Research Article Open Access
Effects of Ultrasound and Sonic Toothbrushes on Oral Hygiene Status
Akane Takenouchi*, Takashi Matsukubo, Miwa Sakurai Matsukubo, Yukiko Satoho, Hiroe Arai, Etsuyo Otani and Yumiko Kakegawa
Taiyo Schoold of Dental Hygiene Arakawa-ku, Tokyo, Japan
*Corresponding Author:
- Akane Takenouchi
BOH, RDH, Taiyo School of Dental Hygiene
116-0013 Tokyo, Arakawa-ku, Nishi-Nippori 2-22-1
Station Plaza Tower 6F, Japan
Tel: (+81)03-5810-8020
Fax: (+81)03-5810-8023
E-mail: lisa_serugio4@hotmail.co.jp
Received Date: October 06, 2016 Accepted Date: November 10, 2016 Published Date: November 17, 2016
Citation: Takenouchi A, Matsukubo T, Matsukubo MS, Satoho Y, Arai H, et al. (2016) Effects of Ultrasound and Sonic Toothbrushes on Oral Hygiene Status. J Oral Hyg Health 4: 208. doi:10.4172/2332-0702.1000208
Copyright: © 2016 Takenouchi A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Objective: To evaluate the effects of ultrasound and sonic toothbrushes on the oral hygiene status of healthy people.
Methods: This study was administered with a randomized, controlled, and double-blind trial. Twenty-nine firstyear dental hygiene students answered a questionnaire on oral hygiene behavior, and they were divided into one of four groups after pre-examination. Each group used an electronic toothbrush with different modes (2 times/day, 3 min) after tooth brushing instruction (TBI) for four weeks; A (control): used with power off; B: used with the sonic mode (sonic wave: 16,000 strokes/min); C: used with the ultrasound mode (ultrasound frequency: 1.6 MHz); D: used with the ultrasound + sonic mode. The plaque index (PlI) and gingival index (GI) were assessed. The unstimulated saliva flow rate was measured (spitting method, 1 min). The Ethical Committee of the Japan Dental Hygienists’ Association approved this study’s protocol (vote number: 2). A Wilcoxon signed-rank test was used.
Results: The PlI decreased in group C (baseline: 1.42 ± 0.83; 4 weeks: 0.92 ± 0.34; p<0.05) and D (baseline: 1.41 ± 0.3; 4 weeks: 0.92 ± 0.3; p<0.01). The unstimulated saliva flow rate of group C and D, which used electronic toothbrushes with ultrasound, increased significantly (baseline: 0.57 ± 0.33 mg; 4 weeks: 0.78 ± 0.5 mg; p<0.05). The GI did not change in all groups. Participants who had received TBI before this study had an increased unstimulated saliva flow rate (baseline: 0.65 ± 0.35 mg; 4 weeks: 0.87 ± 0.5 mg; p<0.05).
Conclusion: The use of electronic toothbrushes with ultrasound for four weeks effectively decreased the PlI and increased the unstimulated saliva flow rate. Professional prophylaxis was required to improve gingival status. TBI enabled participants to use electronic toothbrushes more effectively to stimulate the salivary gland and to increase the unstimulated saliva flow rate.
Keywords
Ultrasound toothbrush; Saliva flow rate; Electronic toothbrush; Oral hygiene
Introduction
Electronic toothbrushes are becoming so popular that many kinds of electronic toothbrushes can now be purchased over the counter at electronic stores. Previous research identifying the effects of electronic toothbrushes on oral hygiene was conducted; however, many studies mentioned the effects of toothbrushes with not only ultrasound but those with ultrasound plus sonic vibration [1–5]. In general, most over-the-counter electronic toothbrushes, called ultrasonic toothbrushes, emit ultrasound plus sonic waves.
The differences in ultrasound and sonic waves are not well-known; ultrasound has an imperceptible vibration, while sonic waves have a perceivable vibration and audible sound. There is very little research related to ultrasound toothbrushes; therefore, some users may be suspicious of the effects of ultrasound toothbrushes because they are imperceptible. More clinical research comparing the effects of toothbrushes with ultrasound and with ultrasound plus sonic waves is required.
