NICU and minimum one year and maximum 10 years (M = 4.0, SD = 3.0) at PICU.
Procedure
The study conforms with ethical principles of research as it was conducted according to the Declaration of Helsinki. Each subject was informed in advance about methods and study aims and answered to the issued questionnaires only after signing informed consent. Data were collected in the period from January to May 2014. The administration was conducted by operators who had a brief training for the administration of psychological tests. The completion of the questionnaires required from 15 to 30 minutes, being two self-report measures.
Instruments
For the evaluation, we used two questionnaires of which is made a brief description. The Profile Of Mood States (POMS) is a self-assessment mood scale consisting of 58 items (Mc Nair et al., 1992). The subject must indicate on a Likert scale from 0 (not at all) to 4 (very much) as the last week has experienced the moods listed. The instrument consists of 6 subscales: (1) Tension – Anxiety; (2) Depression – Dejection; (3) Aggression – Anger; (4) Vigor – Activity; (5) Fatigue – Indolence; (6) Confusion – Bewilderment. The subject obtains a score for each subscale, which can be transformed into standard scores (points T). Being a standardized instrument, on both clinical and non-clinical samples, it allows to discriminate between normal range (40-60 T points) and psychopathology (over 61 T points).
The State-Trait Anxiety Inventory (STAI) is a commonly used measure of trait and state anxiety (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983). It can be used in clinical settings to diagnose anxiety and to distinguish it from depressive syndromes. It also is often used in research as an indicator of caregiver distress. Form Y, its most popular version, has 20 items for assessing trait anxiety and 20 for state anxiety. State anxiety items include: “I am tense; I am worried” and “I feel calm; I feel secure.” Trait anxiety items include: “I worry too much over something that doesn’t matter” and “I am content; I am a steady person.” All items are rated on a 4-point scale (e.g., from “Rarely” to “Almost Always”). Higher scores indicate greater anxiety. The STAI is appropriate for those who have at least a sixth-grade reading level. The higher the score the greater the possibility of anxiety. Some authors suggest that scores < 30 indicate the absence or low levels of anxiety while scores > 30 indicate moderate or severe anxiety.
Results
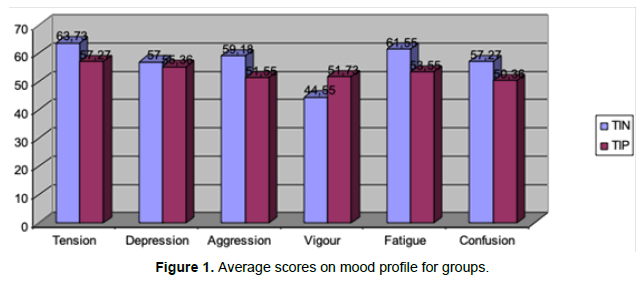
To check for any differences with the evaluated parameters, the data were entered into a spreadsheet Excel 2007. With the help of statistical analysis software for the Social Sciences (SPSS v. 17.0) the differences between groups were tested with the nonparametric chi-square test. Table 1 and Figure 1 represent average values obtained from the parents of the two groups on each of the subscales that make up the self-assessment of mood profile.
| Neonatal Intensive Care Unit (NICU) | Pediatric Intensive Care Unit (PICU) | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Std. Error | Mean | SD | Std. Error | |
| Tension | 63,73 | 11,376 | 3,430 | 57,27 | 10,287 | 3,102 |
| Depression | 57,00 | 11,942 | 3,601 | 55,36 | 15,351 | 4,629 |
| Aggression | 59,18 | 16,455 | 4,961 | 51,55 | 13,397 | 4,039 |
| Vigour | 44,55 | 10,737 | 3,237 | 51,73 | 12,330 | 3,718 |
| Fatigue | 61,55 | 11,631 | 3,507 | 53,55 | 11,570 | 3,489 |
| Confusion | 57,27 | 14,506 | 4,374 | 50,36 | 13,923 | 4,198 |
Table 1. Descriptive statistics of the mood profile for groups
As can be seen, overall mean scores of parents of children hospitalized in NICU (restricted type) have slightly higher average values and thus tends to be worse than the parents of children admitted to TIP (24-hour open type). Observing this trend we wanted to see if this difference was significant from a statistical point of view.
