Effects of Whole-Body EMS on Post-ACL Reconstruction General Conditioning - A Retrospective Comparative Study
Received: 13-Dec-2020 / Accepted Date: 18-Jan-2021 / Published Date: 25-Jan-2021 DOI: 10.4172/2165-7025.1000448
Abstract
Background: Electrical muscle stimulation OR Electromyostimulation has long been used in the field of medicine and sports. Most commonly, Electromyostimulation is used to elicit skeletal muscle contraction which has been effectively employed in circumstances such as prevention of muscular atrophy and muscle strengthening. Recently, whole body-EMS has been introduced as a technology that enables the simultaneous muscle activation of up to 16 regions with different dedicated intensities per region. The aim of the present study is to determine the effect of WBEMS on preventing general deconditioning including improving body composition and lower limb muscle recruitment on post Anterior Cruciate Ligament Reconstruction patients compared to conventional rehabilitation exercises alone. Design: Retrospective, comparative study. Methods: 17 post- Anterior Cruciate Ligament Reconstruction patients’ data were retrieved from their medical records. Patients who had done their rehabilitation with Whole-Body Electromyostimulation were allocated under WholeBody Electromyostimulation while those without were allocated under conventional group. Both groups underwent 6 weeks of a similar rehabilitation program with the WBEMS group having WBEMS superimposed to their exercises 3 times in every two weeks. Data including skeletal muscle mass, body fat mass, bilateral thigh lean mass (Affected Side Thigh Lean Mass & Non-Affected Side Thigh Lean Mass) and quadriceps muscle maximum recruitment (Electromyography) were extracted, compared and analyzed. Results: Both groups experienced Skeletal Muscle Mass and Body Fat Mass gain as well as muscle wasting on affected lower limb, differences between pre- and post-intervention for both groups as well as intergroup differences between Whole-Body Electromyostimulation and conventional group remained non-significant. With regards to Electromyography, both groups shown significant improvement over 6 weeks with Whole-Body Electromyostimulation group demonstrated significantly better improvement (p=0.047) with large effect size (Effect Size=1.044). Conclusion: Our study demonstrated that superimposing WBEMS with post- Anterior Cruciate Ligament Reconstruction rehabilitation for as short as 6 weeks, has beneficial impact on improving operated side quadriceps maximum recruitment, an important factor in preventing quadriceps muscle wasting at early stage of rehabilitation. There were no significant findings on the effect of Whole-Body Electromyostimulation on body composition.
Keywords: Electrical stimulation therapy; ACL reconstruction; Physical conditioning; Body composition; Neuromuscular manifestations
Abbreviation
EMS: Electrical Muscle Stimulation OR Electromyostimulation; WBEMS: Whole-Body Electromyostimulation; ACL: Anterior Cruciate Ligament; ACLR: ACL reconstruction; CONV: Conventional Group; SMM: Skeletal Muscle Mass; BFM: Body Fat Mass; ATLM: Affected Side Thigh Lean Mass; NTLM: Non-Affected Side Thigh Lean Mass; EMG: Electromyography; ES: Effect Size; QAF: Quadriceps Activation Failure; HIT: High Intensity Training; HAL: High Activity Level; LAL: Low Activity Level; POD: Post-Operation Day and JPEC: Joint Penang Independent Ethics Committee.
Introduction
Electromyostimulation has long been used in the field of medicine and sports. The benefits of its usage are well established through a wide range of research. Most commonly, EMS is used to elicit skeletal muscle contraction which has been effectively employed in circumstances such as prevention of muscle atrophy [1] and muscle strengthening [2].
The maintenance and promotion of skeletal muscle mass and strength is vital for functional movement [3]. Restoring muscle strength for instance in the quadriceps following ACLR is an essential aspect of rehabilitation. Despite the improvement made towards ACLR rehabilitation protocols, patients often return to activity with diminished quadriceps strength [4]. Prolonged weakness of the quadriceps has been linked to reduction of physical function [5,6] and quality of life [7] as well as increase in the risk of re-injury [8,6] which may lead to the development of post-traumatic osteoarthritis [9]. Owing to the fact that failure to restore quadriceps strength has deleterious effects to the knee, it is of utmost important that the rehabilitative approaches being capable of maximizing quadriceps strength deficits following ACLR.
Quadriceps activation failure has been identified as a contributor to prolonged strength deficits post-ACLR [4]. The neural signaling changes in QAF, reduce alpha motorneuron recruitment or firing rate, allows only a portion of the quadriceps to be utilized during exercise [10]. Clinically, in the rehabilitation field, QAF reveals itself as quadriceps weakness [11]. Although QAF is thought to be a natural mechanism designed to protect the knee joint from further injury [10], persistent QAF hinders complete muscles activation during strength training and prevents successful rehabilitation [12,13].