Also, this research did not evaluate the change in saliva flow rate, which has a substantial impact on oral hygiene [6]. One of our hypotheses was that the vibration of electronic toothbrushes was effective in stimulating the saliva gland: if so, electronic toothbrushes, which have vibration regardless of their lack of visibility, act as a kind of saliva gland massage, thereby effectively increasing the saliva flow rate [7].
Therefore, this research was conducted to evaluate the effects of ultrasound toothbrushes on the oral hygiene status including the plaque score, gingival status, and saliva flow rate of healthy people. This research will be one to heighten the credibility of ultrasound toothbrushes as well as to encourage dental professionals to explain the differences between ultrasound and sonic toothbrushes in accordance with the evidence.
Methods
Participants
Participants of this research were first-year dental hygiene students. Exclusion criteria were as follows: (i) had active dental caries, (ii) had systemic disease, (iii) took antibiotics regularly, (iv) underwent orthodontic treatments, (v) currently used an electronic toothbrush. This study’s protocol was approved by the Ethical Committee of Japan Dental Hygienists’ Association (vote number: 2). Written informed consent was obtained from all participants.
Examined electronic toothbrush
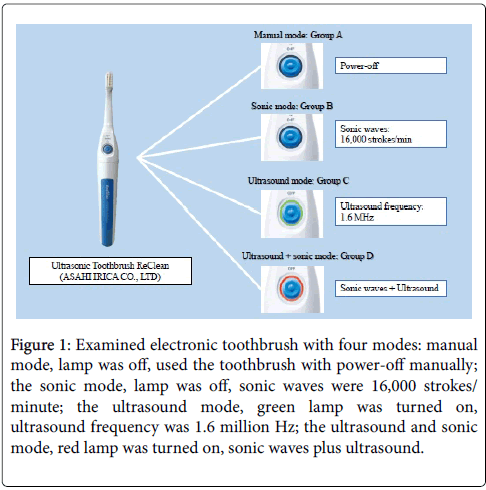
Ultrasound Toothbrush ReClean (ASAHI IRICA CO., LTD) was used [8]. In this research, each participant used this electronic toothbrush with different modes: the manual mode, the lamp was off, and the toothbrush was used manually with power off; the sonic mode, the lamp was off, and sonic waves of 16,000 strokes/minute were used; the ultrasound mode, the green lamp was turned on, and an ultrasound frequency of 1.6 million Hz was used; the ultrasound and sonic mode, the red lamp was turned on, and sonic waves plus ultrasound were used (Figure 1).
Figure 1: Examined electronic toothbrush with four modes: manual mode, lamp was off, used the toothbrush with power-off manually; the sonic mode, lamp was off, sonic waves were 16,000 strokes/ minute; the ultrasound mode, green lamp was turned on, ultrasound frequency was 1.6 million Hz; the ultrasound and sonic mode, red lamp was turned on, sonic waves plus ultrasound.
Once users pushed the button, this toothbrush moved for three minutes with a vibration alarm every 45 seconds. Participants were not informed which mode they used. All of them pushed the button once or twice, though it did not work when participants used the toothbrush with the power off.
Tooth brushing instruction (TBI)
At the first visit, participants received TBI. This study involved four operators, and they did TBI following the manual that the manufacturer had created. Therefore, we can say that all of the four operators conducted common TBI for every participant. These are the five points in the TBI: (i) every participant used an electronic toothbrush with fluoride dentifrice, (ii) the scrubbing tooth brushing technique was taught, (iii) the mouth was closed during tooth brushing to heighten the effects of ultrasound, (iv) enough buccal mucosa was removed for the toothbrush to reach the cervical areas on molar teeth, (v) participants brushed their teeth using an examined toothbrush two times a day for three minutes.
All examined modes in toothbrushes except manual mode had a vibration alarm system every 45 seconds. Therefore, participants brushed each jaw quadrant for 45 seconds following the alarm. Participants who used an examined toothbrush with power off were given a timer to measure three minutes by themselves.
