Research Article Open Access
Efficacy of a Communication Skill Training Fostering Health Promotion in Primary Care: A Mixed Method Analysis
Stefan N1,2,3*, Ueli G2 and Margareta S3
1Institute of Primary Care, University of Zurich, Switzerland
2Swiss College of Primary Care Medicine, Bern, Switzerland
3Institute of Epidemiology, Biostatistics and Prevention, University of Zurich, Switzerland
- *Corresponding Author:
- Neuner-Jehle Stefan
MD, MPH, Institute of Primary Care
Pestalozzistrasse 24, CH-8091 Zurich, Switzerland
Tel: +41 44 255 98 55
Fax: +41 44 255 90 97
E-mail: stefan.neuner-jehle@usz.ch
Received date: Feb 13, 2016; Accepted date: Mar 28, 2016; Published date: April 20, 2016
Citation: Stefan N, Ueli G, Margareta S (2016) Efficacy of a Communication Skill Training Fostering Health Promotion in Primary Care: A Mixed Method Analysis. J Community Med Health 6:413. doi:10.4172/2161-0711.1000413
Copyright: © 2016 Stefan N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Health related behavior is an important determinant of chronic disease, with a high impact on public health. Thus, motivating and assisting people to change their unfavorable health behavior is a major challenge for health professionals. Patients increasingly seek more active participation in healthcare decisions. Thus, communication skills of general practitioners (GPs) are crucial for a successful health promotive counseling, and there is a need of sound competences in communication techniques among them.
Methods: We developed a training program using case vignettes and standardized patients (SPs) and evaluated its effectiveness among GPs and their patients at different levels using a validated evaluation model. Levels refer to a. acceptance and satisfaction; b. adoption of knowledge and skills; c. behavior change in regard to communication competence; d. impact on daily work with results in the targeted aim. Results: Participants' ratings in all levels were positive, between 3.9 and 5.0 on a 5- point Likert scale. Self-rated communication knowledge and skills improved significantly with ratings of 3.4 to 3.7 before and 4.2 to 4.5 after the training course (p < 0.01). Only the integration of the new role into daily work was not, or not yet, changed by the training, but the perceived communication competence and working quality of participating GPs improved.
Conclusion: Communication skills and competence, as well as patient-centeredness and empathy, are crucial for GPs for helping patients to change and sustain their health behavior. Within communication skill trainings for GPs fostering health promotive counseling, the SP method is a promising format of medical education at pre- and postgraduate level, with a potentially high impact on public health.
Keywords
Communication training; Medical education; Health promotion; Standardized patients; Primary healthcare; Prevention
Introduction
Health related behavior is an important determinant of chronic disease, with a high impact on public health. Thus, motivating and assisting people to change their unfavorable health behavior is a major challenge for health professionals. Growing evidence suggests that involving people in decision-making and taking responsibility is fostering their sense of self-determination, self-responsibility, and ownership, and has positive effects in terms of their motivation, satisfaction, adherence to an intervention, and even health outcomes [1,2]. Patients increasingly seek more active participation in healthcare decisions, though not all of them to the same degree [3]. Experts have called for a shift towards a meaningful dialogue between patients and physicians and shared decision making [4].
Communication skills of general practitioners (GPs) are crucial for successful health promotive counseling, as any behavior change is based on the motivation of the patient. Thus there is a need of sound competences in communication techniques and corresponding training programs. Traditional counseling is characterized by a more paternalistic style, delivering decision aids and brief advices, whereas modern techniques like motivational interviewing foster patients' activation and participation [5]. However, it is not yet clear in which settings and populations these elaborated communication techniques improve outcomes compared to more simple and brief approaches [3,6,7]. The change of role and modern communication techniques are beyond the traditional patterns of GPs’ training and professional work, and there is room for improvement in the pre- and postgraduate medical education in regard to communication training [8]. Besides that, there are multiple barriers to be considered towards the implementation of health promotive counseling in ambulatory primary care, such as low self-efficacy in regard to counseling skills, lack of time, and low reimbursement [9-11]. Our study provides further knowledge about the effects of a GP training program in modern communication techniques.
Methods and Materials
The aim of our study was to develop and to test a training program for GPs which intends to improve their communication skills, with special emphasis on techniques based on Motivational Interviewing.