One way to improve or promote muscular strength and mass is through high load exercises. Owing to physical limitation as well as restriction against a wide range of regular exercises, the majority of post-ACLR patients are not able to perform these exercises recommended which will impact strength or muscle mass gains. This leads to muscle wasting which occurs as early as the first several days after surgery [14]. Besides the injured side quadriceps muscle atrophy, a growing number of papers have also demonstrated deterioration of contralateral uninjured side quadriceps deficiency following ACL injury or reconstruction [15,16]. In addition, for athletes or individuals who live an active lifestyle prior to injury, they will likely encounter a general deconditioning post-surgery due to a reduction in physical activity. Thus, the primary focus of ACLR rehabilitation protocols should include preserving and improving the strength of the lower limbs while preventing general deconditioning.
Recently, whole-body EMS has been introduced as a technology that enables the simultaneous muscle activation of up to 16 regions with different dedicated intensities per region. It is a time effective training technology that focuses primarily on body composition (i.e. muscle, bone, fat tissue) and strength-related parameters. Compared to the conventional local EMS, which has to be wire-connected to the control panel, allowing only basic exercises such as isometric exercises or static positional exercises, this wireless WBEMS allows total freedom of movement, permitting a more functional and sport-like exercises which requires total degree of movement such as jumping and running. Coupled with the electrode pad covering all major muscle groups, it allows simultaneous full body muscle stimulation instead of single region which makes it suitable for general conditioning purposes.
Studies done on WBEMS training applied for 18 minutes per session, on three occasions within 14 days over 12 months, had a beneficial impact on muscle mass and abdominal body fat in a cohort of normal weight to underweight non-sportive elderly females [17]. Furthermore, a short-term research article comparing WBEMS and High Intensity (Resistance) Training (WBEMS: 1.5x20 vs. HIT: 2x30 min/week) has shown that both methods were similarly effective in improving body composition and muscle strength [18]. One of the advantages of WBEMS is that it allows muscle strengthening without excessive joint loading as compared to conventional strength exercise which often requires utilization of external weights. WBEMS may be a good choice for post-ACLR patients who are unable to participate in intense resistance training protocols which may produce excessive joint loading and shearing forces to the graft. For these individuals, WBEMS may overcome some of the limitations of conventional strength training and may be a more acceptable option in regards to the beneficial impacts on body composition and functional capacity.
Since December 2017, i-Sports Physiotherapy & Rehabilitation Centre had incorporated WBEMS into rehabilitation. This system has been used in many patients’ exercise therapy program including ACLR to overcome patients’ limitation in strengthening exercises due to their medical condition. With the available patients’ rehabilitation records, our research team aims to identify the effects of superimposed WBEMS in further preventing general deconditioning in post-ACLR patients compared to conventional exercises alone. We hypothesize that superimposing WBEMS on conventional exercises is more effective than conventional exercises alone in preventing body fat gain, muscle wasting and may improve the operated side quadriceps muscle recruitment on post-ACLR patients.
Method
This was a retrospective comparative study. Ethics approval was granted by the Joint Penang Independent Ethics Committee. Past medical records and physiotherapy treatment records of all post-ACLR patients who had underwent rehabilitation in i-Sports Physiotherapy & Rehabilitation Centre, Penang, Malaysia from January 2018 till September 2019, were retrieved and analyzed. To the best of our knowledge, i-Sports Physiotherapy & Rehabilitation Centre is currently the only centre in Malaysia to incorporate WBEMS into rehabilitation, data can only be collected from this centre.
Subjects
Only patients who met the following inclusion criteria were reviewed: patients who had underwent unilateral ACLR with or without meniscus repair and age above 15 years old. Taking into consideration of the variability in terms of post-operation rehabilitation protocol among different surgeons, only patients under the care of Mr Aaron Lim were recruited. Only patients who were compliance to the rehabilitation program, who had attended 14 physiotherapy sessions in between week 3 to week 8 were recruited. These were to minimize the confounding factors caused by variability in rehabilitation program.
Patients who fell under the following criteria were excluded: patients who had surgical repair of other knee ligaments concomitant with the ACLR or had co-existing injuries of any other structures in the operated knee (eg: cartilaginous, ligamentous, fracture). Also excluded were patients with co-existing injuries or musculoskeletal pain at any other parts of the body (eg: painful shoulder). These patients were excluded as they may have restriction in terms of their rehabilitation program which can lead to a wide variation in their rehabilitation ability compared to ‘pure’ ACLR patients.
These patients’ data were categorized into 2 groups. In the first group (WBEMS group, n=8), patients received rehabilitation with WBEMS. In the second group (CONV group, n=9), patients received rehabilitation without WBEMS. A total of 17 sets of patients’ data were extracted from their past medical records.
Intervention
At the selected rehab setting, there is a standardized rehabilitation protocol as well as assessment timeframe for all ACLR patients.
