Efficiency of Surgical Masks and Respirators against Novel Corona Virus
Received: 18-Apr-2020 / Accepted Date: 02-May-2020 / Published Date: 09-May-2020 DOI: 10.4172/2332-0702.1000256
Abstract
A personal shield against the novel coronavirus pandemic is a major concern for health workers and patients in hospitals. In current review article an evaluation of effectiveness of surgical mask and respirators against novel SARS-CoV-2 is done by critical analysis of surgical masks, respirators and spreading mode of COVID-19 disease. The surgical masks have 32.9% particles filtration capability for standard lab aerosol test. Practically respirators also show less filtration capability from designed value. Hence surgical masks are not intended for protection against viral aerosol. Statistical analysis shows that N95 respirator is only beneficial for low inhalation flow rate (6l min-1). For high inhalation flow rate, and clinical encounters where spreading of COVID-19 disease is significance through eyes, N95 respirators are not efficient.
Keywords: Corona Virus; N95; Respirators; Surgical Masks; Filtration
Background
COVID-19 disease, due to novel coronavirus has been reported in December 2019 in Wuhan city, the capital city of Hubei in China. The virus is named by the world health organization (WHO) as ‘severe acute respiratory tract coronavirus-2 ’ (SARS-CoV-2). WHO has declared the SARS-CoV-2 as a pandemic disease SARS-CoV-2 infects the people of all ages [1]. However, old aged people and people with infected immune systems are more susceptible to SARS-CoV-2 [2]. By the date of 31 march, 2020 (for first three months) COVID-19 disease has been spread out to 203 countries with 858,319 total confirmed cases, 638,086 active cases and 42,302 confirmed deaths [3]. For defense against the transmission of this viral disease people are using surgical masks. These masks are fabricated by activated carbon, nonwoven fabric and cotton, these materials have fiber diameter in order of microns [4]. According to American Society for Testing and Materials (ASTM) surgical masks are classified into three categories due to different fluid resistance of 80 mmHg, 120 mmHg and 160 mmHg [5]. A surgical mask is a disposable, loose-fitting medical gadget that provides a bodily barrier among the nose and mouth of the user and viral aerosol in the environment. If the surgical mask is used effectively it will provide blockage against large hazardous particle droplets, sprays, splashes and splatter that could spread out this viral disease [6]. We have another medical gadget named as surgical respirator which is different from surgical mask. Surgical respirators are fabricated by thickened non-woven fabric [4]. Respirators are used to sieve out airborne particles for example bacteria and viruses and produce a seal around the nose and mouth. Respirators are used when viral, hazardous particles or vapors are present in the environment. Filtering face-piece respirators (FFRs) are categories into nine major category by the US National Institute for Occupational Safety and Health (NIOSH) (As shown in Table 1) [7]. Three types of respirator are established concerning sodium chloride salt (NaCl), which is lone slightly degrading to filter-media (N-series filters), similarly dioctyl phthalate (DOP) oil, which is extremely degrading (P or R series filters). N series filters are not resistant to oil, R series filters are weakly resistant to oil and P series filters are strongly resistant to oil. Hence respirators can be used against oily as well as non-oily aerosols. Besides, numerical values such as 95, 99, and 100 represent minimum filtration efficiency by 95%, 99%, and 99.97%, respectively. N series respirators can filter particles of size up to 0.075 ± 0.020 μm (approximately size of NaCl), whereas R and P series respirators can block particles of size up to 0.185 ± 0.020 μm [7].
| Type of Respirator | Filter Aerosol Particles | Resistant to Oily Particles | Block Minimal Particle Size (µm) | Minimum Service Life (Hour) |
|---|---|---|---|---|
| N95 | 95% | Not | 0.075 ± 0.020 | 8 |
| N99 | 99% | Not | 0.075 ± 0.020 | 8 |
| N100 | 99.97% | Not | 0.075 ± 0.020 | 8 |
| R95 | 95% | Weakly | 0.185 ± 0.020 | 8 |
| R99 | 99% | Weakly | 0.185 ± 0.020 | 8 |
| R100 | 99.97% | Weakly | 0.185 ± 0.020 | 8 |
| P95 | 95% | Strongly | 0.185 ± 0.020 | 40 |
| P99 | 99% | Strongly | 0.185 ± 0.020 | 40 |
| P100 | 99.97% | Strongly | 0.185 ± 0.020 | 40 |
Table 1: NIOSH’s Certified Series of Respirators.
