Review Article Open Access
The Electronic Hospital Information System Implemented at the District General Hospital Trincomalee-An Experience of Business Process Reengineering
Ayanthi Saranga Jayawardena*Regional Director of Health Services Office, Kalutara, Sri Lanka
- *Corresponding Author:
- Ayanthi Saranga Jayawardena
Regional Director of Health Services Office
Kalutara, Sri Lanka
Tel: 0345614136
E-mail: jayawardenaayanthi@ymail.com
Received date: February 04, 2014; Accepted date: March 12, 2014; Published date: March 14, 2014
Citation: Jayawardena AS (2014) The Electronic Hospital Information System Implemented at the District General Hospital Trincomalee-An Experience of Business Process Re-engineering. J Community Med Health Educ S2:001. doi: 10.4172/2161-0711.S2-001
Copyright: © 2014 Jayawardena AS. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
The Epidemiology Unit in Sri Lanka with the collaboration of WHO initiated computer based electronic information system in November 2005 at Base Hospital Ampara and Base Hospital Hambanthota. Then the system was expanded to six other selected hospitals in six districts. None of the systems have been evaluated completely so far. The computerized HIS is successfully functioning at the DGH Trincomalee. Long term objective of the project was to build and maintain a patient database for analysis of data and to facilitate evidence-based decision making process Short term objectives were, to have properly maintained hospital health statistics, to have a paperless hospital information system and to reduce costs and improve the accuracy and timeliness of hospital information system. The patient information system was exceptionally user-friendly and thus was readily accepted by the medical staff at the hospital. This system was password protected. User names and password enable graded access to the system thus confidentiality is maintained. Doctors were able to order investigations, radiological images and prescriptions to the patients online. Radiological images were available online which reduce cost of X-ray films. Patients can get their radiological images copied to a CD thus missing of reports or duplicating of reports will not be a problem here after. They also can do online booking in advance for a date for surgery from the theatre. Hospital records are maintained by the out-patient module. This system was readily accepted by the patients too. It is important to maintain this system with future amendments as required in order to meet future demands and challenges.
Keywords
Electronic hospital information system; Multi disease surveillance; Outpatient department; Business process re-engineering
Abbreviations
BH: Base Hospital; CD: Compact Disc; BHT: Bed Head Tickets; DGH: District General Hospital; EHIS: Electronic Hospital Information System; HIS: Health Information System; HMIS: Health Management Information System; IMMR: Indoor Morbidity Mortality Returns; IV/IM: Intra Venous/Intra Muscular; MDGs: Millennium Development Goals; MDS: Multi Disease Surveillance; MLT: Medical Laboratory Technician; MO: Medical Officer; MS: Medical Superintendent; NIC: National Identity Card; OPD: Out Patient’s Department; PID: Patient Identification; TH: Teaching Hospital; WHO: World Health Organization
Introduction
A good Health Management Information System (HMIS) is necessary to manage a health organization effectively and efficiently [1]. HMIS is the key factor for an effective decision making process. A Hospital Information System (HIS) is a comprehensive, integrated information system designed to manage the administrative, financial and clinical aspects of a hospital. This includes paper-based information processing as well as data processing by using machines [2,3]. Hospital information systems may contribute in different ways to quality assurance activities such as assessing the quality of primary care, monitoring quality indicators, supporting clinical care evaluation studies, and auditing concurrently the ongoing process of care using reminders or decision support techniques [3].
The World Health Organization (WHO) is specifically concerned with helping countries to improve their hospital statistics. WHO has realized that the health information in most countries is not up to standard [4]. There are many shortcomings in health information system in our country. Electronic Hospital Information Systems (EHIS) will improve the hospital statistics with less errors and will be accurate and easy to generate so it can be created in time to improve statistics and public health information. WHO has decided for Multi Disease Surveillance (MDS) in implementing EHIS in 27 hospitals in the Eastern and the North Central provinces in Sri Lanka. Four software systems were installed by the Ministry of Health at the TH Baticaloa, Ashroff Memorial Hospital Ampara, BH Kalmunai and BH Akkaraipattu [5]. But in all above hospitals these systems are not fully functioning. The Epidemiology Unit in Sri Lanka with the collaboration of WHO initiated computer based electronic information system in November 2005 at Base Hospital Ampara and Base Hospital Hambanthota. Then the system was expanded to six other selected hospitals in six districts. None of the systems have been evaluated completely so far. The computerized HIS is successfully functioning at the DGH Trincomalee [6].