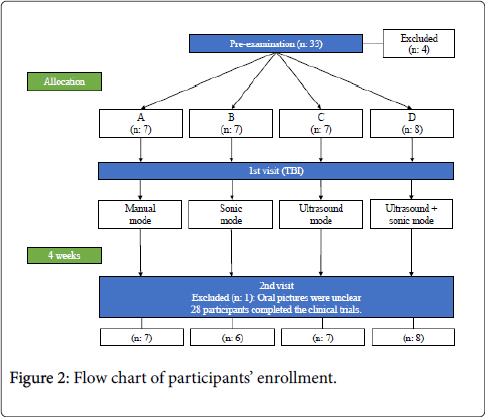
Clinical trials
This study was administered with a randomized, controlled, and double-blind trial. Participants were numbered, and all of the results of this study were treated numerically (Figure 2).
First, 33 participants received pre-examination. The results of the plaque index (PlI), gingival index (GI), and unstimulated saliva flow rate were utilized to divide participants randomly into one of four groups: A (control): used with power off, B: used with the sonic mode, C: used with the ultrasound mode, D: used with the ultrasound + sonic mode.
Second, participants received TBI, they were given an examined electronic toothbrush, and they used it with the allocated mode two times a day for three minutes over four weeks. After that, they received an examination.
Measurements
Participants answered if they had received TBI before this research at pre-examination. Oral pictures were taken, and a masked examiner assessed the Quigley-Hein plaque index (PlI) and Silness and LÓ§e gingival index (GI) viewing the oral pictures and the results of bleeding on probing. The unstimulated saliva flow rate was measured using a spitting method for 1 minute.
Statistical analysis
A Wilcoxon signed-rank test was used for statistical analysis to compare the intragroup differences between baseline and after four weeks in all measurements by group. Group A and B and group C and D were combined into the “Group without ultrasound” and the “Group with ultrasound,” respectively. After that, the changes in all measurements were compared by ultrasound. The Krusal Wallis test was also used to evaluate intergroup differences after four weeks. JMP version 11 for Windows (Statistical Discovery, From SAS) was used for statistical analysis, and p-values <0.05 were considered to be statistically significant.
Results
Twenty-eight participants completed the clinical trials (mean age: 22 ± 6.99). Four of the participants were excluded after the preexamination because they did not meet the inclusion criteria, and data on one of the participants was excluded because the oral pictures were too unclear to be evaluated.
PlI
All groups showed the tendency of a decrease in the PlI, and significant differences were found in Group C (baseline: 1.42 ± 0.83; 4 weeks: 0.92 ± 0.34; p<0.05) and D (baseline: 1.41 ± 0.3; 4 weeks: 0.92 ± 0.3; p<0.01). The group with ultrasound showed a significant decrease in the PlI (baseline: 1.42 ± 0.59; 4 weeks: 0.92 ± 0.31; p<0.001). There were no significant differences among groups (Table 1).
| Baseline | After 4 weeks | P-value | |
|---|---|---|---|
| PlI | |||
| A (n: 7) | 1.41 ± 0.22 | 1.26 ± 0.64 | NS |
| B (n: 6) | 1.38 ± 0.28 | 1.14 ± 0.1 | NS |
| C (n: 7) | 1.42 ± 0.83 | 0.92 ± 0.34 | 0.03 |
| D (n: 8) | 1.41 ± 0.3 | 0.92 ± 0.3 | 0.0078 |
| GI | |||
| A (n: 7) | 0.67 ± 0.3 | 0.78 ± 0.37 | NS |
| B (n: 6) | 0.68 ± 0.47 | 0.87 ± 0.26 | NS |
| C (n: 7) | 0.69 ± 0.12 | 0.7 ± 0.29 | NS |
| D (n: 8) | 0.77 ± 0.38 | 0.83 ± 0.31 | NS |
Wilcoxon signed-rank test *NS: No significance
A: Manual mode, B: Sonic mode, C: Ultrasound mode, D: Ultrasound + sonic mode
Table 1: Averages in the PlI and GI at baseline and after 4 weeks by group.
GI
No significant differences were found in all groups on the GI (Table 1).