Upon completion of the first assessment which was conducted 2 weeks post-operation (POD15), patients had 3 sessions of physiotherapy per week for 2 weeks (week 2 to week 4). From week 5 to week 8, patients had 2 sessions of physiotherapy per week for 4 weeks. In WBEMS group, rehabilitation exercises were superimposed with WBEMS 3 times within the span of 2 weeks giving a total of 9 sessions of exercises with WBEMS. There were 5 sessions without WBEMS from week 2 to 8. The total number of physiotherapy sessions from the first assessment till follow-up assessment was 14 sessions. This rehabilitation flowchart is available in Figure 1.
Rehabilitation exercises protocol: Both groups of patients had done their rehabilitation exercises and progressed based on the same standardized protocol. The rehabilitation exercises included ROM exercises, strength training and balance and proprioception training. The CONV group performed their rehabilitation exercises based on the same standardized exercise program as WBEMS group without WBEMS.
Whole-Body EMS (WBEMS) protocol: On the 1st session, electrical stimulation intensity was kept low for adaptation. During subsequent sessions, the intensity of electrical stimulation was adjusted every 2-3 minutes. The intensity was controlled based on patients’ rate of perceived exertion (RPE). 6 out of 10 of Borg CR-10 Scale were maintained throughout the session and assure a clean dynamic movement. The stimulation was on throughout the session with intermittent off period for resting. This parameter was adopted based on guidelines as well as previous WBEMS researches to ensure sufficient stimulation was given to produce effects as well as preventing over-exertion which could lead to exercise-induced rhabdomyolysis [18].
The ACLR protocol and WBEMS parameter adopted are available in APPENDIX 1.
Outcome variables
Eligible patients’ demographic data including age, sex, present of meniscus repair were collected for further analysis. Patients’ progression on body composition and operated side quadriceps muscle maximum recruitment were retrieved from the physiotherapy treatment records as outcome measure for comparison.
Body composition – Bioelectrical Impedance Analysis (BIA) Inbody 370s: BIA is an instrument for estimating body composition, in particular body fat and muscle mass. The data of SMM, BFM, ATLM and NTLM of the recruited patients were retrieved for analysis.
Quadriceps muscle maximum recruitment – GymnaMYO 200: Electromyography detects and record the sum of electrical activity (motor unit action potential) in the targeted muscle at rest or when producing a movement. The test was performed based on a standardized protocol by 2 assigned, trained therapists to all post- ACLR patients. This protocol included skin preparation and location of electrode placement. Affected side quadriceps muscle EMG reading (EMG) was retrieved from recruited patients’ medical records to represent quadriceps muscle maximum recruitment.
Data collection
All post-ACLR patients in the selected setting follow a standardized assessment timeline to monitor their progression. All patients were assessed starting on post-operation day (POD) 15. Follow-up assessment was done every 2weeks until 2 months post-operation (POD57). All assessment in the selected setting was administered by the same 2 therapists using a standardized protocol including instruction given to patients. The standardized assessment protocol aims to minimize technical error of measurement.
To identify the effect of WBEMS on the targeted outcome stated above, data collected on POD15 were retrieved as baseline data while data collected on POD57 were used as post-intervention data.
Data analysis
Statistical analysis was carried out using SPSS statistics version 23.0. Baseline characteristics and follow-up data were expressed as mean and standard deviations.
Baseline balance between groups in term of participants’ characteristics and baseline outcome measure data were analyzed. The statistical test selected for gender as well as number of participants who had meniscus repair was analyzed using the Chi-squared test. While baseline statistical difference between groups for mean age and all baseline outcome measurement were analyzed using unrelated t-test.
The within-group changes in all outcomes were investigated using paired samples t tests.
ANCOVA test was used to test differences in the effects of additional WBEMS on dependent variables (body composition and quadriceps muscle maximum recruitment) compared to conventional rehabilitation training. Any baseline variable appeared to be an imbalance was measured and included in the analysis as a covariate.
All tests were two-tailed for all outcomes except quadriceps muscle maximum recruitment (EMG) and P ≤ 0.05 is considered as statistically significant for all analysis. Effect sizes based on the absolute difference (± standard deviation) between baseline and follow-up in the WB-EMS group versus the control group were calculated using Cohen’s d.
