Efficacy of Whole Body Vibration on Balance in Chronic Obstructive Pulmonary Disease Patients
Received: 05-Nov-2021 / Accepted Date: 19-Nov-2021 / Published Date: 26-Nov-2021
Abstract
Introduction: Reduced balance function has been observed in the Chronic Obstructive Pulmonary Disease (COPD) population and is associated with an increased risk of falls. This study aimed to examine balance sway by biodex and efficacy of Whole Body Vibration (WBV) on balance.
Materials and methods: Sixty volunteers with Chronic Obstructive Pulmonary Disease with age ranged from 45 years to 60 years old were selected in this study for 12 weeks. They were divided into two equal groups, control group-1 and whole body vibration group-2. Biodex assessment for dynamic balance, the measurement outcome of biodex balance assessment consisted of Anterior–Posterior Stability Index (APSI), Medio Lateral Stability Index (MLSI), and the Overall Stability Index (OST).
Results: There was significant reduction in postural sway, Medio Lateral (ML) and Anterior Posterior (AP) and Overall Stability Index (ST), p-value was respectively (p=0.001), (p=0.038) and (p=0.001). The whole body vibration training protocol include different training frequencies to evoke muscle contractions all over the body.
Conclusion: Whole body vibration training in COPD patients is beneficial and resulted in significant effect on balance with concomitant improvement of postural sway.
Keywords: Chronic Obstructive Pulmonary Disease; Balance; Biodex; Whole Body Vibration; Respiratory failure
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a common and treatable disease characterized by progressive airflow limitation and tissue destruction. It is associated with structural lung changes due to chronic inflammation from prolonged exposure to noxious particles or gases, most commonly cigarette smoke. Chronic inflammation causes airway narrowing and decreased lung recoil. The disease often presents with symptoms of cough, dyspnea, and sputum production. Symptoms can range from being asymptomatic to respiratory failure [1].
Balance impairments are specifically problematic, as individuals with COPD are up to 55% more likely to suffer a fall compared to their non-COPD counterparts. Falls are one of the leading causes of accidental injury death worldwide, and can lead to consequences such as injuries, decreased functioning, loss of independence, reduced quality of life, and an increased risk of morbidity and mortality [2].
Trunk movement and balance in COPD patients during walking has been evaluated by a triaxial accelerometer showed that, mediolateral bilateral difference and left–right symmetry difference of the trunk during walking. This approaches for COPD patient’s for assessment of their balance while walking. It is proven that the ambulatory disability of COPD patients is affected by not only their effort intolerance due to respiratory dysfunction but also their underlying balance control [3].
Across sectional study had done [4], on balance deficit and gait in COPD patients. His study included forty-two patients with COPD aged 45 years and gender-matched control subjects were included in the study. Gait parameters were assessed by Win-Track gait analyzer, the static balance was assessed by post urography, and the dynamic balance was assessed by the time up and go test. The study pointed out that decreased static and dynamic balance as assessed by post urography and time up and go test TUG.
Center-Of-Pressure (COP) displacement data were recorded by a force platform over 30s. Three trials of quiet standing were performed according to standardized verbal instructions given to the subject (e.g., ready go and relax). The subjects were asked to stand bare foot on the force platform with arms parallel to the body, not to talk, and to stand as still as possible for 30s to measure the postural sway of quiet standing results an increased sway velocity during quiet standing in COPD in the Anteroposterior (AP) but not in Mediolateral (ML) direction [4]. Balance training performed on a WBV platform is superior to improve objectively measured balance performance and muscular power compared to conventional balance board training in patients with COPD and functional impairment [5].
Materials and Methods
A randomized control study was carried out at faculty of physical therapy, Cairo University, Egypt. A convenient sample of 60 participants with age ranged from 45-60 years was included in the study. Investigation group consisted of 60 participants with COPD with both sexes, who were selected from kasrelainy clinic, Cairo University. Inclusion criteria consisted of the following: (1) patients in the study will have chronic obstructive pulmonary disease patients stage II, stage III; (2) their age were ranged from 45-60 years and; (3) absence of knee flexion contracture. All participants were divided into two groups equal in number. Control group-A and the whole body vibration group-B. All participants underwent an evaluative procedure to test dynamic (postural stability index) before and after 12 week. They provided written informed consent to participate in the study. Control group were received traditional physiotherapy program breathing exercises, breathing control techniques and home program, walking for 20-30 minutes in days out from session, incentive spirometer. Study group were received whole body vibration exercises and traditional physiotherapy program breathing exercises, breathing control techniques and home program, walking for 20-30 minutes in days out from session, incentive spirometer.
