Effects of a Twelve-Week Program of Lumbar-Stabilization Exercises on Multifidus Muscles, Isokinetic Peak Torque and Pain for Women with Chronic Low Back Pain
Received: 26-Jan-2018 / Accepted Date: 31-Jan-2018 / Published Date: 07-Feb-2018 DOI: 10.4172/2167-0846.1000309
Abstract
Objective: This study aim was to evaluate the effects of the lumbar stabilization exercises on cross-sectional area (CSA) of the multifidus muscle, trunk muscles’ isokinetic peak torque, pain and disability in women with chronic low back pain (cLBP).
Methods: The experimental group (EG; n=55) was enrolled in a 12-week lumbar stabilization exercises program. Control group (CG; n=51) did not undertake exercises. Before starting the exercise program, after completing it and 1 and 2 months after the intervention the following tests were carried out: isokinetic peak torque at an angular velocity of 60 deg/s was measured using a isokinetic dynamometer; measurement of the CSA of the multifidus muscle was performed using a ultrasound system, and patients were assessed using the Oswestry Disability Index (ODI), as well as visual analogue pain (VAS) rating scales.
Results: After intervention, isokinetic peak torque (41.25% extension and 21.53% flexion) and multifidus muscle CSA (right side: 37.41 ± 0.7%; left side: 37.53 ± 0.7%) increased, VAS (44.00%) and ODI (48.74%) decreased.
Conclusion: After 12-week lumbar stabilization exercises program, multifidus muscle CSA and trunk muscles peak torque increased, disability and cLBP decreased, and these changes lasted for 2 months.
Keywords: Lumbar stabilization exercise; Chronic low back pain; Isokinetic trunk flexion and extension
Introduction
Chronic low back pain (cLBP) is one of the most prevalent musculoskeletal disorders and it enhances the economic burden [1]. Over the last decade, a number of studies have reported dysfunction of voluntary activation of multifidus and abdominal muscles in connection with recurrent or cLBP [2-4]. Patients with cLBP show reduced endurance and strength of the muscles of the lumbar and hip, and decreased flexibility of the back as a result of prolonged anomalous posture, which may account for the pain [5]. A common variation is a delay in activation of the deep muscles (transversus abdominis, obliquus internus abdominus) only during rapid voluntary limb movements [6,7].
There is evidence that patients with cLBP have a smaller crosssectional area (CSA) of the multifidus muscles compared to healthy volunteers [8-11]. The multifidus muscles act as lumbar stabilizers and control the intersegment motion of individual vertebrae [12]. Ultrasound imaging has been proved as a non-invasive method to take the measurements of the activation of selected muscles [13]. Using ultrasound imaging and magnetic resonance imaging for a research of healthy young females showed that the multifidus muscles are symmetrical on either side of each vertebral level studied (L2-S1) and grew in size from L2 to L5 [14]. A systematic review by Fortin and Macedo showed that patients with cLBP have smaller multifidus and paraspinal muscle groups than healthy subjects [12]. Dysfunction of the lumbar multifidus muscles is closely associated with cLBP as it is likely to be due to pain inhibition from the spine [15]. Perhaps future studies will determine whether muscle atrophy is a cause or a result of cLBP [12].
The stability of the lumbar spinal segments is an important component of the biomechanics of the body, a deficiency of which can affect the occurrence of cLBP [16]. Hides et al. measured the response to an abdominal drawing-in task of CSA of the waist, the thickness of the internal oblique and transversus abdominis muscles and the shortening of the transversus abdominis muscle and found changes in the measurements between the beginning and the finish of a 13- week cricket training camp [10]. In this research the subjects made 13-week practice of individual skills, gym sessions and weight training. Participants from the group with cLBP experienced with a 6-week stabilization training program which included performing voluntary contractions of the multifidus, pelvic floor and transversus abdominis muscles while obtaining feedback from ultrasound imaging. The motor control of cricketers with cLBP who obtained the stabilization training improved and was similar to that of the cricketers without cLBP in the end of the training.
Stuge et al. established that a group who performed specific stabilizing exercises (20 weeks) showed statistically and clinically lower pain intensity, lower disability, and higher quality of life contrast to a control group (group received individualized physical therapy without specific stabilizing exercises), after intervention and at one-year postpartum [17]. While changes were negligible in the control group, disability was reduced by more than 50% in the exercise group.
Smith et al. study indicated that lumbar extension training with pelvic stabilization can be an effective treatment for cLBP, however lumbar extension training without pelvic stabilization did not increase lumbar muscle strength. Stabilization of the lumbar spine significantly increases back extensor muscle strength, reduces soreness and improves outcomes as measured by the Oswestry Disability Index (ODI) [18]. These results show that the lumbar stabilization exercise program is effective for the treatment of cLBP with the aim of preventing the recurrence of symptoms [19]. It is therefore important to assess the lasting impact of exercise programs on the treatment of cLBP. The lumbar stabilization exercises have been designed in order to enhance the neuromuscular control system and correct the dysfunction [20]. The Pilates method can be used as an adjunctive lumbar stability exercise program to improve flexibility and enhance control of trunk and pelvic segments and core stability [21].