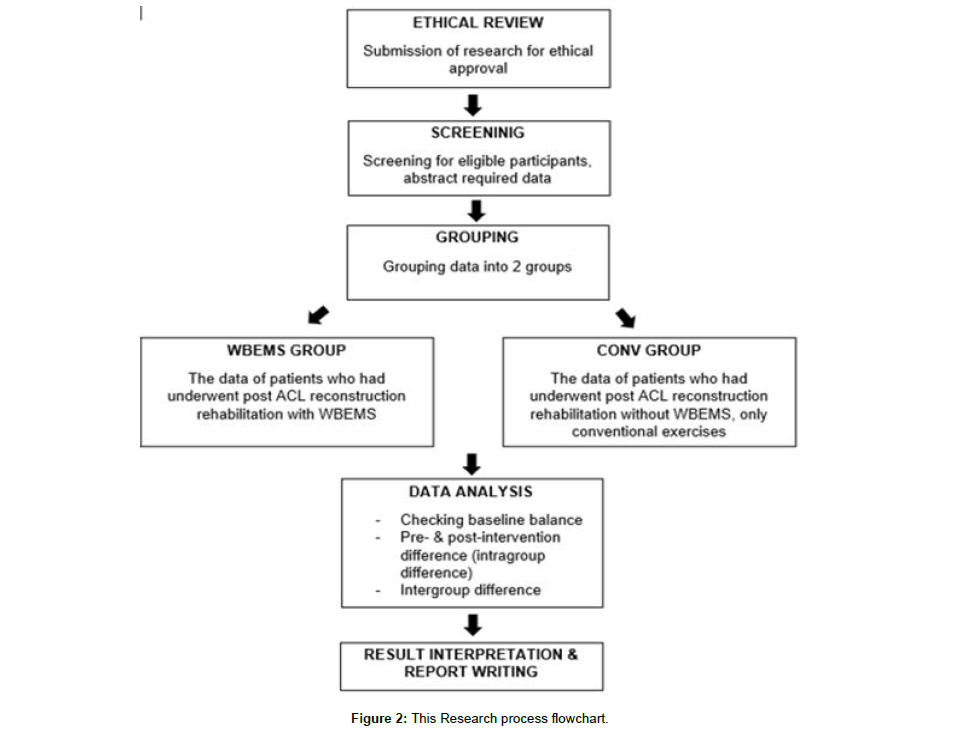
Research process
A flowchart showing the whole research process is available at Figure 2.
Results
Characteristics of subjects and baseline data (pre-intervention data) in WBEMS and CONV group are listed in Table 1. At baseline, a borderline significant difference between groups was observed for BFM. The CONV group had significantly higher BFM mean with a mean difference of 5.94 kg. Thus, ANCOVA was used to test between groups’ differences instead of unrelated t-test to ensure the imbalance was taken into account during the analysis.
| Variables | WBEMS (n=8) | CONV (n=9) |
| Age (years) | 30.25 ± 13.12 | 31.89 ± 9.75 |
| Gender (M/F) n= | 6/2 | 9/0 |
| Meniscus repair (present/absent) n= | 6/2 | 7/2 |
| Activity Level (HAL/LAL)b n= | 4/4 | 3/6 |
| Skeletal muscle mass (kg) | 29.03 ± 5.09 | 31.68 ± 3.92 |
| Body fat mass (kg)* | 15.85 ± 3.38 | 21.79 ± 6.61 |
| Affected side thigh lean mass (kg) | 8.47 ± 1.70 | 9.34 ± 1.34 |
| Non-affected side thigh lean mass (kg) | 8.13 ± 1.50 | 8.78 ± 1.21 |
| Affected side quadriceps maximum recruitment EMG reading (µV) | 62.01 ± 21.63 | 78.99 ± 63.67 |
Abbreviations: WBEMS: Whole-Body Electromyostimulation Group; CONV: Conventional Group; EMG: Electromyography
*indicates significant differences between groups (p<0.05)
a Values are mean ± SD unless otherwise indicated
b HAL: Patients who were actively involved in at least 1 type of sports and had done physical activity or training at least once a week, LAL: others who had not met the high activity level criteria
Table 1: Baseline characteristicsa of WBEMS and CONV group.
Based on the pre- and post-intervention mean differences presented in Table 2, both groups experienced overall skeletal muscle and body fat mass gain, as well as affected side thigh muscle wasting, although the changes were statistically insignificant in both groups.
| Pre | Post | (WBEMS – CONV) Mean Difference (95% CI) | Sig. (p value) | ES | |||
| WBEMS | CONV | WBEMS | CONV | ||||
| SMM (kg) | 29.025 ± 5.088 | 31.678 ± 3.920 | 29.175 ± 5.319 | 31.722 ± 3.780 | 0.160 (-.172 - .492) |
0.318 | 0.90 |
| BFM (kg) | 15.850 ± 3.376 | 21.789 ± 6.612 | 16.613 ± 3.810 | 21.911 ± 6.774 | 0.796 (-.514 – 2.105) |
0.213 | 0.77 |
| ATLM (kg) | 8.466 ± 1.696 | 9.340 ± 1.339 | 8.313 ± 1.780 | 9.041 ± 1.202 | 0.086 (-.322 - .495) |
0.657 | 0.365 |
| NTLM (kg) | 8.133 ± 1.504 | 8.781 ± 1.207 | 8.179 ± 1.612 | 8.827 ± 1.179 | 0.002 (-.244 - .247) |
0.987 | 0.003 |
| EMG (µV) | 62.013 ± 21.632 | 78.989 ± 63.671^ |
307.663 ± 99.902 | 202.649 ± 136.894^^ | 118.835 (1.911– 235.8) |
0.047* | 1.044 |
Abbreviations: WBEMS: Whole-Body Electromyostimulation Group; CONV: Conventional Group; Sig.: Significant Level; ES: Effect Size; SMM, Skeletal Muscle Mass; BFM: Body Fat Mass; ATLM: Affected Side Thigh Lean Mass; NTLM: Non-Affected Side Thigh Lean Mass; EMG: Affected side quadriceps muscle maximum recruitment EMG reading
^ indicates significant differences between pre- & post-intervention (p<0.05)
^^ indicates significant differences between pre- & post-intervention (p<0.001)
* indicates significant differences between groups (p<0.05)
Table 2: Pre- & Post-intervention Mean ± SD, Mean Difference (95% CI), p values & Effect Size data of both groups.