Spreading Mode of SARS-CoV-2
The SARS-CoV-2 is transmitted mostly via tiny droplets or aerosol, but many times through direct interaction with hazardous contaminated surfaces. Any personal prevention from COVID-19 disease needs to concern with both of these approaches [8]. World Health Organization (WHO) proposed that a patient’s sneezing could yield 40,000 droplets nuclei of range 0.5 – 12 μm in diameter. These droplets nuclei could move with speed up to 100 m/s. These droplet nuclei come out of the patient ’ s nose or mouth via sneezing or coughing and spread toward the recipient through a straight spray assault [9]. Such nuclei can enter the eye, nose or mouth of the recipient. The size of droplet nuclei depends upon the distance between the recipient and source. A harmless distance of six feet is suggested which can minimalize the spreading of droplet nuclei [8-10]. According to study govern by National Institutes of Health (NIH) SARS-CoV-2 remains stable for numerous hours on surfaces and in aerosols present in environment. The experts originate that SARSCoV- 2 is observable on copper up to 4 hours, in aerosols up to 3 hours, on cardboard up to 24 hours, on stainless steel and plastic up to 2 days and 3 days respectively. This study offers major information concerning COVID-19 disease [11]. One can also be infected by transmission of SARS-CoV-2 through eyes. The ocular infection in humans by SARS-CoV-2 has not been studied widely. However, SARSCoV- 2 has been recognized to induce several ocular infections in other creatures. In murine and feline models anterior uveitis, conjunctivitis, optic neuritis, and retinitis have been recognized [12].
Efficiency of Surgical Masks against SARS-CoV-2
Non-woven fabric surgical mask only provide 32.9% filtration capability against atmospheric particulate matter of size 2.5 μm (PM2.5) 4. The size of the novel SARS-CoV-2 is about 0.1 μm [13], which is far lessen than the size of PM2.5. Besides, Centers for Disease Control (CDC) specifies that surgical masks are not completely successful in inhibiting breathing of viral aerosol (Such as in case of SARS-CoV-2) because these masks are not meant to designed to offer a close-fitting face cover or to sieve out hazardous particles in the droplet nuclei range of 1-5 microns [14].
Efficiency of Respirators against SARS-CoV-2
Surface of P and R series filters cannot block the penetration of SARS-CoV-2 due of its small size as compare to the filtration capability of filters. In N series filters N99 and N100 provides breathing resistance and cannot be wear for maximum time duration, Whereas N95 offers 50% less breathing resistance and a recommended respirator for health workers [15]. The actual filtration capability of the N95 respirator is reported to be ~90% as compared to surgical masks with ~34% [16]. Another study conclude that, at maximum inhalation flow rate N95 offers filtration capability less than 95% against 0.3 μm viral aerosol [17]. In another research, efficiency of N95 is checked against Bacteriophage MS2, Escherichia Virus T4 and Bacillus Subtilis. The size of MS2 is 0.02 – 0.09 μm, whereas 0.1 μm signify mobility sizes of Escherichia Virus T4 and Bacillus subtilis. The size of T4 and Bacillus Subtilis is best suited for case study of SARS-CoV-2. For normal inhalation flow rate (30 l min-1) T4 and Bacillus Subtilis have penetration percentage (PP) value of 0.23 and 0.58 respectively. For hard work inhalation flow rate (85 l min-1) T4 and Bacillus Subtilis have PP value 0.95 and 1.9 respectively [18].
Regression Analysis
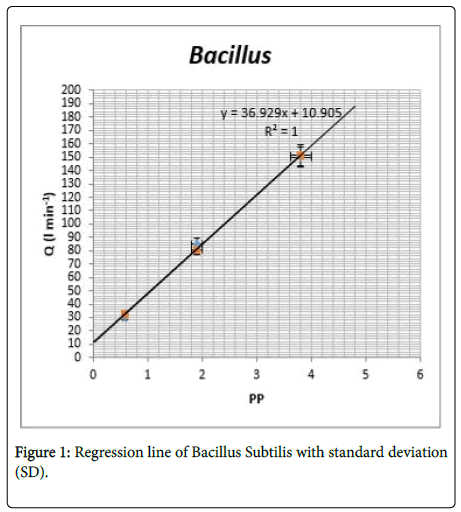
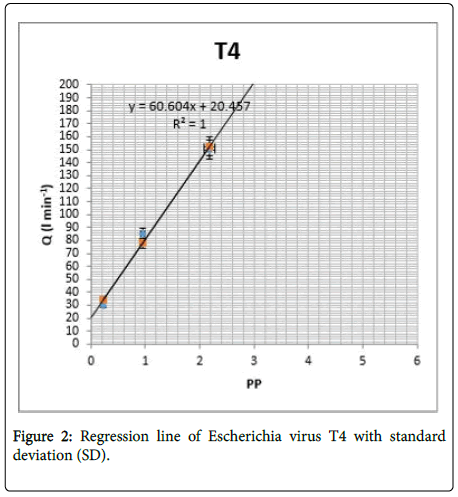
In stationary condition the average human breath rate is 6l min-1 (8 g/min or 11 kg/day) [19]. For calculation of PP at average human breath rate statistical analysis is significant. The regression line (in Figure 1 and 2) postulates that no aerosol penetration is observed at normal human breathing rate for B. Subtilis and T4. Still, there is no clinical study have done yet about respirators and surgical masks for safety against SARS-CoV-2 but the relative study has found in which these masks are tested against influenza virus (similar to SARSCoV- 2). The Medical Research Council (Imperial College) proposes that use of this respirator can decrease the probabilities of evolving COVID-19 disease, but note that the response may be poor [20].