The main aim of this study was to evaluate the effects of a program of lumbar stability exercises on multifidus muscles in parallel on both sides of the spine in the L4-L5 region, isokinetic peak torque of flexor and extensor of trunk muscles, pain and functional condition in women with cLBP. We also assessed changes in trunk muscle size and strength up to 2 months after completing a 12-week training program.
We hypothesize a 12-week lumbar stabilization program for women with cLBP will decrease and this effect will persist after two months.
Materials and Methods
One hundred-six female volunteers suffering non-specific cLBP were divided randomly from an experimental group (EG; n=55) and a control group (CG; n=51). All subjects had been suffering from cLBP for at least 3 months. The study did not include patients with neurological symptoms, spinal damage, cancer or infectious diseases that could lead to cLBP, and other diseases that could affect physical performance. Those who had paresthesia, myoparalysis, or psychological problems as well as those who had difficulty in performing exercise due to lack of comprehension were also excluded. None of the study participants had undergone surgery for cLBP. Participants in the CG and EG groups had not performed lumbar stabilization exercises before. The mean age of the EG subjects was 53.3 ± 5.3 years, their body weight was 68.1 ± 8.9 kg, height 166.4 ± 2.8 cm. The CG included women aged 51.5 ± 7.4 years, with a body weight of 65.1 ± 6.4 kg, and a height of 167.5 ± 1.9 cm. The EG subjects were enrolled in a 12-week exercise program to increase lumbar stability. None of the women had previously been involved in similar studies. All subjects were asked not to use any medication, such as muscle relaxants, analgesics, and psychotropic drugs, for at least 4 days before testing.
Inclusion criteria of EG are as follows:
• cLBP persisting for more than 3 months in the absence of an underlying pathology
• Aged between 51 and 58 years
• Pain between 3 and 6 at rest on a 0- to 10-point pain visual analog scale (VAS), where 0 represents no pain and 10 is the worse pain imaginable
• No contraindication for exercise
• No obvious deformity of the spine, pelvis, and lower extremities
• No autoimmune diseases (e.g., rheumatoid arthritis)
• No pregnancy
CG women did not undertake lumbar stabilization exercises program. This study was approved by Regional Biomedical Research Ethics Committee. Each volunteer read and signed the informed consent form before participation in the study.
Before starting the lumbar stabilization exercise program, after completing it and 1 and 2 months after the intervention the following tests were carried out: isokinetic peak torque at an angular velocity of 60 deg/s was measured using a Biodex System 3 Pro isokinetic dynamometer; measurement of the cross-sectional area of the multifidus muscle was performed using a TITAN™ ultrasound system, and patients were assessed using the ODI, as well as VAS rating scales.
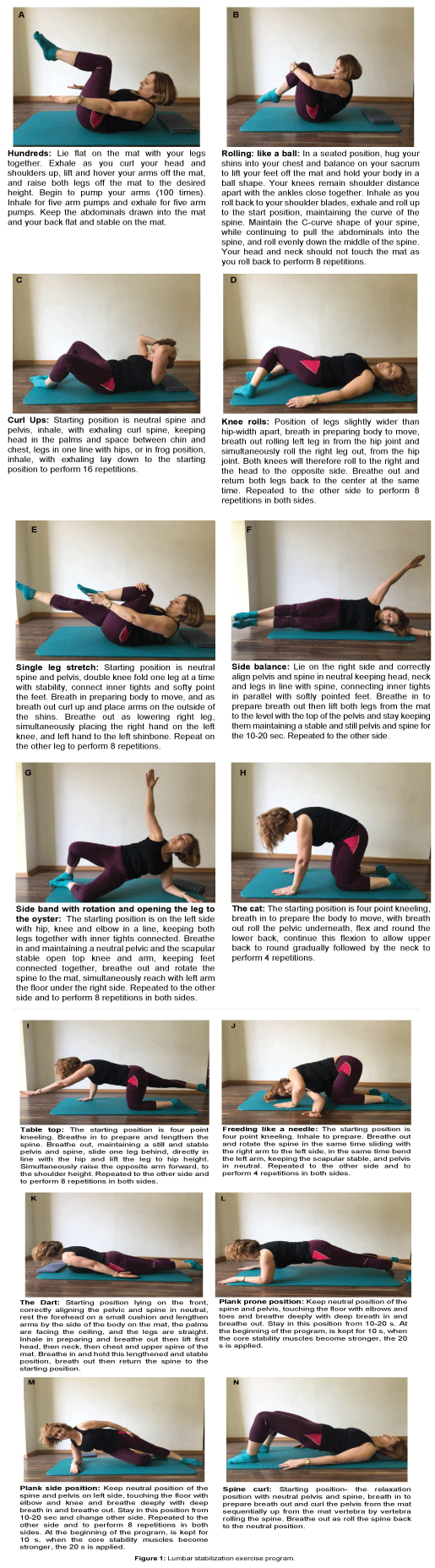
Lumbar stabilization exercises were performed twice per week; the duration of each session was 45 min. The program lasted for 12 weeks, thus patients underwent a total of 24 exercise sessions. Exercise program consisted from stretching, pelvic tilt, flexion and extension strengthening of the abdomen and the trunk muscles. The subjects conducted the lumbar stabilization exercise program for 45 min. This program is divided into 3 categories: warm up, main part and cool down [22]. The EG participants were required to perform from 4 to 16 repetitions some of exercise. The physiotherapist controlled the subject’s lumbar neutral spine position at the start of each exercise, and the subjects were asked to keep this position through the exercise. The exercises were performed in a same order. Markers were placed on the floor to standardize the position of the subject and the equipment. The exercises met suggested criteria for safety; these included the avoidance of active hip flexion with fixed feet positioning and pulling with the hands behind the head and ensuring knee and hip flexion during all upper body exercises (Figures 1A-1N).
