Effectiveness of Expanded Cardiac Rehabilitation on Mortality and Lifestyle Risk Factors in Patients Diagnosed With Coronary Heart Disease-A Systematic Review
Received: 21-Dec-2017 / Accepted Date: 05-Jan-2018 / Published Date: 10-Jan-2018
Abstract
Cardiac rehabilitation (CR) aims at decreasing risk and increasing the self-management of care. There is a need to determine which CR interventions are more effective.
Objective: What is the effectiveness of expanded CR compared to standard CR in coronary heart disease (CHD) patients? The review included randomized controlled trials (RCTs) that examine expanded CR compared to standard CR.
Expanded CR was defined as any multimodal intervention added to and targeting secondary prevention by other means than standard CR. Thus, expanded CR was typically reinforced, multifactorial educational and behavioral interventions.
Standard CR consisted of different guideline-defined interventions. There were no requirements for duration and intensity of the interventions. All settings on a global level were considered for inclusion.
The primary outcomes were readmission and mortality. Secondary outcomes were adherence to lifestyle risk factors: cholesterol, Body Mass Index, hypertension, smoking, diet, and physical activity. Databases searched included PubMed, Scopus, CINAHL, clinical.trials.gov and WHO trial registry. The search included English, Danish, Norwegian and Swedish language studies from 2000.
Two reviewers independently assessed the methodological quality of studies and extracted data. Appropriate data could not be pooled for meta-analysis due to heterogeneity of interventions.
The review included 30 RCTs. Compared to standard care one of six expanded CR interventions reduced mortality, and readmission was significantly reduced in seven of 11 RCTs. The most commonly reported outcome was level of cholesterol. In nine of 17 expanded CR interventions level of cholesterol was significantly reduced compared to standard CR. Few RCTs reported on adherence as maintenance of health behaviour. The review indicated beneficial effects of expanded CR compared to standard CR primarily on lifestyle risk factors, suggesting use in CHD patients. However, expanded CR should be tailored to sustainable lifestyle behavior changes measured by adherence to healthy lifestyle and include outcomes of functioning.
Keywords: Coronary heart disease; Cardiac rehabilitation; Prevention program; Patient education; Guideline adherence
Introduction
Coronary heart disease (CHD) is a chronic condition which often has serious physical, psychological and social consequences for the patients [1]. Coronary heart disease causes disability and it is estimated that the disability-adjusted life years (DALYs) estimate will rise from a loss of 85 million in 1990 to a loss of approximately 150 million DALYs in 2020. Coronary heart disease is the leading somatic cause of lost productivity; therefore, it is not only disabling for the patients but also a great burden to society [2]. Poor risk factor control and high prevalence of unhealthy lifestyle exist, therefore the identification of optimal patient management and CR remains a public health priority [2].
It is estimated that 42% and 38% of all deaths in European women and men, respectively that occur below 75 years of age are due to CHD [2]. The total number of patients living with CHD increases due to an ageing population in the western part of the world and a reduced case fatality of acute coronary events. The earliest and most prominent decline in death caused by CHD was seen in the more affluent countries in Europe between the 1970s and 1990s and is partly attributed to better treatments for acute coronary events, heart failure and other cardiac conditions. This development illustrates the potential for prevention of premature deaths and for prolonging healthy life expectancy [2].
In 2010, the human and economic arguments in favor of CHD prevention were estimated by the National Institute for Health and Clinical Excellence (NICE) as overwhelmingly positive regarding possible benefits and savings [3]. For secondary prevention of CHD, multimodal, behavioral interventions are recommended. A multimodal intervention may be composed by physical training and patient education delivered in weekly sessions. The interventions must include components such as nutrition advice, exercise, weight management, smoking cessation and adherence to prescribed medication. The NICE state that the benefits from such interventions are numerous and include [3].
• Narrowing of the gap in health inequalities
• Cost savings because of the number of CHD events prevented
• Prevention of co-morbidity
• Cost savings associated with CHD such as medication, primary care visits and outpatient attendances
• Cost savings to the wider economy as a result of loss of production, benefit payments and pension costs of early retirement due to CHD
• Improvement of the quality of life (QoL) and length of CHD patients’ lives.
