Research Article Open Access
Effects of Eccentric Exercise and Extracorporeal Shock Wave Therapy onRehabilitation of Patients with Noncalcific Rotator Cuff Tendinopathy
Tien-Wen Chen1, Jyong-Huei Su2, Tz-Yan Lin1, Cheng-Wei Lin3, Pei-Shi Chou4 and Mao-Hsiung Huang2*1Department of Physical Medicine and Rehabilitation, Kaohsiung Municipal Ta-Tung Hospital, Kaohsiung City, Taiwan1Department of Physical Medicine and Rehabilitation, Kaohsiung Municipal Ta-Tung Hospital, Kaohsiung City, Taiwan
2Department of Physical Medicine and Rehabilitation, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Taiwan
3Department of Physical Medicine and Rehabilitation, Kaohsiung Municipal Siaogang Hospital, Kaohsiung City, Taiwan
4Department of Orthopedic Surgery, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Taiwan
- *Corresponding Author:
- Mao-Hsiung Huang
Department of Physical Medicine and Rehabilitation
Kaohsiung Medical University Hospital, Kaohsiung, Taiwan
No.100 Tzyou 1st Road, Kaohsiung 807, Taiwan
Tel: +886-07-3121101
Fax: +886-07-3208211
E-mail: maohuang@ms24.hinet.net
Received date: November 30, 2016; Accepted date: December 20, 2016; Published date: December 29, 2016
Citation: Chen TW, Huei Su J, Lin TY, Lin CW, Chou PS et al. (2017) Effects of Eccentric Exercise and Extracorporeal Shock Wave Therapy on Rehabilitation of Patients with Noncalcific Rotator Cuff Tendinopathy. Clin Res Foot Ankle 5:222. doi: 10.4172/2329-910X.1000222
Copyright: © 2016 Huang MH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
Objective: In this study, in order to establish a more effective therapeutic model for the patients with chronic rotator cuff tendinosis, the authors attempted to compare the therapeutic effects of general physical therapy, eccentric contraction exercise, extracorporeal shock wave therapy (ESWT) and their combination for patients with noncalcific subscapular tendinosis.
Methods: 120 patients with subscapular tendinosis Grade II tendinopathy were divided randomly into four groups: I-IV, with 30 patients in each group. In group I (GI): the patients received conventional rehabilitation program, which included 20 minute of local hot packs, 15 min interferential electrotherapy and 10 min of passive range motion exercise three times weekly for 8 weeks; in Group II: the patients received eccentric contraction exercise three times per day and a rehabilitation program as in GI; in GIII: the patients received ESWT therapy weekly except for a rehabilitation program as in GI; in GIV: they received three combination therapies including a conventional rehabilitation program, three rounds of eccentric contraction exercises per day and weekly ESWT for 8 weeks. The outcome measurements include visual analogue pain scale (VAS), range of shoulder motion, subscapular muscle peak torques, and proprioception of the affected shoulder.
Results: The results showed that the combination therapy group GII-IV all had more improvement than the conventional rehabilitation program group I. However, the integrated therapy group IV had the best improvement over GII and GIII in pain reduction and improvement of range of motion, proprioception and muscle peak torques. Additionally, group III and IV had better improvement of range of motion and muscle peak torques than did GII.
Conclusion: Eccentric exercise and ESWT had benefit in rehabilitation of patients with noncalcific subscapular tendinosis, and conventional rehabilitation combined with these two therapies will result in more therapeutic effects.
Keywords
Extracorporeal shock wave; Non-calcific tendinopathy; Eccentric contraction exercise
Introduction
Shoulder pain is a common problem with up to half of the population experiencing this at least once per year [1]. The prevalence of rotator cuff (RC) disease has been shown to increase as a function of age starting at 40 years [2-3], and to exceed as much as 50% by the age of 60 years [4]. The pain and disability resulting from RC disease has an impact on health-related quality of life [5].
Although the causes of such tendinopathies are still not well known [6], different intrinsic factors such as anatomical variants, muscle imbalance, nutrition, age and joint laxity [7], and extrinsic factors such as occupation, physical load and overuse, technical errors, inadequate equipment and environmental contributing to the pathologic processes have been identified. It is recognized that most tendinopathies are rarely caused by a single factor, and the process that precedes tendon rupture may result from a variety of different pathways and etiological factors [8]. Aging can cause a decrease in mean collagen fibril diameter and the size shift may be related to the reduction of mechanical strength of older tendons [9].
