Effectiveness of Obstacle Cross Training on Gait Performance in Ambulatory Patients with Spinal Cord Injury
Received: 04-Oct-2022 / Manuscript No. jnp-22-77154 / Editor assigned: 06-Oct-2022 / PreQC No. jnp-22-77154 (PQ) / Reviewed: 20-Oct-2022 / QC No. jnp-22-77154 / Revised: 25-Oct-2022 / Manuscript No. jnp-22-77154 (R) / Accepted Date: 31-Oct-2022 / Published Date: 01-Nov-2022 DOI: 10.4172/2165-7025.1000549
Abstract
Gait and balance is a significant issue for the majority of ambulatory patients with incomplete spinal cord injuries. Indeed, they are at greater risk of falling. Direct or indirect damage to the central or peripheral nervous system can reduce an individual’s ability to perform activities of daily living. In a significant number of spinal cord individuals, incomplete injury to the spinal cord may spare their descending motor control pathways and allow their ability to retain the ability work. However most of them can walk non functionally walking at slow speed, short distance or within the house. The ability to functionally ambulate is decreased. Seventeen patients with SCI (ASIA impairment scale C and D) who were able to walk independently with or without walking devices or braces were recruited for the study. Participants received 10 sessions of obstacle crossing training and conventional over ground walking training in a randomized controlled trial. Pre and post scores after each training program, functional ability of all participants was measured. The outcome measures used were Five Times Sit to Stand Test (FTSST), Timed Up and Go (TUG), 10 Meter Walk Test (1OMWT), Walking index for spinal cord injury (WISCI II). Results showed that the experimental group demonstrated a significant differences in WISCI II, FTSST, TUG, 1OMWT than the control group in in-between comparison within the groups.
Keywords
Spinal cord injuries; Walking; Obstacle crossing training; Walking device; Rehabilitation
Introduction
Spinal cord injury (SCI) is one of the most devastating conditions possible. Spinal cord injury (SCI) is possibly the most disruptive and traumatic event that can occur in anyone’s life. SCI poses huge challenges in the form of coping process as well as rehabilitation. A multidisciplinary approach is required to restore their life and expect the opportunity for an independent and productive future, shown to be beneficial with lower mortality, decreased pressure sores, slightly greater chance of neurologic recovery. The annual incidence of Spinal Cord Injury (SCI) worldwide has been reported to be between 11.5 and 57.8 cases per million population. As per report of the International conference (spinal injuries management), the incidence of spinal injury was estimated at 15 new cases per million per year in India [1].
Walking is one of the principal goal after a spinal cord injury and is considered the most important objective by patients and is the principal target of rehabilitation approaches. Depending on the severity of the lesion, most patients have the potential to recover walking. Independent walking is an ultimate goal that patients with Spinal Cord Injury (SCI) want to achieve. However the patients can improve walking ability after participation in a rehabilitation program, the majority of them do not recover functional walking. Approximately 70% of patients with incomplete spinal cord injury can become ambulatory after participation in a rehabilitation program. However, most of them walk only within the house, walk only at a short distance, require assistance from person or walking device and fail to walk over small obstacle of sizes that are commonly found in homes and communities. Previous studies indicate that 39% to 75% of independent ambulatory patients with SCI have experienced at least 1 fall during a 6 month to 12 month follow up period, with most of the falls occurring as a result of stumbling over an obstacle while walking.
To successfully walk over a high obstacle, patients must use a flexor strategy to increase foot clearance, whereas a wide obstacle requires them to lengthen their step length. In addition, to effectively walk over obstacles, patients must be able to balance themselves on double limb support when lifting the walking devices off the ground. It has been seen that obstacle crossing training immediately enhanced functional ability related to walking of ambulatory patients with spinal cord injury. However, randomized controlled trial is needed to support benefits of incorporation of obstacle crossing training into rehabilitation practice. Therefore, purpose of this study is to find out the effectiveness of obstacle crossing training and conventional over ground walking training on functional ability among ambulatory patients with spinal cord injury [2].