Objectives of the Project
Short term objectives
1. To have properly maintained hospital health statistics
2. To have a paperless hospital information system
3. To reduce costs and improve the accuracy and timeliness of hospital information system
Long term objective
To build and maintain a patient database for analysis of data and to facilitate evidence-based decision making process.
Business Process Re-engineering
Today we are in an ever changing world, where the only thing that does not change is ‘change’ itself. Every customer oriented process is driven by three Cs: Customer, Competition and Change [7]. The two cornerstones of any organization are the people and the processes. Business Process Re-engineering is more fundamental, radical and is the key to transforming how people work [8]. This Re-engineering process had three stages namely pre-implementation, implementation and post implementation. In order to achieve the objectives through computerization of the hospital functions at the District General Hospital Trincomalee, each unit was studied and then radical changes were brought about by re-engineering the processes with the newly set up of computerization. Few examples of re-engineering processes were given in Table 1.
| Process/Result | Benefits |
|---|---|
| 1.Issue a Patient Identification number to patients | Easy tracking of patients at their second visits/No duplication of attendance |
| 2.Record history, examination findings of every patients | Easy retrieval of records |
| 3.Minimize use of sheets to request laboratory investigations | Improve medical officers’ productivity |
| 4.Laboratory test results stored, consolidate in one sheet, print only when necessary | No duplication of test on same patient, reduce patient waiting time, eliminate wastage of stationary |
| 5.Radiological images store in the computer | Easy retrieval of reports, minimize duplication of same film, reduce cost for X-ray filming |
| 6.On-line theatre time booking | Reduce patient waiting time |
| 7.Generation of IMMR, Out patient records, notification record, etc. | Accurate and timeliness of data |
Table 1: Re-engineering processes and their benefits.
Structure and Functions of the System
The computerized hospital information system was implemented at the District General Hospital Trincomalee in August 2008. There was a central computer management unit established within the hospital premises with a system operator. It was a 24- hour functioning unit. The system operator had control of the whole system and can quickly locate where the system has gone wrong. Files were automatically backed up every 4 hours in this unit therefore in a case of total corruption of the database they will miss data for several hours at the most. Fortunately this event is rare and has not happened in this hospital as yet.
The system was installed at the admission counter and in a few wards at first and then introduced step by step to the OPD, the laboratory, other wards, the pharmacy, the theatre and the radiology department. At the OPD a wireless network system was installed while wards, theatre, laboratory, and radiology departments were connected through Ethernet cabling. The software database used in the hospital was called Multi Disease Surveillance System (MDS). This system was a database developed by the HIS project of the Australian Swiss Red Cross in 2006. They introduced the system to hospitals, funded by them from 2006-2009 and the system has undergone several stages of improvements from MDS-1 to MDS-5. It runs under the database system Caché distributed by the Intersystems Corporation. The software using now is MDS-5 which is distributed and maintained by a local company in Sri Lanka.
The District General Hospital Trincomalee has computerized the following sections and functions:
- Admission/Discharges/Transfers
- All OPD functions
- Pathology test results information
- Radiology test results
- Issuing medicines/Stock balancing/Inventory maintenance
- Theatre functions information with appointment scheduling
- Communications with the management/intra department/inter department and with external organizations
The ECG department, CSSD, and the kitchen have not been connected with the system
Changes in the clinical practice
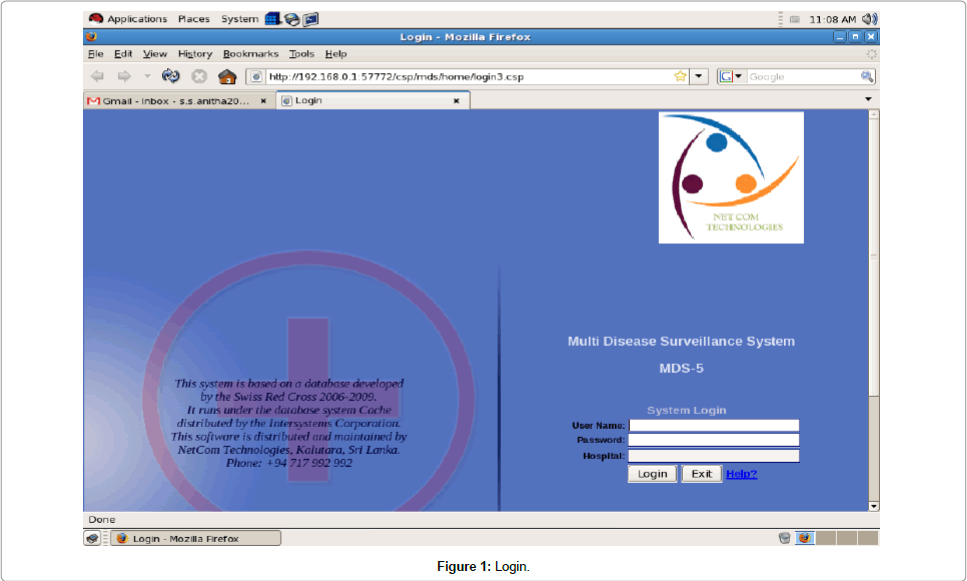
This system was password protected. Each member of the staff of the DGH Trincomalee was given a password to enter into the system (Figure 1) thus having limited and controlled access to this system.
