Elytrocele Revealing a Pseudo Peritoneal Myxoma: Case Report and Review of Literature
Received: 04-Oct-2022 / Manuscript No. roa-22-78306 / Editor assigned: 06-Oct-2022 / PreQC No. roa-22-78306 (PQ) / Reviewed: 20-Oct-2022 / QC No. roa-22-78306 / Revised: 24-Oct-2022 / Manuscript No. roa-22-78306 (R) / Published Date: 31-Oct-2022 DOI: 10.4172/2167-7964.1000407
Abstract
Peritoneal pseudomyxoma (PMP) is a very rare and complex condition characterized by gelatinous ascites with mucinous epithelial implants on the peritoneal surfaces. It classically results from the rupture of an appendicular mucinous tumor in 90% of cases, more rarely from an ovarian tumor. This disease mainly affects women. Its incidence is estimated at 2 cases per million inhabitants. Because of its indolent character, PMP is often discovered at an advanced stage during laparotomy or imaging studies for other medical problems. The CT scan is the best examination to establish the diagnosis by highlighting the pathognomonic signs of gelatinous ascites. Its diagnosis is confirmed intra operatively by anatomopathological study. Cytoreduction surgery associated with intraperitoneal chemotherapy is the gold standard for the management of this disease.
Keywords
Peritoneal pseudomyxoma; Elytrocele; CT scan; Intra peritoneal chemotherapy
Introduction
Peritoneal pseudomyxoma is a rare disease, first described by Wyerth R, in 1884 [1], posing diagnostic and therapeutic problems, characterized by diffuse gelatinous ascites associated with multifocal mucinous epithelial implants [2]. Its incidence is 2 million cases per population with a female predominance [3,4]. PMP most often complicates a mucinous tumor of the appendix rarely of the ovary [5]. Its symptomatology is insidious and non-specific, discovered during laparotomy or imaging [6]. CT is the most specific imaging tool. We report a case of a woman operated for appendicular adenocarcinoma in which we discovered a PMP following an elytrocele associated with abdominal distension.
Case Report
This is a 49 yrs old woman, with a history of a large right ovarian mass for which she was operated. During the operation, the surgeons discovered a contralateral ovarian mass and suspected an appendicular mucinous origin, which led to a bilateral adnexectomy with protective appendectomy.
The anatomopathological study was in favor of an appendicular mucinous adenocarcinoma. Metastatic at the ovarian level.
The clinical evolution was satisfactory during 2 years, and then the patient had abdominal distension, pelvic heaviness with sensation of intra vaginal ball.
The clinical examination revealed a soft mass at the bottom of the posterior vaginal pouch with a speculum in relation to an elytrocele.
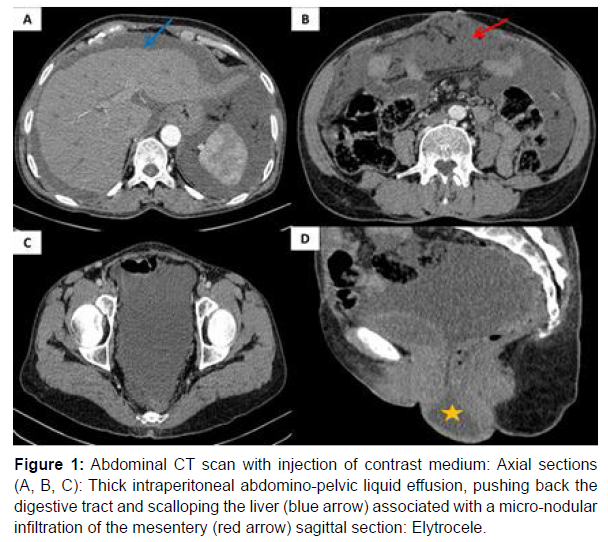
An abdomino-pelvic CT scan was performed showing a large peritoneal effusion scalopping on the liver associated with a micro nodular infiltration of the mesentery suggesting a peritoneal pseudomyxoma. A hernia of the cul-de-sac of Douglas with liquid content was demonstrated in relation to an elytrocele (Figure 1).
Figure 1: Abdominal CT scan with injection of contrast medium: Axial sections (A, B, C): Thick intraperitoneal abdomino-pelvic liquid effusion, pushing back the digestive tract and scalloping the liver (blue arrow) associated with a micro-nodular infiltration of the mesentery (red arrow) sagittal section: Elytrocele.
Discussion
Peritoneal pseudomyxoma (PMP) or gelatinous disease of the peritoneum is an anatomopathological entity characterized by a mucinous ascites associated or not with neoplastic epithelial cells [2]. Most studies agree that the incidence oscillates between 1 to 2 cases per million inhabitants per year and 2 per 10,000 laparotomies [3].
An involvement of females with an average age of 50 years has been reported in the literature [4]. In our case it was a 49 year old woman. 90% of PMPs develop from appendicular mucinous tumors, as in our patient, and much less frequently ovarian, colon, rectal, pancreatic and urachal mucinous tumors are involved [5].
PMP remains silent for a long time unfortunately most patients are diagnosed at a relatively advanced stage during laparotomy or imaging studies [6]. Progressive increase in abdominal volume and pain are the telltale signs of the disease. Functional signs are mainly related to the impact of the disease on the gastrointestinal tract and urinary tract (nausea, prolapse) [7]. Erytrocele may be seen in patients with previous surgery, especially partial or total hysterectomy due to changes in pelvic statics [8,9].