Framework
The training program was embedded in a program for health promotion in primary health care practice called “Health Coaching”, delivered by a project team of the Swiss College of Primary Care Medicine. The concept and efficacy of this approach is described in detail elsewhere [12]: GPs are encouraged to assist patients in their motivation and efforts to change unhealthy behavior. At the beginning of a "Health Coaching" session, the goal is set by the patient, in the spirit of patient-centeredness and thus fostering the intrinsic motivation of patients: Beyond traditional patterns like prescribing drugs or treatments the GP is supporting patients' decision-making, planning and implementation activities, in the role of a coach. The study program was submitted to and approved by the local ethics committee (Canton St. Gallen, Switzerland). In the pilot study with 20 GPs and 1,045 patients we evaluated acceptance and feasibility using questionnaires and semi-structured interview techniques. The main outcomes were participation rates, the duration of counseling, patients’ self-rated behavioural change in their field of choice and ratings of motivational, conceptual, acceptance and feasibility issues. The results were excellent: Every second participant improved her or his behaviour in the area of choice by at least one (of two possible) categories [12]. Dissemination of the program is now ongoing in northern Switzerland.
Development of the training program
The change of roles and fostering patients' participation requires a special way of communication between GPs and patients. This communication style needs to be learned and rehearsed by GPs, as it is not a mandatory part of their professional education up to now. Thus we designed a training program which integrates mandatory elements as follows:
• Lectures and live-demonstrations by experienced communication teachers of up-to-date communication concepts and skills for behavioral changes, such as the transtheoretical model of behaviour change proposed by Prochaska and DiClemente [13], the Motivational Interviewing (MI) approach [14], Shared Decision Making [15], and Self-Management Support [16]
• Case vignettes with real-life situations taken from GPs’ daily office practice with the aim to facilitate implementation of the lessons learned in GPs' daily work
• Training sessions with standardized patients (SPs) experienced in MI and feedback-giving, presenting real-life situations based on the scripted vignettes. This method of SPs was first developed in the 1960s by Howard Barrows [17] and established in medical education in the mean time [18]. Their effectiveness in medical education has been reported in different settings and for various objectives [18,19]. While the SP technique is mainly established in medical examinations to guarantee equal conditions for candidates and to simulate a setting close to clinical reality [20], it is not yet as widely used for training purposes where the technique offers the unique opportunity for trainees to get immediate and repeated feedback on their performance from the SP.
Material: Scripts (case vignettes) for SPs and GPs
SPs were trained in collaboration with the communications training division of the University of Applied Health Sciences Bern/Switzerland. All of them were professional actors and had had thorough training as standardized patients. For our program they learned - in an interactive training session with the study team - to portray a patient with several unfavorable behaviors like physical inactivity, tobacco smoking, overuse of alcohol and more. The case vignettes were developed by the study team in the spirit of consensus and based on the clinical experience of the team members. Table 1 gives an example of a typical patient's and GPs case vignette script. The actors were trained to leave their role after the interview and to give feedbacks in detail about what they experienced during the interview with the GP, in terms of understanding as well as in terms of emotional response to the communication provided by the GP. This immediate feedback from actors enabled participants to perceive how different communicative approaches may affect patients, and it allowed to repeat, rehearse and practice pertinent skills.
| SPs' script (*): Mrs. Miller Present situation: Mrs. Miller had an acute coronary syndrome (ACS) one month ago and was treated with coronary stenting. She is a heavy smoker and was advised to quit. Age: 53 Profession: CEO's secretary of a big lawers' company. High workload, high esteem by her employer. Social situation: Single, no family. Intercurrent relationships but no engagement. Some friends who mostly have own families. Not very much spare time for leisure. Close relationship to a niece who sometimes stays at her flat. She wears moderately elegant clothes. Family history: Her father died in his fifties of a heart attack. Her brother had suffered (and survived) a heart attack in his fifties as well. Most family members are overweight. Eating and drinking habits: rather fast food type of eating, she does not take much time for cooking and eating, neither on the job or at home. Regularly drinking red wine, moderate quantities. Smoking habits: She started smoking at 18 years of age, 10 cigarettes a day. In between up to 30/d. Physical activity: She used to play tennis until some years ago, when her tennis partner moved abroad. She did not have the time to look for a new one. Leisure activities: She likes spending evenings in concert or theatre halls. Sometimes city trips. Drugs: Aspirin cardio 100mg/d and Pravastatin 20mg/d which she does not always take. Ideas, concerns, expectations: She knows the association between smoking, physical activity, eating behavior, stress and coronary heart disease. Generally, she is satisfied with her present situation in life, but she fears that she could suffer a heart attack as her relatives did. She does not like the thought that this could be her fate, she would prefer to have more influence herself on what will happen to her. This is, in her awareness, how she lives: like a self-made woman. She agrees to discuss about physical activity and other lifestyle issues, but to quit smoking is not her first intention right now. But, yes, she also thinks that she might have to change something in her life. |
| b. GPs' script: Mrs. Miller You don't know the patient yet, as you sit in for a colleague who normally cares for her. You got a medical report from hospital about the ACS and stenting, and the suggestion to go on with the drugs and to continue quit smoking support, as started in hospital. |
| *The actor should answer to GPs' questions and also provide some informations spontaneously. Besides portraying this personality the actor should perceive how the GP does organize the interview and what emotions his/her questions and remarks are triggering in regard to motivation. Finally, the actor is feeding back his perceptions to the GP. |
Table 1: Typical script of a case vignette for standardized patients (a) and information provided for the participant / GP (b).