For intergroup differences, ANCOVA test indicated that after accounting for the significant differences in BFM between groups at pre-intervention data, this test revealed non-significant differences in all body composition parameters when comparing changes of WBEMS and CONV group. However, mean differences showed more overall skeletal muscle gain including non-affected side thigh lean mass as well as less muscle wasting on the affected side lower limb on WBEMS group with small to moderate effect size.
In terms of affected side quadriceps muscle maximum recruitment EMG readings, related t-test showed highly significant increase in both groups (CONV 123.67 ± 92.88, p=0.004; WBEMS 220.65 ± 98.23, p=0.000) with significantly more improvement shown in WBEMS group (p=0.047). EMG readings of the WBEMS group also presented large magnitude treatment effect (ES=1.044) when compared with the control group.
Sub-analysis was done to investigate the possible effects of patients’ premorbid activity level in relation to the treatment outcome. All patients’ data were reallocated into 2 different groups based on their premorbid activity level, regardless of whether they did their rehabilitation exercises with or without WBEMS. Patients who were actively participating in at least 1 type of sport and had done physical activity or training at least once a week were allocated into High Activity Level group (HAL), while others who had not met those criteria were grouped under Low Activity Level (LAL) group.
Among the 17 recruited participants, 7 were categorized under HAL while the remaining 10 were under LAL group. In the 7 HAL patients, 4 did their rehab with WBEMS; while in LAL group, 4 out of 10 underwent rehabilitation with WBEMS.
Checking on the baseline characteristics balance between HAL & LAL group, no significant imbalance was identified. Baseline characteristics for both groups are available in Table 3.
| Variables | HAL (n=7) | LAL (n=10) |
| Age (years) | 30.29 ± 8.361 | 31.70 ± 13.124 |
| Gender (M/F), n= | 5/2 | 10/0 |
| Meniscus repair (present/absent), n= | 4/3 | 9/1 |
| Done rehab (with / without WBEMS), n= | 4/3 | 4/6 |
| Skeletal muscle mass (kg) | 29.386 ± 4.985 | 31.16 ± 4.370 |
| Body fat mass (kg) | 16.786 ± 3.407 | 20.54 ± 7.081 |
| Affected side thigh lean mass (kg) | 8.849 ± 1.716 | 8.985 ± 1.489 |
| Non-affected side thigh lean mass (kg) | 8.36 ± 1.471 | 8.557 ± 1.338 |
| Affected side quadriceps maximum recruitment EMG reading (µV) | 69.957 ± 46.102 | 91.73 ± 63.657 |
Abbreviations: HAL: High Activity Level; LAL: Low Activity Level; WBEMS: Whole-Body Electromyostimulation; EMG: Electromyography
a Values are mean ± SD unless otherwise indicated
*indicates significant differences between groups (p<0.05).
Table 3: Baseline characteristicsa of HAL and LAL group.
Descriptive information of HAL group at each outcome measurement is presented in Table 4. There is no significant difference between WBEMS and CONV participants with respect to body composition changes in HAL group. While patients who had undergone WBEMS had significantly better operated side quadriceps muscle recruitment compared to CONV group with large Effect Size (ES=1.702).
| Pre | Post | Mean Difference (WBEMS – CONV) (95% CI) | Sig. (p value) | ES | |||
| WBEMS | CONV | WBEMS | CONV | ||||
| SMM (kg) | 27.0 ± 5.415 | 32.567 ± 2.003 | 26.9 ± 5.593 | 32.5 ± 2 | -0.175 (-.626 - .276) |
0.379 | 0.585 |
| BFM (kg) | 14.85 ± 2.972 | 19.367 ± 2.021 | 15.125 ± 2.762 | 19.467 ± 1.595 | 0.25 (-1.093 – 1.593) |
0.665 | 0.243 |
| ATLM (kg) | 7.95 ± 1.821 | 10.047 ± 0.307 | 7.683 ± 1.749 | 9.56 ± 0.242 | 0.185 (-.155 - .525) |
0.231 | 0.862 |
| NTLM (kg) | 7.702 ± 1.724 | 9.203 ± 0.225 | 7.67 ± 1.718 | 9.203 ± 0.225 | 0.0325 (-.126 - .191) |
0.634 | 0.314 |
| EMG (µV) | 92.4 ± 49.015 | 40.033 ± 20.544 | 338.3 ± 97.909 | 136.747 ± 113.282 | 137.24 (3.898 – 270.58) |
0.045* | 1.702 |
Abbreviations: HAL: High Activity Level; WBEMS: Whole-Body Electromyostimulation Group; CONV: Conventional Group; Sig.: Significant Level; ES: Effect Size; SMM: Skeletal Muscle Mass; BFM: Body Fat Mass; ATLM: Affected Side Thigh Lean Mass; NTLM: Non-Affected Side Thigh Lean Mass; EMG: Affected side quadriceps muscle maximum recruitment EMG reading
* indicates significant differences between groups (p<0.05)
Table 4: Pre- & Post-intervention Mean ± SD, Mean Difference (95% CI), p values & Effect Size data of HAL group.