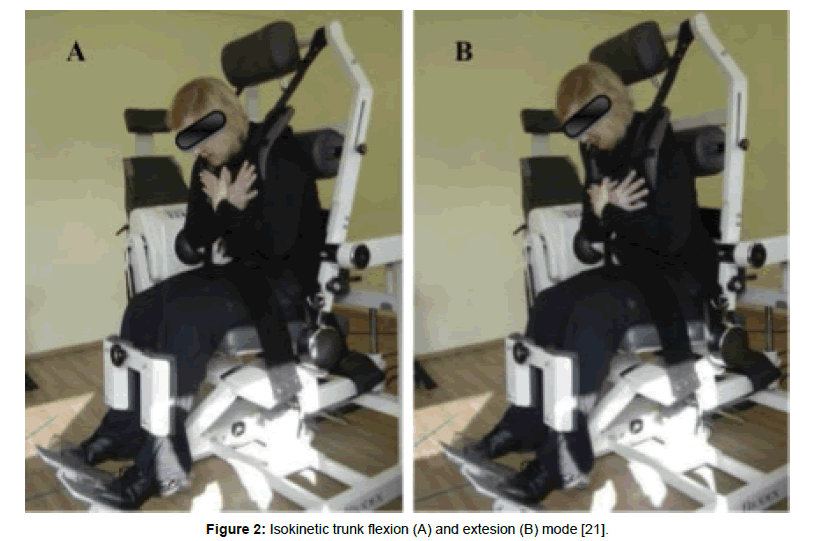
The subjects were tested using a Biodex Medical System PRO 3 dynamometer (certified ISO 9001 EN 46001; Shirley, NY, USA). Isokinetic peak torque was measured at an angular velocity of 60 deg/s [23,24]. Mechanical brakes were applied at 60° of amplitude in order to minimize unwanted movements [25]. Prior to testing, all subjects were familiarized with the methodology of the assessment and then performed a standard warm-up which involved exercising on the ergometer (Ergo-Fit Ergo Cycle 177, Germany) at low intensity for 5 min (heart rate 110-130 beats/min). After warming up, the subjects sat in the Biodex System 3 PRO chair (Figure 2) and remained quiet for 2 min. Shoulder, torso and thigh straps were used to maintain the angle between the waist and thigh at 90° [23]. During the test the subjects were asked to minimize head movements and keep hands crossed on the chest. After several practice movements followed by 5 min rest, volunteers performed maximal isokinetic voluntary trunk flexion involving three trunk flexion and extension movements using maximal effort. For data analysis we used the value indicating the highest maximal force.
Figure 2: Isokinetic trunk flexion (A) and extesion (B) mode [21].