Intervention: The training courses
The pilot sequence of training courses for GPs during 2011 consisted of two modules of 1.5 days duration each, with a time distance of four months in between. We chose this duration in order to guarantee a sufficient time for knowledge and skill transfer and provide multiple occasions to exercise for each participant. The four months intervall between modules allowed participants to apply the acquired knowledge and skills repeatedly while working with their patients.
Teaching was provided by certified motivational interviewing trainers with personal experience in their own primary care practice. In order to allow for a maximum of role play and interaction, the training courses were conducted in two parallel groups of 10 GPs each.
In the subsequent dissemination phase (2012–2015) we trained another 48 GPs in four courses (11 to 13 GPs per course) of 1.5 days duration each but consisting of only one module compared to two in the pilot phase.
This reduction from two modules to one was chosen in order to improve acceptance among GPs in favor of a successful dissemination strategy, as proposed by participants of the pilot phase in the group interviews.
The basic structure of our training courses of 1.5 days duration was as follows:
• A theory section (2 hrs) explaining the underlying models and concepts with room for discussion.
• Four sequences of 1.5 to 2 hours each for practical training, according to the four steps of counseling as suggested by our program's approach [12], i.e., "sensitize", “promote motivation”, “prepare an action plan” and “assist and evaluate”. Each of these counseling steps was – after a short introduction and demonstration – practiced by role play between each participant and the SP, with structured feedback by SP and MI-teacher, plus open discussion.
• Two sequences of 1-2 hrs each (at the end of the first day and of the second day) were dedicated to inputs and discussions on how to transfer the acquired knowledge, skills and attitude (e.g., role change) into one’s own daily practice.
Evaluation methods
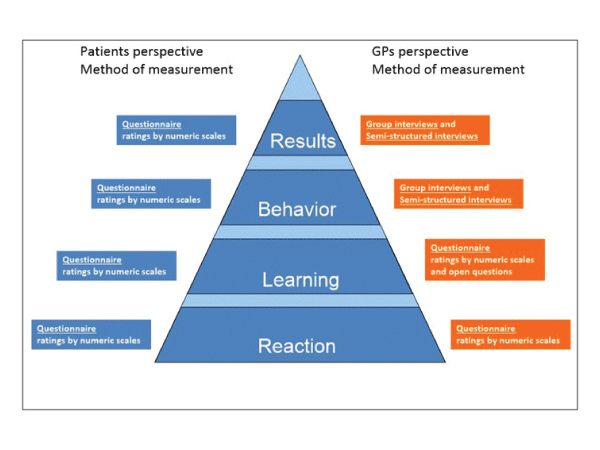
Corresponding with the different levels of aims of our training program, we used the four-level evaluation model of Kirkpatrick and Kirkpatrick [21] to evaluate the training program (Figure 1). The different levels translate into outcomes as follows: level 1: acceptance and satisfaction; level 2: adoption of knowledge and skills; level 3: behavior change in regard to communication competence; level 4: impact on daily work with results in the targeted aim.
Figure 1: Measurement in regard to the evaluation model levels, adapted from Kirkpatrick and Kirkpatrick [21]. This model describes a stepwise process of how knowledge and skills are adopted by trainees, from a basic level (first reaction) to more advanced levels (achanged behavior resulting in an impact). These levels can be used in the evaluation of an intervention: A higher level in the pyramid translates into a better success of the intervention in regard to the ultimate aim of changing patients' health.
We applied the model to the participating GPs (direct target group) as well as to patients (ultimate target group) in order to evaluate the effects of our intervention (Table 2).
| Steps in the "Health coaching" program, GP perspective | Steps in the "Health coaching" program, patient perspective | Level in the evaluation model | Method of measurement | |
|---|---|---|---|---|
| 1 | Interest in the topic, willingness to join the training program | Sensitization | Reaction: Acceptance and satisfaction of GPs of the intervention (training) as important base for adoption | Questionnaires with ratings by numeric scales Specific questions: inTable 3 |
| 2 | Increase of communication skills by the training course | Increase of knowledge in regard to the own health | Learning: Increase in knowledge and adoption of new skills (or increase in existing skills). Have learning objectives been reached? | Questionnaire with ratings by numeric scales and open (qualitative) questions Specific questions: inTable 4 |
| 3 | Change of attitude and increase in communication competence | Change in motivation and health competence | Behavior change: Application of new competences by participants and transfer in their practice | Group interviews Semi-structured interviews as provided in the quotes |
| 4 | Implementation of new communication style in practice work | Behavior change | Results: Measurable changes in target outcomes in GP's work or patient's life | Group interviews Semi-structured interviews as provided in the quotes |
Table 2: Objectives, evaluation levels (adapted from Kirkpatrick and Kirkpatrick [21]), and corresponding measurements in the pilot training course.