Materials and Methods
A pre and post-test experimental design was used in our study. A sample of 17 spinal cord subjects who met the inclusion criteria and willing to participate in the study voluntarily were recruited in the study. Out of 17 patients, 1 subject was dropped out from study. Inclusion criteria were as follows: Subjects with subacute incomplete spinal cord injury (ASIA C, D), having age of 18 years-65 years, gender: both male and female, subjects should have ability to walk independently with or without walking device or braces, ability to rise from a chair independently with or without the use of hands. Exclusion criteria were as follows: Patients with SCI from progressive disease, any neurological or medical disorder that could have negative impacts on ambulatory ability, any sign or symptom that might face participation in study such as pain in musculoskeletal system (>5 on VAS) having any condition in which patient cannot communicate effectively such as head injuries,cognitive issues, active cardiac or pulmonary conditions, Parkinson’s disease, peripheral neuropathy in lower extremities, stroke, psychiatric history or any other active clinical conditions.
All the subjects were given a detailed explanation of the procedure and a written content was obtained. Participants were assessed for their baseline demographics and neurological deficits, that is, motor and sensory scores, level of injury and severity using the American Spinal Injury Association (ASIA). Baseline measurements and post intervention scores are taken after 2 weeks (5 sessions per week). Participants were then randomly divided into two groups by computer generalized randomization and undergo training. Group 1: (Experimental group) Obstacle crossing training with conventional over ground walking training [3].
The test was conducted in a 10 meter walking space. Wooden obstacles (0.5 cm wide and 360 cm long) were in 3 heights (1 cm, 4 cm and 8 cm) to represent obstacles likely found in homes and communities. To provide a high obstacle, each obstacle was placed vertically, to present a wide obstacle, each obstacle was placed flat on the floor. A physiotherapist walked alongside the participant throughout the test. During training, participants were instructed to walk continuously over every obstacle at their self-determined walking speed with or without a walking device, and not to attempt any obstacle that might pose a risk of injury for them. During taking part in the study, participants still received routine treatments from other rehabilitation professionals as needed. They were able to take a period of rest as required.
During testing, participants used walking devices, orthosis (Eg: ankle-foot orthosis), and the glasses or corrective lenses that they normally wore during walking. Progression of the task included increasing obstacle frequency, varying rates of obstacle delivery, and increasing obstacle size. Group 2: (Control group) conventional over ground walking training. Different types of walking in parallel barforward walking, backward walking, straight line walking, heel to toe walking, sit to stand activity. Rocker board training, unsupported sitting, and unsupported walking. Participants were instructed to walk at a self-determined walking speed along a 10 m walkway with or without a walking device continuously as good and as long as they could [4].
Outcome measures
• Meters Walk Test: Participants were instructed to walk a set of distance (10 meters). To minimize acceleration and deceleration effects, the time required over the middle 6 m of walkway was recorded. The average time for the three trials was recorded.
• Five times sit to stand test: Participants sat on an armless chair with their back upright against the backrest of chair, placing their feet flat on the floor, while their arms at the side or on the walking devices. The test measured the time taken to complete five repetitions of the sit to stand maneuver.
• Timed up and go test: Participants sat against the backrest of the chair and their arms on the arm rest or on the walking device. They were instructed to stand up from the chair, walk at a fast speed for 3 m, turn around a cone, walk back and sit down with or without walking device. The average of three trials was recorded.
• WISCI II: It assesses the amount of physical assistance needed, as well as devices required, for walking following paralysis that results following spinal cord injury. They are more precise measure of improvement in walking ability specific to SCI. Rank orders the ability of a person to walk 10 m after a spinal cord injury from most to least severe impairment.
Statistical analysis
The Statistical Package of Social Science (SPSS) for windows, version 20.0. The normality of the distribution of the data was tested using the Shapiro-Wilk test. As a result of SW test (p ≤ 0.05), the parametric test analysis used to determine statistical significance between and within the groups. Analysis was done for 16 subjects who completed the study. Independent t-test was also used to analyze the age, time since injury to check the homogeneity of the subjects in both the groups. Independent t-test was used to analyze the difference between group 1 and group 2. Within group analysis between pre intervention and post intervention was performed using and paired t-test. A significance level of p ≤ 0.05 was fixed the value of confidence interval was set at 95%.