Differing from HAL results, LAL participants generally showed better improvement in all muscle parameters (SMM, ATLM, NTLM) favoring WBEMS. However, the mean differences were still statistically insignificant for all body composition parameters. Similar to HAL group, the EMG readings also demonstrated better outcome in the WBEMS group as compared to CONV but this difference did not achieve statistical significance (P=0.43). Descriptive information of LAL group is illustrated in Table 5.
| Pre | Post | Mean Difference (WBEMS – CONV) (95% CI) | Sig. (p value) |
ES | |||
| WBEMS | CONV | WBEMS | CONV | ||||
| SMM (kg) | 31.05 ± 4.487 | 31.233 ± 4.720 | 31.45 ± 4.576 | 31.333 ± 4.552 | 0.3 (-.205 - .805) |
0.208 | 0.75 |
| BFM (kg) | 16.85 ± 3.885 | 23 ± 7.94 | 18.1 ± 4.511 | 23.133 ± 8.187 | 1.117 (-.648 – 2.881) |
0.183 | 1.614 |
| ATLM (kg) | 8.983 ± 1.638 | 8.987 ± 1.543 | 8.943 ± 1.81 | 8.782 ± 1.430 | 0.165 (-.402 - .732) |
0.521 | 0.372 |
| NTLM (kg) | 8.563 ± 1.346 | 8.553 ± 1.462 | 8.688 ± 1.557 | 8.638 ± 1.441 | 0.04 (-.317 - .397) |
0.803 | 0.167 |
| EMG (µV) | 81.625 ± 60.639 | 98.467 ± 70.368 | 277.025 ± 105.821 | 235.6 ± 144.714 | 58.267 (-103.3 – 219.9) |
0.430 | 0.60 |
Abbreviations: LAL, Low Activity Level; WBEMS: Whole-Body Electromyostimulation Group; CONV: Conventional Group; Sig.: Significant Level; ES: Effect Size; SMM: Skeletal Muscle Mass; BFM: Body Fat Mass; ATLM: Affected Side Thigh Lean Mass; NTLM: Non-Affected Side Thigh Lean Mass; EMG: Affected side quadriceps muscle maximum recruitment EMG reading
* indicates significant differences between groups (p<0.05)
Table 5: Pre- & Post-intervention Mean ± SD, Mean Difference (95% CI), p values & Effect Size data of LAL group.
One interesting finding was that there was more body fat mass gained in the WBEMS group in both HAL and LAL patients with no significant difference from CONV group.
Discussion
The major findings of the study documented non-significant differences between groups that could be noted in all body composition parameters, other than the fact that superimposed WBEMS induced significantly more improvement in quadriceps maximum recruitment of the affected limb.
Differing from our study, 2 previous studies had shown significant gain in muscle mass and strength as well as reduction in abdominal body fat on the group of untrained subjects who had WBEMS training for 16 to 52 weeks [19,17]. Despite adopting the same guideline on EMS stimulation parameters, our study samples did not show significant improvement in body composition. A few differences were identified between our study and the previous studies. Both studies conducted previously recruited only untrained elderlies with a training period of 16 and 52 weeks. While our study recruited a mixture of sedentary individuals to elite athletes and our training period was only 6 weeks (2 months post-operation). We hypothesized that 1) active individuals / athletes require higher volume/intensity of training to achieve muscle hypertrophy 2) WBEMS requires more than 6 weeks training (9 sessions) to achieve significant body composition changes. These hypotheses are also supported by another study done on a group of athletes who had done at least 2 years of resistance training with 3 to 6 hours of sport-specific training per week [20]. In this study, EMS was superimposed on the participants’ quadriceps while doing squat exercises. Training duration was 6 weeks, 2 times per week. The study results showed non-significant differences on quadriceps muscle strength between EMS group and control group.
Therefore, in this study, a sub-analysis was done to determine whether the patients’ premorbid level of activity could affect the results of the study. Patients were divided into two groups; high activity level (HAL) and low activity level (LAL). The study documented non-significant differences in the parameters of body composition in both groups. However, the LAL group documented better results for all muscle mass parameters, more so for those with superimposed WBEMS, although it was still statistically insignificant. This could be due to the small sample size. This sub-analysis attained similar results with the previous researches mentioned above.