Measurement of the outcomes on these different levels was performed by quantitative and qualitative methods - questionnaires with rating scales and open questions, group interviews, semistructured individual interviews - and at different time points (Table 2 and Figure 1).
After the end of the pilot phase we conducted another four courses for another 48 GPs. Based on the pilot experience and due to time constraints of participants, the duration of these courses was shortened to 1.5 days in a single module (in contrast to the pilot phase courses with two modules of 1.5 days duration each); the basic course structure and content (as described above) remained the same.
This allowed us to compare the answers of both GP cohorts regarding the longer and shorter format. The purpose of this ongoing evaluation was rather a formative evaluation plan (to adapt training techniques if necessary) than an explorative approach as in the pilot setting.
Data sampling and data analysis
GPs were recruited by postal or e-mail invitation delivered by the regional physicians' societies to all their members as well as by personal contacts during Continuous Medical Education sessions. In the pilot study participating GPs carried out the program with their patients during 12 months. Quantitative and qualitative data of the courses, e.g., monthly records of the GPs perceptions or records about individual need of GPs for support were collected continuously by study team members at the GPs' offices (visits, questionnaires, individual interviews) and at the training courses (group interview, questionnaires). We pilot-tested the questionnaires in five practices in order to test feasibility and acceptance.
The group interview took place after the second module of the pilot course training, and focussed on barriers, solutions and potential support needed. On the basis of these results the guide for the semistructured interviews with the GPs at the end of the pilot phase was constructed. All interviews were conducted by the same researcher, the group interview with the presence of another two researchers out of the study team.
Data were extracted from questionnaires and analyzed by SPSS Statistical Software Package, Version 19 (IBM SPSS Inc., Chicago IL) by a single study team member. For each item we calculated frequencies, means and standard deviations (SD). For items repeatedly measured we calculated differencies between means by nonparametric tests (Wilcoxon t-test) for dependent groups (in case of two subsequent modules, same participants) or for independent groups (in case of independent courses, different participants).
For level 2 and 3 items we calculated Cronbach's Alpha to test reliability of item discrimination. For the qualitative data analysis the group interviews and the individual interviews were recorded digitally and transcribed verbatim. The transcripts were analysed on the base of Mayring´s quality content analysis method [22] by one researcher. Based on the interview guides, a category system was elaborated.
After the coding procedure, a synthesis of all important findings was compiled in discussions with the research team. The data material resulting from these discussions served as a basis for interpretation and formative evaluation of the training courses.
Results
a. Results of the pilot training course (2011)
21 out of 348 GPs (8.5%) were willing to join the study. Finally 20 GPs agreed to participate, and 18 practices provided a complete data set after the 12 months study period. Baseline characteristics and results of the trial in regard to patients' outcomes are published in extent elsewhere [12].
Evaluation level 1: Acceptance and satisfaction:
Acceptance of and satisfaction with the training courses were consistently high, with means of 4.4 to 5.0 on a 5-point Likert scale (Table 3). The SP method was rated high in both modules (4.8 and 4.9), similar to the ratings of the case vignettes' quality (4.7 and 4.8). Time available for the skill training in the course was rated high in module 2 (4.8) and somewhat lower in module 1 (4.1). In the qualitative part of the study GPs pointed out that rehearsing and reflecting one’s own awareness was most important to them, rather than listening and understanding the information provided.
