Research Article Open Access
Efficacy of Endoscopic Nasobiliary Drainage in Consecutive 100 Patients: A Single Center Experience
Fatih Tekin*, Omer Ozutemiz, Galip Ersoz and Oktay Tekesin
Department of Gastroenterology, Ege University Medical School, Izmir, Turkey
- Corresponding Author:
- Dr. Fatih Tekin
Ege Universitesi Tip Fakultesi
Gastroenteroloji Bilim Dali
Bornova, 35100, Izmir, Turkey
Tel: +90-232-3904357
Fax: +90-232-3427764
E-mail: drtekinfatih@gmail.com
Received Date: July 16, 2015 Accepted Date: September 15, 2015, Published Date: September 21, 2015
Citation:Tekin F, Ozutemiz O, Ersoz G, Tekesin O (2015) Efficacy of Endoscopic Nasobiliary Drainage in Consecutive 100 Patients: A Single Center Experience. J Gastrointest Dig Syst S13:001. doi:10.4172/2161-069X.1000S13-001
Copyright: ©2015, Tekin F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Objective: The aim of this retrospective study was to assess the efficacy of endoscopic nasobiliary drainage (ENBD) at a tertiary referral center.
Methods: Patients who had been performed ENBD were included in the study.
Results: ENBD was performed in 100 patients (53 female, median age: 46 (17-84)) with biliary leak (n=30), cholangitis (n=67), and iatrogenic duodenal perforation (n=3). The most common etiologies for biliary leak were laparoscopic cholecystectomy (LC) (n=19) and orthotopic liver transplantation (OLT) (n=8). The most common site of biliary leak was found to be cystic duct stump (15/19, 79%) in LC patients, and biliary anastomosis in OLT patients (6/8, 75%). All of the patients with biliary leak (n=30) underwent to endoscopic papillary sphincterotomy (EST). Healing of biliary leak was observed in all patients. Viscous pus in the bile was observed during ERCP procedure in all patients with cholangitis. The most common etiologies for cholangitis were malignant biliary obstruction (n=21), benign biliary stricture (n=18), and bile duct stone (n=14). Of the 67 patients with cholangitis, EST was performed in 64 (95.5%) patients. Recovery was achieved, and second ERCP session or surgical treatment was applicable in all 67 patients with cholangitis.
Conclusions: ENBD with EST is efficient and safe to treat both the postoperative biliary leaks and the lifethreating cholangitis, and gives chance to perform subsequent definite treatments in patients with cholangitis.
Keywords
Nasobiliary Drainage; Endoscopic sphincterotomy; Biliary leak; Cholangitis
Introduction
Many surgeons now prefer laparoscopic cholecystectomy (LC) instead of open cholecystectomy (OC). However, it has been reported that LC has more complication incidence of bile duct injuries than OC [1]. Bile duct leak is known to be one of the main postoperative biliary complications after LC. In addition, orthotopic liver transplantation (OLT) is widely applied to end-stage liver disease, and 13-35% of procedures are complicated by biliary tract problems, mainly being biliary anastomotic strictures and leaks [2-4]. Therapy options of postoperative biliary leaks include reoperation, percutaneous transhepatic biliary drainage (PTBD) and endoscopic retrograde cholangiopancreatography (ERCP). Reoperation has a higher percentage of complication [5], and PTBD has a lower success rate because of lack of biliary dilation [6]. Thus, ERCP is now the gold standart therapeutic option for postoperative biliary leaks, however, controversy exists about the method of endoscopic therapy (endoscopic nasobiliary drainage (ENBD) vs. stent placement, ±endoscopic papillary sphincterotomy (EST)) [7]. Controversy also exists about the endoscopic therapeutic method for patients with cholangitis [8]. In this study, we evaluated the efficacy of ENBD with/ without EST for patients with biliary leaks and cholangitis.
Patients and Methods
The reports of ERCP performed between March 2006 and January 2008 were retrospectively evaluated. The patients who have been performed ENBD included into the study. ERCP was performed by four resident endoscopists with therapeutic duodenoscopes (Olympus TJF 145, TJF 160 and TJF 240) under sedation, if there was no contraindication, with midazolam+meperidine. Routine iv hyoscine N-butylbromide was used for duodenal peristalsis. Informed consent was routinely obtained from all the patients before the procedure.