We believe that the reason why those in the HAL group documented non-significant differences in body composition reading as compared to those in the LAL group lies in the pre-injury training intensity level. Numerous studies had observed that novices only require 60% of 1RM training intensity to achieve any significant improvement in strength while high activity level individuals would need at least 80% of 1RM training intensity to achieve any significant strength improvement [21]. For the HAL group, before injury their muscles are subjected to higher load on a regular basis, leading the muscle to be adapted to high load. During the early phase of post-operation, due to the movement and activity restrictions, HAL individual has now observed a drop in their training intensity. Lower intensity training requires less muscle recruitment. When this is prolonged, muscle wasting or atrophy would occur [22]. In contrast, for the relatively sedentary individual whose muscles were mainly used for normal daily activities only, more muscle fibers were forced to be recruited to generate sufficient force to perform post-ACLR rehabilitation training. With the assistance of WBEMS, muscle fibers recruitment was enhanced. After numerous sessions of training, muscles will go through neural adaptation leading to increase strength and ultimately muscle hypertrophy [23]. However, despite having the additional stimulation from EMS, 6 weeks (9 sessions) of training might still be insufficient to cause significant changes on body composition.
On the other hand, our study results on quadriceps muscle maximum recruitment (EMG) showed highly significant differences between groups, with WBEMS group showing more improvement than the control group. Post-ACLR inflammation is thought to increase joint receptors activity, leading to arthrogenic muscle inhibition [24]. Due to this reason, individuals are unable to recruit higher threshold motor units during voluntary muscle contraction [24]. With EMS superimposed on the muscle during exercises, the electrical stimulation is able to force more motor unit recruitment at different muscles length and during different contraction modes [25]. Not only does electrical stimulation works as a facilitator in muscle fibers recruitment, the simultaneous firing of the antagonist muscle acts as a resistant, similar effect as external weights, forcing more voluntary muscle force without overloading the joint. This might explain the highly significant difference between WBEMS and conventional group in quadriceps muscle maximum recruitment (EMG) reading. Moreover, as this paper is targeted on the early phase of ACLR rehabilitation, the exercises done were relatively low intensity to prevent excessive shearing force to the newly constructed ligament. Submaximal strength training recruited mostly type 1 muscle fibers instead of type 2 fibers [22]. Superimpose EMS using surface electrode might help to assist recruitment of type 2 fibers which lie superficially. Continuous application might enhance the cumulative physiological effects including strength gain and eventually increase muscle mass [23]. Poor muscle activation contributes substantially to early post-operation muscle weakness and atrophy [26]. Thus, quadriceps muscle activation at early phase of post- ACLR rehabilitation is important in preventing quadriceps muscle weakness and delay muscle atrophy.
Limitations
Factors which may affect the results of this study but were not addressed included participants’ knee condition. Patients’ ROM, swelling and pain level will affect the quality of execution of the exercise as well as the quality of muscle engagement [27]. Limited ROM and pain resulting from the disruption of tissue or joint swelling may compromise the joint receptors and cutaneous nerves, inhibiting the ability to generate joint movement [27]. Through our observation, our patients’ condition varied widely in terms of ROM, pain level and swelling at the early stage of recovery. Patients who had more limited knee ROM due to scar tissue formation or experienced more pain upon knee movement or weight bearing tend to have more difficulty in doing rehabilitation exercises, resulting in increased muscle atrophy as compared to those who had less limitation. Other factors which may also influence patients’ recovery include patients’ nutritional status, physical activity level and nature of job.
Besides, as Inbody uses bioelectric impedance to estimate body composition, we suspect that the swelling retained in the operated limb may affect the result, leading to less accurate data.
Conclusion
Our results clearly demonstrate that superimposing WBEMS with ACLR rehabilitation exercises for as short as 6 weeks, has beneficial impact on improving operated side quadriceps maximum recruitment. This is an important factor at the early stage of rehabilitation in preventing quadriceps muscle wasting. However, the treatment dosage might be insufficient to impact body composition. As this is a retrospective study, more robust research design is needed in future study which takes into consideration of the potential confounding factors stated above to identify the true effect of WB-EMS in the field of rehabilitation.
Conflict of Interest
The authors reported no conflict of interest in this work
Acknowledgements
The authors would like to thank the i-Sports team and Symone Lee Yeng Yeng for their invaluable support and their assistance on data collection.
Ethics Approval
Joint Penang Independent Ethics Committee (JPEC) approved this study. As this is a retrospective study which only involve patients’ past medical records, thus approval been given by board of ethics to wave off written informed consent.
References
- Andersen JL, Aagaard P (2010) Effects of strength training on muscle fiber types and size; consequences for athletes training for high-intensity sports. Scand J Med Sci Sports 20: 32-38.
- Buckthorpe M, Rosa GL, Villa FD (2019) Restoring knee extensor strength after anterior cruciate ligament reconstruction: A clinical commentary. Int J Sports Phys Ther 14: 159-72.
- Chung KS, Ha JK, Yeom CH, Ra HJ, Kwon MS, et al. (2015) Are muscle strength and function of the uninjured lower limb weakened after anterior cruciate ligament injury? Two-year follow up after reconstruction. Am J Sports Med 43: 3101-21.