| Item | Mean Module 1 | SD | Mean Module 2 | SD |
|---|---|---|---|---|
| Clear goal setting | 4.4 | 0.7 | 4.9 | 0.3 |
| Good structure and didactics of the course | 4.7 | 0.5 | 4.9 | 0.2 |
| Enough time available | 4.1 | 1.0 | 4.8 | 0.4 |
| Topics matching to the daily work | 4.7 | 0.5 | 4.9 | 0.3 |
| Feedback by moderators after interviews useful | 4.9 | 0.4 | 4.9 | 0.3 |
| Enough occasion to participate actively | 4.8 | 0.4 | 4.9 | 0.2 |
| Use of SP for the personal gain in skills | 4.8 | 0.5 | 4.9 | 0.2 |
| Case vignettes well applicable to daily work | 4.7 | 0.7 | 4.8 | 0.4 |
| Good knowledge of moderators | 5.0 | 0.0 | ||
| Good instruction for the exercises | 4.7 | 0.6 | ||
| Discussions on change of role useful | 4.0 | 0.8 | ||
| Hints for time managementin the coaching process useful | 4.2 | 0.8 | ||
| Theoretical input useful for the implemention of motivational interviewing | 4.5 | 0.7 | ||
| Could integrate my own experience into discussions | 4.9 | 0.2 | ||
| Course helpfulto analyze own experience | 4.6 | 0.8 | ||
| Counseling technique helpfulfor tricky situations | 4.6 | 0.5 | ||
| Tricky situations adressed | 4.5 | 0.6 | ||
| Role as a coach sufficiently discussed | 4.6 | 0.7 |
Table 3: Ratings of Level 1 (acceptance and satisfaction) evaluation items in the pilot training course (n=18) which consisted of two modules of 1.5 days duration each, with a delay of four months from module 1 to module 2. Values refer to a 5-point Likert scale (from 1 = "I do not agree at all" to 5 = "I totally agree").
They perceived the change of role and time management in consultations as the most challenging points in their work with patients. GPs perceived that work started to be more interesting again, that patients were mostly open and interested in joining the program, and that patient-doctor relationships became closer.
Evaluation level 2 and 3: Knowledge/Skills and communication competence:
Adoption of knowledge and skills and increase in communication competence were rated similarly high, with means of 3.9 to 4.7 on a 5- point Likert scale (Table 4). The self-rated competence for the first step of counseling significantly increased between baseline and after module 1 (p < 0.05), similarly to the competence to coach patients (p < 0.01) and to perceived communication skills (p < 0.01) without further improvement after module 2.
| Item | Mean Baseline* | SD | Mean module 1 | SD | Mean module 2 | SD |
|---|---|---|---|---|---|---|
| I manage to ask and sensitize the patient (competence for the first step of counseling) | 3.7 | 0.8 | 4.2 | 0.5 | ||
| I succeed in integrating my new role in counseling | 4.0 | 0.7 | 4.2 | 0.7 | ||
| I feel sure enough to implement the tools in my work | 3.9 | 1.0 | 4.6 | 0.6 | ||
| I manage to coach patients in planning and working out a concrete change of behavior (competence to coach patients) | 3.4 | 0.8 | 4.2 | 0.5 | 4.1 | 0.5 |
| My skills in interview technique, counseling and coaching have improved (communication skills) | 3.6 | 0.7 | 4.5 | 0.5 | 4.7 | 0.5 |
| *Baseline data were measured at a self-assessment session one month before training courses | ||||||
Table 4: Ratings of level 2 (knowledge and skills) evaluation items in the pilot training course (n=18) which consisted of two modules of 1.5 days duration each, with a delay of four months from module 1 to module 2. Values refer to a 5-point Likert scale (from 1 = "I do not agree at all" to 5 = "I totally agree").
The self-rated competence for the first step of counseling significantly increased between baseline and after module 1 (p < 0.05), similarly to the competence to coach patients (p < 0.01) and to perceived communication skills (p < 0.01) without further improvement after module 2.
The implementation of the new role into daily work was rated similar after module 1 and module 2 (4.0 and 4.2, respectively, p = 0.48). Reliability between items in this level 2 and level 3 section was sound, with a Cronbach's Alpha of 0.7 to 0.8 (data not shown in detail).
GPs' comments on their own behavior change in their communication with patients reflect that this is not easy-going:
"Listening, and especially listening actively is difficult. By listening actively a change process in the patient can be started."
Evaluation level 4: Impact on daily work
The impact on the daily work by the communication training is more difficult to measure. Our study was not designed to measure clinical outcomes as a result of patients' behavior change.
However, some quantitative and qualitative results give us hints on effects of the training at this level: GPs recognized that communication skills would be an advantage for their practice work in general (not restricted to counseling) (mean 4.6 after module 1 and 4.5 after module 2, SD 0.6). GPs perceived an improvement in their communication and interview competence:
"My competences in talking with patients increased: I am sure that my communication is of a better quality."