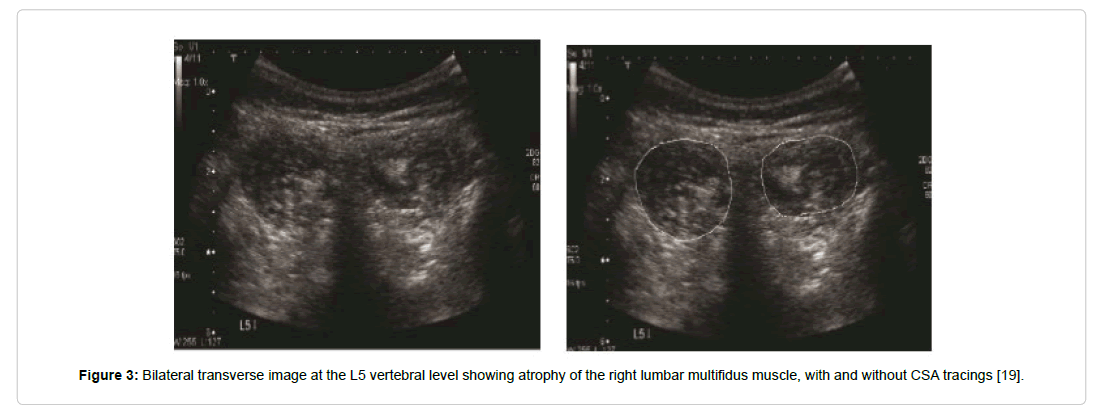
Ultrasound scanning of the muscles was carried out using a TITAN™ ultrasound system (SonoSite Inc., Bothell, WA, USA). Multifidus muscle CSAs (cm2) were measured in the B-scan mode. An HST/10-5 MHz 25 mm linear probe was used to image the surfaces of the muscles, organs and blood vessels, at a frequency of 10 MHz. During the study, subjects were positioned face down in a relaxed, neutral head position, with their arms relaxed at their sides. A small pillow was placed under the abdomen to reduce lordosis of the lumbar spine. Ultrasound scanning of multifidus muscles was performed in parallel on both sides of the spine in the L4–L5 region (Figure 3). The fourth lumbar vertebra (L4) was identified by palpation, starting from the wings of the hip bones towards the centre line [22,26].
Figure 3: Bilateral transverse image at the L5 vertebral level showing atrophy of the right lumbar multifidus muscle, with and without CSA tracings [19].
The ODI questionnaire was used to evaluate the influence of cLBP intensity on the patient’s functional state in different life situations. The ODI questionnaire was used to evaluate the influence of cLBP intensity on the patient’s functional state in different life situations [27]. Pain intensity was evaluated using a visual analogue pain scale (VAS) with a range of 0 to 10 points, where 0=no pain; 2=mild pain; 4=moderate pain; 6=severe pain; 8=very severe pain; and 10=unbearable pain [28,29].
The data were tested for normal distribution using the Shapiro- Wilk test, and all data were found to be normally distributed. A twoway mixed analysis ANOVA (General Linear Model) was used to determine the effect of the lumbar stabilization exercise program as within subject factor of two levels in group and between groups (CG and EG). A significant result was followed by LSD post hoc adjustment to determine differences between the lumbar stabilization exercisetraining conditions. If Mauchly's Test of Sphericity was significant then the Greenhouse-Geisser correction was used. The level of significance was set at p
Result
At the start of the study maximal isokinetic trunk extension and flexion peak torque did not differ between the EG and the CG (p>0.05). After completing the 12-week lumbar stabilization exercise program, trunk flexion (41.25 ± 9.25%) and extension (21.53 ± 4.48%) strength increased (p<0.001) in the EG. This increase in strength remained statistically significant after 1 month and 2 months post the lumbar stabilization exercise program. (p<0.05) (Table 1).
| Baseline | Post intervention | 1mth post LSEP | 2 mth post LSEP | |||||
|---|---|---|---|---|---|---|---|---|
| Group | Extension | Flexion | Extension | Flexion | Extension | Flexion | Extension | Flexion |
| Experimental (N = 25) | 153.42 ± 22.35 | 100.29 ± 22.24 | 216.70 ± 26.93*# | 121.88 ± 20.22*# | 194.93 ± 29.81*# | 119.15 ± 19.63*# | 168.46 ± 26.69*# | 112.53 ± 15.01*# |
| Control (N=11) | 137.64 ± 19.35 | 92.05 ± 18.91 | 140.15 ± 23.39 | 91.9 ± 16.55 | 132.78 ± 20.26 | 84.91 ± 15.88 | 131.75 ± 23.31 | 85.25 ± 13.42 |
| (*-Difference from the initial Peak torque values, p<0.05; #-Difference peak torque between the experimental and the control groups, p<0.05) (LSEP-lumbar stabilization exercise program) | ||||||||
Table 1: Values of maximal isokinetic trunk extension and flexion Peak Torque (Nm).
The isokinetic trunk flexion muscles post intervention of the lumbar stabilization exercise program significantly depended on the isokinetic trunk flexion muscle endurance baseline the intervention (r=0.552, p<0.05). The results of isokinetic trunk flexion muscle endurance tests significantly depended on the trunk extension muscle endurance baseline the intervention, and at 1 month post LSEP (r=0.734, p<0.001) and 2 month post intervention (r=0.781, p<0.001).