RC tendinopathy has been classically described as a progressive disorder of RC tendons that begins with an acute tendinitis, progresses to tendinosis with degeneration and partial thickness tears, finally resulting in full thickness rupture [10-11]. The tendinosis is a degenerative pathological condition with lack of inflammatory change and failed healing response, with haphazard proliferation of tenocyted, intracellular abnormalities in tenocytes, disruption of collagen fibers, and subsequent increase in non-collagenous matrix [11].
The conservative treatment of RC diseases includes exercise alone or in combination with a multimodal rehabilitation program, which includes the use of anti-inflammatory drugs, rest and stretching and strengthening exercises [12]. Regardless of treatment, more than a third of patients do not have a successful outcome with continuing persisted pain and disability [13].
The eccentric contraction training consists of the contraction of a muscle for controlling or decelerating a load while the muscle and the tendon are stretching or remaining stretched. Eccentric exercises have been proposed to promote collagen fiber cross-link formation within the tendon, thereby facilitating tendon remodeling, and have been suggested as counteracting the failed healing response that underlies tendinopathy [14].
It is possible that eccentric contraction exercises do not just exert a beneficial mechanical effect, but act on pain mediators as well, decreasing their presence in tendinopathic tendons [15].
The technique has been advocated as a treatment of tendinopathies, such as chronic Achilles, patellar, lateral humeral epicondylalgia and rotator cuff tendinopathy [16-18].
Extracorporeal shockwave therapy has emerged as an alternative therapy either when conservative treatment fails or when introduced prior to invasive procedures for rotator cuff disease, and its efficacy and low morbidity is well demonstrated [19-23].
It is thought that hyperstimulation analgesia can be achieved with energy densities that are lower than those required to disintegrate calcific deposits, and another rationale for use of shock wave for noncalcific RC tendinopathy relates to the suggestion that pain is caused by hypovascular change [24].
Shock wave therapy can decrease pain by increasing neovascularization and improving tissue regeneration [25-26].
Though the most common site of calcific deposits in rotator cuff tendinopathy diagnosed by plain radiography and sonography is revealed to be supraspinatus, the second site is subscapularis and the tertiary site then infraspinatus as reported by Goff [27], the same incidence of initial noncalcific tendinopathy has been reported by Kim [28].
However, the secondary site tendinosis has high prevalence in aging which makes it hard for dressing and solid application of hygiene practice in daily activity while the internal rotation of movement needed.
There were many clinical reports related to the effects of ESWT or eccentric exercise for rotator cuff tendinosis included supraspinatus [29-32], infraspinatus [33] and subacromial impingement syndrome [34]. However, there was few report related with subscapular tendinosis.
In order to establish a more effective therapeutic model for patients with chronic tendinosis, in the present study, the authors attempted to compare the therapeutic effects of conventional rehabilitation, eccentric contraction exercise, shock wave therapy and their combination for patients with chronic subscapular tendinosis.
Materials and Methods
120 patients with subscapular tendinosis Grade II tendinopathy according to high-definition ultrasound classification [35] were recruited from the clinic of the department of Rehabilitation Kaohsiung Medical University Hospital, Taiwan.
All participants gave informed consent for the study, and the study protocol was approved by the Ethical Review Committee of Kaohsiung Medical University.
Patients with previous humerus fracture, or other rotator cuff tendinopathy or adhesive capsulitis were excluded. The patients were divided randomly into four groups: I-IV, 30 patients in each group. In group I (GI): the patients received traditional rehabilitation program, which included 20 min of local hot pack s, 15 min of interferential electrotherapy and 10 min of passive range motion exercise three times weekly for 8 weeks; in Group II: the patients received three rounds of eccentric contraction exercises per day for 8 weeks and a conventional rehabilitation program as in GI; in GIII: the patients received ESWT therapy weekly and a conventional rehabilitation program as in GI; in GIV: the patients received three combination therapies including the conventional rehabilitation program, three rounds of eccentric contraction exercises per day and weekly shock wave therapy for 8 weeks.
The outcome measurements include the visual analogue pain scale (VAS), range of shoulder motion, subscapular muscle peak torques, and proprioception of the affected shoulder. The measurements were performed before and after treatment and at follow-up 3 months later.
Sonography assessments of the shoulder
The procedure protocol was fixed and performed by a single physiatrist. The data were recorded from the left shoulder then the right shoulder on a specific data collection sheet. The ultrasound examination was performed using an ultrasound machine with 10-16 MHz linear probe.
The protocol for ultrasound examination of the shoulder is laid out below, and is based upon the recommendation of the Nuffield orthopedic centre musculoskeletal radiology unit protocol [36].