Results
Droplet nuclei (of size 0.5 μm) produce by the patient’s sneezing can easily penetrate through the surface of surgical masks due to its high size than the filtration ability of masks. Surgical masks only have 32.9% filtration ability due to poor filtration ability and loose fitting round the face. Surgical masks should not recommend for precaution gadget against SARS-CoV-2 aerosol. N95 respirators can block viral aerosol of size 0.1 μm but at low inhalation flow rate (6l min-1). For maximum inhalation flow rate N95 respirator should not recommended as safety gadget against SARS-CoV-2.
Conclusion
In light of the above indications, it can be conclude that surgical masks should not be suggested as a precaution in front of SARS-CoV-2 pandemic. Surgical masks only provide protection against contamination yield by surgical wounds, produced by the surgical team. Secondly, N95 respirators are only suggested for low inhalation flow rate (6 l min-1) and minor hazard clinical encounters. N95 could be valuable to safe the health workers from an unintended aerosol challenge against an asymptomatic transporter of SARS-CoV-2 throughout the cultivation phase. Correspondingly if a health worker is in the asymptomatic incubation phase, this will reduce the aerosol challenge for an uninfected coworker or patient. It is suggested that an identified victim of COVID-19 disease attires this respirator to decrease coronavirus spreading and this measure is defensive to the health workers. In self-quarantine, this respirator is valuable for symptomatic patients to decrease virus load transportation to the other family members in quarantine. Lastly, for the high zone of COVID-19 pandemic (like hospitals), where infection through eyes is conceivable full-face respirators should be suggested. Eyes protection is necessary for health workers when they are dealing with patients of COVID-19 disease at clinics, since it might be possible that the virus may infect the eyes conjunctiva via droplets nuclei.
References
- Saqlain M, Munir MM, Ahmed A, Tahir AH, Kamran S (2020) Is Pakistan prepared to tackle the coronavirus epidemic?. Drugs Ther Perspect 20: 1-2.
- Meo SA, Al-Khlaiwi T, Usmani AM, Meo AS, Klonoff DC, et al. (2020) Biological and Epidemiological Trends in the Prevalence and Mortality due to Outbreaks of Novel Coronavirus COVID-19. J King Saud Univ Sci
- Li X, Gong Y (2015) Design of Polymeric Nanofiber gauze mask to prevent inhaling PM2.5 Particles from Haze Pollution. J Chem 2015: 1-5.
- Bałazy A, Toivola M, Adhikari A, Sivasubramani SK, Reponen T, et al. (2006) Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks?. Am J Infect Control 34: 51-57.
- Chartier Y, Pessoa-Silva CL. Natural ventilation for infection control in health-care settings. World Health Organization; 2009.
- American Academy of Opthalmology (2020) Corona Virus Eye Safety. [Available from: https://www.aao.org.eye health/tips prevention/corona-Virus-covid19-eye-infection-pinkeye]
- Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, et al. (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 382: 1564-1567.
- Seah I, Agrawal R (2020) Can the coronavirus disease 2019 (COVID-19) affect the eyes? A review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm 15:1-5.
- Zhu N, Zhang D, Wang W, Li X, Yang B, et al. (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382: 727-733.
- Charney W (2019) Handbook of Modern Hospital safety. CRC Press 2: 11-89.
- Nirvana Being (2020) Why N95 is a better choice for pollution protection than N99? [Available from: https://nirvanabeing.com/n95-better-choice-pollution-protection-n99/]
- Bowen LE (2020) Does that face mask really protect you?. Appl Biosafety 15: 67-71.
- Bałazy A, Toivola M, Adhikari A, Sivasubramani SK, Reponen T, et al. (2006) Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks?. Am J Infect Control 34: 51-57.
- Eninger RM, Honda T, Adhikari A, Heinonen-Tanski H, Reponen T, et al. (2008) Filter performance of N99 and N95 facepiece respirators against viruses and ultrafine particles. Ann Occup Hyg 52: 385-396.
- Halek, G. (1951) Physics of breathing. Bri Med J 1(4700): 246 [Available from: https//www3.nd.edu/~nsl/Lectures/mphysics/]
- A face mask may prevent you getting flu – but only if you wear it | Imperial News | Imperial College London.
Citation: Hassan JU (2020) Efficiency of Surgical Masks and Respirators against Novel Corona Virus. J Oral Hyg Health 8: 256. DOI: 10.4172/2332-0702.1000256
Copyright: © 2020 Hassan JU. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2431
- [From(publication date): 0-2020 - Apr 24, 2025]
- Breakdown by view type
- HTML page views: 1667
- PDF downloads: 764