Effectiveness of Oral Antipsychotic versus Long-Acting-Injectable Antipsychotics: A Comparison of Suicidality, Relapse, and Recidivism
Received: 01-Jan-1970 / Accepted Date: 01-Jan-1970 / Published Date: 04-Nov-2017 DOI: 10.4172/1522-4821.1000373
Abstract
Background: Long acting injectable antipsychotic (LAI) medication has been shown extensively to reduce relapse rates in schizophrenic patients previously treated with oral antipsychotics (OA). This study seeks to determine whether the long acting injectable mechanism, despite the drug-type being administered, is an effective treatment for all mental health (MH) disorders associated with psychosis; and moreover, whether it has the potential to improve patient suicidal ideation and overdose rates.
Methods: This was a retrospective chart review conducted on all patients being treated for a MH disorder with OA medication at a mid-sized community hospital in Oshawa, Ontario, Canada. Patients who switched from OA to LAI regimens between June 2014 and June 2015 were identified and included in the study. Relapse rates and patient outcomes were measured by a means of hospitalizations (ward admissions and emergency room (ER) visits) due to relapse, suicidal ideation, or intentional drug overdose. Data was collected in the form of frequencies for consecutive one-year periods on OA and LAI medications and then compared using descriptive statistics.
Result: Collectively, 92 patients met the inclusion criteria. The number of patients who were hospitalized at least once (ER visits and ward admissions) decreased by 54%, the frequency of suicidality by 60% and the number of drug over dose events by 71%. The median number of patients who visited the ER at least once decreased from 2 (0-16), to 0 (0-19), and the median number of patients who were admitted to the hospital at least once decreased from 1 (0-12), to 0 (0-10).
Conclusions: This study found that the LAI drug-delivery mechanism, in comparison to OA treatment, is associated with reduced relapse rates, and frequencies of suicidal ideation and overdose events in patients with MH disorders associated with psychosis.
Introduction
Patients who suffer from psychiatric disorders associated with psychosis relapse despite treatment with antipsychotic medication (Lafeuille et al., 2013), leading to re-hospitalization (emergency room (ER) visits, and admissions), high healthcare costs, and other poor outcomes (Koczerginski & Arshoff, 2011; Su et al., 2009). Traditionally, treatment of with oral antipsychotic (OA) medications is effective, despite the evidence for poor, overall patient prognoses (Denham & Adamson, 1971; Velligan et al., 2006; Lindstrom, 1989). Furthermore, patients suffering from psychotic disorders tend to have high suicide rates, especially in patients who repeatedly relapse (Pompili et al., 2017). A multitude of factors must therefore contribute to patient relapse.
Many factors are linked with non-adherence to medication as part of the treatment plan. These include symptoms that interfere with therapy, such as hallucinations, poor cognition, lack of insight, social stigma and other factors; furthermore, many patients need assistance to take the medication (Haddad et al., 2014). Many antipsychotic medications have been made available in a longacting- injectable (LAI) formulation, in which patients are required to receive an appropriate dosage on a specific recurring timeinterval (Lafeuille et al., 2013). Medical professionals are then able to assume greater confidence that their patients are adhering to their treatment plans - if they regularly attend appointments scheduled for injection. MH illnesses treated with antipsychotics often pose many obstacles for patients, families and providers to overcome - this solution reduces these challenges, improves patient outcomes and is believed to reduce hospitalization rates.
Previous studies have exhibited a reduction in healthcare resource utilization in schizophrenic patients treated with LAI medication (Lafeuille et al., 2013; Koczerginski & Arshoff, 2011; Su et al., 2009; Davis, 1975; Sena et al., 2003; Olivares et al., 2009; Sheperd et al., 1989). At Lakeridge Health Oshawa (LHO), a midsized community hospital in Oshawa, Ontario, Canada, a group of patients with disorders associated with psychosis were switched from OA treatment to LAI regimens, and multiple drug types were included. Mental health (MH)-related ER visits, hospital admissions, reports of patient suicidal ideation and attempts, as well as intentional drug overdose rates were compared before and after switching from an OA to a LAI formulation.