Initially, there was no significant difference in the CSA of the multifidus muscle CSA between the EG and the CG, either on the right side or on the left side (p>0.05). At the end of the 12-week exercise training program, the multifidus muscle CSA values were significantly higher on both the right side (45.24 ± 1.2%) and the left side (44.81 ± 0.9%) in women in the EG (p<0.05). This increase in multifidus muscle’s CSA was maintained after 1 month (right side: 39.45 ± 0.6%; left side: 40.12 ± 0.7%) (p<0.05) and 2 months (right side: 37.41 ± 0,7%; left side: 37.53 ± 0.7%) (p<0.05) (Table 2).
| Baseline | Post intervention | 1mth post LSEP | 2 mth post LSEP | |||||
|---|---|---|---|---|---|---|---|---|
| Group | Right side | Left side | Right side | Left side | Right side | Left side | Right side | Left side |
| Experimental (N = 25) | 6.57 ± 0.7 | 6.55 ± 0.9 | 9.12 ± 0.9*# | 9.38 ± 1.1£€ | 8.26 ± 0.6*# | 8.41 ± 0.7£€ | 7.46 ± 0.6*# | 7.53 ± 0.7£€ |
| Control (N=11) | 6.98 ± 1.2 | 7.04 ± 1.1 | 6.88 ± 1.2 | 6.99 ± 0.9 | 6.77 ± 0.8 | 6.78 ± 0.7 | 6.84 ± 0.8 | 6.87 ± 0.7 |
| (*-Difference from the initial values CSA right side, £-Difference from the initial values SCA left side, p <0.05; #-Difference between the experimental and the control groups SCA right side, p<0.05, £-Difference between the experimental and the control groups CSA left side, p<0.05) | ||||||||
Table 2: Values of cross-sectional area (cm2) of lumbar multifidus muscles.
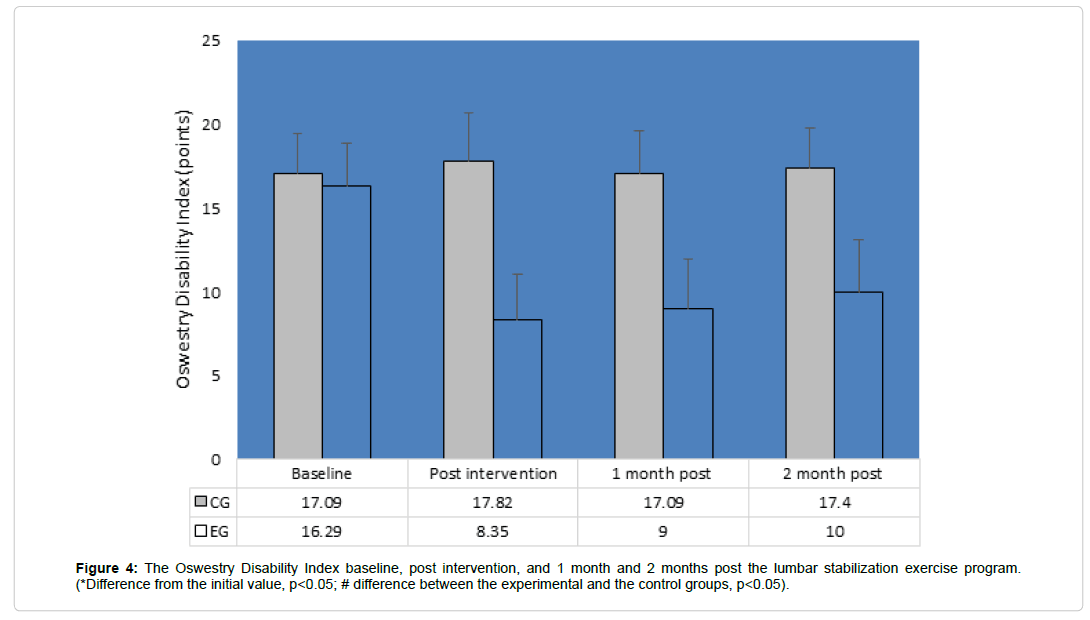
At the start of the study ODI scores did not differ (p>0.05) between the EG and CG groups. After completing the 12-week lumbar stabilization exercise program the ODI scores decreased by 48.74 ± 7.81% (p<0.05) in the EG, and this reduction persisted for 1 month and 2 months post the lumbar stabilization exercise program (Figure 4).
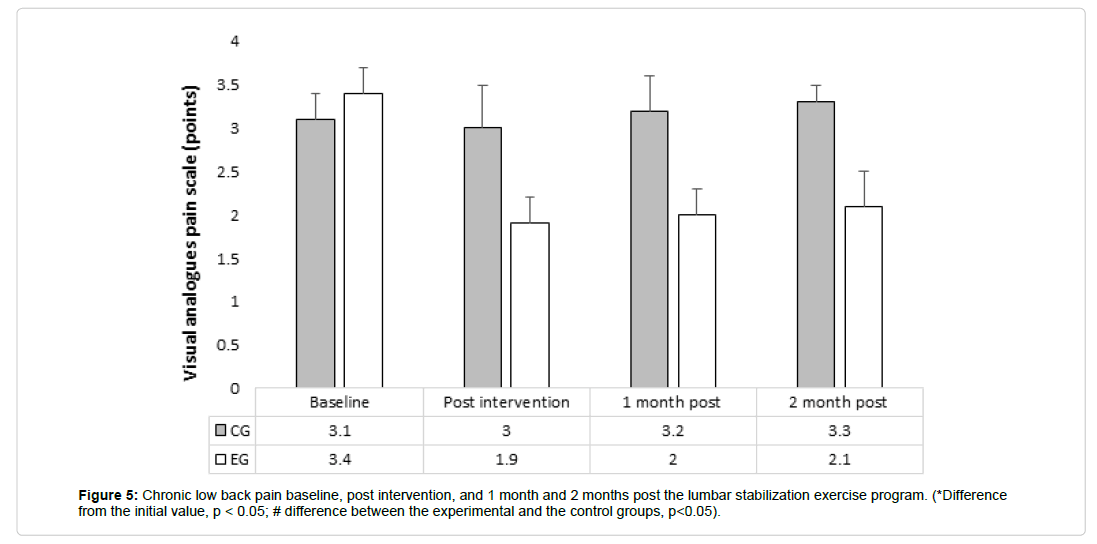
At the start of the study there was no significant difference in pain intensity between the EG and the CG (p>0.05). At the end of the 12- week exercise program, cLBP intensity decreased by 1.50 ± 0.3 (p<0.05) in the EG, and this reduction persisted for 1 month and 2 months post the lumbar stabilization exercise program (Figure 5).
