Research Article Open Access
Elderly Patients with Painful Bone Metastases. The Impact of Comorbidity on the Choice of Radiation Therapy Regimen
Francesca Maria Giugliano1*, Rossella Di Franco2, Luciano Iadanza3, Valentina Borzillo1, Luisa Cutillo4 and Paolo Muto11Department of Radiation therapy, National Cancer Institute, Pascale Foundation, Naples, Italy
2Department of Radiotherapy, Second university of Naples, Italy
3Medical Physics Department, National Cancer Institute, Pascale Foundation, Naples, Italy, Naples, Italy
4Department of Statistics and Mathematics for the Economic Research, Parthenope University of Naples, Italy
- *Corresponding Author:
- Maria Giugliano
Department of Radiation therapy
National Cancer Institute
Pascale Foundation, Naples, Italy
Tel: 39-081-5903277
E-mail: fm.giugliano@istitutotumori.na.it
Received date: October 29, 2014; Accepted date: November 07, 2014; Published date: November 16, 2014
Citation: Giugliano FM, Franco RD, Iadanza L, Borzillo V, Cutillo L et al. (2014) Elderly Patients with Painful Bone Metastases. The Impact of Comorbidity on the Choice of Radiation Therapy Regimen. J Palliat Care Med 4:199. doi:10.4172/2165-7386.1000199
Copyright: © 2014 Giugliano FM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: The aim of this study was to demonstrate comparable pain relief with two schedules of radiotherapy(RT) for painful bone metastases in elderly patients assessed at baseline with the Cumulative Illness Rating Scale for Geriatrics (CIRS-G). Materials and methods: 132 elderly were analyzed. 77 received a single 8-Gy fraction and 55 received 20 Gy in 5 fractions. The choice of the treatment schedule was related to comorbidity, disability, target size and compliance. Pain intensity was measured with Numeral Rating Scale (NRS: 0=no pain; 10=high pain). Complete response was defined a pain reduction >3 of three points, partial response as a pain reduction ≥2 (2 ≤ pain reduction ≤ 3), no response was defined by pain score<2. Pain evaluation was recorded at baseline and at 1-4-8 weeks after completing RT. Results: overall response: 90.3% in 8 Gy arm (49.8% complete and 40.5% partial), 94.6% in 20 Gy arm (44.6% complete and 50%partial). No high grade toxicity were reported. The relief of pain was attained faster with single fraction (p-value ~ 0.2). We observed maximum response of pain control after 8 weeks and no significant differences were noted between two groups. The re-treatment rate was 17.6% vs. 11.1% respectively. Conclusions: no significant differences between the two arms in terms of pain response, pain control and toxicity. Our experience showed that not influenced by age, but in the elderly, life expectancy, comorbidities evaluated with the CIRS-G, and compliance, are crucial in selecting of shorter treatment.
Keywords
Bone metastases; Elderly patients; Radiation therapy; Pain control; Comorbidity index
Introduction
Thanks to the global improvement of health care, the world population is aging, so geriatric oncology is a growing field reflecting the demographic changes [1]. The definition of elderly patient is arbitrary, and in clinical practice biological age is more relevant than chronological age; some clinical trials use 70 years as the cut-off between elderly and younger patients. The elderly (people aged 65 years or older) account for 61% of all new cancer cases and 70% of all cancer deaths [2]. The incidence and prevalence of other chronic medical conditions increase with age. Therefore, elderly patients with cancer often have to not only the diagnosis of cancer, but a number of other medically relevant conditions in addition, evaluated thanks to a lot score [3].
Bone metastases (BM) are observed in approximately 50% of patients with cancer. Pain is the most common symptom in patients with bone metastases and radiation therapy provides significant pain relief. Quality of life, symptom control and toxicity of treatment are of major importance when considering the choice and efficacy of treatments [4]. The palliative radiation therapy, as in bone metastatic disease, has been shortened to minimize the time commitment for therapy while reaching the pain control [5-7]. However, the best schedule is still debated. Numerous randomized trials have been conducted on comparison between different dose fractionation schedules but this comparison have not been done in elderly population. In order to evaluate the efficacy of two different schedules in elderly patients, we analyzed 132 patients, in terms of pain relief and social advantages considering the CIRS-G score.