Results
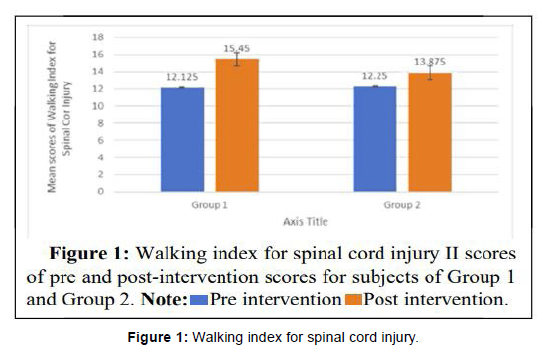
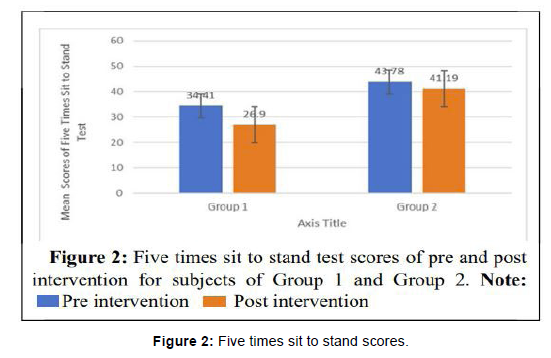
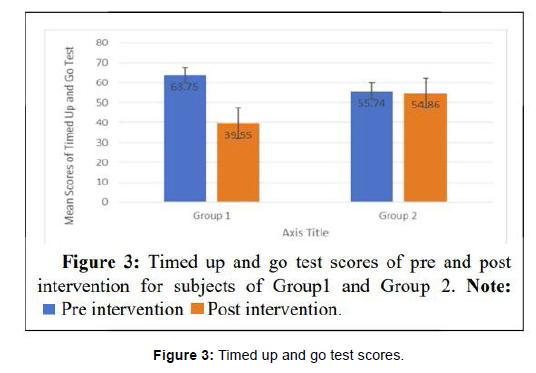
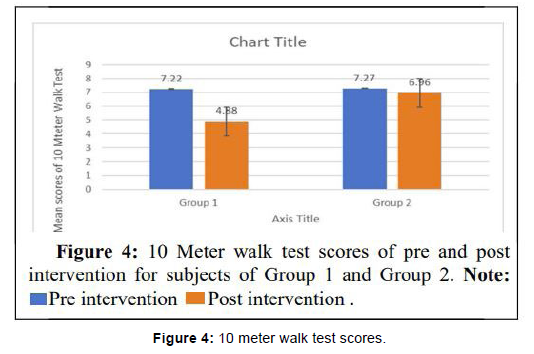
The experimental group demonstrated a significant difference in the 10 meter walk test (p ≤ 025), WISCI II (p ≤ 017), five times sit to stand test (p ≤ 000) and times up and go test (p ≤ 002) than the control group in in-between comparison within the groups (Tables 1-3) [5].
| Outcome measures | Pre-scores | Post-scores | t-value | Sig (p-value) |
|---|---|---|---|---|
| WISCI II | 12.13 ± 4.764 | 15.38 ± 3.503 | -3.1 | 0.017* |
| FTSST | 34.41 ± 12.88 | 26.90 ± 12.42 | 6.33 | 0 |
| TUG | 63.76 ± 30.48 | 39.55 ± 16.24 | 4.63 | 0.002* |
| 10MWT | 7.22 ± 4.16 | 4.88 ± 2.29 | 2.84 | 0.025* |
| Note: Values are given as mean ± standard deviation, * indicates significance difference at p ≤ 0.05 level, WISCI II: Waking Index for Spinal Cord Injury, FTSST: Five Times Sit to Stand Test, TUG: Timed Up and Go test, 10MWT: 10 meter walk test |
||||
Table 1: Comparison between pre and post intervention scores of Group 1 using paired t-test.