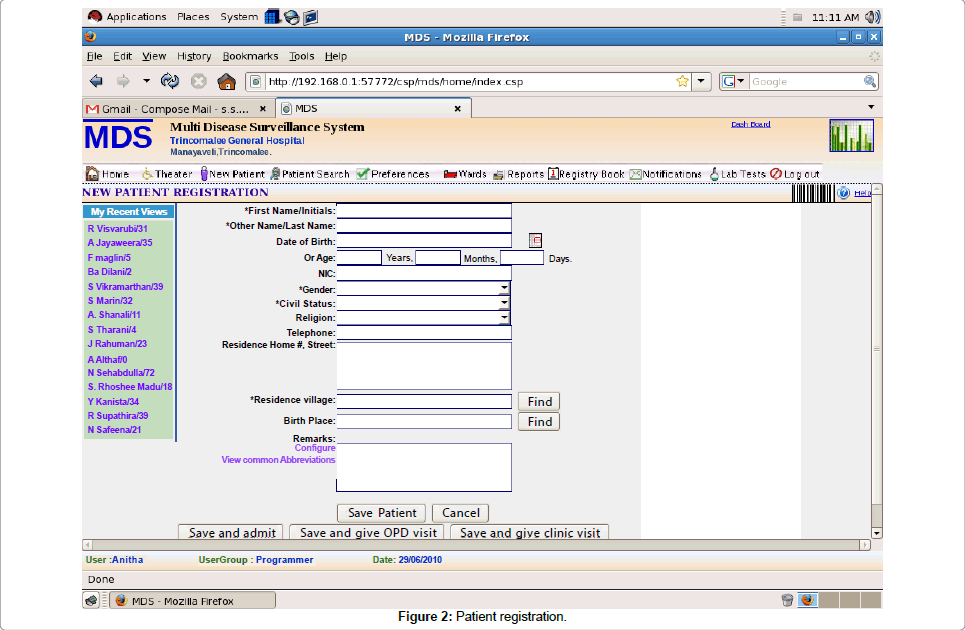
Attendants at the OPD had access only to enter data on the screen given below (Figure 2) which was entering data on patient’s socio demographic status mainly. It is completely a paperless system running at the OPD.
Admission/OPD visit/Clinic visit module: At the OPD, the patient received a small card with a number and came to the OPD registration desk with that card. An attendant entered this number to the computer then the patient identification number was generated automatically. The socio-demographic data of the patient was entered including first name/initials, last name, date of birth, age, NIC number, gender, civil status, religion, telephone no, residence address, residence village and birth place from a database where almost all the villages and districts in Sri Lanka have been covered. After this initial step of registration at the OPD, the hospital PID number was given to the patient. One patient gets only one PID during his lifetime.