Discussion
Our results show that the 12-week lumbar stabilization exercise program induces beneficial adaptations in women with cLBP. We found that multifidus muscle CSA and trunk muscle isokinetic peak torque increased while ODI decreased after this intervention, suggesting that lumbar stabilization exercises are effective in relieving cLBP. Previous studies have also shown that 4, 6, 10, 12, 16 or 20 weeks of the lumbar stabilization exercise program are effective for pain relief and improvement of trunk muscle function [17,18,22,23,30,31].
After completing the lumbar stabilization exercise program, back pain intensity and ODI decreased in the women in our study. Comparing the results obtained immediately after finishing the lumbar stabilization exercise program with the results after 2 months it was evident that without continuing lumbar stabilization exercises, the maximal isokinetic trunk flexion strength and maximal isokinetic trunk extension strength both decreased.
Our results showed a large increase in trunk muscle strength after completing the 12-week exercise program. It is likely that muscle strength was influenced by pain during initial measurements. Motor control might therefore change significantly as activity of the agonist muscles decreases while antagonist muscle activity increases to reduce speed, strength and amplitude of the movements in the presence of pain [6]. After lumbar stability exercise program on pain and active range of motion of trunk flexion increased significantly in the lumbar stability exercise group, but a significant increase was not found in the control group [31]. Gruther et al. considered that in chronic cLBP, dynamometric trunk muscle measures are limited to muscle functions evaluation purposes [32]. Goldby et al. applied a 10-week lumbar stabilization exercise program and collected data at baseline, and at 3, 6, 12, and 24 months after intervention [30]. Their results indicated statistically significant improvements in favour of the spinal stabilization group at the 6-month stage in pain (65.9% reduction in symptoms) and dysfunction, and at the 1-year stage in disability. In contrast, Unsgaard- Tøndel et al. found no significant group differences in pain, disability, trunk flexibility, or fear-avoidance beliefs after treatment 8 weeks of motor control exercises, sling exercises, and general exercises and at a 1-year follow-up in patients with chronic nonspecific cLBP [33]. In a recent scientific research was found that were no differences between lumbar stability exercise program and general exercises with regard to pain and functionality in nonspecific cLBP subjects, but general exercises were better than lumbar stability exercise program for increasing functionality and flexibility [34].
We found that the lumbar stabilization exercise program resulted in a significant increase in the cross-sectional area of the multifidus muscle CSA and strength of rectus abdominis and erector spine muscles for women in the EG and these increases were maintained for 2 months. The significant improvement in the ability to contract the transversus abdominis after a program of lumbar stabilization exercises concurs with the findings of Ferreira et al. [35]. In their study, 11 patients undertook stabilization exercise therapy, and a further 23 patients either performed general exercise or received spinal manipulation. Compared with the latter groups, the stabilization group showed significantly (r=-0.35; 95% CI 0.02 to 0.62) greater changes after intervention in the ability to recruit the transversus abdominis 7.8% than participants receiving general exercise 4.9% or spinal manipulative therapy 3.7%.
The pain intensity of cLBP in the women in the EG immediately after the intervention significantly correlated with maximal isokinetic trunk flexion strength and the ratio of isokinetic trunk extension and flexion strength. After 1 month without the lumbar stabilization exercise program, pain intensity significantly depended on the maximal isometric flexion strength. Gruther et al. established that among dynamometric tests, isokinetic measurements produced the best area under the curve for discriminating between patients with cLBP and healthy controls [32]. Above mentioned authors research showed that reliability testing revealed highly significant learning effects for isokinetic trunk flexion and isokinetic measurements. Sekendiz et al. found that stabilization program exercises were an efficient training method, producing a positive significant changes in abdominal and lower back strength, posterior trunk flexibility and abdominal muscular endurance in sedentary adult females [24]. The results showed a significant difference between pre- and post-exercise measurements with isokinetic dynamometer of abdominal and lower back peak torque at 60 deg/s flexion/extension and 120 deg/s flexion. The trunk muscle peak torque was measured at an angular velocity of 60 deg/s flexion/extension in our studies and also showed significant improvement after stabilization program exercises.