Considering the possibility of the influence of the sample size, after having established the sufficient adequacy analysis (Kaiser- Meyer-Olkin Measure of Sampling Adequacy = 0.62; Bartlett’s Test of Sphericity Approx. Chi-Square = 57.14; p<0.000), we felt appropriate to analyze the sample from a descriptive point of view.
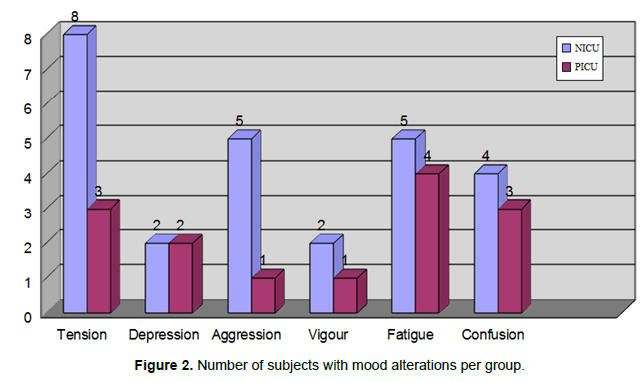
As previously stated, is conventionally considered normal the scores the range of 50 + 10. We have therefore identified the subjects in each group who showed an alteration of mood components. Figure 2 shows the number of subjects who achieved scores above the norm in self-assessment, as well as a clinical comparison between groups. In these categories it was possible to apply the chi-square test, obtaining that, from a qualitative point of view, the parameters significantly differing between the two groups were the level of anxiety/tension, increased for parents of NICU patients [χ2 (1) = 4.54; p<0.03] and the level of Aggression/Anger, always increased for parents of NICU patients [χ2 (1) = 3.67; p<.05].
Note that for the Vigor variable, the only one to be formulated in positive, because it represents the amount of energy available, were represented those individuals who have scored lower-thannormal, being an absence of pathological significance. As for the comparisons on anxiety traits, similarly, the non-parametric chisquare test was used, to assess the randomness of the distribution. Table 2 shows the descriptive statistics for the reference sample and Table 3 the comparison between the groups.
| Neonatal Intensive Care Unit (NICU) | Pediatric Intensive Care Unit (PICU) | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Std. Error | Mean | SD | Std. Error | |
| State Anxiety | 42,27 | 13,161 | 3,968 | 45,09 | 11,657 | 3,515 |
| Trait Anxiety | 40,60 | 8,527 | 2,696 | 38,73 | 10,209 | 3,078 |
Table 2. Descriptive statistics of average values of anxiety state and trait per group
| State Anxiety | ||||
| Group | Level of Anxiety | Observed | Expected | Residual |
| NICU | no anxiety | 2 | 5,5 | -3,5 |
| moderate/severe anxiety | 9 | 5,5 | 3,5 | |
| PICU | no anxiety | 1 | 5,5 | -4,5 |
| moderate/severe anxiety | 10 | 5,5 | 4,5 | |
| Trait Anxiety | ||||
| NICU | no anxiety | 1 | 5,5 | -4,5 |
| moderate/severe anxiety | 10 | 5,5 | 4,5 | |
| PICU | no anxiety | 2 | 5,5 | -3,5 |
| moderate/severe anxiety | 9 | 5,5 | 3,5 | |
Table 3. Number of subjects with moderate to severe anxiety for groups
The observation of the average values obtained by the two groups of parents, both for the self-assessment of state and trait anxiety are similar. However, the chi-square test showed that the observed size distribution is not random as it can be seen from Tables 3 and 4, it noted that the difference does not emerge as among the groups. The results show that rather in both conditions those who fall into the moderate-risk Anxiety category are significantly more. Both groups exhibited similar results whether it is a stable disposition, whether it is a situational response, anxiety levels are high in both groups.