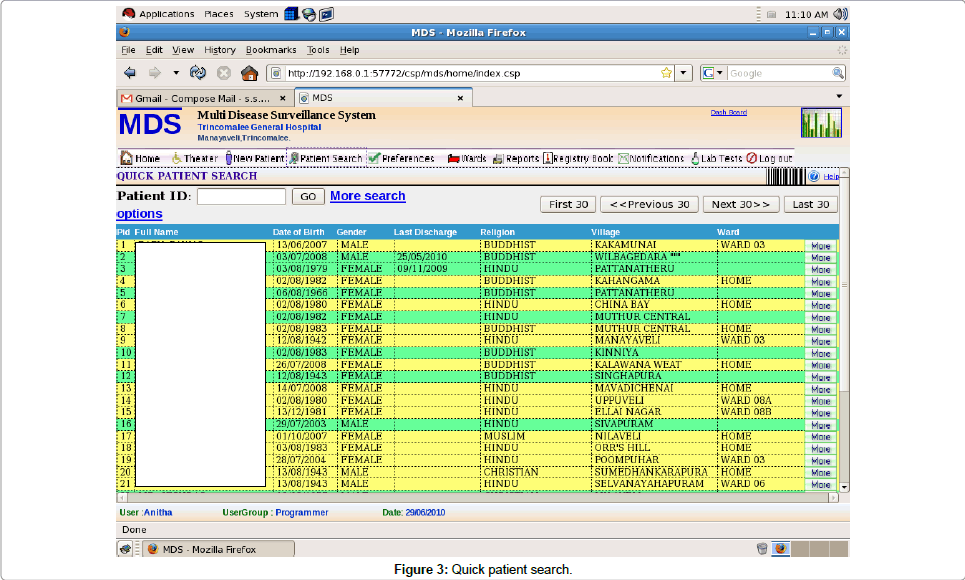
Quick patient search module: Then patient went to a doctor with this patient ID number. Medical officers had full access to the system. Once the doctor entered the Patient ID number, patients’ previous details automatically came to the screen. If by chance a patient lost his/ her ID number, the doctor can go to the quick patient search option, then by entering patient’s name or date of birth or NIC number or the village doctor can trace the Patient ID number (Figure 3). At the same time he/she can trace previous OPD visits, clinic visits, or previous admission records of the same patient on more search options.
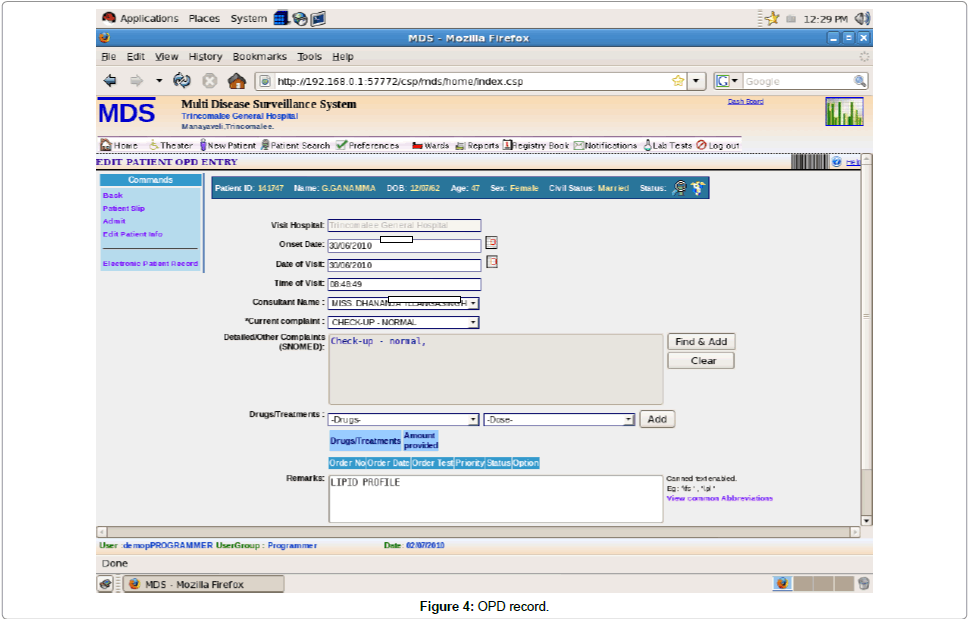
Visit at the doctors counter module: The doctor then entered into the OPD entry module. The screen came up as below (Figure 4).
The onset date of the disease was entered, date of visit also was entered then the time of visit was automatically come to the screen. Then the MO who saw the patient entered his/her name. Patient’s main complaint was selected from complaints list database which was prepared by a two weeks study of the main complaints among patients who came to the OPD. Then detailed history of other complaints and positive examination findings was entered by the doctor. After that the doctor prescribed the medications from the drug list database with the dose and duration, calculated the amount of drugs to be issued and added it to the prescription. The MDS system has generated a medicine database using SNOWMED software database. When doctor entered the name of a drug he/she can verify whether that particular drug was available at the dispensary or out of stock so he/she can write an alternative if the drug was not available. Finally doctor saved the record or can save and get a print out or update the record as an OPD entry or can refer to a relevant clinic or can admit the patient if required.