It is performed from standing behind the patient who seated on a stool to allow easy movement of the arm. For further confirmation of the subject with subscapular tendinopathy only, the biceps and supraspinatus were routinely surveyed to exclude the subjects with combined tendinopathy.
Examination of long head of biceps: The hand is placed on the thigh with the palm facing upwards. The biceps tendon is found in the intertubercular groove of the humerus. Comment is made on the presence of the tendon, any fluid surrounding the tendon and the stability of the tendon in the grove when the arm is externally rotated.
Examination of subscapularis: With the arm maximally externally rotated the subscapularis tendon is viewed in the transverse and longitudinal planes from its insertion on the lesser tuberosity to the point at which it becomes hidden behind the coracoid process.
The quality of the tendon and the presence/absence of a full thickness tear are noted.
Examination of the supraspinatus tendon: The subject’s hand is placed on their back with the palm facing the lumbar spine. This extends and internally rotates the shoulder bringing the tendon out from underneath the acromion where it can now be visualized using ultrasound.
The tendon is examined anteriorly in a near sagittal plane as it inserts into the greater tuberosity, and in the transverse plane from the leading edge backward. Any fluid in the overlying bursa is commented upon, along with tendon quality and presence of full-thickness tear. If a full thickness tear is present this is measured on the transverse view, and recorded in cm.
Radiographic assessments of the shoulder
All patients underwent affected shoulder radiographic images at anterior-posterior view, and axillary view. These images were optimized for evaluation of bony structures and their related position deviated by the rotator cuff tendinopathy.
Shoulder ROM measurement
A goniometer was used to measure the cervical active ROM (AROM); the patients were seated in a chair in an upright position and did some warm-up exercises before measurement.
Using a universal goniometer, the examiner measured shoulder AROM in flexion-extension, abduction, external and internal rotation three times.
Then the mean values of the three measurements of total flexionextension, abduction, external and internal rotation were calculated and recorded. All these clinical measurements were done by one of the authors, a rehabilitation physician, without any information from the patients’ radiographs.
Measurement of pain severity
The severity of neck pain was evaluated by the VAS after patients had remained in a sitting upright posture with back support. The instrument consisted of horizontal lines 10 cm long, with anchor points of 0 (no pain) and 10 (maximum pain).
Measurement of muscle peak torque
Isokinetic strength testing was performed using a Kin-Com dynamometer (Kin-Com 505, Chattanooga, TN, US) before and after treatment and follow-up. The patient was seated upright on an adjustable stool with back support and a footrest, tested at 60 degrees/sec in 3 axes of movement: flex/extension, abduction/ adduction, and external/internal rotation. Each person performed 3 maximum-effort shoulder movements, and peak torque was recorded for each of the three axes of movement.
Measurement of proprioception
Position sense was tested by moving the extremity by passive robotic control at a constant angular velocity of 2 degrees/second to a predetermined angle, holding it in that position for 5 seconds, and then returning to the start position.
The arm was then brought through a similar range of motion until the patient identified the angle by pressing a button to disengage the device. An electronic goniometer recorded the actual and perceived angles. Three trials were performed for each axis.
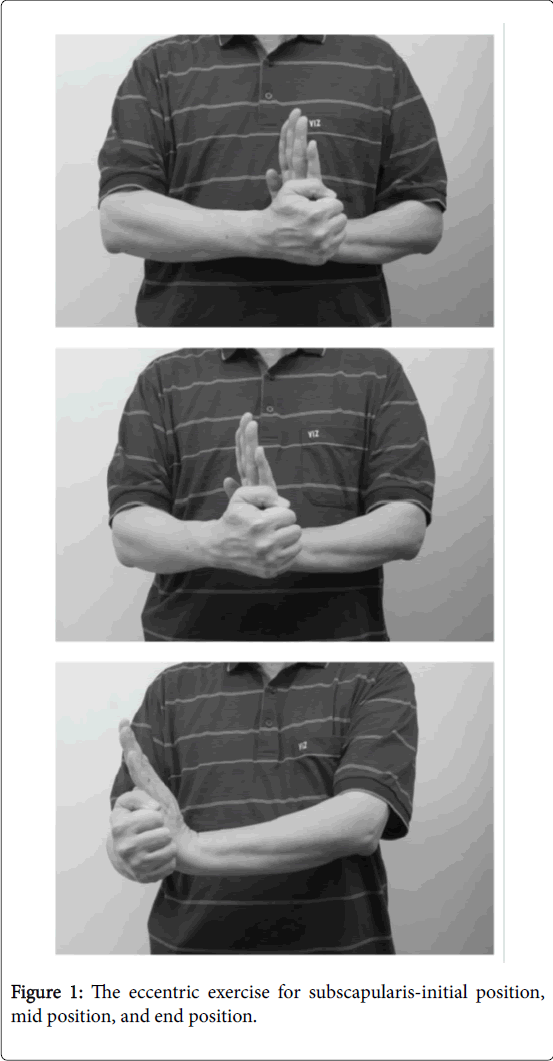
The eccentric exercise for subscapularis
For set up a more convenience home eccentric exercise program, a home eccentric contraction exercise program introduced as followed:
The patient was kept in a sitting position with affected shoulder kept in natural position, with elbow flexion at 90 degrees. The exertional internal eccentric contraction of subscapular muscle was started from the position of the fist just over the abdomen and pushing of the fist externally by the other wrist till the position of fist reached to 90 degrees from the initial position (Figure 1).