Test methods and measurement outcome
Dynamic balance control assessment: Biodex Balance System (BBS) was used to assess both PSIs and DLOS [6]. Biodex Balance System has demonstrated high reliability for evaluating dynamic postural balance in healthy people, in blind people. The system comprises eight stability levels, with level 8, the most stable and 1, the least stable. It also consists of a movable balance foot platform providing up to 20˚ of surface tilt in a 360˚ range of motion. The platform includes a foot grid illustration to determine the optimal foot position, allowing consistency in each trial in positioning the vertical ground reaction forces as well as the center of gravity in each test trial. The platform is connected to computer software that automatically calculates the measurement outcomes.
The measurement outcome consisted of Anterior–Posterior Stability Index (APSI), Mediolateral Stability Index (MLSI), and the Overall Stability Index (OSI). These measures calculate the amount of deviation and displacement angle of the platform from the baseline position. The higher the scores, the increased motion from baseline level, the higher the sway, and the poorer the balance. With the participant standing barefoot on the platform holding onto the support handle, its height was adjusted accordingly. With eyes open, the participant was instructed to maintain his/her foot in a centered position on the platform by using the foot angles and coordinates on the platform grid. The participant’s weight, height, and age were then logged into the device. The platform stability level was set at five (moderate), and test duration was set for 30s as the test proceeded, the participant was instructed to release the device handle and maintain a leveled platform by means of sustaining a cursor centered on a bull’s eye located on the screen grid through visual feedback. The start key was then engaged in the control panel to unlock the platform (which took five seconds to actually start), and an auditory alarm beeped just before the test proceeded. Two test trials were executed before the specific trial outcome was recorded for the purpose of instrumentation familiarity before data collection. At the end of each test trial, a printout report was obtained documenting OSI, APSI, and MLSI.
Therapeutic procedure of whole body vibrations
Practical protocol: Training frequency three times per week, for duration three sets three minutes (nine minutes) per day at 25-35 Hz, and 6 mm peak-to-peak amplitude that’s evokes muscle contractions all over the body, that occurs passively, patient standing with static squatting (semi flexion in knees) [5].
Statistical procedures
Data collection: Data were collected, revised, coded and entered to the statistical package for social science (IBM SPSS).
Data analysis: Results are expressed as mean ± standard deviation. Comparison between categorical data number (%) was done using Chi square test. Test of normality, kolmogorov-smirnova test, was performed to measure the distribution of data. Comparison between normally distributed data (variables) in the two groups was performed using unpaired t test. Analysis of Covariance (ANCOVA) test was used to compare the pre-treatment values of the two groups and on the same time between post-treatment values on controlling the effect of pre-treatment values. Comparison between pre and post-treatment data in the same group was performed using paired t test. Comparison between not normally distributed data (variables) in the two groups was performed using Mann Whitney test. Comparison between pre and post-treatment data in the same group was performed using Wilcoxon signed ranks test. Statistical Package for Social Sciences (SPSS) computer program was used for data analysis. p value ≤ 0.05 was considered significant.
Results
General characteristics of the patients
Age (years): As presented in Table 1 and Figure 1, the mean ± SD values of age in groups-A and group-B were 51.87 ± 4.64 and 52.50 ± 4.45 years, respectively. The unpaired t test revealed that there was no statistically significant difference between them (t value=-0.539, p=0.592).
| Group A (n=30) | Group B (n=30) | t-value | p-value | |
|---|---|---|---|---|
| Age (yrs.) | 51.87 ± 4.64 | 52.50 ± 4.45 | -0.539 | 0.592 (NS) |
| Gender | ||||
| Female | 13 (43.3%) | 13 (43.3%) | x2=0.00 | 1.000 (NS) |
| Male | 17 (56.7%) | 17 (56.7%) | ||
| Weight (kg) | 81.50 ± 11.13 | 82.80 ± 7.70 | -0.526 | 0.601 (NS) |
| BMI (kg/m2) | 30.32 ± 3.66 | 29.98 ± 2.95 | 0.396 | 0.694 (NS) |
Note: Data are expressed as mean ± SD or number (%); NS=p>0.05=Not significant.