Our results demonstrate that 12 weeks of a lumbar stabilization exercise program involving 24 sessions carried out two times per week is effective in relieving cLBP and improving patients’ function. Even after a month without exercise, muscle CSA and strength remained elevated compared to the initial measurements and the CG which did not perform exercise training. Nevertheless, the program did not result in the permanent reduction of cLBP, which returned to previous levels within 2 months. Stuge et al. showed that the effect of 20 weeks of a specific stabilization exercise program reduced pain and level of disability and increased quality of life (ODI) compared to an exercise program without stabilization exercises [17]. They found that this improvement remained even after a year of inactivity. The most important factors for the treatment of cLBP, ensuring improvements in the patients’ functional state and maintaining its lasting effect are abdominal and back muscle static endurance, isometric abdominal muscle strength and similarity between trunk flexion and extension strength. The purpose of specific stabilization exercises is to improve the endurance and strength of muscles responsible for dynamic stabilization and neural-muscular control of the lumbar spine [10]. We found that, at 1 and 2 months after ending the lumbar stabilization exercise program, the pain intensified and functional state deteriorated much faster than the maximum trunk muscle strength, leading to the conclusion that to reduce pain and improve function, regular exercise, not only improved strength and endurance, is necessary. We established that, although the 12-week lumbar stabilization exercise program increased multifidus muscle CSA and trunk muscles peak torque increased, disability and cLBP decreased, and these changes lasted for 2 months.
The limitation of this study is its short duration, as the long-term effects of lumbar stabilization exercise program in patients with cLBP remain unknown after 6 months of suspended exercises.
Conclusion
After 12-week lumbar stabilization exercises program, multifidus muscle CSA and trunk muscles peak torque increased, disability and cLBP decreased, and these changes lasted for 2 months.
Conflict of Interests
The authors declare that they have no conflict of interest.
References
- Dagenais S, Caro J, Haldeman S (2008) A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 8: 8-20.
- Critchley DJ, Coutts FJ (2002) Abdominal muscle function in chronic low back pain patients. Physiother 88: 322-332.
- Pulkovski N, Mannion AF, Caporaso F, Toma V, Gubler, et al. (2012) Ultrasound assessment of transversus abdominis muscle contraction ratio during abdominal hollowing: A useful tool to distinguish between patients with chronic low back pain and healthy controls? Eur Spine J 21: 750-759.
- Mannion F, Caporaso F, Pulkovski N, Sprott H (2012) Spine stabilisation exercises in the treatment of chronic low back pain: A good clinical outcome is not associated with improved abdominal muscle function. Eur Spine J 21: 1301-1310.
- Leinonen V, Kankaanpää M, Airaksinen O, Hänninen O (2000) Back and hip extensor activities during trunk flexion-extension: Effects of low back pain and rehabilitation. Arch Phys Med Rehabil 81: 32-37.
- Hodges PW (2001) Changes in motor planning of feed forward postural responses of the trunk muscles in low back pain. Exp Brain Res 141: 261-266.
- Ferreira PH, Ferreira ML, Hodges PW (2004). Changes in recruitment of the abdominal muscles in people with low back pain: Ultrasound measurement of muscle activity. Spine 29: 2560-2566.
- Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, De Cuyper HJ (2000) CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J 9: 266-272.
- Kamaz M, Kiresi D, Oguz H, Emlik D, LevendoÄŸlu F (2007) CT measurement of trunk muscle areas in patients with chronic low back pain. Diag Inter Radiol 13: 144-148.
- Hides JA, Stanton W, McMahon S, Sims K, Richardson CA (2008) Effect of stabilization training on multifidus muscle cross-sectional area among young elite cricketers with low back pain. J Orthop Sports Phys Ther 38: 101-108.
- Wallwork TL, Stanton WR, Freke M, Hides JA (2009) The effect of chronic low back pain on size and contraction of the lumbar multifidus muscle. Man Ther 14: 496-500.
- Fortin M, Macedo LG (2013) Multifidus and paraspinal muscle group cross-sectional areas of patients with low back pain and control patients: A systematic review with a focus on blinding. Phys Ther 93: 873-888.
- Kiesel KB, Uhl TL, Underwood FB, Rodd DW, Nitz AJ (2007) Measurement of lumbar multifidus muscle contraction with rehabilitative ultrasound imaging. Man Ther 12: 161-166.
- MacDonald DA, Moseley GL, Hodges PW (2006) The lumbar multifidus: Does the evidence support clinical beliefs? Man Ther 11: 254-263.