This article investigates the relationship between antipsychotic delivery methods (OA and LAI) with respect to hospitalization rates and suicidal ideation to better determine methods for improving patient prognoses. Specifically, patients were switched from OA to LAI treatment regimens, and to our knowledge, this is first investigation of its kind to examine health services outcomes associated with suicidality in such a population.
Methods
Study Design
A retrospective chart review was conducted for 92 adult patients (age ≥ 18) previously treated with OA medication whose regimens were subsequently switched to LAI monotherapy formulations from June 2014 to June 2015. The primary comparison was the year prior to LAI to the year on LAI. All LAI drugs were included. The study followed a mirror-image model in which hospitalizations were compared in all patients for one year on OA therapy and one year on LAI therapy. Furthermore, efficacy of the treatment methods was also assessed by comparing patient self-reports of suicidal ideation and attempts in patients while on OA and LAI regimens. Approval from the hospital’s Research Ethics Board was granted prior to beginning the study.
Health System
Lakeridge Health Oshawa (LHO) is based in Oshawa, Ontario, and is a part of the Lakeridge Heath Corporation, which is one of Ontario’s largest community hospitals, with 16 sites spanning across the Durham region from Bomanville to Pickering. The Lakeridge Health Corporation sites provide primary, secondary, tertiary and post-acute care in inpatient and ambulatory settings to the eastern part of the Greater Toronto Area. The system has four medical emergency rooms (ERs), including the LHO site.
Procedures for Collecting Data
The following patient demographic values were collected in the study: age, sex, diagnosis, medication type and date of LAI initiation. Data were collected by chart review of the following information in the health system: 1) health care utilization of inpatient, emergency and outpatient services; 2) notes in charts about patient self-reports of suicidal ideation and attempts; and 3) medication type and date of LAI initiation.
Utilization was computed by manual chart review - this included MH and non-MH services. Patients who met the inclusion criteria had been formally diagnosed with a MH disorder associated with psychosis upon routine clinical assessment by multiple psychiatrists at LHO. Schizophrenia, schizoaffective disorder, bipolar disorder, and other disorders consistent with psychotic features were included in the study population.
Patient privacy was maintained by removing patient identifiers. An independent data collector, a registered nurse on the hospital’s Mental Health and Crisis Intervention Team.
Statistical Methods
Patient demographics and outcomes were analyzed with descriptive methods to compare percentages and ratios for categorical variables, and to compare means, medians, standard deviations and standard errors for continuous variables. P values and 95% Confidence Intervals were additionally calculated to interpret the differences in the values obtained while subjected to OA vs. LAI therapy. All statistical analyses were performed in R Studio (RStudio, Inc., Boston, MA, USA).
Results
Patient Demographics and Treatment Plans
A total of 94 charts met the inclusion criteria and were selected for review. Two patients were removed from the study due to unrelated comorbidities leading to discontinuation of LAI treatment in one patient and mortality in the other (underlying cardiac issues). As a result, 92 of the included patients generated sufficient two-year data.
Approximately 63% of patients were male and 37% of patients were female (see Table 1). The median age was 36.5. Primary diagnoses were schizophrenia (58.7%), schizoaffective (22.8%), bipolar disorder (7.6%), and psychosis (7.6%) (Table 1). Additionally, one patient was diagnosed with delusional disorder, one patient with personality disorder, and one patient with paranoia.
| Characteristic | Value |
|---|---|
| Males: N (%) | 58 (63.04%) |
| Females: N (%) | 34 (36.96%) |
| Age: Mean +/- SD, Median (Range) | 39.13 +/- 16.63, |
| 36.5 (18 - 90) | |
| Diagnosis | |
| Schizophrenia: N (%) | 54 (58.70%) |
| Schizoaffective: N (%) | 21 (22.83%) |
| Bipolar: N (%) | 7 (7.61%) |
| Psychosis: N (%) | 7 (7.61%) |
| Other: N (%) | 3 (3.26%) |
| Treatment | |
| i) First Generation Depot Antipsychotics | |
| Flupentixol decanoate N (%) | 33 (35.87%) |
| Haloperidol decanoate: N (%) | 2 (2.17%) |
| ii) Second Generation Antipsychotics | |
| Paliperidone palmitate (Sustenna): N (%) | 38 (41.30%) |
| Risperidone long acting injectable (RLAI): N (%) | 19 (20.65%) |
Table 1: Patient demographic, diagnosis, and treatment characteristics
The most common LAI regimens were paliperidone palmitate (41.3%) and flupentixol decanoate (35.9%), followed by risperidone long-acting injectable (20.7%) and haldolperidol decanoate (2.2%) (Table 1).