Quite unexpectedly many GPs reported important improvements in professional wellbeing:
"Working this way may well be the best prophylaxis against professional burn-out.”
b. Results of the subsequent training courses (2012–2015)
The majority of items tested in these training courses related to the levels 1 and 2 of our evaluation model: The satisfaction, acceptance and knowledge / skill transfer items were rated rather high (3.9 to 4.9 on a 5-point Likert scale) throughout the four one-module courses (Table 5).
| Item | Mean | SD |
|---|---|---|
| Clear goal setting | 4.3 | 0.9 |
| Good structure and didactics of the course | 4.3 | 0.7 |
| Enough time available | 3.9 | 0.8 |
| Topics matching to the daily work | 4.5 | 0.5 |
| Good knowledge of moderators | 4.8 | 0.4 |
| Good instruction for the exercises | 4.3 | 0.7 |
| Feedback by moderators after interviews useful | 4.7 | 0.6 |
| Enough occasion to discuss | 4.5 | 0.7 |
| Enough occasion to participate actively | 4.5 | 0.8 |
| SP’s performance close to reality | 4.8 | 0.4 |
| Use of SP for the personal gain in skills | 4.9 | 0.4 |
| Case vignettes well applicable to daily work | 4.6 | 0.5 |
| Information material to the course sufficient | 4.1 | 0.9 |
Table 5: Ratings of different evaluation level items in the subsequent courses (n=48) which consisted of one module of 1.5 days duration. Values refer to a 5-point Likert scale (from 1 = "I do not agree at all" to 5 = "I totally agree").
Again, in line with the pilot test result, the ratings for SP performance and usefulness of the SP training sessions were among the highest (4.8 and 4.9, SD 0.4), whereas the time available for rehearsing with SPs was rated lower (3.9, SD 0.8). There were only minor differences in the ratings between courses (data not shown).
Discussio
Knowledge and skill transfer by traditional ex cathedra teaching is not very effective in regard to adoption of skills and competence [23]. This is especially true for communication training because it has to address much more the behavioral and attitudinal dimensions than a purely cognitive one [24,25]. Sufficient mastery of these skills and competence by physicians is crucial for positive effects of communication and counseling in the ultimate target group (i.e., patients).
In our study, we tested and evaluated our program “Health Coaching” focussing on enabling GPs to support patients on their way towards behavior change. We could show that the GPs’ communicative skills and competences increased substantially by a specific training. These results are in line with recent literature in regard to the impact of MI-based communication training for GPs [26]. The training module consisted of short lectures, in-depth one-on-one practice sessions with standardized patients and group discussions on transfer of skills, competences and attitudes into participants’ professional practice. According to the participants’ feedback, their favorite method were the training sessions with SPs who were experienced in MI techniques and providing feedback. This method has various advantages:
a. It provides an immediate feedback to participants about how their communication was perceived;
b. It offers a "safe" setting for the participant for testing various communication approaches, without the risk of harming patients or exposing themselves;
c. It provides the opportunity of repeatedly rehearsing various interview styles and comparing its effects, supplemented and enhanced by watching their peers ("vicarious learning") [11,27].
We doubt that less time-consuming training formats like short courses (of one hour or similarly short sessions) would achieve similar effects, as a change of (communicative) behavior is not only challenging for our patients, but also for ourselves as clinicians.
The main reason is that any change requires time. This also applies to changing communication techniques and adopting new ones, because it requires considerable attitudinal and skills changes as well as the opportunity to repeatedly experience the reactions of patients. Nevertheless, short lectures or skills labs (for example during medical congresses) offer an unique occasion to sensitize colleagues for the issues of counseling, communication and health promotion and are useful to awaken and foster their interest in further training.
The 4-level evaluation model of Kirkpatrick and Kirkpatrick [21] is specially valuable for our purpose as it reflects the hierarchy in goals and outcomes of our intervention: The ultimate goal is that GPs change their communicative behavior in their clinical work, and this is of clearly higher value compared to the acceptance of a method or understanding concepts. Nevertheless, all the steps of "lower" levels are necessarily required to achieve the final aim, and thus they are of similar interest as the level 4 outcomes.
An additional possibility of information and skill transfer is onlineteaching via websites or apps. Some few options exist already, and we are currently developing an own online teaching format for our website (www.gesundheitscoaching-khm.ch). As mentioned above we think that these formats do not replace face-to-face training courses, but can serve as appetizers and sensitizers for future course participants, and they offer support for their learning and practicing [28].
Last but not least, communication training is of utmost importance for undergraduate and graduate physicians [29]. It is here were the groundwork for professional communication is laid. In the last decade many efforts in this direction have taken place at Swiss medical faculties [19,30] but there still is considerable room for improvement [31,32].
Finally, in the light of decreasing numbers of GPs it is crucial to invite medical practice assistants and practice nurses to join training courses and to implement counseling in collaboration with the GP and under his/her responsibility [33,34]. In our program “Health coaching” we recently started this initiative.
These professions may benefit from the training which will support them in their central function in medical office practices, i.e., manage key points like admission and leading the patient through the practice visit, as well as continuous patients' support.