- Currier DA, Mann R (1983) Muscular strength development by electrical stimulation in healthy individuals. Phys Ther 63: 915-21.
- Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, et al. (2007) Effects of early progressive eccentric exercise on muscle structure after anterior cruciate ligament reconstruction. J Bone Joint Surg Am 89: 559-70.
- Hart JM, Pietrosimone B, Hertel J, Ingersoll CD (2010) Quadriceps activation following knee injuries: A systematic review. J Athl Train 45: 87-97.
- Hopkins JT, Ingersoll CD (2000) Arthrogenic muscle inhibition: a limiting factor in joint rehabilitation. J Sport Rehab 9: 135-59.
- Hurley MV, Jones DW, Newham DJ (1994) Arthrogenic quadriceps inhibition and rehabilitation of patients with extensive traumatic knee injuries. Clin Sci (Colch) 86: 305-10.
- Kemmler W, Teschler M, Weibenfels A, Bebenek M, Fröhlich M, et al. (2016) Effects of whole-body electromyostimulation versus high-intensity resistance exercise on body composition and strength: A randomized controlled study. Evid Based Complement Alternat Med 2016.
- Kemmler W, Bebenek M, Engelke K, von Stengel S (2014) Impact of whole-body electromyostimulation on body composition in elderly women at risk for sarcopenia: The Training and ElectroStimulation Trial (TEST-III). Age (Dordr) 36: 395-406.
- Kemmler W, von Stengel S (2013) Whole-body electromyostimulation as a means to impact muscle mass and abdominal body fat in lean, sedentary, older female adults: Subanalysis of the TEST-III trial. Clin Interv Aging 8: 1353-64.
- Konin JG, Jessee B (2012) Range of Motion and Flexibility. Physical Rehabilitation of the Injured Athlete (4th Edn.). Andrews JR, Harrelson GL, Wilk KE, (ed.) Philadelphia, Elsevier Saunders: 74-88.
- Lewek M, Rudolph K, Axe M, Snyder-Mackler L (2002) The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech 17: 56-63.
- Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50: 3145-52.
- Mizner RL, Petterson SC, Stevens JE, Vandenborne K, Snyder-Mackler L (2005) Early quadriceps strength loss after total knee arthroplasty. J Bone Joint Surg Am 87: 1047-53.
- Nitz AJ, Dobner JJ (1987) High intensity electrical stimulation effect on thigh musculature during immobilization for knee sprain. Phys Ther 67: 219-22.
- Paillard T (2018) Training based on electrical stimulation superimposed onto voluntary contraction would be relevant only as part of submaximal contractions in healthy subjects. Front Physiol 9: 1428.
- Palmieri-Smith RM, Thomas AC (2009) A Neuromuscular mechanism of posttraumatic osteoarthritis associated with ACL injury. Exerc Sport Sci Rev 37: 147-53.
- Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, et al. (2010) Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 38: 1968-78.
- Ratamess NA, Alvar BA, Evetoch TK, Housh TJ, Kibler WB, et al. (2009) Progression models in resistance training for healthy adults. Med Sci Sports Exerc 41: 687-708.
- Rice DA, McNair PJ (2010) Quadriceps arthrogenic muscle inhibition: Neural mechanisms and treatment perspectives. Semin Arthritis Rheum 40: 250-66.
- Schmitt LC, Paterno MV, Hewett TE (2012) The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament Reconstruction. J Orthop Sports Phys Ther 42: 750-9.
- Slysz JT, Burr JF (2018) The Effects of Blood Flow Restricted Electrostimulation on Strength and Hypertrophy. J Sport Rehabil 27: 257-62.
- Tourville TW, Jarrell KM, Naud S, Slauterbeck JR, Johnson RJ, et al. (2014) Relationship between isokinetic strength and tibiofemoral joint space width changes after anterior cruciate ligament reconstruction. Am J Sports Med 42: 302-11.
- Urbach D, Nebelung W, Weiler HT, Awiszus F (1999) Bilateral deficit of voluntary quadriceps muscle activation after unilateral ACL tear. Med Sci Sports Exerc 31: 1691-6.
- Westing SH, Seger JY, Thorstensson A (1990) Effects of electrical stimulation on eccentric and concentric torque-velocity relationships during knee extension in man. Acta Physiol Scand 140: 17-22.
- Wirtz N, Zinner C, Doermann U, Kleinoeder H, Mester J (2016) Effects of loaded squat exercise with and without application of superimposed EMS on physical performance. J Sports Sci Med 15: 26-33.
Citation: Neo JX, Chew KH, Lim ABK (2021) Effects of Whole-Body EMS on Post- ACL Reconstruction General Conditioning - A Retrospective Comparative Study. J Nov Physiother 11: 448. DOI: 10.4172/2165-7025.1000448
Copyright: © 2021 Neo JX, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2427
- [From(publication date): 0-2021 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 1687
- PDF downloads: 740