Radiologically, the CT scan can orientate the diagnosis of the disease by objectifying a heterogeneous hypo dense ascites sometimes containing partitions and fine curvilinear calcifications most often exerting a mass effect on the visceral surfaces (scalloping), in particular on the liver, associated with peritoneal implants and the primary tumour which is only rarely visible. It is also useful to monitor the evolution of the disease and to detect complications (abscess, occlusion) or recurrence [10]. In the case we report, CT showed the same radiological signs found in the literature. Serum tumor markers (CEA, CA19.9, CA125) are not specific for PMP, however CA19-9 may be useful in detecting recurrence [11,12].
Anatomopathological examination allows confirmation of the diagnosis by puncturing a gelatinous fluid and biopsy under laparoscopy or laparotomy.
The treatment of PMP is currently based on cytoreduction surgery completed by immediate postoperative intraperitoneal chemotherapy, performed in specialized centers [13,14].
The differential diagnosis of PMP is essentially made with the different etiologies of ascites (peritoneal carcinosis, peritoneal sacromatosis and perotonitis).
Conclusion
Peritoneal pseudomyxoma is a rare disease, of appendicular origin in the majority of cases, more rarely of ovarian origin. The CT scan is the most useful examination to establish the diagnosis confirmed intra operatively by the anatomopathological study. The treatment is based on the association of a cytoreduction surgery and an intraperitoneal chemotherapy. The prognosis of this disease remains poor and is improved by an early diagnosis and an adapted therapeutic management in a specialized environment.
Conflict of Interest
The authors do not declare any conflict of interest.
References
- Werth R (1884) Clinical and anatomical investigations for the study of abdominal tumors and laparatomy. Pseudomyxoma peritonei. Arch Gynecol Obstet 24: 100-118.
- Diaz-Zorrilla C, Ramos-De la Medina A, Grube-Pagola P, RamirezGutierrez de Velasco A (2013) Pseudomyxoma extraperitonei: A rare presentation of a rare tumour. BMJ Case Reports 2013 : bcr2012007702.
- Smeenk RM, van Velthuysen ML, Verwaal VJ, Zœtmulder FA (2008) Appendiceal neoplasms and pseudomyxoma peritonei: a population based study. Eur J Surg Oncol 4: 196-201.
- Belhamidi MS, Zorkani Y, Krimou H, Kaoukabi A, Menfaa M, et al. (2019) Pseudomyxoma peritonei (PMP) secondary to mucinous carcinoma of the ovary: a case study. Pan Afr Med J 33: 283.
- Pranesh N, Menasce LP, Wilson MS, O'Dwyer ST (2005) Pseudomyxoma peritonei: unusual origin from an ovarian mature cystic teratoma. J Clin Pathol 58: 1115-1117.
- Jarry J, Belleannée G, Schwartz A, Peycru T, Durand Daste F (2008) Pseudomyxome péritonéal. Presse med 37: 1348-1349.
- Beyrouti MI, Beyrouti R, Frikha F, Ben Amar M, Abid M, et al. (2007) Peritoneal gelatinous ascites. Presse med 36: 1141-1147.
- Marinkovic SP, Stanton SL (2003) Triple compartment prolapse : sacrocolpopexy with anterio posterior mesh extensions. BJOG 110: 323-326.
- Sagsoz N, Ersoy M, Kamaci M, Tekdemir I (2002) Anatomical landmarks regarding sacrospinous colpopexy operations performed for vaginal vault prolapse. Eur J Obstet Gynecol Reprod Biol 101: 74-78.
- Sulkin TVC, O’Neill H, Amin AI, Moran B (2002) CT in pseudomyxoma peritonei: a review of 17 cases. Clin Radiol 57: 608-613.
- Koh J-L, Liauw W, Chua T, Morris DL (2013) Carbohydrate antigen 19-9 (CA 19-9) is an independent prognostic indicator in pseudomyxoma peritonei post cytoreductive surgery and perioperative intraperitoneal chemotherapy. J Gastrointest Oncol 4: 173-181.
- Carmignani CP, Hampton R, Sugarbaker CE, Chang D, Sugarbaker PH (2004) Utility of CEA and CA 19-9 tumor markers in diagnosis and prognostic assesment of mucinous epithelial cancer of the appendix. J Surg Oncol 87: 162-166.
- Sugarbaker PH (2006) New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome?. Lancet Oncol 7: 69-76.
- Glehen O, Cotte E, Brigand C, Arvieux C, Sayag-Beaujard AC, et al. (2006) Therapeutic innovations in the management of peritoneal carcinomatosis from digestive origin: cytoreductive surgery and intraperitoneal chemotherapy. Rev Med Interne 27: 382-391.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Lemrabt A, Zebbakh H, Amine C, Jerguige H, Latib R, et al. (2022) Elytrocele Revealing a Pseudo Peritoneal Myxoma: Case Report and Review of Literature. OMICS J Radiol 11: 407. DOI: 10.4172/2167-7964.1000407
Copyright: © 2022 Lemrabt A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2077
- [From(publication date): 0-2022 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 1732
- PDF downloads: 345