Strengths
It is a strength of our study that we used a comprehensive and validated model of evaluation at various levels with multiple measurements. The levels of this model are in line with the steps of our counseling approach, from sensitization to knowledge transfer and a gain in skills and competence, which made the ratings more intuitive and accurate for participants in our opinion.
Another strength is the pre-post analysis of key items which allowed us to quantify the presumed effect of the standardized patient technique on participants' communication skills. The use of a mixedmethods evaluation technique to assess effects, acceptance and feasibility of our intervention is essential for exploring attitudes, barriers and facilitators of our innovative approach among GPs. Techniques restricted to either quantitative or qualitative methods would not allow such a variety of results and conclusions.
We did not restrict our outcomes to GPs' perceptions and behaviors but measured a variety of patients' outcomes as well and reported the results elsewhere [12]. As these outcomes are modified by many covariates it was not possible to use them for investigating the effect of the communication training. This has been the reason to evaluate the training with a set of indicators as described above.
Limitations
A weakness of the study is the relative small number of participants in the pilot trial; but this weakness was neutralized to some extent by investigating substantially more participants in the subsequent courses. Another weakness in regard to generalizability is the fact that our measurements were restricted to self-ratings and that we did not evaluate communication skills by third party raters, video-assisted objective analysis or questionnaires to elicit knowledge, nor formal long-term follow-up. Finally the probability of selection bias in participants' recruitment is considerable, as GPs attending our training courses might have a higher intrinsic motivation to deal with communication topics than their non-attending colleagues.
Conclusion
Our intention was to develop and to test a training program for GPs which improves their communication skills and competence, which are crucial for GPs for helping patients to change and sustain their health behavior, as well as patient-centeredness and empathy. Our findings support the SP training method as a promising format of medical education at pre- and postgraduate level, with a potentially high impact on public health.
Authors’ Contributions
UG, SNJ, and MS developed the concept and designed the feasibility and acceptance study including the skill training program. MS conceived the evaluation process, carried out the data collection, and performed the statistical analysis. SNJ drafted the manuscript. All authors contributed to the writing of the manuscript, and all authors read and approved the final manuscript.
Conflict of Interest Disclosure
The study was financed by the Swiss College of Primary Care Physicians, the Federal Authority of Public Health and a pool of cosponsors, within the "Health Coaching" Project. Sponsors had no influence on study results, reporting nor publication policy.
Acknowledgements
Special thanks go to the Communications Training Division of the University of Applied Health Sciences Berne (training of SP), to the Medical Association of the Canton of St. Gallen and to the pool of sponsors for the underlying pilot study “Swiss Health Coaching”. Last but not least we thank the primary care physicians and their patients who took part in the pilot study.
References
- Van Steenkiste B, van der Weijden T, Stoffers HE, Kester AD, Timmermans DR, et al. (2007) Improving cardiovascular risk management: a randomized controlled trial on the effect of a decision support tool for patients and physicians. Eur J CardiovascPrevRehabil 14: 44-50.
- O’Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas H, Rovner D, et al. (2009) Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev CD001431.
- Levinson W, Kao A, Kuby A, Thisted R (2005) Not all patients want to participate in decision making. A National Study of Public Preferences. J Gen Intern Med 20: 531-535.
- Politi MC, Han PKJ, Col NF (2007) Communicating the uncertainty of harms and benefits of medical interventions. Med Decis Making 27: 681-695.
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL (2010) A meta-analysis of motivational interviewing: twenty-five years of empirical studies. Res Soc Work Pract 20: 137-160
- Catley D, Goggin K, Harris K (2015) A Randomized Trial of Motivational Interviewing: Cessation Induction Among Smokers With Low Desire to Quit. Am J Prev Med.
- Lindson-Hawley N, Thompson TP, Begh R. (2015) Motivational Interviewing for smoking cessation (Review). Cochrane Database Syst Rev 3: CD006936.
- Aspegren K (1999) BEME Guide no. 2: Teaching and learning communication skills in medicine - a review with quality grading of articles. Med Teach 21: 563-657.
- Geense WW, van de Glind IM, Visscher TLS, von Achterberg T (2013) Barriers, facilitators and attitudes influencing health promotion activities in general practice: an explorative pilot study. BMC FamPract 14: 20.
- Jacobsen ET, Rasmussen SR, Christensen M, Engberg M, Lauritzen T (2005) Perspectives on lifestyle intervention: the views of general practitioners who have taken part in a health promotion study. Scand J Public Health 33: 4-10.
- Lambe B, Collins C (2010) A qualitative study of lifestyle counseling in general practice in Ireland. FamPract 27: 219-223.