Twenty repetitions were performed each time, three rounds per day at home for 8 weeks.
The treatment of extracorporeal shock wave (ESWT)
The patient was kept in a sitting position. ESWT was performed with a piezoelectric shockwave generator (F10G4 Richard Wolf GmbH, Knittlingen, Germany).
The dose of ESWT applied was according to the general therapeutic dose for fibrotic tendinopathy [37], and the level of density depended on the size of the fibrotic tendon.
In present study, an impulse energy flux density around the average of 0.27 mJ/mm2 (ranging from scales of 15–18/20), with frequency range of 1–8 Hz and a pressure range from 11–82 MPa.
Patients in Group II and IV received ESWT 1000 impulses for subscapular tendon weekly for 8 weeks. The location and the depth of the probe of shock wave applied were guided by X-ray image and sonography.
Statistical analysis
A paired Student’s t-test was used to study the changes in ROM, VAS, MPT and Proprioception in each group immediately after treatment and at follow-up 3 months later compared to initial respectively. A one-way ANOVA with the Tukey test was used to compare the differences in ROM, VAS, MPT and proprioception between treated groups. A statistically significant difference was defined as p <0.05.
Results
Improvement of active range of motion (ROM)
The changes of active range of motion (internal plus external rotation) of the shoulder are showed in Table 1. The average active range motion of affected shoulders was improved in each group after treatment, and combination therapy group GII-IV showed more improvement than the conventional rehabilitation group I. However, the integrated therapy group IV had better improvement than GII and GIII and shock wave therapy group III was better than eccentric therapy group GII.
| I (n=30) | II (n=30) | III(n=30) | IV(n=30) | |
| Before | 119±10 | 119 ±12 | 118±12 | 120 ±14 |
| After | 128±12* | 138±16* | 143±12* | 160 ±17* |
| Follow-up | 130±12 | 145±16† | 150±12† | 165 ±17‡ |
†:Significant difference of ROM of each group compared with the control group at various time periods (p<0.05)
‡: Significant difference compared with other treated groups (p<0.05)
( ):The number of knees in each group at various time periods
Table 1: The average ROM (internal plus external rotation) of shoulders in each subject group before and after treatment, and at follow-up. (Mean ± S.D).
Improvement of affected shoulder pain
The changes of the shoulder pain are showed in Table 2. The average VAS pain score of the affected shoulder were improved in each group after treatment, and additional therapy group GII-IV had more improvement than traditional therapy group I. Furthermore, the integrated therapy group IV had better improvement than GII and GIII and shock wave therapy group III showed better improvement than eccentric therapy group GII.
| I (n=30) | II (n=30) | III(n=30) | IV(n=30) | |
| Before | 6.7 ±1.3 | 6.4 ±1.4 | 6.6 ±1.5 | 6.5 ±1.4 |
| After | 5.0 ±1.3* | 3.8 ±1.3* | 3.6±0.7 * | 2.3 ± 0.6*‡ |
| Follow-up | 3.5±1.3 | 2.6 ±1.3 | 2.1 ±0.6 | 1.5 ±0.7‡ |
†: Significant difference of VAS of each group compared with the control group at various time periods (p<0.05)
‡: Significant difference compared with other treated groups (p<0.05)
( ): The number of knees in each group at various time periods
Table 2: The average VAS score of shoulder pain in each group before and after treatment, and at follow-up (Mean ± S.D).