Materials and Methods
Patient characteristics
Our study sample was derived from elderly patients with painful BM, treated at single center of Radiation Therapy Department – National Cancer Institute "G. Pascale" in Naples, Italy, between January 2011 and May 2012. The study was retrospective. We analyzed 132 elderly patients: 69 males and 63 females with a median age of 76 years (range, 65-86).The inclusion criteria were: presence of only one site of pain and estimated life expectancy of at least 1 month. We divided the patients in two different groups: Group 1 treated with 8 Gy in single fraction and Group 2 treated with 20 Gy in 5 fractions. The choice of the schedule was related to comorbidity, disability, target size and compliance of patients. General condition was evaluated before and after treatment according to the Karnofsky Performance Status (KPS) index.
The comorbidities were recorded with the Cumulative Illness Rating Scale Geriatric Version (CIRS-G) [8]. CIRS-G is a valid instrument in elderly patients [9,10].
The score differentiates between 14 organ systems (vascular problems, haematopoietic system, respiratory tract, liver, gallbladder, pancreas, endocrine and metabolic diseases, breast, heart, musculoskeletal/integument, lower gastrointestinal tract, eyes, ears, nose, throat, genitourinary tract, upper gastrointestinal tract, neurological diseases, renal disorders, and psychiatric disorders). Every comorbidity of a patient was assigned to one of the organ systems and rated from 1 (mild comorbidity) to 4 (extremely severe comorbidity).
Patients who presented a number of affected organ system >3, and a number of affected organ system with severe or extremely severe disorders (levels 3-4) with cumulative score from 20 to 56 were preferentially included in the treatment with single fraction. Clinical signs of cord compression or poor state of health were considered exclusion criteria. Table 1 shows the characteristics of the sample.
| Group A (8Gy) | Group B (20Gy) | |
|---|---|---|
| Number of patients | 77 | 55 |
| Age(median) | 76 years (range 65-86) | |
| Sex | ||
| M | 41 | 28 |
| F | 36 | 27 |
| CIRS-G | 20-48 | 19-Aug |
Table 1: Pretreatment characteristics of groups studied.
Toxicity was assessed using the Radiation Therapy Oncology Group (RTOG) criteria [11].
BM of different sites were treated, the spine (vertebrae) was the most frequent site (54%), followed by the femur (20%) and pelvis (9.6%). The most frequent primary tumors (Table 2) were breast cancer (46.6%), prostate cancer (17%), lung cancer (11.1%), colon cancer (8%), liver (2.9%), and others (13.9%). In 75% the diagnosis were made by radiological exams as standard x-ray (67.6%), bone scintigraphy (26.7%), Magnetic Resonance Imaging (5.7%). In 25% the diagnosis were suspected during the clinical examination for the onset of pain [12].
| Characteristics of primary tumor and site lesion | ||
|---|---|---|
| N° of patients | Percentage (%) | |
| Site primitive tumor | ||
| Breast | 63 | 46.6 |
| Prostate | 23 | 17 |
| Lung | 15 | 11.1 |
| Colon | 11 | 8.1 |
| Kidneys | 9 | 6.6 |
| Liver | 4 | 2.9 |
| Other sites | 6 | 4.4 |
| Unknown | 4 | 2.9 |
| Site lesion | ||
| Spine | 73 | 54 |
| Femorus | 27 | 20 |
| Rib | 9 | 7 |
| Sternum | 6 | 4 |
| Pelvis | 13 | 9.6 |
| Humerus | 7 | 5 |
| Total | 135 | 100 |
Table 2: Characteristics of primary tumor and site lesion
Radiation therapy treatment
A Computed Tomography (CT) scan was performed for each patient, the positioning was realized using personalized vack-lock system and/or feet support related to different sites. CT axial scanning (slice tickness: 3 mm) was performed at 3 mm intervals (Toshiba Aquilion). 3D conformal treatment were planned using two opposed or multiple fields, with energy of 6-20 MV of photons. The dose distribution to the target was between 95% and 107% of the prescribed dose. Varian Eclipse planning station (Varian, Palo Alto, CA) was used for calculation and optimization.