Table 1: General characteristics of the two studied groups.
Gender: In group-A, the number of females and males were 13 (43.3%) and 17 (56.7%), respectively.
Also in group-B, the number of females and males were 13 (43.3%) and 17 (56.7%), respectively.
They were statistically comparable (Chi square test=0.00 and p-value=1.000) (Figure 2).
Weight (kilograms): As presented in Figure 3, the mean ± SD values of weight in groups-A and group-B were 81.50 ± 11.13 and 82.80 ± 7.70 kg, respectively. The unpaired t test revealed that, there was no statistically significant difference between them (tvalue=- 0.526, p=0.601).
BMI (kg/m2): As presented in and Figure 4, the mean ± SD values of BMI in groups-A and group-B were 30.32 ± 3.66 and 29.98 ± 2.95 kg/m2, respectively. The unpaired t test revealed that there was no statistically significant difference between them (t-value=0.396; p=0.694).
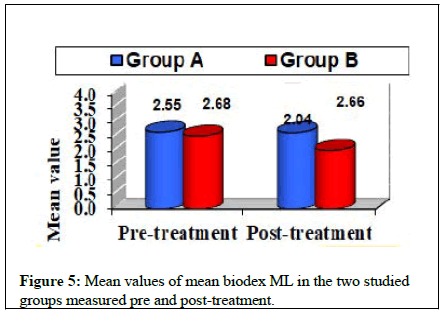
Biodex ML
Within group comparison (intra-group comparison): In group-A, there was no statistical significant difference between the mean value of biodex ML measured at pre-treatment (2.68 ± 0.68) and its corresponding value measured at post-treatment (2.66 ± 0.77) with tvalue= 0.310 and p-value=0.759 (Table 2 and Figure 5). While in group-B, there was a statistical significant decrease in the mean value of biodex ML measured at post-treatment (2.04 ± 0.37) when compared with its corresponding value measured at pre-treatment (2.55 ± 0.70) with t-value=4.993 and p-value=0.001 (Table 2 and Figure 5). The percent decrease in biodex ML value in group-A and group-B was 0.75% and 20.0%, respectively (Table 2).
| Group A (n=30) | Group B (n=30) | F value | p-value | |
|---|---|---|---|---|
| Pre-treatment | 2.68 ± 0.68 | 2.55 ± 0.70 | 0.568 | 0.454 (NS) |
| Post-treatment | 2.66 ± 0.77 | 2.04 ± 0.37 | 25.738 | 0.001 (S) |
| Mean difference | 0.02 | 0.51 | ||
| % change | 0.75 ↓↓ | 20.00 ↓↓ | ||
| t-value | 0.31 | 4.993 | ||
| p-value | 0.759 (NS) | 0.001 (S) |
Data are expressed as mean ± SD. F value=ANCOVA test; t value=paired t test. NS=p>0.05=not significant; S=p ≤ 0.05=significant.
Table 2: Inter- and intra-groups comparison between mean values of biodex ML in the two studied groups measured at pre- and posttreatment.
Between group’s comparison (inter-groups comparison): At pretreatment, in groups A and B, the mean values (± SD) of biodex ML were 2.68 ± 0.68 and 2.55 ± 0.70, respectively. There was no statistical significant difference between the two groups (F=0.568 and p=0.454) (Table 2). ANCOVA test was used to compare the posttreatment values of the two groups on controlling the effect of pretreatment value. The results of biodex ML revealed that there was a statistical significant decrease in its values in group B (2.04 ± 0.37) when compared with its corresponding value measured in group A (2.66 ± 0.77) (F=25.738 and p=0.001) (Table 2 and Figure 5).