Biliary leak was diagnosed by the clinical features of bile peritonitis (physical examination, laboratory and radiologic findings) and/or the presence of bile-like drainage from the abdominal suction tube. Healing of the biliary leak was suggested when the bile-like drainage from the abdominal suction tube disappeared for consecutive three days or cholangiography through the nasobiliary drainage tube confirmed the healing on the 14th day after the procedure. Cholangitis was suggested when the pus in the bile was observed during ERCP procedure. The presence of, if any, abdominal pain, fever, leukocytosis and/or jaundice supported the diagnosis of cholangitis.
Normal tip ERCP catheters, pull-type or needle-type sphincterotomes were used for selective common bile duct (CBD) cannulation. Pigtail-tip nasobiliary drainage tube with a 7-Fr diameter was used in all patients. EST was performed in all patients except the ones with prolonged prothrombin time and/or low platelet count (<50.000/mm3
Results
ENBD was performed in 100 consecutive patients (47 male, 53 female, median age: 46 (17-84)) for biliary leak (n=30), iatrogenic type 2 (peri-Vaterian) perforation during ERCP procedure (n=3), and cholangitis (n=67). Viscous pus in the bile was observed during ERCP procedure in all patients with cholangitis. EST was performed in all patients except three cases with prolonged prothrombin time and low platelet count due to disseminated intravascular coagulation with severe cholangitis and sepsis. Biliary leak was mostly due to OLT and LC operations, and cholangitis was mostly induced by benign stricture, bile duct stone, and malignancy (Table 1).
| Indication | n (%) |
|---|---|
| Biliary leak | 30 (30) |
| After LC | 19 (19) |
| After OLT | 8 (8) |
| Post cyst hydatid operation | 2 (2) |
| Traffic accident | 1 (1) |
| Cholangitis | 67 (67) |
| Stricture | 18 (18) |
| Bile duct stone | 14 (14) |
| Bile duct stone with stricture | 8 (8) |
| Bile duct stone with Mirizzi syndrome | 5 (5) |
| Caroli disease with intrahepatic abscess | 1 (1) |
| Malignancy | 21 (21) |
| Perforation during ERCP procedure | 3 (3) |
Table 1: Indications for endoscopic nasobiliary drainage (n=100). LC: laparoscopic cholecystectomy, OLT: orthotopic liver transplantation, ERCP: endoscopic retrograde cholangiopancreatography.
All the biliary leaks (n=30) healed after ENBD with EST. The median time of leak resolution was 9.6 days (4-19 days) in 22 patients with complete documentation. There were 19 patients with biliary leak after LC operation, and the most common site of biliary leak was found to be cystic duct stump. Among the patients with LC operation, there were 4 patients with T-tube, 4 patients with accompanying bile duct stone and 2 patients with accompanying common hepatic duct stricture. Bile duct stones were extracted in these 4 patients, and strictures were dilated in 2 patients before ENBD was performed. ERCP revealed anastomotic leak in 6 (75%) of 8 patients with biliary leak after OLT operation (Table 2). Biliary reconstruction included single duct-to-duct anastomosis in all patients with OLT.
| Features of the patients | n (%) |
|---|---|
| After LC | 19 (63.3) |
| Healed / reoperation needed | 19 (100) / 0 (0) |
| Leak site (cystic duct stump / CHD) | 15 (79) / 4 (21) |
| T-tube present (yes / no) | 4 (21) / 15 (79) |
| Accompanying bile duct stone (yes / no) | 4 (21) / 15 (79) |
| Accompanying stricture at CHD (yes / no) | 2 (11) / 17 (89) |
| After OLT | 8 (26.7) |
| Healed / reoperation needed | 8 (100) / 0 (0) |
| Leak site (anastomosis / RHD) | 6 (75) / 2 (25) |
| Post cyst hydatid operation | 2 (6.7) |
| Healed / reoperation needed | 2 (100) / 0 (0) |
| Leak site (RHD) | 2 (100) |
| Traffic accident | 1 (3.3) |
| Healed / operation needed | 1 (100) / 0 (0) |
| Leak site (CHD) | 1 (100) |
Table 2: Features of the patients with biliary leak (n=30). LC:Laparoscopic cholecystectomy, OLT: Orthotopic liver transplantation,CHD: Common hepatic duct, RHD: Right hepatic duct.