Cardiac rehabilitation (CR) is a generic term for the multimodal and behavioral interventions in the secondary prevention of CHD, which is typically prescribed for 36 supervised exercise sessions over a 12 week period. The Scottish Intercollegiate Guidelines Network (SIGN) develops evidence-based guidelines derived from systematic reviews of the scientific literature. SIGN defines CR as: “…the process by which patients with cardiac disease in partnership with a multidisciplinary team of health professionals are encouraged and supported to achieve and maintain optimal physical and psychosocial health. The involvement of partners other family members, and careers is also important” [4].
The effect of CR has been studied in a Cochrane overview of reviews which included six systematic reviews [5]. The results are based on 148 randomized controlled trials (RCTs) and 98,093 patients. Exercisebased CR was found to be an effective and safe therapy to be used in the secondary prevention of clinically stable CHD patients in relation to reducing readmissions and improving health related QoL
A systematic review, not included in the overview, has also concluded that CR reduces patients' likelihood of depression and anxiety [6]. In addition a reduction in cholesterol and body mass index (BMI) was seen and patients tended to quit smoking and increase their exercise performance regarding intensity and duration [6]. The effect of CR was similarly studied in a large community cohort of CHD patients. The study showed that multidisciplinary CR was associated with a significant survival benefit in the first four years following an acute coronary syndrome (ACS) or cardiac intervention [7].
Patients’ lifestyles are based on long-standing behavioral patterns, which are caused by an interaction between environmental factors and personal and genetic factors [2,8]. Psychosocial risk factors such as stress, social isolation and negative emotions may act as barriers against behavioral change, and therefore should be addressed in CR [2,8].
Surveys show that a large proportion of CHD patients still do not achieve the lifestyle, the risk factor levels, and the therapeutic targets set in CR [2,8]. In the standard CR setting adherence to lifestyle recommendations and treatment regimens start to decline within six months of discharge from the hospital. Adherence to behavioral change concerning diet, exercise and smoking cessation after an ACS is associated with a significantly lower probability of re-infarctions compared with non-adherence [2].
Secondary prevention of CHD is considered a lifelong effort. Cardiac rehabilitation efforts help to maintain long-term adherence to the optimal treatment program by educating the patients and repeatedly emphasizing the importance of achieving and maintaining the prescribed treatments and recommended lifestyle [2,8]. Cardiac rehabilitation interventions may lead to better long-term results when it comes to behavioral change and somatic outcome [2].
Two RCTs have studied the effect of expanded CR versus standard CR [9,10]. Expanded CR consisted of everything contained in the standard CR; besides an interactive learning process, a long duration, and a mixed approach, a better collaboration with general practice, more focus on support from relatives and more intensive CR-lessons; for example with one-to-one support and hands-on practices. Patients randomized to expanded CR had significantly fewer readmissions, reinfarctions and a lower probability of cardiovascular death compared to patients randomized to standard CR [9,10]. A prospective cohort study found effect of expanded CR to socially vulnerable patients regarding significantly better adherence to prescribed medication at one-year follow-up compared to socially vulnerable patients who received standard CR. The same trend was seen in lipid profile, systolic blood pressure and BMI [11].
Based on this, it was relevant to conduct a systematic review concerning expanded CR versus standard CR. Expanded CR is defined as any interventions in addition to standard CR or usual care. It is of importance to examine the role of CR in the 21st century given the fact that treatment options for CHD have improved rapidly during the last decades, and the fact that it therefore has been questioned whether CR has retained its efficacy [7]. An initial search in the databases PubMed, the Cochrane Library, the Joanna Briggs Institute (JBI) Database of Systematic Reviews and Implementation Reports, CINAHL and PROSPERO indicated that no systematic reviews or protocols on this topic exist.
The objectives, inclusion criteria and methods of analysis for this review were specified in advance and documented in a protocol [12]. The research question of this review was: what is the effectiveness of expanded CR compared to standard CR in adult patients diagnosed with CHD?
Inclusion Criteria
Studies that included adult patients (more than 18 years old) diagnosed with CHD (also known as ischemic heart disease or coronary artery disease) were considered for inclusion. The patients were included in a rehabilitation program after surviving an episode of ACS including unstable angina, non-STEMI elevation myocardial infarction (non-ST) or ST-elevation myocardial infarction (STEMI). Studies with patients who underwent percutaneous coronary intervention (PCI) or coronary bypass graft surgery were included. Exclusion criteria were studies: including CHD patients with heart failure, very old adults, focusing on co-morbidity (e.g. diabetes or depression) or on primary prevention of hypertension, hyperlipidaemia, or hypercholesterolemia in CHD patients.