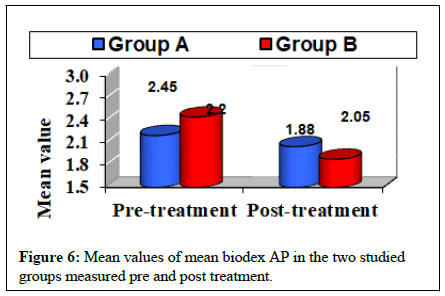
Biodex AP
Within group comparison (intra-group comparison): In group-A, there was no statistical significant difference between the mean value of biodex AP measured at pre-treatment (2.20 ± 0.80) and its corresponding value measured at post-treatment (2.05 ± 0.47) with t value=0.939 and p value=0.356 (Table 3 and Figure 6). While in group-B, there was a statistical significant decrease in the mean value of biodex AP measured at post-treatment (1.88 ± 0.39) when compared with its corresponding value measured at pre-treatment (2.45 ± 0.53) with t value=8.392 and p value=0.001 (Table 3 and Figure 6). The percent decrease in biodex AP value in groups A and B was 6.82% and 23.27%, respectively (Table 3).
| Group A (n=30) | Group B (n=30) | F value | p value | |
|---|---|---|---|---|
| Pre-treatment | 2.20 ± 0.80 | 2.45 ± 0.53 | 2.049 | 0.158 (NS) |
| Post-treatment | 2.05 ± 0.47 | 1.88 ± 0.39 | 4.51 | 0.038 (S) |
| Mean difference | 0.15 | 0.57 | ||
| % change | 6.82 ↓↓ | 23.27 ↓↓ | ||
| t value | 0.939 | 8.392 | ||
| p value | 0.356 (NS) | 0.001 (S) |
Data are expressed as mean ± SD. F value=ANCOVA test; t value=paired t test. NS=p>0.05=not significant; S=p ≤ 0.05=significant.
Table 3: Inter- and intra-groups comparison between mean values of biodex AP in the two studied groups measured at pre- and posttreatment.
Between group’s comparison (inter-groups comparison): At pretreatment, in groups A and B, the mean values (± SD) of biodex AP were 2.20 ± 0.80 and 2.45 ± 0.53, respectively. There was no statistical significant difference between the two groups (F=2.049 and p=0.158) (Table 3). ANCOVA test was used to compare the posttreatment values of the two groups on controlling the effect of pretreatment value. The results of biodex AP revealed that there was a statistical significant decrease in its values in group B (1.88 ± 0.39) when compared with its corresponding value measured in group A (2.05 ± 0.47) (F= 4.510 and p=0.038) (Table 3 and Figure 6).
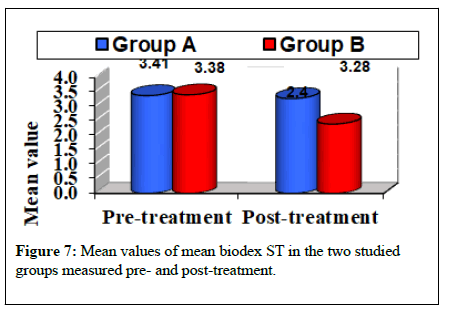
Biodex ST
Within group comparison (intra-group comparison):In group A, there was no statistical significant difference between the mean value of biodex ST measured at pre-treatment (3.38 ± 0.85) and its corresponding value measured at post-treatment (3.28 ± 0.80) with tvalue= 1.072 and p-value=0.292 (Table 4 and Figure 7). While in group B, there was a statistical significant decrease in the mean value of biodex ST measured at post-treatment (2.40 ± 0.36) when compared with its corresponding value measured at pre-treatment (3.41 ± 0.61) with t-value=10.386 and p-value=0.001 (Table 4 and Figure 7). The percent decrease in biodex ST value in groups A and B was 2.96% and 29.62%, respectively (Table 4).
| Group A (n=30) | Group B (n=30) | F value | p-value | |
|---|---|---|---|---|
| Pre-treatment | 3.38 ± 0.85 | 3.41 ± 0.61 | 0.037 | 0.848 (NS) |
| Post-treatment | 3.28 ± 0.80 | 2.40 ± 0.36 | 65.158 | 0.001 (S) |
| Mean difference | 0.1 | 1.01 | ||
| % change | 2.96 ↓↓ | 29.62 ↓↓ | ||
| t-value | 1.072 | 10.386 | ||
| p-value | 0.292 (NS) | 0.001 (S) |
Note: Data are expressed as mean ± SD. F value=ANCOVA test; t-value=paired t-test. NS= p>0.05=not significant; S=p ≤ 0.05=significant.