Pain evaluation
Pain evaluation was recorded at baseline and at 1-4-8 weeks after completing RT. Not all patients were able to return for follow up so, in some cases, we used the telephone interviews. We analyzed the pain level using a Numeral Rating Scale (NRS: 0=no pain; 10=high pain). This method is very simple, repeatable and understandable, especially in this population . We defined complete response a pain score reduction >3, partial response a pain score reduction = 2 (2 = pain reduction = 3), no response was defined by a pain score<2. The pain score was obtained by subtracting pain value at 8 weeks after RT from pain value at baseline. The patients who were re-treated were considered relapsed, but we did not recorded the pain score value before the re-treatment.
Statistical analysis
We performed a likelihood ratio tests for Negative Binomial generalized linear models. A sequential analysis of deviance table is given for the fitted model. Given that for each time series 3 time point were available, we could consider a two factors model. More specifically we considered the factor treatment (trt), with the two levels 8 Gy and 20 Gy and the factor time, with the three levels 1w, 4w and 8w. As you can see from the Table 3, the factor treatment was not statistically significant (p>0.05), suggesting that the mean pain reduction between 8 Gy and 20 Gy is not relevant.
| Df | Deviance | Resid. Df | Resid. Dev | P(>|Chi|) |
|---|---|---|---|---|
| Trt1 | 3.247 | 394 | 206.58 | 0.07156 |
| Times2 | 62.788 | 392 | 143.79 | 2.322e-14*** |
| Trt:Times2 | 2.868 | 390 | 140.92 | 0.23832 |
Table 3: The factor treatment was not statistically significant (p>0.05), suggesting that the mean pain reduction between 8 Gy and 20 Gy is not relevant
Results
The present study compares two regimens, RT with 8 Gy in 1 fraction (Group 1: 77 patients) versus 20 Gy in 5 fractions (Group 2: 55 patients). In the prescription of radiotherapy fractionation, we considered comorbidity of patients: patients with a CIRS-G score = 20, usually was prescribed a single fraction which involved an lower patient access to the treatment center, and lower compliance to treatment.
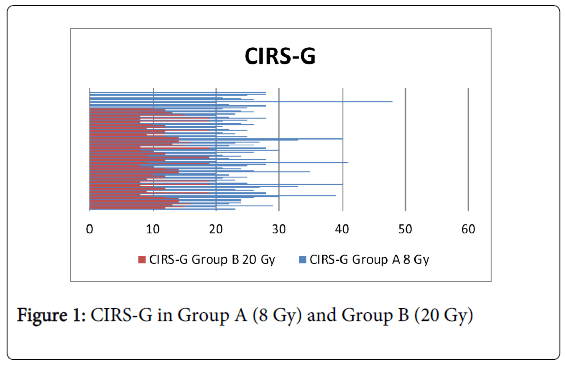
As shown in Figure 1 the CIRS-G was significantly higher in Group 1 (range 20-48) compared to Group 2 (range 8-19). Patients in Group 1 showed CIRS-G = 20. Patients in Group 2, with CIRS-G<20. All patients (Group 1-Group 2) completed the treatment.
The mean pain value at baseline, relative to NRS, was 7.4 in Group 1 and 7.16 in Group 2, respectively. The mean pain values at one and four weeks after the treatment were: 5.26 and 4.23 in Group 1 and 5.56 and 4.3 in Group 2. The mean pain reduction after 8 weeks from the end of the treatment was: 3.92 and 3.75, respectively. Statistical analysis shows that there is no significant difference between the two treatments in terms of pain reduction (p-value ~ 0.07). Figure 2 reports values of pain at 1-4-8 weeks, comparing single fraction with 5 fractions.
In terms of response at the end of radiation therapy (Table 4), we identified in Group 1: 37 patients (49.3%) with complete response, 32 patients (40.5%) with partial response and 8 no-responders (10.2%). Instead in Group 2 we observed 25 patients (44.6%) with complete response, 27 patients (50%) with partial response and 3 no responder (5.4%).The results of gain were 3.48 and 3.41 for single fraction and multifraction respectively. We observed the maximum response of pain control after 8 weeks and no significant differences were noted between two groups. Also KPS showed an improvement in both groups of patients. Treatment was well tolerated by patients. No cases of high grade toxicity were reported in both groups as hematological, skin toxicity, gastrointestinal and mucosytis. The most common acute toxicity was dermitis: 17% (12% was grade I and 5% was grade II) of patients with protracted treatment and in 7% in the single-fraction arm (5% grade I and 2% grade II). Gastrointestinal toxicity occurred less frequently (2% and 2%), in both arms was grade I. There were no grades 3 and 4 toxicity.