Unstimulated saliva flow rate
The unstimulated saliva flow rate significantly increased in the group with ultrasound after four weeks (baseline: 0.57 ± 0.33 mg/min;4 weeks: 0.78 ± 0.5 mg/min; p<0.05). Furthermore, participants who had received TBI before this research showed the tendency to have a significantly increased unstimulated saliva flow rate (baseline: 0.65 ± 0.35 mg/min; 4 weeks: 0.87 ± 0.5 mg/min; p<0.05). There were no significant differences among groups (Table 2).
| Baseline | After 4 weeks | P-value | |
|---|---|---|---|
| Unstimulated saliva flow rate | |||
| w/o ultrasound (n: 13) | 0.63 ± 0.42 | 0.76 ± 0.47 | NS |
| with ultrasound (n: 15) | 0.57 ± 0.33 | 0.78 ±0.5 | 0.0312 |
| Unstimulated saliva flow rate | |||
| Had never received TBI (n: 15) | 0.56 ± 0.39 | 0.68 ± 0.46 | NS |
| Had received TBI before (n: 13) | 0.65 ± 0.35 | 0.87 ± 0.5 | 0.0146 |
Discussion
First, ultrasound was effective in decreasing the PlI and in increasing the saliva flow rate for four weeks, which was in accordance with modern research that showed that toothbrushes with only ultrasound disrupted Streptococcus mutans chains [9]. Also, the effects of ultrasonically activated water streams on removing plaque were identified in other modern research [10]; that is, imperceptible vibration of ultrasound was effective to remove biofilms on the teeth including noncontact surfaces, to stimulate the saliva gland, and to improve oral hygiene status. Using technology to improve oral hygiene status should be promoted because electronic toothbrushes showed higher benefits than a certain standard for all participants regardless of their tooth brushing technique. More RCT related to ultrasound toothbrushes are required to heighten their credibility and to get more people to use them. In this process, dental professionals could keep learning about ultrasound or ultrasonic, which is used widely in dental treatment—not only in professional prophylaxis but also in root canal treatments [11-13]. Actually, dental hygiene education programs will be changed to reflect a contemporary approach to ultrasonic instrumentation [14].
Second, professional prophylaxis is essential to improve gingival status, though it was not implemented in this research. Hence, this study showed the pure effects of the use of electronic toothbrushes and identified that only self-care was insufficient to improve gingival status because no toothbrushes could remove biofilms in periodontal pockets. Thus, these biofilms should be removed by professional prophylaxis including ultrasonic scaling or debridement utilizing cavitation [15–17] because previous research showed that the quality of self-performed mechanical plaque removal was not sufficiently effective in adults with gingivitis [18]. If professional prophylaxis had been included in this research, gingival status would likely have improved, as previous research has shown [19].
Third, TBI enabled participants to use electronic toothbrushes more effectively to stimulate the saliva gland. Whether or not users could remove enough buccal mucosa for toothbrushes to reach cervical areas was very important. The point was whether or not the saliva gland was exposed to ultrasound. Actually, previous research showed that the learning effect had a higher impact on improvement in oral hygiene [20]. Furthermore, some users may misunderstand how to use ultrasound toothbrushes, for instance, they might just put the head of the toothbrush on the tooth surfaces but not move it, which is completely different from how to use sonic toothbrushes. Users should receive TBI before using any kind of electronic toothbrushes.
The population of this study was healthy youngsters; moreover, they were dental hygiene students. This was one of the limitations in this research. Hence, the results of this study cannot be generalized; however, this study showed the highly possibility that the imperceptible vibration of ultrasound was effective in improving the PlI as well as in stimulating the saliva gland to increase the unstimulated saliva flow rate. Whether or not the same results will be obtained for older people will be identified in our future research.
Conclusion
Electronic toothbrushes with ultrasound were effective to improve oral hygiene of dental hygiene students; however, patients should visit dental clinics and receive TBI before using it to heighten the effects of ultrasound. In doing so, patients will receive professional prophylaxis and improve their gingival status, as well.
Acknowledgement
The authors thank the dental hygiene students who participated in this study and the Taiyo School of Dental Hygiene students and educators who assisted in this research. Michael Bayne’s (Kurdyla and Association Co.) editing of the manuscript is really appreciated by the authors. This study was conducted with the help of the Ito Co. Examined electronic toothbrushes were supplied by the Ito Co.