Changes of muscle peak torque (MPT) of internal/ external rotation of shoulder
The changes of the muscle peak toques are showed in Table 3. The average MPT of the affected shoulder was improved in each group after treatment, and combination therapy group GII-IV had more improvement than traditional therapy group I. However, the integrated therapy group IV had best improvement over those in GII and GIII, and subjects in shock wave therapy group III had better improvement than those in eccentric therapy group GII.
| I (n=30) | II (n=30) | III (n=30) | IV (n=30) | ||
| 60°(In/Con) | Before | 68.9 ± 8.0 | 67.1±7.1 | 69.3±6.6 | 66.9±6.2 |
| After | 76.1±6.7* | 82.7±8.2 *† | 88.1±7.3*† | 98.2±9.0*†‡ | |
| Follow-up | 77.1±5.1 | 85.7±8.2 | 93.1±7.3 | 104.2±9.0‡ | |
| 60°(In/Ecc) | Before | 84.7±6.9 | 83.5±7.1 | 84.6±8.4 | 85.1±5.8 |
| After | 93.3±5.7 | 98.9±5.7*† | 107.4±5.3*† | 119.5±5.6*† ‡ | |
| Follow-up | 95.3±5.7 | 105.9±5.7 | 115.4±5.3 | 125.5±5.6 ‡ | |
| 60°(Ex/Con) | Before | 68.1±7.1 | 65.5±6.3 | 67.3±5.9 | 64.6±7.7 |
| After | 73.6±6.1 | 77.6±7.3 *† | 85.1±6.4*† | 91.6±6.3*†‡ | |
| Follow-up | 73.2±8.1 | 82.6±7.3 | 90.1±6.4 | 99.6±6.3‡ | |
| 60°(Ex/Ecc) | Before | 74.0±7.3 | 69.8±7.2 | 75.1±6.6 | 70.7±8.0 |
| After | 78.8±7.1 | 84.9± 8.4*† | 86.7±5.9*† | 92.8±6.7*†‡ | |
| Follow-up | 76.8±4.1 | 78.9± 8.4 | 90.7±5.9 | 97.8±6.7‡ |
†: Significant difference of peak torque in each group compared with the control atvarious time periods ( p<0.05)
‡: Significant difference compared with other treated groups (p<0.05)
( ): The number of knees in each group at various time periods
Table 3: The mean peak torque of shoulder internal/external (Ex/In) rotation in concentric and eccentric contraction at 60°/second in each group before and after treatment, and at follow-up (Nm).
The changes of proprioception of shoulder
The changes of proprioception of shoulder before and after treatment, and follow-up are showed in Table 4. The average proprioception of the affected shoulder was improved in each group after treatment, and combination therapy group GII-IV had more improvement than traditional therapy group I. However, the patients with eccentric exercise in II and IV showed better improvement than those in GI and GIII.
| I (n=30) | II (n=30) | III(n=30) | IV(n=30) | |
| Before | 7.7±1.2 | 7.9±1.8 | 7.8 ±1.6 | 8.1±1.5 |
| After | 6.3±1.2 | 4.7±1.2* | 5.0±1.7* | 3.8±1.0*‡ |
| Follow-up | 5.3±1.2 | 3.9±1.2 | 4.3 ±1.7‡ | 3.2 ±1.0‡ |
†: Significant difference of angle of each group compared with the control group at various time periods (p<0.05)
‡: Significant difference compared with other treated groups (p<0.05)
( ): the number of knees in each group at various time periods
Table 4: The degree of angle difference to research a target angle of shoulders in each group before and after treatment (mean ± S.D).
Discussion
Non-calcified tendinopathy generally includes degenerative processes determining tendinosis and partial tendon ruptures not eligible for surgery. The degenerative processes suffered by the muscles and tendons over the course of several years result in functional and structural disorders. Comparing the therapy effects in GI with GII, and GIII with GIV, the active ROM, pain severity, MPT and proprioception are more improved in GII than GI, and GIV than GIII as shown in Tables 1-4. This implies that eccentric exercises have significant effects for management of RC disease.
Three basic principles in an eccentric loading regime have been proposed including: first, the length of tendon: the tendon length increases when the tendon is pre-stretched, and less strain will happen on the tendon during movement; secondly is load: the strength of the tendon should increase by progressively increasing the load exerted on the tendon; and thirdly is speed: by increasing the speed of contraction, a greater force will be developed [38]. Possible mechanism that might explain the efficacy of eccentric loading include: firstly, the high –frequency oscillations in tendon force produced by eccentric contractions, the fluctuations in force may provide an important stimulus for the remodeling of the tendon [38]; second, the increase in fibroblast activity, acceleration of collagen formation, increase in type I collagen, collagen organization/alignment (remodeling of the tendon) [38-39] by muscular lengthening (stretching) and increase in the number of sarcomeres in series [40]; third, traction and consequent disappearance of neovessels [41] that lead to a lack of perfusion produced by the tendinosis. The therapeutic effects of eccentric contraction may be mediated through decreasing pathological increased capillary tendon flow without deterioration of local tendon microcirculation, but more evidence is warranted; and neuromuscular benefits through central adaptations and pain habituation may be considered. In many eccentric exercise studies, a weight or resistance band was used for eccentric exercise performance. For more convenience and practical for patients to performance the eccentric exercise anytime and anywhere without any equipment, a self-serial eccentric exercise was prescribed as shown in Figure 1. From the positive findings of presented study, the self-eccentric home exercise may be applied to other rotator cuff tendinopahty.