On the same screen there was a facility for doctors to order laboratory reports if required. The OPD computers were directly connected with the main laboratory. Doctors can give a priority order on requesting laboratory or radiological reports. MO can add individual tests or group tests if required.
Then patient went to the OPD pharmacy with only the patient ID number. At the pharmacy, a pharmacist or a dispenser entered the patient ID number and got into the same screen as screen 4 where the prescription of a relevant patient was highlighting. Then a pharmacist or a dispenser issued drugs according to the prescription and automatically stock balance of a particular drug appeared.
At the same time this system was connected with the injection room. When doctor prescribed an IV/IM injection such as Tetanus toxoid/Hydrocortisone or to nebulize an asthmatic patient at the OPD, patient again went with only the PID number to the injection room. The nurse entered into the system by entering his/her password and entered PID number to get the prescribed treatment procedures for the particular patient. Once she/he has carried out the procedure, it can be entered into the record and updated. At the moment staff maintained a log book and manual record keeping was still proceeding in parallel.
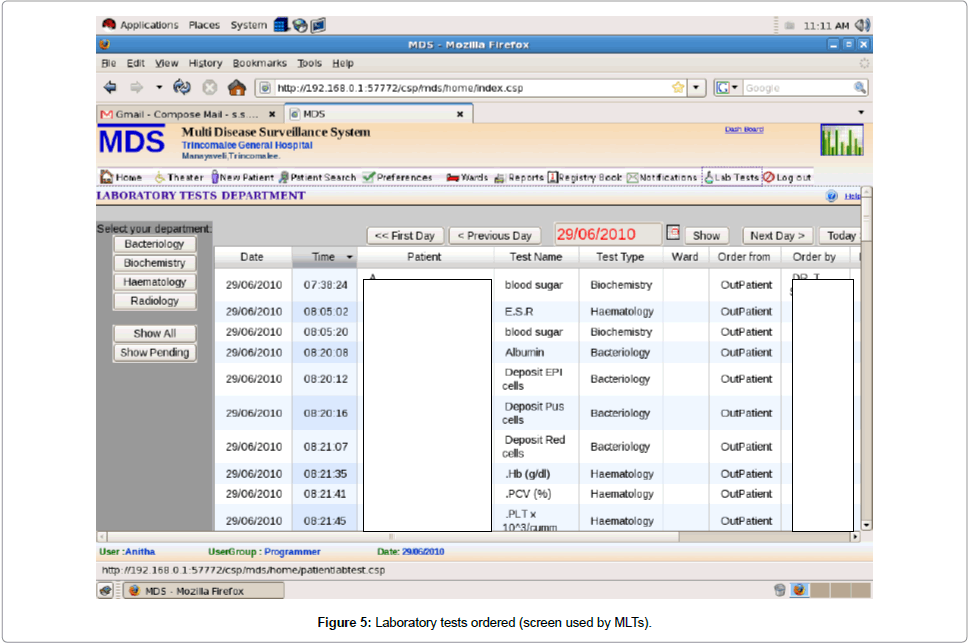
Laboratory test results information module: When a doctor wanted to retrieve an investigation they ordered, they return to the record of the OPD visit and the screen showed whether the test has been carried out or not. It was also possible for the doctors to select the relevant department out of bacteriology, biochemistry,haematology or radiology departments and visualized all the tests recently carried out on the screen used by MLTs. By entering into the relevant laboratory department through the system doctor was able to see the test date and time, patient name, test name, test type, ward/OPD, order from (OPD/ clinic or ward), ordered by (Doctor’s name who ordered the test), priority, status whether test has done or pending and status whether the test was open or in process. Doctors can see the reports by entering “_show all reports”_ or “_show pending reports”_ as required. It was also possible to get the laboratory technician’s name who carried out the reporting. A doctor can order tests and at the same time can see previous laboratory reports done on the same patient. The system therefore prevents duplicating laboratory reports on the same patient (Figure 5).