Patient Outcomes
ER visits
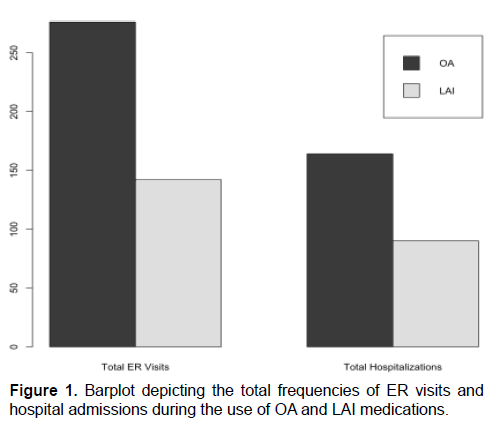
The number of patients who visited the ER at least once, for conditions related to MH decreased from 84 (91.3%) to 41 (44.6%) for OA and LAI, respectively; a reduction of 51.2%. The total number of ER visits at LHO also decreased from 276 visits to 142 visits after the switch to LAI medication (Figure 1). The mean MHrelated ER visits prior to the switch in treatment decreased from 3.0 visits/patient (95% CI 2.34-3.66) to 1.5 visits/patient (95% CI 0.96-2.13).
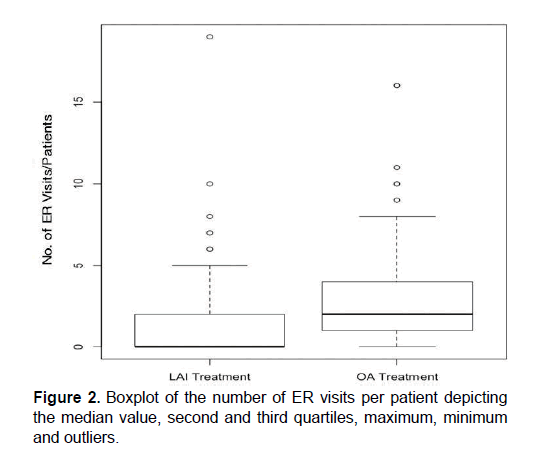
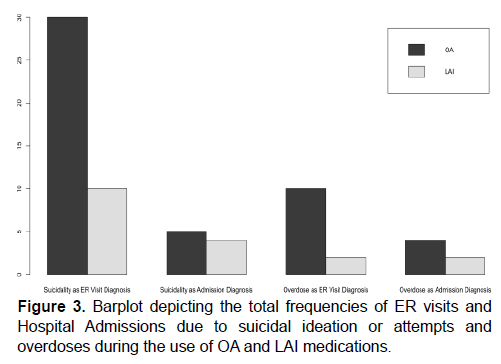
The median values were also calculated to be 2 visits/patient (0-16) on OA and 0 visits/patient (0-19) on LAI (Figure 2). The number of ER visits due to patient suicidal ideation and attempts decreased by 66.7% (from 30 to 10 visits; Figure 3). Additionally, ER visits due to intentional overdose decreased by 80%, from 10 to 2 visits respectively (Figure 3).
Hospital admissions
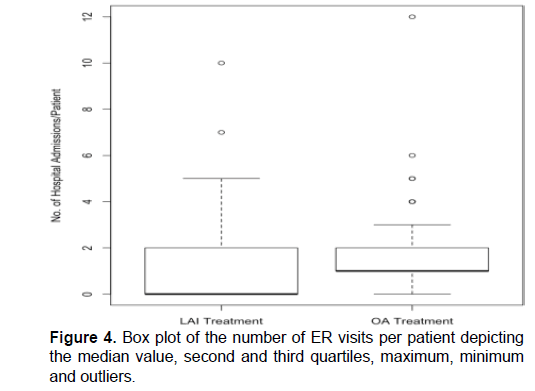
The number of patients admitted to the hospital at least once for issues pertaining to MH decreased from 84 (91.3%) for OA treatment phase to 36 (39.1%) with LAI treatment; a reduction of 57.1% (Figure 1). The total number of MH related hospital admissions at LHO also decreased from 164 to 90 after the switch to LAI medication (Figure 1). The mean MH related hospital admissions per patient while on OA treatment decreased from 1.8 (95% CI 1.44-2.13) to 0.98 visits/patient (95% CI 0.62-1.33). The median number of hospitalizations per patient was 1 visits/patient (0-12) on OA and 0 visits/patient (0-10) on LAI medication (Figure 4). The number of patients admitted to the hospital with a diagnosis of suicidal ideation/attempt decreased by 20%, from 5 occurrences during OA treatment to 4 occurrences with LAI treatment (Figure 3). Additionally, the number of intentional patient overdoses as hospital admission diagnosis decreased by 50%, from 4 to 2 occurrences respectively (Figure 3).