Table 4: Inter and intra-groups comparison between mean values of biodex ST in the two studied groups measured at pre and posttreatment.
Between group’s comparison (inter-groups comparison): At pretreatment, in groups A and B, the mean values (± SD) of biodex ST were 3.38 ± 0.85 and 3.41 ± 0.61, respectively. There was no statistical significant difference between the two groups (F=0.037 and p=0.848) (Table 4). ANCOVA test revealed that there was a statistical significant decrease in the mean values biodex ST in group B (2.40 ± 0.36) when compared with its corresponding value measured in group A (3.28 ± 0.80) (F=65.158 and p=0.001) (Table 4 and Figure 7).
Discussion
Chronic Obstructive Pulmonary Disease (COPD) is a diversified disease with many extra pulmonary manifestations. Impaired balance function is frequently found in these patients and is associated with functional problems in daily life and an elevated fall risk. Preserving balance function in COPD patients is critical importance to sustain their quality of life and reduce the risk of falls. Hence, the American Thoracic Society/European Respiratory Society guidelines recommended that balance function needs to be assessed after pulmonary rehabilitation in COPD patients. Previous studies in COPD focused mainly on one or more risk factors of balance impairment including age, lung health (e.g., severity of lung disease, COPD phenotype [6], the presence of exacerbations, [7] muscle strength, physical activity level [8], mobility, and usage of oxygen [9]. In this study, there is significant (p=0.001) in ML (Mediolateral sway) biodex, (p=0.038) in AP biodex (Anteroposterior sway) and (p=0.001) in overall Stability Index of biodex (ST). These results of this study were coincided with results of many studies [5] who confirm that whole body vibration improve balance performance and muscular power significantly more, compared to conventional balance training. The study [9] revealed that whole body vibration training can be an effective training mode to counteract consequences of physical inactivity such as muscle atrophy and loss of bone density. WBVT can be used and required add-on exercise modality during pulmonary rehabilitation of COPD patients. Also the study [10] concluded that using Whole-Body Vibration (WBV) as a type of exercise that improves muscle function and the Distance Walked (DW) especially in Egyptian patients with COPD.
Moreover Porto, et al. [11] showed that, a four-week WBV training setup was compared to a matched intervention program with identical training parameters in both training settings. Balance, jump height and local static muscle endurance revealed significant interaction effects for balance and local static muscle endurance in whole body vibration group. Complementary to these finding our study also supported by Nasrallah, et al. [12] who demonstrated that, use of Whole-Body Vibration (WBV) as a component of pulmonary rehabilitation to assist management of patients with COPD as it beneficial in improvement functional performance of the lower limbs. Regarding Ritzmann, et al. [13] demonstrated that, postural sway was significantly reduced after (WBV) a reduction of H-reflexes, M-waves as well as muscle cocontraction was observed. Postural sway changes correlated positively with reflex amplitude change. Thus, greater inhibition in spinal excitability after whole body vibration. The balance assessment done by Postural sway, antagonist co-contraction of selected lower limb muscles soleus, gastrocnemius medialis, tibialis anterior, rectus femoris, biceps femoris and soleus spinal excitability (H-reflexes) were recorded by means of post urography and electromyography, respectively.so whole body vibration represents a possible intervention to improve postural control.
Moreover Sá-Caputo, et al. [14] who demonstrated that, eight weeks of WBV training improves limits of stability and sit-to-stand performance, isokinetic knee extensor power compared with body weight exercises. The results of our study were also supported by Krause, et al. who found that whole body vibration exercise improve physical performance and neuromuscular function in individuals with chronic obstructive pulmonary disease [15]. Our research is not compatible with the research proved that combining strengthening with Whole-Body Vibration Training (WBVT) has significant beneficial short-term effects on Functional Exercise Capacity (FEC) in adults with COPD [16].