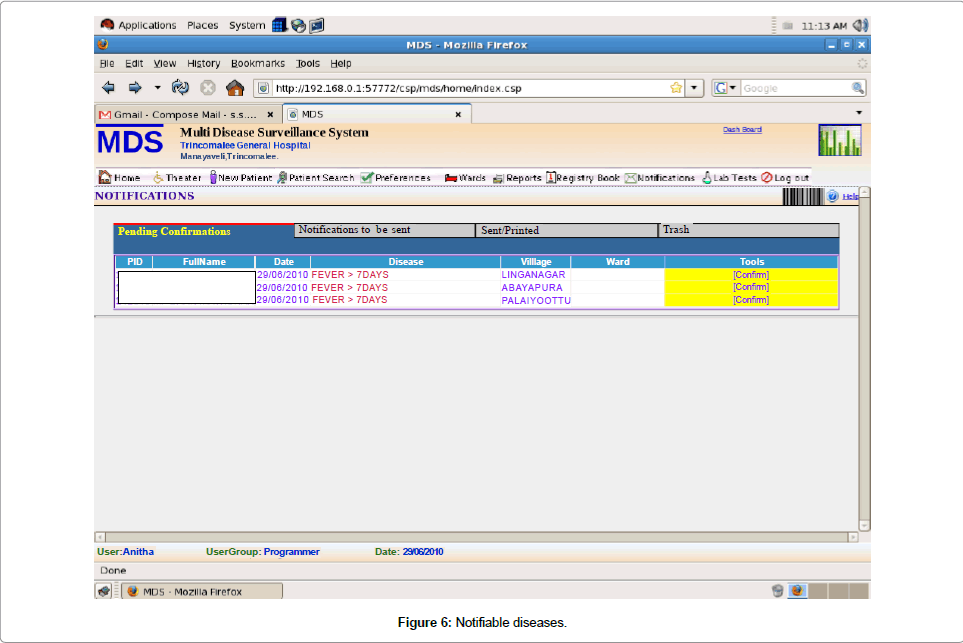
Notification of diseases module: There was a notification system also connected with the OPD service. When a doctor entered in to the notification module he/she can see columns of pending confirmations, notifications to be sent, those sent/printed and those suggested by the computer but discharged. In the pending confirmations column you get PID, patient’s full name, date, disease, village, ward and tools whether confirm or pending (Figure 6).
Hospital statistics module: Hospital records maintained by the out-patient module were the daily OPD patient list, OPD entries, OPD disease morbidity pattern and by the in- patient module were daily midnight report, top 10 diseases at the OPD and wards, hospital performances, daily ward activities, admissions, procedures, notification and daily functions at the laboratory, radiology and theatre. The admissions are also documented in the standard statistical manner used by the Government Statistical Unit (the Indoor Morbidity and Mortality Return). Manual production of this report used to take 3 months for several persons - it is now produced in seconds.
Training of the staff
A training program on using computers and system oriented training was conducted at the initial stage for the staff members for all categories of staff. There were about nearly 500 staff members in all categories of staff but only 100 participated for the first training program. In addition, the Medical Superintendent of the hospital has taken personal interest in training all staff members, one department at a time.
A competent doctor who was familiar with the system can enter details of the patient admission within several minutes. It took longer time for, examination of the patient and doctor can spend more time with patient on examining because he/she can record the findings very quickly. A competent nurse can enter the details within a period of 1-2 minutes. An attendant who was familiar with the system can enter demographic details of a patient with in 40-45 seconds.
Doctors were able to order investigations, radiological images and prescriptions to the patients online. Radiological images were available online which reduce cost of x-ray films. Patients can get their radiological images copied to a CD thus missing of reports will not be a problem here after. They also can do online booking in advance for a date for surgery from the theatre.
The patient information system was exceptionally user-friendly and thus was readily accepted by the medical staff at the hospital. The MS has the full authority regarding the system, has full access to the system and can get all the information about the hospital at once online, and reply promptly to any queries or requests by retrieving information in the system.