Discussion
This study has revealed that patient relapse, suicidality and the corresponding hospitalization rates were reduced in patients with various psychiatric disorders when OA treatment plans were replaced with LAI regimens. Hospitalization and suicidality frequencies, as well as the mean patient values for these variables, all decreased after one year on LAI medication relative the OA phase of the study.
Our results are consistent with many similar studies that seek to compare the efficacy of OA to LAI medications (Su et al., 2009; Gastpar et al., 2005; Kishimoto et al., 2013; Vincent et al., 2017). The reduction seen in the total number of MH ER visits (~48.6%) is consistent with other studies which have previously documented decreases between ~36% and 73% (Su et al., 2009; Denham & Adamson, 1971; Schooler, 2003). However, in contrast to our results, randomized controlled trials (RCTs) have generally not found statistically significant differences between the efficacy of OA and LAI regimens (Kishimoto et al., 2012; Ostuzzi et al., 2017). Although meta-analyses of both standard study-designs clearly contradict each other, there is no evidence of OA to LAI superiority. It is thus plausible that the two treatment types are equally effective, given that that patient adherence is equal regardless of whether treatment consists of OA or LAI medications (Suzuki, 2016). This notion must be treated with caution as patients with severe mental illnesses, responsible for self-administering OAs, cannot be assumed to have equal adherence with patients who are receiving physician administered LAI treatment. Furthermore, RCTs operate under idealized conditions that are not as realistic as observational studies, especially in a community hospital setting (Kirson et al., 2013). RCTs have stringent selection criteria, often solely enrolling patients expected to have high adherence, and moreover, promote patient engagement that is typically higher than in real world circumstances, utilizing frequent appointments and patient-reminders (Suzuki, 2016). Observational studies may therefore, better represent patient outcomes when exposed to a greater selection of real-world variables.
The research comparing OA and LAI efficacy - almost solely based on patients diagnosed with schizophrenia and a single drug type - is furthered by this study which encompasses a broad range of disorders and medication types. Non-adherence and other common factors interfering with medication adherence are common in a variety of patients and this research has significant treatment implications (Haddad et al., 2014). In particular, patients with bipolar disorder, have frequent re- admissions and are high utilizers of services due to non-adherence and unstable mood episodes (Xiong et al., 2010). This study’s patient population is helpful compared to some studies evaluating patients with longterm, chronic schizophrenia, as the latter group has many other factors that interfere with medication adherence making it difficult to assess the efficacy of the LAI delivery mechanism, despite drug type or disorder, in comparison to the OA method of delivery.
We used ER visits and hospitalization events, as well as suicidality and overdose events, to measure patient relapse since clinical assessment data was unavailable. We believe these are reasonable indicators of patient relapse as the psychiatric disorders included in the study are often linked to extreme symptoms and behaviours including: psychosis, suicidal ideation, violence, drug abuse and others, all of which warrant medical attention (Lafeuille et al., 2013; Chapman et al., 2015; Hogarty and Ulrich, 1998). Repeated relapses in patients has been shown to increase the risk for shorter remission periods and higher severity of future episodes (Su et al., 2009; Sheperd et al., 1989). Poor adherence and/or compatibility with the treatment could therefore increase healthcare costs significantly, given that previous investigations have demonstrated schizophrenia and other disorders that are associated with psychosis account for some of the costliest diseases to treat in Canada (Vincent et al., 2017; Goeree et al., 2005). Lastly, patient outcomes and quality of life may be assessed via suicidality and drug abuse data; however more substantial evidence, such as physician assessment notes, may be useful to evaluate this subjective variable in future studies (Pompili et al., 2017).