Outcome measures |
Pre-scores | Post-scores | t-value | Sig (p-value) |
|---|---|---|---|---|
| WISCI II | 12.25 ± 4.32 | 13.88 ± 6.83 | -1.45 | 0.189ns |
| FTSST | 43.78 ± 14.96 | 41.19 ± 14.15 | 1.86 | 0.105ns |
| TUG | 55.74 ± 29.96 | 54.86 ± 28.17 | 0.54 | 0.600ns |
| 10MWT | 7.27 ± 4.11 | 6.96 ± 3.65 | 1.346 | 0.220ns |
| Note: ns-no significant difference at p ≤ 0.05 level. | ||||
Table 2: Comparison between pre and post intervention scores of Group 2 using paired t-test.
Outcome measures |
Pre-scores | Post-scores | t-value | Sig (p-value) |
|---|---|---|---|---|
| WISCI II | 15.38 ± 3.50 | 13.88 ± 6.83 | 0.553 | 0.589 ns |
| FTSST | 26.90 ± 12.42 | 41.19 ± 14.15 | -2.419 | 0.05* |
| TUG | 39.50 ± 16.24 | 54.86 ± 28.17 | -1.332 | 0.204ns |
| 10MWT | 4.88 ± 2.29 | 6.96 ± 3.65 | -1.1365 | 0.194ns |
| Note: Values are given as mean ± standard deviation, ns-no significant difference at p ≤ 0.05 level, *indicates significance difference at p ≤ 0.05 level. | ||||
Table 3: Comparison between post intervention scores of group 1 and group 2 using independent sample t-test.
Discussion
This study was done to compare the effectiveness of obstacle crossing training on gait performance in ambulatory patients with spinal cord injury. The results obtained after 10 treatment sessions over a period of 2 weeks between two groups were compared [6]. The subjects in both the groups were compared with respects to their age, time since injury and ASIA grading from each other pre-intervention. On comparison between both the groups there was no statistically significant different in Walking Index of Spinal Cord Injury (WISCI II), Timed Up and Go Test (TUG) and 10 Meter Walk Test (10MWT) except Five Times Sit to Stand Test (FTSST). Our result are in consensus with the 12 who quoted that obstacle crossing training may not replicate its results on extrinsic factors like functional ability and fall. Therefore, further studies can be to train the patients in community environment where they get hands on exposure to extrinsic factors (Figure 1) [7].
However FTSST has found to be significant between two groups. The potential reason can be attributed to be because of good quadriceps muscle strength of some patients which is the main component to make a patient stand from sitting. As we did not measure strength objectively before intervention so we cannot justify improved FTSST scores was due to our intervention. The potential reasons for not getting the significant difference in majority of the outcome measures might be attributed to various factors [8]. One might be the small sample size, which may have attribute to type-II statistical error and less duration of treatment. As walking and balance are broader domains to be achieved in rehabilitation of spinal cord injury patients. These outcome depends upon too many factors like age, ASIA grading, time since injury, functional ability and rehabilitation time. Since in our study we only emphasized on obstacle training for 2 weeks due to time constraints which was insufficient to bring significant changes in domains (Figure 2) [9].
Immediate effects and better generalization of results we proposed an intervention of 2 weeks and planned for RCT. However at the end we found a longer duration (4 weeks or more) of obstacle crossing might yield positive result. Majority of the studies on obstacle crossing training were focused on ASIA D. In our inclusion criteria we added ASIA C as it was as unexplored facet till date. On comparison within both the groups, the pre and post intervention scores of Walking Index of Spinal Cord Injury, Five Times Sit to Stand Test, Timed Up and Go Test and 10 Meter Walk Test of Obstacle Crossing Training along with conventional over ground walking training (Group 1) have shown statistically significant improvement as compared to their pre intervention scores (Figure 3) [10].
The pre and post intervention scores of Walking Index of Spinal Cord Injury, Five Times Sit to Stand Test, Timed Up and Go Test and 10 Meter Walk Test of control group (Group 2) have no statistically significant improvement. This means that there was an improvement in experimental group studied the immediate effect of obstacle crossing training in independent ambulatory patients with spinal cord injury and conventional over ground walking on functional ability among independent patients with spinal cord injury and concluded that obstacle crossing (Figure 4) [11].