Advantages of the System
It is a draw-back of hospital information in Sri Lanka that OPD statistics are not available. This was a great problem during the posttsunami period when thousands of people were treated at the OPD per day but the actual number was not recorded by the authorities and the patient record was not kept, so nobody knows who came to the hospitals for treatment, from where, when and for what conditions. This system provides all the details of OPD statistics as mentioned above, which is the best and major advantage of this system. Other advantages in general are as follows,
• Increased time doctors, nurses spend with patients
• Easy access to information
• Improved quality of documentation
• Improved quality of patient care
• Increased nursing productivity
•Improved communications
• Reduced errors of omission
• Reduced medication errors
• Development of a village map of Sri Lanka in order to easily locate patient residence for notification of diseases
• Development of a common clinical database
• Improved patient’s perception of care
• Enhanced ability to track patient’s record
• Improved hospital image
• Ability to get radiological images online thus reducing the cost of X-ray films
• Prevent duplicating investigations done on a same patient
Advantages of the password protected system,
1. Hospital staff has limited access to the system so they cannot misuse the laboratory reports
2. They cannot enter or alter patient’s complains
3. They cannot misuse prescriptions to the pharmacy
Challenges Faced by the Management of the Hospital
In each stage of re-engineering process there were several steps to be followed and each one of these steps would be a challenge to the management. At the pre-implementation stage changing minds of the staff from traditional to new computerization system was the biggest challenge. At first they did not accept the whole process. Most of them thought that this was an additional work burden for them. They initially thought that this was a fault finding process by the hospital management. The Medical Superintendent (MS) had organized several discussions over and over again for several months to change their minds. Most of them initially did not participate for the training programme and only very few participated. At the implementation stage, getting away from the papers were major challenge because everybody were very much familiar with the papers. From top to bottom of staff members wanted to use papers instead of a computer. Most of the staff members thought it is easy to use paper records than computers. Once they were familiar with the system they accepted the new system and now they work with computers happily. At the post implementation period the MS had a major challenge on finding funds after the Swiss Red Cross handed over the system maintenance after the period of three years to the government.
Quality of Care
Automated entry of patient records, laboratory results and the ability to cross-check reports means that human error is reduced and that clinical problems can be identified more quickly. Automated medication reports and prescriptions improve the safety of drug administration. Multiparty expert consultations can be conducted online, and all the pertinent data are readily accessible by all parties.
Cost Containment
The initial cost for the introduction of the system in the Trincomalee General Hospital with hardware, software and the network system was roughly Rs. 10 million (about $US 80,000). The project implementation was funded by the Australian/Swiss Red Cross from 2006-2009 then handed over to the government. The maintenance cost was roughly around Rs. 0.5 million.
Security and Confidentiality
User names and password enable graded access to the system thus confidentiality is maintained. For protection against unauthorized access to confidential information, these computers do not have modems and this network system function at the hospital has no link with any external networks.
Legal Acceptability
The legal acceptance of an electronic patient record by the Sri Lankan judiciary/courts is still an issue which is not covered by Sri Lankan law. Therefore how much effort is taken to eliminate paper work from hospital information system it is still a requirement to maintain a manual BHT specifically in a case of legal interest.
Discussion and Conclusion
• This cross-sectional study of EHIS at the OPD has contributed to a better understanding of the EHI system at the DGH Trincomalee
• It was observed that the MDS software used in this hospital was very much user friendly and easy to learn. The wireless network system was also successful with less error
• This system was password protected and these passwords enable graded access to the system by different categories of staff. Therefore the system provided confidentiality and security to patient information
• The personal interest showed by the hospital MS, the commitment given by the hospital staff were the most important key factors that made this computerization of hospital health record system successful
• This system was readily accepted by the patients too
• It is important to maintain this system with future amendments as required in order to meet future demands and challenges
Other Information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- DelpierreC, Cuzin L, Fillaux J, Alvarez M, Massip P,et al. (2004) A systematic review of computer-based patient record system and quality care: more randomized clinical trials or a broader approach? Int J QualHealth Care 16: 407-416.
- Lippeveld T, Sauerborn R, Bodart C (2000) Design and implementation of health information systems. World Health Organization, Geneva.
- Littlejohns P, Wyatt JC, Garvican L (2003) Evaluating computerised health information systems: hard lessons still to be learnt. BMJ 326: 860-863.
- Components of a strong health information system: A guide to the HMN Framework. Health Metrics Network, WHO, Geneva.
- Introduction of Multi Disease Surveillance/Health Information System, 2008. Epidemiology Unit, Ministry of Healthcare and Nutrition, Sri Lanka.
- Jayawardena DBAS (2012)Electronic Hospital Information System at the Outpatient Department in District Genetal Hospital Trincomalee. 8th e-India, e-Health Conference, Hyderabad, Andhra Pradesh, India.
- Muthu S, Whitman L (1999)Business Process Re-engineering: A consolidated methodology. 4th Annual International Conference on Industrial engineering theory, applicationand practice,Texas, USA.
- Carter P. (2005) Business Process Re-engineering: An Introductory Guide. Team Technology
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 23647
- [From(publication date):
specialissue-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 18879
- PDF downloads : 4768