| Group A (8Gy) | Group B (20 Gy) | |
|---|---|---|
| Complete response | 37 | 25 |
| Partial response | 32 | 27 |
| No responders | 8 | 3 |
| Re-treatment | 16 | 3 |
Table 4: Gain and percentage of pain progression, net pain relief, toxicity, and re-treatment.
The re-treatment was performed in 16 patients Group 1 (20.7%) and 3 Group 2 (5.4%), respectively. The dose delivered was 8 Gy in all these cases.
Discussion
Radiation oncologist are often reluctant to treat elderly patients due to related adverse events. Gomez-Millan, in a recent review about radiotherapy in elderly patients, recommended specific geriatric examination to define appropriate sample for this treatment, in terms of side-effects and complications [13]. Moreover Zachariah et al. demonstrated that the age is not an exclusion criteria for an aggressive treatment in patients aged 80 years and older, proving, also, good outcomes [14]. Treatment of pain should be a top priority in cancer care. Pain occurs in about 50% of cancer patients and develops gradually over a period of weeks or months, worsening the quality of life of these patients [15]. Bone metastases are an important cause of pain and increase the risk of skeletal related events as pathological fractures, spinal cord compression, hypocalcaemia and bone marrow infiltration. Recent positive developments have occurred in all aspects of metastatic disease management: skeletal imaging, reconstructive orthopedic surgery and RT technique [16]. Radiation therapy is the optimal option for symptom control, low rates of side effects, short hospitalization. However, under-treatment of pain remains a considerable problem in the elderly population with cancer.
Comorbidity is any disease that coexist with but is not related to the index disease being studied. Many elderly patients have an increasing number of comorbidity [17].
A review by de Groot et al. identify 13 different method to measure comorbidity. They classified the Charlson-Index, the cumulative Illness rating scale (CIRS) and the Kaplan-Index as method to measure comorbidity for clinical research [18].
Numerous randomized trials have been conducted on dose fractionation schedules [7-19]; but without an analysis of the age 'elderly.
In our department we proposed this comparative study exclusively in elderly population considering the comorbidity and the pain relief using two different schedules of RT. The choice of the schedule was connected to comorbidity, disability, target size and compliance of patients. The results of our statistical analysis shows that single-fraction 8 Gy compared to 20 Gy in 5 fractions, in elderly patients, produced no significant difference in terms of pain reduction at the 8 weeks follow up, (p-value ~ 0.07).
These results are aligned with the systematic review of Chow et al. [20], that identified a total of 16 randomized trials from 1986 onward and showed that the overall response rates for pain were similar for single fraction (58%) and multiple fractions (59%), also, the complete response rates for pain were 23% for single and 24% for multiple fractions. In these studies the age wasn’t considered as a factor to analyze.
In 2003 Wu et al. [7] conducted a meta-analyses concluding there was no significant difference in complete and overall pain relief between single and multiple fractions, even though re-treatment rates were higher in patients treated with single schedule.
However, there is some evidence that certain group of patients would benefit from multiple fractions. Roos et al. [21] compared 8 Gy versus 20 Gy about neuropathic pain control and established that a single fraction was not effective for neuropathic pain as multiple, but also not significantly worse. Generally Roos recommend multiple fractions but he considered single taking into account long wait time in treatment medical center and short survival patients.
In terms of radiobiology, 8 Gy delivered in single fraction is a lower dose than the usual dose used for palliative intent, as 30 Gy (3 Gy/10 fractions), but it is sufficient to pain control. However, some questions are still unanswered as: the “optimal” single fraction to be used, the possibility of retreatment, and prognostic factors to identify patients that are more likely to respond to a single fraction.
About our selection, we chosen single fraction schedule in many cases for comorbidities and life expectancy, but also to the difficulty of keeping the position during the treatment. In some cases, patients wanted a short treatment to reduce the inconvenience (prolonged daily therapy, no companions, absence of RT center in small town and distance from main centers). Moreover, we completed consultation, treatment simulation and treatment itself on the same day, reducing the difficulty associated with travel. We thought that the cost of travel to reach our department had to be considered in the choice of the fractionation.