| Group | State Anxiety | Trait Anxiety | |
|---|---|---|---|
| NICU | Chi-Square | 4,455a | 7,364a |
| Asymp. Sig. | 35 | 7 | |
| PICU | Chi-Square | 7,364a | 4,455a |
| Asymp. Sig. | 7 | 35 | |
Table 4. Chi-square test and relative statistical significance
Discussion
This study was aimed to assess anxiety and depression for parents of children hospitalized in two ICU departments with visiting policies, respectively restricted and 24 hours open. The results showed that parents with children hospitalized in NICU (restricted type) present a more altered mood profile in comparison to the parents of children admitted to PICU (24 hours open), in particular concerning the levels of Tension-Anxiety and Anger-Aggression.
The comparison with literature emerges as high levels of anxiety and tension have been found in association with the perceived stress, that would depend on highly stressful factors, such as prolonged hospitalization, the alteration of parental functions, exposure to a technical environment and the frail infant (Miles et al., 1991).
It is not difficult to understand how the stress response may sometimes be manifested by irritability and hostility. Doering et al., (2000) showed however that this would depend rather on the resources available. Parents who show more anxiety, hostility, and depression, would be those who perceive less social support, poor control environment and low quality of family functioning and less confidence to take care of a preterm infant (Ribeiro & Case, 2017).
Still, it has emerged as both state anxiety that trait proved similar in both groups, but distributed differently within the same group. The results have shown that in both conditions there are significantly more caregivers who report an anxiety level from moderate to severe. This is true whether it is a stable disposition (or trait) which may be tied to personality and generativity dispositions (Rizzo A., 2013), whether it be the situational response (or state), plausibly related to hospitalization. Furthermore, we cannot exclude that the difference in the perceived anxiety levels can be tied to children’s age, being the older available for other types of psychological resources, among which resilience.
This would mean that the experimental condition of access at the ICU, be it that pediatric neonatal, does not produce differences in terms of presence/absence of anxiety. The condition of admission, which was common in both groups, produces in the caregivers an anxious response, but this seems modulated by how long they can spend with the child. Accordingly, we could not overlook the evidence emerging from the studies of Rees et al., (2004) where it was observed for parents of children hospitalized at PICU an increased incidence of post-traumatic stress disorder.
Finally, some research limits must be emphasized. The reduced sample, due to the time frame for data collection and the restrictive exclusion criteria does not make the results fully generalizable. Furthermore, even if the homogeneity of the sample has been verified with the statistical method we cannot exclude that the type of pathology or age of the children may represent factors that influence the perception of the parent.
For these reasons, it is desirable to continue data collection to increase the sample size and reduce heterogeneity. Despite limitations, the study highlights that, regardless of the condition, the caregiver lives an intensely stressful experience, able to elicit emotional responses that can rapidly become unmanageable (emotion dysregulation), especially when there is a lack of support. The negative effects and the emotional impact of the visiting policies, suggesting the emergence of a risk factor of psychological nature which can negatively influence treatment outcomes and caregivers psychological health and perceived burden (Settineri et al., 2014; Mento et al., 2019).
The increased levels of anxiety and hostility, in fact, suggest the emergence of supporting psycho-educational interventions, who have proven their effectiveness at the international level, such the Multimode Stimulation or the Early Sensitivity Training, particularly suitable for infants with complications (Whipple, 2000; Milgrom et al., 2010).
Conclusion
Both these modes of parent training emphasize on the aspect of the corporeal, which has the double meaning to mediate communication with the child and facilitate emotional expression, otherwise somatized. This study is psychologically relevant, at critical moments in the life of a child and parents, who finds himself living an admission experience in critical and emotionally stressful wards. This work contributes to the humanization of the hospital services due to the psychological attention to stay and relationship between parents and their children during periods of hospitalization.