Conclusion
Combined whole body vibration training and strengthening was not more effective than strengthening alone for improving lower limb muscle strength, pulmonary function and quality of life.
In conclusion, supervised whole body vibration training program in COPD patients is beneficial and resulted in significant effect on balance with concomitant improvement of postural sway.
References
- Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, et al. (2007) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 176: 532-555.
- Hakamy A, Bolton CE, Gibson JE, McKeever TM (2018) Risk of fall in patients with COPD. Thorax 73: 1079-80.
- Terui Y, Iwakura M, Suto E, Kawagoshi A, Sugawara K, et al. (2018) New evaluation of trunk movement and balance during walking in COPD patients by a triaxial accelerometer. Int J Chron Obstruct Pulmon Dis 13: 3957.
- Jirange P, Vaishali K, Sinha MK, Bairapareddy KC, Alaparthi GK (2021) A cross-sectional study on balance deficits and gait deviations in COPD patients. Can Respir J 16: 89-95.
- Gloeckl R, Schneeberger T, Leitl D, Reinold T, Nell C, et al. (2021) Whole-body vibration training versus conventional balance training in patients with severe COPD—A randomized controlled trial. Respir Res 22: 1-2.
- Voica AS, Oancea C, Tudorache E, Crisan AF, Fira-Mladinescu O, et al. Chronic obstructive pulmonary disease phenotypes and balance impairment. Int J Chron Obstruct Pulmon Dis 11: 919.
- Ghareeb DM, McLaine AJ, Wojcik JR, Boyd JM (2017) Effects of two warm-up programs on balance and isokinetic strength in male high school soccer players. J Strength Cond Res 31: 372-379.
- Tudorache E, Oancea C, Avram C, Fira-Mladinescu O, Petrescu L, et al. (2015) Balance impairment and systemic inflammation in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 10: 1847.
- Iwakura M, Okura K, Shibata K, Kawagoshi A, Sugawara K, et al. (2016) Relationship between balance and physical activity measured by an activity monitor in elderly COPD patients. Int J Chron Obstruct Pulmon Dis 11: 1505.
- Vanfleteren LE, Gloeckl R (2019) Addâ€on interventions during pulmonary rehabilitation. Respirology 24: 899-908.
- Porto EF, Pradella CO, Rocco CM, Chueiro Jr M, Maia RQ, et al. (2017) Comparative postural control in COPD patients and healthy individuals during dynamic and static activities. J Cardiopulm Rehabil Prev 37: 139-145.
- Nasrallah TM, Emam H, Alwakil IM, Ahmad AA (2020) Effects of Whole-Body Vibration on Egyptian Patients with Chronic Obstructive Pulmonary Disease. J Med Arts 2: 420-426.
- Ritzmann R, Kramer A, Bernhardt S, Gollhofer A (2014) Whole Body Vibration Training - Improving Balance Control and Muscle Endurance. PloS one 9: e89905.
- Sá-Caputo D, Gonçalves CR, Morel DS, Marconi EM, Fróes P, et al. (2016) Benefits of whole-body vibration, as a component of the pulmonary rehabilitation, in patients with chronic obstructive pulmonary disease: a narrative review with a suitable approach. Evid Based Complement Alternat Med.
- Krause A, Ritzmann R, Lee K, Freyler K, Gollhofer A (2019) Acute Neuromuscular Modulation Enhances Postural Control after Whole-Body Vibration. Dtsch Z Sportmed 70.
- Ko MC, Wu LS, Lee S, Wang CC, Lee PF, et al. (2017) Whole-body vibration training improves balance control and sit-to-stand performance among middle-aged and older adults: a pilot randomized controlled trial. Eur Rev Aging Phys Act 14: 11.
Citation: Ezzat H, Sabry IM, Mehmed S, Rashid MM (2021) Efficacy of Whole Body Vibration on Balance in Chronic Obstructive Pulmonary Disease Patients. J Card Pulm Rehabi 5:152.
Copyright: © 2021 Ezzat H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 2309
- [From(publication date): 0-2021 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 1735
- PDF downloads: 574