Regarding pain control, Cole et al. [22] concluded that a relief of pain can be achieved by single treatment and a quicker response can be observed in comparison to 24 Gy in 6 fractionation. Also, he observed an acceptable toxicity in single treatment. Instead, in our report the mean pain reduction between 8 Gy and 20 Gy was not relevant.
Considering the age of our patients, the duration of follow-up was limited and it could explain also the low rate of re-treatment in our sample, compared to data of literature [23]. Not all patients were able to return to make subsequent clinical visits; for this reason, in some cases, we used the telephone interviews.
In our study there were no cases of severe toxicity and the differences between the schedules were not significant. Dermatitis was the most common acute toxicity (7% in single fraction versus 17% in multi fraction schedules). Gastrointestinal toxicity was grade I in both arms. In the RTOG study [11] there were significant differences, and toxicity was higher in the 30-Gy arm compared with the 8-Gy arm: 17% vs. 10%, respectively.
Respect to the re treatment area, in a study of Hartsell et al. [24] observed a substantial difference in number of patients needing re-treatment, 18% of patients in the 8-Gy arm versus 9% in the 30-Gy arm (p<0.001). These results are observed in almost all reported studies [25,26]. According with these data, our results, concerning re-treatment, report 16 patients Group 1 versus 3 patients Group 2. Also Sze's meta-analysis [23] reported that in patients receiving single-fraction, the incidence of re-irradiation was 21.5% compared with 7.4% in the multifraction arm. In terms of economic costs, retreatment and non-medical costs, in van den Hout et al. analysis, on the Dutch Bone Metastasis Study [27], observed a significantly advantages for patients who received single fraction radiotherapy. Also, he considered the reduction in waiting times from insufficient treatment capacity the mayor economic advantage of single fraction RT.
Our observation about economic aspect was conducted taking into account the waiting list, the time machine, the cost of travel and the compliance of our patients.
We also believe that clinicians should encourage the enrolment of elderly patients on to clinical trials [28] to develop target guidelines.
Conclusions
The high incidence of cancer patients, as well as greater survival rates, leads a higher proportion of patients with painful bone metastases, so radiation therapy provides significant pain relief of symptomatic bone metastases. Literature data show that single-fraction regimen of 8 Gy is able to control the pain as a multi fraction regimen of 30 Gy. The choice in the internal protocol of our department of two different schedules in elderly patients, takes into account the location of bone metastases, the grade of pain, the comorbidity, the possibility to reach the center of radiotherapy, social and cultural issues. As is observed in other studies published, also in our report, there are no significant differences between the two arms in pain response, pain control and toxicity. Radiation departments should critically examine elderly patients considering comorbidities, life expectancy and lesion characteristics, to optimize the efficient use of radiation treatment for painful bone metastases.
Acknowledgment
The authors are grateful to Dr. Martina Samarelli for data collection.
References
- (1975-2004) SEER Cancer Statistic reviewed.
- Yancik R, Ries LA (2000) Aging and cancer in America. Demographic and epidemiologic perspectives. HematolOncolClin North Am 14: 17-23.
- Feinstein AR (1970) The pre-therapeutic classification of co-morbidity in chronic disease. J Chronic Dis23:455–469.
- Dempster M, Donnelly M (2000) How well do elderly people complete individualised quality of life measures: an exploratory study. Qual Life Res 9: 369-375.
- Timmerman RD (2008) An overview of hypofractionation and introduction to this issue of seminars in radiation oncology. SeminRadiatOncol 18: 215-222.
- van der Linden YM, Lok JJ, Steenland E, Martijn H, van Houwelingen H, et al. (2004) Single fraction radiotherapy is efficacious: a further analysis of the Dutch Bone Metastasis Study controlling for the influence of retreatment. Int J RadiatOncolBiolPhys 59: 528-537.
- Wu JS, Wong R, Johnston M, Bezjak A, Whelan T (2003) Cancer Care Ontario Practice Guidelines Initiative Supportive Care Group Meta-analysis of dose-fractionation radiotherapy trials for the palliation of painful bone metastases. Int J RadiatOncolBiolPhys 55: 594-605.