There were 67 patients with cholangitis mostly induced by benign stricture, bile duct stone, and malignancy. The bile stones (n=14) could not be extracted during the first ERCP session because of the big sizes of the stones and/or the short ERCP procedure time due to the poor general status of the patients.
The bile stones were extracted at the second ERCP session in 12 of these 14 patients. Eight of these patients underwent dilation with large balloons (10- to 20-mm diameter, esophageal/pyloric type) as defined previously [9]. Plastic stent placement was performed in the remaining 2 patients since cholecystectomy operation was found to be highly risky due to advanced age and coexisting disease(s).
There were 8 patients with bile duct stone plus benign stricture (Table 1). These inflammatory strictures were probably due to traumatic effect of bile stones, and all were at the distal part of the CBD. Biliary dilation plus stone extraction was successfully performed at the second ERCP procedure in all these 8 patients.
Histopathological examination of the endoscopic biopsy specimens taken from the strictures revealed no malignancy in 4 patients. Endoscopic biopsy was not performed in the remaining 4 patients.
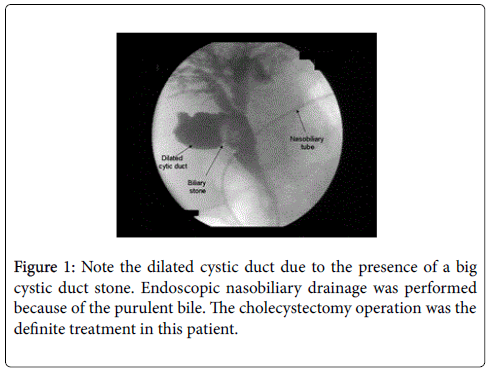
Accompanying common bile duct stones were extracted at the first ERCP session in 5 patients with Mirizzi syndrome, and thereafter these 5 patients were sent to surgery for cholecystectomy operation (Figure 1). Details of the patients with benign biliary stricture and malignancy were summarized in Tables 3 and 4, respectively.
| Etiology of the structure | n (%) | Subsequent treatment |
|---|---|---|
| After OLT (at anastomosis) placement | 6 (33.3) | 2nd ERCP: Dilation + stent |
| After LC (at CHD) placement | 4 (22.2) | 2nd ERCP: Dilation + stent |
| Compression of CHD by cyst hydatid | 4 (22.2) | Surgical treatment |
| PSC (at CHD) | 2 (11.1) | 2nd ERCP: Dilation |
| Post cyst hydatid operationplacement | 1 (5.6) | 2nd ERCP: Dilation + stent |
| Chronic pancreatitis | 1 (5.6) | Surgical treatment |
Table 3: Features of the patients with cholangitis due to benign stricture (n=18). OLT: orthotopic liver transplantation, LC: Laparoscopic cholecystectomy, CHD: Common Hepatic Duct, PSC: Primary Sclerosing Cholangitis, ERCP: ndoscopic Retrograde Cholangiopancreatography
| Features of the patients | n (%) | Subsequent treatment (n) |
|---|---|---|
| Cholangiocellular carcinoma | 14 (66.7) | Surgical treatment (8), SEMS |
| placement (6) Bismuth type 1 | 4 (28.6) | Surgical treatment (3), SEMS |
| placement (1) Bismuth type 2 | 5 (35.7) | Surgical treatment (3), SEMS |
| placement (2) Bismuth type 3 | 5 (35.7) | Surgical treatment (2), SEMS |
| placement (3)Carcinoma of the ampulla of Vater placement |
4 (19) | Surgical treatment (3), SEMS |
| (1)Carcinoma of head of the pancreas placement (1) | 3 (14.3) | Surgical treatment (2), SEMS |
Table 4: Features of the patients with cholangitis due to malignancy (n=21). SEMS: Self-expandable metallic stent.
There were 3 patients underwent to ENBD because of the iatrogenic type 2 (peri-Vaterian) perforation during ERCP procedure. All of them were healed with conservative treatment.