The study has strengths and weaknesses. This community hospital sample avoided selection bias based on patient demographics, disease and treatment types. The mirror- image study design allowed patients to serve as their own controls, thereby reducing the effects of patient-specific confounding variables. There is some degree of variability observed in the number of ER visits (sOA=3.2, sLAI=2.8) and rehospitalizations (sOA=1.7, sLAI=2.8) but this is not uncommon.
Variability due to the presence of positive outliers is hard to exclude, as they may be subject to underlying conditions and highly stressful environments leading to decreased stability, such as homelessness (Clarke et al., 2000). The diagnostic assessment, chart review and other procedures for data collection could be stronger by capturing the number of additional psychiatric medications, the duration of MH illness in each patient, and healthcare utilization in other systems. Another limitation may be a bias toward the results of individuals who seek emergency medical attention - whether they were in the OA or LAI phase of the study.
This study was limited to a one-year assessment period on each of the control and treatment phases; a longer period would be helpful. A multi-site study would also improve perspective and generalizability of our data. Lastly, the retrospective-observational design - rather than a randomized one - allows for other potential confounding variables to have impact, though as discussed above, observational studies may yield more clinically relevant data than RCTs which have highly specific patient inclusion criteria (Kirson et al., 2013).
Conclusions
This one-year, observational study found that the LAI treatment method for antipsychotic drug administration is superior to the OA treatment method by reducing hospitalizations, as well as rates of suicidal ideation and drug overdose in patients treated at LHO in Oshawa, Ontario, Canada. LAI is underutilized in psychiatric populations and could have significant impact in my patient populations, particularly when combined with other biopsychosocial interventions. Future studies with better methodology and which are longer and expand on non-schizophrenic populations are indicated.
References
- Lafeuille, M.H., Laliberté-Auger, F., Lefebvre, P., Frois, C., Fastenau, J., & Duh, M. S. (2013). Impact of atypical long-acting injectable versus oral antipsychotics on rehospitalization rates and emergency room visits among relapsed schizophrenia patients: A retrospective database analysis. BMC psychiatry, 13(1), 221. Koczerginski, D., & Arshoff, L. (2011). Hospital resource use by patients with schizophrenia: Reduction after conversion from oral treatment to risperidone long-acting injection. Healthcare quarterly (Toronto, Ont.), 14(1), 82-87. Su, K.P., Chang, H.C., Tsai, S.J., Yen, F.C., & Tang, C.H. (2009). Relapse and long-acting injectable risperidone: A 1-year mirror image study with a national claims database in Taiwan. Value in Health, 12, S118-S121. Denham, J., & Adamson, L. (1971). The contribution of fluphenazine enanthate and decanoate in the prevention of readmission of schizophrenic patients. Acta Psychiatrica Scandinavica, 47(4), 420-430. Velligan, D.I., Lam, Y.W.F., Glahn, D.C., Barrett, J.A., Maples, N.J., Ereshefsky, L., & Miller, A.L. (2006). Defining and assessing adherence to oral antipsychotics: A review of the literature. Schizophrenia Bulletin, 32(4), 724-742. Lindström, L.H. (1989). A retrospective study on the long-term efficacy of clozapine in 96 schizophrenic and schizoaffective patients during a 13-year period. Psychopharmacology, 99, S84-S86. Pompili, M., Orsolini, L., A Lamis, D., R Goldsmith, D., Nardella, A., Falcone, G., et al. (2017). Suicide Prevention in Schizophrenia: Do Long-Acting Injectable Antipsychotics (LAIs) have a Role? CNS & Neurological Disorders-Drug Targets (Formerly Current Drug Targets-CNS & Neurological Disorders), 16(4), 454-462. Haddad, P.M., Brain, C., & Scott, J. (2014). Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Related Outcome Measures, 5, 43. Davis, J.M. (1975). Overview: maintenance therapy in psychiatry: I. Schizophrenia. The American Journal of Psychiatry. Sena, E.P.D., Santos-Jesus, R., Miranda-Scippa, Â., Quarantini, L.D.C., & Oliveira, I.R.D. (2003). Relapse in patients with schizophrenia: a comparison between risperidone and haloperidol. Revista Brasileira de Psiquiatria, 25(4), 220-223. Olivares, J.M., Rodriguez-Morales, A., Diels, J., Povey, M., Jacobs, A., Zhao, Z., & Lam, A. (2009). Long-term outcomes in patients with schizophrenia treated with risperidone long-acting injection or oral antipsychotics in Spain: Results from the electronic Schizophrenia Treatment Adherence Registry (e-STAR). European psychiatry, 24(5), 287-296. Shepherd, M., Watt, D., Falloon, I., & Smeeton, N. (1989). The natural history of schizophrenia: a five-year follow-up study of outcome and prediction in a representative sample of schizophrenics. Psychological Medicine Monograph Supplement, 15, 1-46. Gastpar, M., Masiak, M., Latif, M.A., Frazzingaro, S., Medori, R., & Lombertie, E.R. (2005). Sustained improvement of clinical outcome with risperidone long-acting injectable in psychotic patients previously treated with olanzapine. Journal of Psychopharmacology, 19(5_suppl), 32-38. Kishimoto, T., Nitta, M., Borenstein, M., Kane, J.M., & Correll, C.U. (2013). Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. The Journal of clinical psychiatry, 74(10), 957-965. Vincent, P.D., Demers, M.F., Doyon-Kemp, V., Duchesneau, J., Halme, A., & Masson, V. (2017). One year mirror-image study using paliperidone palmitate for relapse prevention of schizophrenia in four university hospitals in Canada. Schizophrenia research. Schooler, N.R. (2003). Relapse and rehospitalization: comparing oral and depot antipsychotics. The Journal of clinical psychiatry, 64, 14-17. Kishimoto, T., Robenzadeh, A., Leucht, C., Leucht, S., Watanabe, K., Mimura, M., et al. (2012). Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized trials. Schizophrenia bulletin, 40(1), 192-213. Ostuzzi, G., Bighelli, I., So, R., Furukawa, T.A., & Barbui, C. (2017). Does formulation matter? A systematic review and meta-analysis of oral versus long-acting antipsychotic studies. Schizophrenia research, 183, 10-21. Suzuki, T. (2016). A further consideration on long-acting injectable versus oral antipsychotics in the treatment of schizophrenia: a narrative review and critical appraisal. Expert opinion on drug delivery, 13(2), 253-264. Kirson, N.Y., Weiden, P.J., Yermakov, S., Huang, W., Samuelson, T., Offord, S.J., et al. (2013). Efficacy and effectiveness of depot versus oral antipsychotics in schizophrenia: synthesizing results across different research designs. Xiong, G.L., Iosif, A.M., Brook, M., & Hilty, D.M. (2010). Predictors of decertification from involuntary hospitalization for patients with bipolar disorder. Psychiatric Services, 61(2), 200-203. Chapman, C.L., Mullin, K., Ryan, C.J., Kuffel, A., Nielssen, O., & Large, M.M. (2015). Metaâ€analysis of the association between suicidal ideation and later suicide among patients with either a schizophrenia spectrum psychosis or a mood disorder. Acta Psychiatrica Scandinavica, 131(3), 162-173. Hogarty, G.E., & Ulrich, R.F. (1998). The limited effects of antipsychotic medication on schizophrenia relapse and adjustment and the contributions of psychosocial treatment. Journal of psychiatric research, 32(3), 243-250. Goeree, R., Farahati, F., Burke, N., Blackhouse, G., O’Reilly, D., Pyne, J., & Tarride, J.E. (2005). The economic burden of schizophrenia in Canada in 2004. Current medical research and opinion, 21(12), 2017-2028. Clarke, G.N., Herinckx, H.A., Kinney, R.F., Paulson, R.I., Cutler, D.L., Lewis, K., et al. (2000). Psychiatric hospitalizations, arrests, emergency room visits, and homelessness of clients with serious and persistent mental illness: findings from a randomized trial of two ACT programs vs. usual care. Mental health services research, 2(3), 155-164.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 7844
- [From(publication date): 0-2017 - Dec 15, 2025]
- Breakdown by view type
- HTML page views: 6802
- PDF downloads: 1042