- Linn BS, Linn MW, Gurel L (1968) Cumulative illness rating scale. J Am GeriatrSoc 16: 622-626.
- Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L (2005) Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med 3: 223-228.
- Hudon C, Fortin M, Vanasse A (2005) Cumulative Illness Rating Scale was a reliable and valid index in a family practice context. J ClinEpidemiol 58: 603-608.
- Cox JD, Stetz J, Pajak TF (1995) Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC) Int J RadiatOncolBiolPhys 31: 1341-1346.
- Evangelista L, Panunzio A, Polverosi R, Ferretti A, Chondrogiannis S, et al. (2012) Early bone marrow metastasis detection: the additional value of FDG-PET/CT vs. CT imaging. Biomed Pharmacother 66: 448-453.
- Gomez-Millan J (2009) Radiation therapy in the elderly: more side effects and complications? Crit Rev OncolHematol 71: 70-78.
- Zachariah B, Balducci L, Venkattaramanabalaji GV, Casey L, Greenberg HM, et al. (1997) Radiotherapy for cancer patients aged 80 and older: a study of effectiveness and side effects. Int J RadiatOncolBiolPhys 39: 1125-1129.
- Slatkin N (2006) Cancer-related pain and its pharmacologic management in the patient with bone metastasis. J Support Oncol 4: 15-21.
- Souchon R, Feyer P, Thomssen C et al. (2010) Clinical Recommendations of DEGRO and AGO on Preferred Standard Palliative Radiotherapy of Bone and Cerebral Metastases, Metastatic Spinal Cord Compression, and LeptomeningealCarcinomatosis in Breast Cancer. Breast Care (Basel) 5:401-407
- Boyd CM, Darer J, Boult C et al. (2005) Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance Jama294:716-724
- de Groot V, Beckerman H, Lankhorst GJ, Bouter LM (2003) How to measure comorbidity. a critical review of available methods. J ClinEpidemiol 56: 221-229.
- Donato V, Valeriani M, Zurlo A (2003) Short course radiation therapy for elderly cancer patients. Evidences from the literature review. Crit Rev OncolHematol 45: 305-311.
- Chow E, Harris K, Fan G, Tsao M, Sze WM (2007) Palliative radiotherapy trials for bone metastases: a systematic review. J ClinOncol 25: 1423-1436.
- Roos DE, Turner SL, O'Brien PC et al. (2005) Trans-Tasman Radiation Oncology Group, TROG 96.05. Randomized trial of 8 Gy in 1 versus 20 Gy in 5 fractions of radiotherapy for neuropathic pain due to bone metastases (Trans-Tasman Radiation Oncology Group, TROG 96.05). Radio therOncol 75:54-63
- Cole DJ (1989) A randomized trial of a single treatment versus conventional fractionation in the palliative radiotherapy of painful bone metastases. ClinOncol (R CollRadiol) 1: 59-62.
- Sze WM, Shelley M, Held I et al. (2004) Palliation of metastatic bone pain: single fraction versus multifraction radiotherapy a systematic review of the randomised trials. Cochrane Database Syst Rev.
- Hartsell WF, Scott CB, Bruner DW, Scarantino CW, Ivker RA, et al. (2005) Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst 97: 798-804.
- Huisman M, van den Bosch MA, Wijlemans JW, van Vulpen M, van der Linden YM, et al. (2012) Effectiveness of reirradiation for painful bone metastases: a systematic review and meta-analysis. Int J RadiatOncolBiolPhys 84: 8-14.
- Hayashi S, Hoshi H, Iida T (2002) Reirradiation with local-field radiotherapy for painful bone metastases. Radiat Med 20: 231-236.
- van den Hout WB, van der Linden YM, Steenland E, Wiggenraad RG, Kievit J, et al. (2003) Single- versus multiple-fraction radiotherapy in patients with painful bone metastases: cost-utility analysis based on a randomized trial. J Natl Cancer Inst 95: 222-229.
- Zeng L, Chow E (2013) The added challenges of bone metastases treatment in elderly patients. ClinOncol (R CollRadiol) 25: 283-289.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 15196
- [From(publication date):
November-2014 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 10645
- PDF downloads : 4551