Cholangitis and intrahepatic abscess was diagnosed in one patient with Caroli disease. OLT was planned in this patient after the complete resolution of the cholangitis with ENBD and intravenous antibiotic administration.
Discussion
Endoscopic therapy for bile duct leaks after cholecystectomy is the gold standart method and superior to both reoperation and PTBD [5,6]. This estimation is true for also biliary anastomotic leaks after OLT. The regimens of therapeutic ERCP include ENBD or stent placement. EST alone for low-grade leak (leak identified only after intrahepatic opacification) and stent placement for high-grade leak (leak observed before intrahepatic opacification) has been recommended, however, performance of EST, in addition to ENBD or stent placement, is controversial in patients with high-grade leak [10]. On the other hand, another study revealed that ENBD or stent placement across the leak site is more effective than a short transpapillary biliary stent [11]. Thus, the most favorable endoscopic method for biliary leaks remains to be elucidated.
It has been stated that a well-placed ENBD tube may cure all biliary leaks [12]. Although a risk of nasobiliary tube removal by the patient exists in unconscious cases and nasobiliary tube is known to be uncomfortable, ENBD shortens the recovery period with the help of a higher bilioathmospheric gradient than bilioduodenal gradient [13]. In addition, it is possible to monitor the healing of the leak without a repeated ERCP. EST, if there is no contraindication, provides additional bilioduodenal gradient and accelerates the healing. In this study, ENBD with EST was successful to heal the postoperative biliary leaks in all patients. The most common site of biliary leak was found to be the cystic duct in LC patients, and anastomotic leak in OLT patients; these results were concordant with the literature [11,14,15].
Acute cholangitis may be life-threating; resulting mostly from choledocholithiasis, benign strictures, and malignant biliary obstructions. ENBD or stent placement is the choice of therapy in patients with stricture-induced cholangitis. On the other hand, in the case of the presence of choledocholithiasis-induced acute cholangitis, the goal is to extract the biliary stone(s), however, it is not always possible due to the size of the stone(s). In addition, poor patient status due to cholangitis may lead to the endoscopist to delay the stone(s) extraction procedure and to prefer to perform the placement of nasobiliary tube or stent. Thus, ENBD or stent placement may play a critical and life-saving role in these patients. However, there is controversy about the endoscopic therapeutic method for patients with cholangitis [8]. Two randomized controlled trial comparing ENBD and stent placement in patients with cholangitis showed no significant difference in success rate, effectiveness, or morbidity [16,17]. But many authors suggest that placement of nasobiliary tube vs. plastic stent depends on viscosity of the bile, and ENBD has to be preferred when there is pus in the bile [8]. In concordance to this suggestion, in our routine procedures of patients with clinically cholangitis, we observe the character of the bile after EST. If we see that the bile shows purulent character than we prefer ENBD instead of stent placement. Frequent lavage of the biliary tract via the nasobiliary tube is possible and usually prevents the tube obstruction. Previous experiences learned us that purulent bile may obstruct plastic stent in a few days after the procedure. Although it may be more preferable to use a 10-Fr nasobiliary tube in patients with cholangitis, 7-Fr nasobiliary tube was used in all patients bacause of the lack of 10-Fr nasobiliary tube in our region.
There are two reports of case-series studies which examined whether or not EST should be added to ENBD or stent placement; they revealed that there was no significant difference in the success rate and effectiveness of drainage between these two methods [18,19]. However, to our knowledge, no randomized controlled trial exist in the literature about this issue. On the other hand, although it is not evidence-based, many endoscopists prefer to perform EST in these patients [8]. In addition to the additive effect on the bilioduodenal gradient, EST may be useful as an alternative pathway for biliary drainage when ENBD or stent obstruction occurs. Thus, we believe that ENBD with EST plus intravenous administration of antibiotics may be the favorable therapeutic option in cases with cholangitis. In this study, ENBD tube placement with EST plus intravenous administration of antibiotics was life-saving, successful to treat the cholangitis and gave us chance to perform the subsequent definite treatments.
The limitations of the study include the following: the retrospective study might have resulted in unintentional bias; in addition, there exist a small number of patients in subgroups. On the other hand, we can claerly conclude that; (1) ENBD with EST is efficient and safe to treat the postoperative biliary leaks, (2) ENBD with EST plus intravenous administration of antibiotics is efficient and safe to treat the lifethreating cholangitis and gives chance to perform subsequent ERCP session or surgical treatment for the definite therapy.