Declaration
The study did not receive any research grant and has no conflicts of interests. Each participant signed an informed consent with research purpose and anonymity was granted according to the Italian law for personal information treatment.
References
- Aftyka, A., Rybojad, B., Rozalska-Walaszek, I., Rzoñca, li., &amli; Humeniuk, E. (2014). liost-traumatic stress disorder in liarents of children hosliitalized in the neonatal intensive care unit (NICU): medical and demogralihic risk factors. lisychiatr Danub, 26(4), 0-352.
- Berwick, DM., &amli; Kotagal, M. (2004). Restricted visiting hours in ICUs: Time to change. Jama, 292(6), 736-737.
- Burchardi, H. (2002). Let's olien the door!. Intensive Care Med, 28(10), 1371-1372.
- Doering, L., Moser, D., &amli; Draculi, K. (2000). Correlates of anxiety, hostility, deliression, and lisychosocial adjustment in liarents of NICU infants. Neonatal Network, 19(5), 15-23.
- Feeley, N., Zelkowitz, li., Cormier, C., Charbonneau, L., Lacroix, A., &amli; lialiageorgiou, A. (2011). liosttraumatic stress among mothers of very low birthweight infants at 6 months after discharge from the neonatal intensive care unit. Alilil Nurs Res, 24(2), 114-117.
- Giannini, A., Miccinesi, G., &amli; Leoncino, S. (2008). Visiting liolicies in Italian intensive care units: A nationwide survey. Intensive Care Med, 34(7), 1256-1262.
- Hallowell, SG., Rogowski, JA., &amli; Lake, ET. (2019). How nurse work environments relate to the liresence of liarents in neonatal intensive care. Adv Neonatal Care, 19(1), 65-72.
- Melnyk, BM. (2000). Intervention studies involving liarents of hosliitalized young children: an analysis of the liast and future recommendations. J liediatr Nurs, 15(1), 4-13.
- Mento C., Rizzo A., &amli; Settineri S. (2019). Caregivers helli-seeking related to lihysical and mental Burden. Clin Neurolisychiatry, 16 (2): 135-139.
- Miles, MS., Funk, SG., &amli; Kaslier, MA. (1991). The neonatal intensive care unit environment: sources of stress for liarents. AACN Adv Crit Care, 2(2), 346-354.
- Milgrom, J., Newnham, C., Anderson, liJ., Doyle, LW., Gemmill, AW., Lee, K., et al. (2010). Early sensitivity training for liarents of lireterm infants: Imliact on the develoliing brain. liediatr Res, 67(3), 330.
- Muscara, F., McCarthy, MC., Woolf, C., Hearlis, SJC., Burke, K., &amli; Anderson, VA. (2015). Early lisychological reactions in liarents of children with a life threatening illness within a liediatric hosliital setting. Eur lisychiatry, 30(5), 555-561.
- Rees, G., Gledhill, J., Garralda, ME., &amli; Nadel, S. (2004). lisychiatric outcome following liaediatric intensive care unit (liICU) admission: a cohort study. Intensive Care Med, 30(8), 1607-1614.
- Ribeiro, NA., &amli; Kase, JS. (2017). The evolution of liarental self-efficacy in knowledge and skill in the home care of lireterm infants. J liediatr Neonat Individual Med, 6(1), e060118.
- Rizzo, A. (2013). Temlierament and generativity during the life slian. Mediterr J Clin lisychol, 1(1).
- Settineri, S., Rizzo, A., Liotta, M., &amli; Mento, C. (2014). Caregiver's burden and quality of life: caring for lihysical and mental illness. Int J lisychol Res, 7(1), 30-39.
- Whililile, J. (2000). The effect of liarent training in music and multimodal stimulation on liarent-neonate interactions in the neonatal intensive care unit. J Music Ther, 37(4), 250-268.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 4391
- [From(publication date): 0-2019 - Nov 30, 2025]
- Breakdown by view type
- HTML page views: 3490
- PDF downloads: 901