The mechanism of shockwave therapy is still not completely clear. The potential mechanisms of beneficial of ESWT was studied, including direct tissue trauma and cavitation, altered cell-membrane permeability, direct effect on nociceptors and peripheral nerve stimulation. Direct tissue trauma can have mechanical and chemical effects, the proposed beneficial effects showed it could cause the transient inflammatory response, disintegration of calcium and stimulation of tissue healing. Some studies investigated the effect in animal experiments had demonstrated that shockwave therapy enhance the angiogenesis-related factors (e.g., eNOS, VEGF and PCNA) which could induces neovascularization [42]. The results could early induce tendon healing after injury. Besides, the shock wave energy had impact force to destroy and clean the mucoid substance which formed followed repeated microtrauma or inflammation, and disturbed the healing of tendon or ligament injury. In our previous study, we had performed shock wave therapy on the rehabilitation of patients with knee osteoarthritis and cyamella formation over popliteal fossa, it showed significant effect on knee OA rehabilitation, and rehabilitation of cervical spondylosis patients with nuchal ligament calcification [43-44]. In present study, we try to apply ESWT on noncalcific subscapular tendinosis.
Comparing the therapeutic effects in GI with GIII, and GII with GIV, the active ROM, pain severity, MPT and proprioception more improved in GIII than G I, and GIV than GII. It implied that shock wave therapy had significant effects for management of non-calcific subscapular tendinopahty.
However, the clinical efficacy of ESWT in non-calcific tendinopathy is controversial. Some authors show that ESWT is not effective in these cases [31]. On the other hand, good results have been presented by Galasso [32] that analyzed the effect of ESWT in patients with noncalcific tendinopathy of the supraspinatus and affected by subacromial impingement syndromes stages I and II according to Neer by low energy ESWT [37]. The present results were compatible with these reports which implied that the effects of ESWT for tendinopahty are dose depended, in non-calcific tendinopahty, a low energy ESWT is more appropriated.
Beside, ESWT could be a valuable tool to relax the tightness of disorganization of the tendon fiber bundles and increase the range of motion of affected shoulder immediately after treatment as results showed in Table 1, and resulted more pain reduction in GIII and GIV at follow-up as showed in Table 2, and more MPT improvement in GIII and GIV at follow-up as showed in Table 3. ESWT could have a complementary role in the treatment of chronic RC tendinopathy.
Comparing the combination therapeutic groups II-IV, it showed that combing eccentric exercise and ESWT with traditional rehabilitation program got most therapeutic effects for noncalcific RC disease. It implied that after the shock wave energy impact force to destroy and clean the mucoid substance which formed followed repeated microtrauma or inflammation, and disturbed the healing of tendon, followed by the high-frequency oscillations in tendon force produced by eccentric contractions, provide an important stimulus for the remodeling of the tendon and increase in fibroblast activity, acceleration of collagen formation. The present integrated therapy for noncalcific RC disease results in more functional improvement included MPT and proprioception except pain reduction and range motion of the shoulder.
The limitation of the study was that the subjects recruited only focuses on patients with subscapular tendinosis Grade II tendinopathy according to high definition ultrasound classification. Multiple rotator cuff tendinopathy, more severe tendinopathy or calcific tendinopathy tried by the integrated therapy were warranted in the future.
In Conclusion, eccentric exercise and ESWT had benefit in rehabilitation of patients with noncalcific subscapular tendinosis, and conventional rehabilitation combined with these two therapies will result in more therapeutic effects.
References
- Luime JJ, Koes BW, Hendriksen IJ, Burdoorf A, Verhagen AP, et al. (2004) Prevalence and incidence of shoulder pain in the general population: a systematic review.Scand J Rheumatol 33:73-81.
- Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, et al. (1991) Magnetic resonance imaging of the shoulder. Sensitivity, Specificity and predictive value.J Bone Joint Surg Am 73:17-29.
- Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M (1995) Rotator cuff changes in asymptomatic adults.The effect of age, hand dominance and gender. J Bone Joint Surg Am 77:296-298.
- Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB (1995) Abnormal findings on magnetic resonance images of asymptomatic shoulder. J Bone Joint Surg Am 77:10-15.
- MacDermid JC, Ramos J, Drosdowech D, Faber K, Patterson S (2004) The impact of rotator cuff pathology on isometric and isokinetic strength, function, and quality of life. J Shoulder Elbow Surg 13: 593-598.
- Fredberg U, Stengaard-Pedersen K (2008) Chronic tendinopathy tissue pathology, pain mechanisms, and etiology with a special focus on inflammation. Scand J Med Sci Sports18:3-15.
- Yuan J, Wang MX, Murrell GA (2003) Cell death and tendinopathy.Clin Sports Med22:693-701.
- Riley G (2004) The pathogenesis of tendinopathy. A molecular perspective. Rheumatology 43:131-142.
- Fan L, Sarkar K, Franks DJ,Uhthoff HK (1997) Estimation of total collagen and types I and III collagen in canine rotator cuff tendons. Calcif Tissue Int 61:223-229.
- Tempelhof S, Rupp S, Seil R (1999) Age-related prevalence of rotator cuff tears in asymptomatic shoulder. J Shoulder Elbow Surg8:296-299.
- Arya S, Kulig K (1985) Tendinopathy alters mechanical and material properities of the Achilles tendon. J Appl Physiol108:670-675.
- Khan KM,Cook JL, Bonar F, Harcourt P,Astrom M (1999) Histopathology of common tendinopathies.Update and implications for clinical management. Sports Med 27:393-408.
- Brox JI, Gjengedal E, Uppheim G, Bohmer AS, Brevik JI, etal. (1999) Arthroscopic surgery versus supervised exercise in patients with rotator cuff disease(stage II impingement syndrome):a prospective, randomized, controlled study in 125 patients with a 2 1/2-year follow-up. J Shoulder Elbow Surg8:102-111.
- Maffulli N, Longo UG (2008) How do eccentric exercisework in tendinopathy? Rheumatology 47:1444-1445.
- Rees JD, Lichtwark GA, Wolman RL,Wilson AM (2008) The mechanism for efficacy of eccentric loading in Achilles tendon injury; an in vivo study in humans. Rheumatology 47:1493-1497.
- Jonsson P, Wahlstrom P, Ohberg L, Alfredson H (2006) Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc 14:76-81.
- Visnes H,Hoksrud A, Cook J, Bahr R (2005) No effect of eccentric training on jumper’s knee in volleyball players during the competitive season:a randomized clinical trial. Clin J Sport Med 15:227-234.
- Groisier JL, Foidart-Dessalle M,Tinant F, Crielaard JM,Forthomme B (2007) An isokinetic eccentric programme for the management of chronic lateral epicondylar tendinopahty. Br J Sports Med41: 269-275.
- Hsu CJ, Wang DY, Tseng KF, Fong YC, Hsu HC, et al.(2008)Extracorporeal shockwave therapy for calcifying tendinitis of shoulder. J Shoulder Elbow Surg 17:55-59.
- Ioppolo F, Tattoli M, Di Sante L, Venditto T, Tognolo L, et al. (2013) Clinical improvement and resorption of calcifications in calcific tendinitis of the shoulder after shock wave therapy at 6 months' follow-up: a systematic review and meta-analysis. Arch Phys Med Rehabil94:1699-1706.
- Louwerens JK, Sierevelt IN, van Noort A, van den BekeromMP (2014) Evidence for minimally invasive therapies in the managementof chronic calcific tendinopathy of the rotator cuff: a systematic review and meta-analysis. J Shoulder Elbow Surg23:1240-1249.
- Wang CJ, Yang KD, Wang FS, Chen HH, Wang JW (2003) Shock wave therapy for calcific tendinitis of the shoulder: a prospective clinical study with two-year follow-up. Am J Sports Med 31:425-430.
- Branes J, Contreras HR, Cabello P, Antonic V, Guiloff LJ, et al. (2012) Shoulder rotator cuff responses to extracorporeal shockwave therapy: morphological and immunohistochemical analysis. J Shoulder Elbow Surg 4: 163-168.
- Rompe JD, Burger R, Hopf C, Eysel P (1998) Shoulder function after extracorporal shock wave therapy for calcific tendinitis. J Shoulder Elbow Surg 7: 505-509.