References
- Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, et al. (1993) Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg 165: 9-14.
- Morelli J, Mulcahy HE, Willner IR, Baliga P, Chavin KD, et al. (2001) Endoscopic treatment of post-liver transplantation biliary leaks with stent placement across the leak site. Gastrointest Endosc 54: 471-475.
- Rerknimitr R, Sherman S, Fogel EL, Kalayci C, Lumeng L,et al. (2002) Biliary tract complications after orthotopic liver transplantation with choledochocholedo chostomy anastomosis: endoscopic findings and results of therapy. Gastrointest Endosc 55: 224-231.
- Morelli J, Mulcahy HE, Willner IR, Cunningham JT, Draganov P (2003) Long-term outcomes for patients with postliver transplant anastomotic biliary strictures treated by endoscopic stent placement. Gastrointest Endosc 58: 374-379.
- Wills VL, Jorgensen JO, Hunt DR (2000) Role of relaparoscopy in the management of minor bile leakage after laparoscopic cholecystectomy. Br J Surg 87: 176-180.
- Park JS, Kim MH, Lee SK, Seo DW, Lee SS, et al. (2003) Efficacy of endoscopic and percutaneous treatments for biliary complications after cadaveric and living donor liver transplantation. Gastrointest Endosc 57: 78-85.
- Liao JZ, Zhao Q, Qin H, Li RX,Hou W,et al. (2007) Endoscopic diagnosis and treatment of biliary leak in patients following liver transplantation: a prospective clinical study. Hepatobiliary Pancreat Dis Int 6: 29-33.
- Nagino M, Takada T, Kawarada Y, Nimura Y, Yamashita Y,et al. (2007) Methods and timing of biliary drainage for acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg 14: 68-77.
- Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F (2003) Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc 57: 156-159.
- Sandha GS, Bourke MJ, Haber GB, Kortan PP (2004) Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc 60: 567-574.
- Hwang S, Lee SG, Sung KB, Park KM, Kim KH, et al. (2006) Long-term incidence, risk factors, and management of biliary complications after adult living donor liver transplantation. Liver Transpl 12: 831-838.
- Bhattacharjya S, Puleston J, Davidson BR, Dooley JS (2003) Outcome of early endoscopic biliary drainage in the management of bile leaks after hepatic resection. Gastrointest Endosc 57: 526-530.
- Parlak E, Ciçek B, Dişibeyaz S, Kuran SO, Oğuz D, et al. (2005) Treatment of biliary leakages after cholecystectomy and importance of stricture development in the main bile duct injury. Turk J Gastroenterol 16: 21-28.
- Woods MS, Shellito JL, Santoscoy GS, Hagan RC, Kilgore WR, et al. (1994) Cystic duct leaks in laparoscopic cholecystectomy. Am J Surg 168: 560-563.
- Prat F, Pelletier G, Ponchon T, Fritsch J, Meduri B, et al. (1997) What role can endoscopy play in the management of biliary complications after laparoscopic cholecystectomy? Endoscopy 29: 341-348.
- Lee DW, Chan AC, Lam YH, Ng EK, Lau JY, et al. (2002) Biliary decompression by nasobiliary catheter or biliary stent in acute suppurative cholangitis: a prospective randomized trial. Gastrointest Endosc 56: 361-365.
- Sharma BC, Kumar R, Agarwal N, Sarin SK (2005) Endoscopic biliary drainage by nasobiliary drain or by stent placement in patients with acute cholangitis. Endoscopy 37: 439-443.
- Sugiyama M, Atomi Y (1998) The benefits of endoscopic nasobiliary drainage without sphincterotomy for acute cholangitis. Am J Gastroenterol 93: 2065-2068.
- Hui CK, Lai KC, Yuen MF, Ng M, Chan CK,et al. (2003) Does the addition of endoscopic sphincterotomy to stent insertion improve drainage of the bile duct in acute suppurative cholangitis. Gastrointest Endosc 58: 500–504.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14660
- [From(publication date):
specialissue-2015 - Apr 19, 2025] - Breakdown by view type
- HTML page views : 10119
- PDF downloads : 4541