References
- Costa MR, Marcantonio RA, Cirelli JA (2007) Comparison of manual versus sonic and ultrasonic toothbrushes: a review. Int J Dent Hyg 5: 75-81.
- Yaacob M, Worthington H, Deacon S, Deery C, Walmsley A, et al. (2014) Powered versus manual tooth brushing for oral health (Review). Cochrane Database Syst Rev CD002281.
- Schmidt JC, Zaugg C, Weiger R, Walter C (2013) Brushing without brushing? A review of the efficacy of powered toothbrushes in noncontact biofilm removal. Clin Oral Investig 17: 687-709.
- Forgas-Brockmann LB, Carter-Hanson C, Killoy WJ (1998) The effects of an ultrasonic toothbrush on plaque accumulation and gingival inflammation. J Clin Periodontol 25: 375-379.
- Goldman HM (1974) Effectiveness of an ultrasonic toothbrush in a group of uninstructed subjects. J Periodontol 45: 84-87.
- Deery C, Heanue M, Deacon S, Robinson PG, Walmsley AD, et al. (2004) The effectiveness of manual versus powered toothbrushes for dental health: A systematic review. J Dent 32: 197-211.
- Ohara Y, Yoshida N, Kono Y, Hirano H, Yoshida H, et al. (2015) Effectiveness of an oral health educational program on community-dwelling older people with xerostomia. Geriatr Gerontol Int 15: 481-489.
- (2003) Ultrasound Toothbrush ReClean Japanese. Ito Co.
- Hashizume LN, Dariva A (2015) Effect of sonic vibration of an ultrasonic toothbrush on the removal of Streptococcus mutans biofilm from enamel surface. Am J Dent 28: 347-350.
- Howlin RP, Fabbri S, Offin DG, Symonds N, Kiang KS, et al. (2015) Removal of dental biofilms with an ultrasonically activated water stream. J Dent Res 94: 1303-1309.
- Jiang LM, Verhaagen B, Versluis M, Zangrillo C, Cuckovic D, et al. (2010) An evaluation of the effect of pulsed ultrasound on the cleaning efficacy of passive ultrasonic irrigation. J Endod 36: 1887-1891.
- Jiang LM, Verhaagen B, Versluis M, Langedijk J, Wesselink P, et al. (2011) The influence of the ultrasonic intensity on the cleaning efficacy of passive ultrasonic irrigation. J Endod 37: 688-692.
- Macedo RG, Verhaagen B, Rivas DF, Versluis M, Wesselink P, et al. (2014) Cavitation measurement during sonic and ultrasonic activated irrigation. J Endod 40: 580-583.
- Asadoorian J, Botbyl D (2015) Dental hygienists’ perception of preparation and use for ultrasonic instrumentation. Int J Dent Hyg 13: 30-41.
- Felver B, King DC, Lea SC, Price GJ, Damien Walmsley A (2009) Cavitation occurrence around ultrasonic dental scalers. Ultrason Sonochem 16: 692-697.
- Walmsley AD, Lea SC, Felver B, King DC, Price GJ (2013) Mapping cavitation activity around dental ultrasonic tips. Clin Oral Investig 17: 1227-1234.
- Derdilopoulou FV, Nonhoff J, Neumann K, Kielbassa AM (2007) Microbiological findings after periodontal therapy using curettes, Er: YAG laser, sonic, and ultrasonic scalers. J Clin Periodontol 34: 588-598.
- Van Der Weijden GA, Hioe KPK (2005) A systematic review of the effectiveness of self-performed mechanical plaque removal in adults with gingivitis using a manual toothbrush. J Clin Periodontol 32: 214-228.
- Zimmer S, Nezhat V, Bizhang M, Seemann R, Barthel C (2002) Clinical efficacy of a new sonic/ultrasonic toothbrush. J Clin Periodontol 29: 496-500.
- Lazarescu D, Boccaneala S, Illiescu A, De Boever JA (2003) Efficacy of plaque removal and learning effect of a powered and a manual toothbrush. J Clin Periodontol 30: 726-731.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 10413
- [From(publication date):
November-2016 - Apr 19, 2025] - Breakdown by view type
- HTML page views : 9327
- PDF downloads : 1086