- Neuner-Jehle S, Schmid M, Grüninger U (2013) The “Health Coaching” programme: a new patient-centred and visually supported approach for health behaviour change in primary care. BMC FamPract 14: 100.
- Prochaska JO, DiClemente CC (1986) Towards a comprehensive model of change: Treating addictive behaviors. New York: Plenum Press, Newyork.
- Miller WR, Rollnick S (2002) Motivational Interviewing. Preparing People for Change. London: The Guilford Press, Newyork.
- Elwyn G, Dehlendorf C, Epstein RM (2014) Shared Decision Making and Motivational Interviewing: Achieving Patient-Centered Care Across the Spectrum of Health Care Problems. Ann Fam Med 12: 270-275.
- Packer TL, Boldy D, Ghahari S (2012) Self-management programs conducted within a practice setting: Who participates, who benefits and what can be learned?Pat EducCouns 87: 93-100.
- Barrows H (1993) An overview of the uses of standardized patients for teaching and evaluating clinical skills. Acad Med 68: 443-453.
- Kurtz SM, Silverman J, Draper J (2005) Simulated patients. In: Teaching and Learning Communication Skills in Medicine. Radcliffe Publishing.
- Humair JP, Cornuz JA (2003) New curriculum using active learning methods and standardized patients to train residents in smoking cessation. J Gen Intern Med 18: 1023-1027.
- Stillman P, Swanson D, Regan MB, Philbin MM, Nelson V, et al. (1991). Assessment of clinical skills of residents utilizing standardized patients. A follow-up study and recommendations for application. Ann Intern Med 114: 393-401.
- Kirkpatrick JD, Kirkpatrick DL (2006) Evaluating Training Programs. The Four Levels. (3rd edn.) San Francisco: BerrettKoehler, San Francisco.
- Mayring P (2000) Qualitative Content Analysis. Forum: Qualitative Social Research 1.
- Davis DA, Thomson MA, Oxman AD, Haynes RB (1995) Changing physician performance. A systematic review of the effect of continuing medical eduation strategies. JAMA 274: 700-705.
- Davis D, O'Brien MA, Freemantle N, Wolf FM, Mazmanian P, et al.(1999) Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA 282: 867-874.
- Helitzer DL, LaNoue W, de Hernandez BUB, Warner T, Roter D (2011) A randomized controlled trial of communication training with primary care providers to improve patient-centeredness and health risk communication. Pat EducCouns82: 21-29.
- Söderlund LL, Madson MB, Rubak S, Nilsen P (2011) A systematic review of motivational interviewing training for general health care practitioners. Pat EducCouns 84: 16-26.
- Craig SD, Driscoll D, Gholson B (2004) Constructing knowledge from dialog in an intelligent tutoring system: Interactive learning, vicarious learning, and pedagogical agents.J Educ Multimedia Hypermedia 13: 163-183.
- Lanken PN, Novack DH, Daetwyler C, Gallop R, Landis J, et al. (2015) Efficacy of an Internet-Based Learning Module and Small-Group Debriefing on Trainees’ Attitudes and Communication Skills Toward Patients With Substance Use Disorders: Results of a Cluster Randomized Controlled Trial. Acad Medicine 90: 345-354.
- Wagenschutz H, Ross P, Purkiss J, Yang J, Middlemas S, et al. (2011) Standardized Patient Instructor (SPI) interactions are a viable way to teach medical students about health behavior counseling. Pat EducCouns 84: 271-274.
- Daeppen JB, Fortini C, Bertholet N, Bonvin R, Berney A, et al. (2012) Training medical students to conduct motivational interviewing: A randomized controlled trial. Pat EducCouns 87: 313-318.
- Badertscher N, Rossi P, Rieder A, Herter-Clavel C, Rosemann T, et al. (2012) Attitudes, barriers and facilitators for health promotion in the elderly in primary care. Swiss Med Wkly 142: w13606.
- Junod PN, Sommer J, Louis-Simonet M, Nendaz M (2015) Teaching communication skills: beyond wishful thinking. Swiss Med Wkly 145: w14064.
- Taylor CA, Shaw RL, Dale J, French D (2011) Enhancing delivery of health behaviour change interventions in primary care: A meta-synthesis of views and experiences of primary care nurses. Pat EducCouns 85: 315-322.
- Manca DP, Greiver M, Carroll JC, Salvalaggio G, Cave A, et al. (2014) Finding a BETTER way: A qualitative study exploring the prevention practitioner intervention to improve chronic disease prevention and screening in family practice. BMC FamPract 15: 66.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 12612
- [From(publication date):
April-2016 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 11713
- PDF downloads : 899