Adapt locomotors training was feasible for chronic spinal cord injury individuals. Stated that patients failed to walk over an obstacle so incorporation of obstacle crossing in walking training would help patients to successfully manage hazardous environment or make them aware that they are at risk of injury. However, the statistical analysis between the group showed that the result was significant only for Five Times Sit to Stand Test, but the functional ability gait measures was improved in obstacle crossing training group than the conventional over ground walking training group when examined clinically.
Conclusion
The result shows that there was no significant difference in between the group comparisons, but within group comparisons showed significant improvement in Walking Index of Spinal Cord Injury, Five Times Sit to Stand Test, Timed Up and Go Test and 10 Meter Walk Test, the mean difference in all domains were more in the experimental group as compared to the controlled group. The study concluded that Obstacle Crossing Training shall be incorporated for gait and walking training with other rehabilitation procedures on functional ability and gait performance in individual with incomplete spinal cord injury.
Limitations of the study
1. The sample size was small to establish the effectiveness of obstacle crossing training statically.
2. Future research with a large sample may help to establish the effectiveness of obstacle crossing training on functional ability among patients with spinal cord injury.
3. The duration of the obstacle crossing training could have been long to show the significant change.
4. Also, no follow up measures were taken to assess the retention of the gait and functional ability improvement over a longer period of time.
Acknowledgement
Not applicable.
Conflict of Interest
The authors declare no conflict of interest.
References
- New P, Simmonds F, Stevermuer T (2010) A population-based study comparing traumatic spinal cord injury and on-traumatic spinal cord injury using a national rehabilitation database. Spinal Cord 49: 397-403.
- Ditunno P, Patrick M, Stineman M, Morganti B, Townson A, et al. (2005) Cross-cultural differences in preference for recovery of mobility among spinal cord injury rehabilitation. Spinal Cord 44: 567-575.
- Pramodhyakul W, Wattanapan P, Siritaratiwat W, Eungpinichpong W, Amatachaya S, et al. (2013) Immediate effects of obstacle crossing training in independent ambulatory patients with spinal cord injury. Spinal Cord 51: 379-383.
- Amatachaya S, Pramodhyakul W, Srisim K (2015) Failures on obstacle crossing task in independent ambulatory patients with spinal cord injury and associated factors. Arch Phys Med 96: 43-48.
- Amatachaya S, Thaweewannakij T, Adirek-Udomrat J, Siritaratiwat W (2010) Factors related to obstacle crossing in independent ambulatory patients with spinal cord injury. J Spinal Cord Med 33: 144-149.
- Poncumhak P, Saengsuwan J, Kamruecha W, Amatachaya S (2012) Reliability and validity of three functional tests in ambulatory patients with spinal cord injury. Spinal Cord 51: 214-217.
- Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS et al. (2005) Clinical measurement of sit-to-stand performance in people with balance disorders: Validity of data for the five-times-sit-to stand test. Phys Ther 85: 1034-1045.
- Lam T, Noonan V, Eng J (2007) A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord 46: 246-254.
- Dittuno PL, Dittuno JF (2001) Walking index for spinal cord injury (WISCI II): Scale revision. Spinal Cord 39: 654-656.
- Fox EJ, Tester NJ, Butera KA, Howland DR, Spiess MR, et al. (2017) Retraining walking adaptability following incomplete spinal cord injury. Spinal Cord Ser Cases 3: 1-10.
- Amatachaya S, Pramodhyakul W, Wattanapan P, Eungpinichpong W (2015) Ability of obstacle crossing is not associated with falls in independent ambulatory patients with spinal cord injury. Spinal Cord 53: 598-603.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Kataria C, Sagar D (2022) Effectiveness of Obstacle Cross Training on Gait Performance in Ambulatory Patients with Spinal Cord Injury. J Nov Physiother 12: 549. DOI: 10.4172/2165-7025.1000549
Copyright: © 2022 Kataria C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1658
- [From(publication date): 0-2022 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 1311
- PDF downloads: 347