- Freeman MD, Woodham MA, Woodham AW (2010) The role of the lumbar multifidus in chronic low back pain: A review. PM R 2: 142-146.
- Kumar SP (2011) Efficacy of segmental stabilization exercise for lumbar segmental instability in patients with mechanical low back pain: A randomized placebo controlled crossover study. N Am J Med Sci 3: 456-461.
- Stuge B, Lærum E, Kirkesola G, Vøllestad N (2004) The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: A randomized controlled trial. Spine 29: 351-359.
- Smith D, Bissell G, Bruce-Low S (2011) The effect of lumbar extension training with and without pelvic stabilization on lumbar strength and low back pain. J Back Musculoskelet Rehabil 24: 241-249.
- Hides J, Stanton W, Mendis MD, Sexton M (2011) The relationship of transversus abdominis and lumbar multifidus clinical muscle tests in patients with chronic low back pain. Man Ther 16: 573-577.
- McGill S (2007) Low Back Disorders. Evidence-based Prevention and Rehabilitation, Human Kinetics, Champaign, Illinois, Hardcover 312.
- Phrompaet S, Paungmali A, Pirunsan U, Sitilertpisan P (2011) Effects of Pilates training on lumbo-pelvic stability and flexibility. Asian J Sports Med 2: 16-22.
- Kliziene I, Sipaviciene S, Klizas S, Imbrasiene D (2015) Effects of core stability exercises on multifidus muscles in healthy women and women with chronic low-back pain. J Back Musculoskelet Rehabil 28: 841-847.
- Kliziene I, Sipaviciene S, Vilkiene J, Astrauskiene A, Cibulskas G, et al. (2016) Effects of a 16-week Pilates exercises training program for isometric trunk extension and flexion strength. J Bodyw Mov Ther 21: 124-132.
- Sekendiz B, Altun O, Korkusuz F, Akin S (2007) Effects of Pilates exercise on trunk strength, endurance and flexibility in sedentary adult females. J Bodyw Mov Ther 11: 318-326.
- Hartog D, Eker HH, Tuinebreijer WE, Kleinrensink GJ, Stam HJ, et al. (2010) Isokinetic strength of the trunk extensor muscles after surgical repair for incisional hernia. Hernia 14: 243-247.
- Stokes M, Rankin G, Newham DJ (2005) Ultrasound imaging of lumbar multifidus muscle: Normal reference ranges for measurements and practical guidance on the technique. Man Ther 10: 116-126.
- Fritz J, Irrgang J (2001) A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Phys Ther 81: 776-788.
- Dones I, Messina G, Nazzi V, Franzini A (2011) A modified visual analogue scale for the assessment of chronic pain. Neurol Sci 32: 731-733.
- Aoki Y, Sugiura S, Nakagawa K, Nakajima A, Takahashi H, et al. (2012) Evaluation of nonspecific low back pain using a new detailed visual analogue scale for patients in motion, standing, and sitting: Characterizing nonspecific low back pain in elderly patients. Pain Res Treat.
- Goldby LJ, Moore AP, Doust J (2006) A randomized controlled trial investigating the efficiency of musculoskeletal physiotherapy on chronic low back disorder. Spine 31: 1083-1093.
- Cho HY, Kim EH, Kim J (2014) Effects of the CORE Exercise Program on Pain and Active Range of Motion in Patients with Chronic Low Back Pain. J Phys Ther Sci 26: 1237-1240.
- Gruther W, Wick F, Paul B, Leitner C, Posch M, et al. (2009) Diagnostic accuracy and reliability of muscle strength and endurance measurements in patients with chronic low back pain. J Rehabil Med 41: 613-619.
- Unsgaard-Tøndel M, Fladmark AM, Salvesen Ø, Vasseljen O (2010) Motor control exercises, sling exercises, and general exercises for patients with chronic low back pain: a randomized controlled trial with 1-year follow-up. Phys Ther 90: 1426-1440.
- Mostagi FQRC, Dias JM, Pereira LM, Silva MF, Silva MAC, et al. (2015) Pilates versus general exercise effectiveness on pain and functionality in non-specific chronic low back pain subjects. J Bodyw Mov Ther 19: 636-645.
- Ferreira PH, Ferreira ML, Maher CG, Refshauge K, Herbert RD, et al. (2010) Changes in recruitment of transversus abdominis correlate with disability in people with chronic low back pain. Br J Sports Med 44: 1166-1172.
Citation: Sipaviciene S, Kliziene I, Pozeriene J, Zaicenkoviene K (2018) Effects of a Twelve-Week Program of Lumbar-Stabilization Exercises on Multifidus Muscles, Isokinetic Peak Torque and Pain for Women with Chronic Low Back Pain. J Pain Relief 7: 309. DOI: 10.4172/2167-0846.1000309
Copyright: ©2018 Sipaviciene S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15793
- [From(publication date): 0-2018 - Apr 18, 2025]
- Breakdown by view type
- HTML page views: 14442
- PDF downloads: 1351