- Wang CJ, Huang HY, Pai CH (2002) Shock wave-enhanced neovascularization at the tendon-bone junction:an experiment in dogs. J Foot Ankle Surg 41:16-22.
- Orhan Z, Alper M,Akman Y, Yavuz O,Yalciner A (2001) An experimental study on the application of extracorporeal shock waves in the treatment of tendon injuries: preliminary report. J Orthop Sci 6: 566-570.
- Goff BL, Berthelot JM, Guillot P, Glemarec J, Maugars Y (2010) Assessment of calcific tendonitis of rotator cuff by ultrasonography: comparison between symptomatic and asymptomatic shoulders. Joint Bone Spine 77:258-63.
- Kim HM, Dahiya N, Teefey SA, Middleton WD, Stobbs G, et al. (2010) Location and initation of degenerative rotator cuff tears: an analysis of three hundred and sixty Shouders. J Bone Joint Surg Am92:1088-1096.
- Zandt JF, Hahn D, Buchmann S, Beitzel K, Schwirtz A, et al. (2010) May eccentric training be effective in the conservative treatment of chronic supraspinatus tendinopathies? A review of the current literature. Sportverietz Sportsschaden 24: 190-197.
- Kim SY, Ko JB, Farthing JP, Butcher SJ (2015) Investigation of supraspinatus muscle architecture following concentric and eccentric training. J Sci Med Sport 18:378-382.
- Efe T, Felgentreff M, Heyse TJ, Stein T, Timmesfeld N, etal. (2014)Extracorporeal shock wave therapy for non-calcific supraspinatus tendinitis-10 –year follow-up of a randomized placebo-controlled trial.Biomed Tech 59:431-437.
- Galasso O, Amelio E, Riccelli DA, Gasparini G (2012) Short-term outcome of extracorporeal shock wave therapy for the treatment of chronic non-calcific tendinopahty of the supraspinatus: a double-blind, randomized, plabebo-controlled trial. BMC Musculoskeletal Disord 13:86-95.
- Oyama S, Myers JB, Blackburn JT, Colman EC (2011) Changes in infraspinatus cross-sectional area and shoulder range of motion with repetitive eccentric external rotator contraction. Clin Biomech 26:130-135.
- Bernhardsson S, Klintberg IH, Wendt GK(2011) Evaluation of an exercise concept focusing on eccentric strength training of the rotator cuff for patients with subacromial impingement syndrome. Clinic Rehabil 25:69-78.
- Hinsley H, Nicholls A, Daines M, Wallace G, Arden N, et al. (2014) Classification of rotator cuff tendinopathy using high definition ultrasound. Muscles Ligaments Tendons J 4:391-397.
- Iannotti JP, Ciccone J, Buss DD, Visotsky JL, Mascha E, et al. (2005) Accuracy of office-based ultrasonography of the shoulder of rotator cuff tear. J Bone Joint Surg Am87:1305-1311.
- Speed CA (2004) Extracorporeal shock-weve therapy in the management of chornic soft-tissue conditions. J Bone Joint Surg Br86:165-171.
- Peers KH, Lysens RJ (2005) Patellar tendinopathy in athletes:current diagnostic and therapeutic recommendations. Sports Med35:71-87.
- Jeffery R, Cronin J, Bressel E (2005) Eccentric strengthening : Clinical application to Achilles tendinopathy. New Zealand J Sports Med33:22-30.
- Whitehead NP, Allen TJ, Morgan DL, Proske U (1998) Damage to human muscle from eccentric exercise after training with concentric exercise.J Physiol 512:615-620.
- Ohberg L, Alfredson H (2004) Effects on neovascularization behind the good results with eccentric training in chronic midportion Achilles tendinosis?. Knee Sury Sports Traumatol Arthrosc12:465-470.
- Wang CJ, Wang FS, Yang KD, Weng LH, Hsu CC, et al. (2003) Shock wave therapy induces neovascularization at the tendon–bone junction: A study in rabbits. J Orthop Res21:984-989.
- Chen TW,Lin CW, Lee CL, Lin ZY, Chen CH, et al. (2014) Effects of shock wave therapy in patients with knee osteoarthritis andpopliteal cyramella. Kaohsiung J Med Sci30:362-7.
- Lin TY, Chen JT, Chen YY, Chen TW, Lee CL, et al. (2015) The efficacy of ultrasound-guided extracorpal shock wave therapy in patients with cervical spondylosis and nuchal ligament calcification. Kaohsiung J Med Sci 31:337-343.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 6183
- [From(publication date):
March-2017 - Mar 29, 2025] - Breakdown by view type
- HTML page views : 5134
- PDF downloads : 1049