This review considered only RCTs that examined expanded CR compared to standard CR. Standard CR consisted of different guideline-defined medical and behavioral interventions, typically management of medical risk factors and lifestyle risk factors (e.g. diet and smoking). CR could be delivered by anyone, e.g. by specialist nurses or physiotherapists [2,8]. There were no requirements for duration and intensity of the CR. Expanded CR was defined as any multimodal intervention/s in addition to standard CR targeting lifestyle changes and medicine management for the secondary prevention of CHD by other means than traditional CR, e.g. internetbased programs. Expanded CR was typically reinforced, multi-factorial educational and behavioral interventions delivered or coordinated by a specialist [2,8]. All kinds of settings where CR interventions are undertaken were included.
This review considered RCTs including the following primary outcomes: all-cause mortality, cardiac mortality, all cause hospital admission, readmissions due to any cardiac event.
Secondary outcomes were adherence to secondary prevention guidelines´ life-style risk factors measured as:
• Low density lipoprotein (LDL), high density lipoprotein (HDL) and total cholesterol measured as mmol/ml
• Systolic blood pressure measured as mmHg
• BMI, measured as weight (kg)/height (m) 2
• Smoking status, measured as yes/no
• Physical activity measured as hours/week of exercise, daily steps, heart rate recovery, 6-min-walk test, and the Metabolic Equivalent of Task (MET)
• Dietary habits measured as grams of fruit and vegetables per day and daily intake of saturated fat
• Self-management
RCTs included had to measure at least two outcomes. After completion of the intervention all outcomes were measured at followup with no restrictions regarding duration after CR in the included studies.
Search Strategy
The databases and trial registries searched included: PubMed, Scopus, and CINAHL for published studies, and clinical.trials.gov, and the WHO trial registry for unpublished studies. A three-step search strategy was utilized. An initial limited search of PubMed, Scopus and CINAHL was undertaken followed by an analysis of the index terms and the text words contained in the title and abstract. A second search using all identified keywords and index terms was then undertaken across all included databases and the trial registries. Third, the reference list of all identified papers was searched for additional studies.
Studies published in English, Danish, Swedish or Norwegian were considered for inclusion. Only papers published after January 1, 2000 were considered for inclusion. This was because secondary prevention underwent several changes during 1990-2000 including new recommendations in medical treatment (i.e. ACE inhibitors and statins) as well as invasive treatments (e.g. primary PCI and implantable cardioverter-defibrillators and more uniform guidelines were published and endorsed) [13,14]. Since 2000, guidelines and recommendations regarding rehabilitation and secondary prevention have been regularly updated in international guidelines and still emphasize the same core components of CR [2,8]. The search included the following keywords for the concepts population and intervention, respectively: “coronary heart disease”; “cardiac rehabilitation”; “rehabilitation”; “prevention programme”; guidelines, recommendations; “patient education”; “patient management”; “secondary prevention”; “guidelines as topic”; “patient education as topic”; “health planning guidelines”; “patient care management” (Appendix I: Search strategy).
Assessment of Methodological Quality
Papers selected for retrieval were assessed by two independent reviewers (AM, KH) for methodological validity prior to inclusion in the review using the standardized critical appraisal instrument from the JBI. Any disagreements that arose between the reviewers were resolved through discussion, or with a third reviewer (ML). Papers were included if they met seven out of ten criteria: "truly randomized", "withdrawal described", "comparable control and treatment groups", "identical treatment between groups", "equal measurement of outcomes in groups", "reliable measurement" and "appropriate statistical analysis", respectively. The three criteria regarding blinding were not to be met (Appendix II: Quality assessment of included studies).
Data Extraction
Quantitative data was extracted by two independent reviewers (AM, KH) including: specific details about the interventions, populations, study methods, time to follow-up, and outcomes of significance to the review question and specific objectives. All results were subject to double data entry. Effect sizes were planned to be calculated and be pooled in statistical meta-analysis. However, if this was not possible the findings would be presented in narrative form including tables to aid in data presentation where appropriate. In studies with missing data; i.e. standard deviations, the authors e-mailed the corresponding author in order to complete the recording. Eight of the 15 authors responded and these data were added for the analysis.
Results
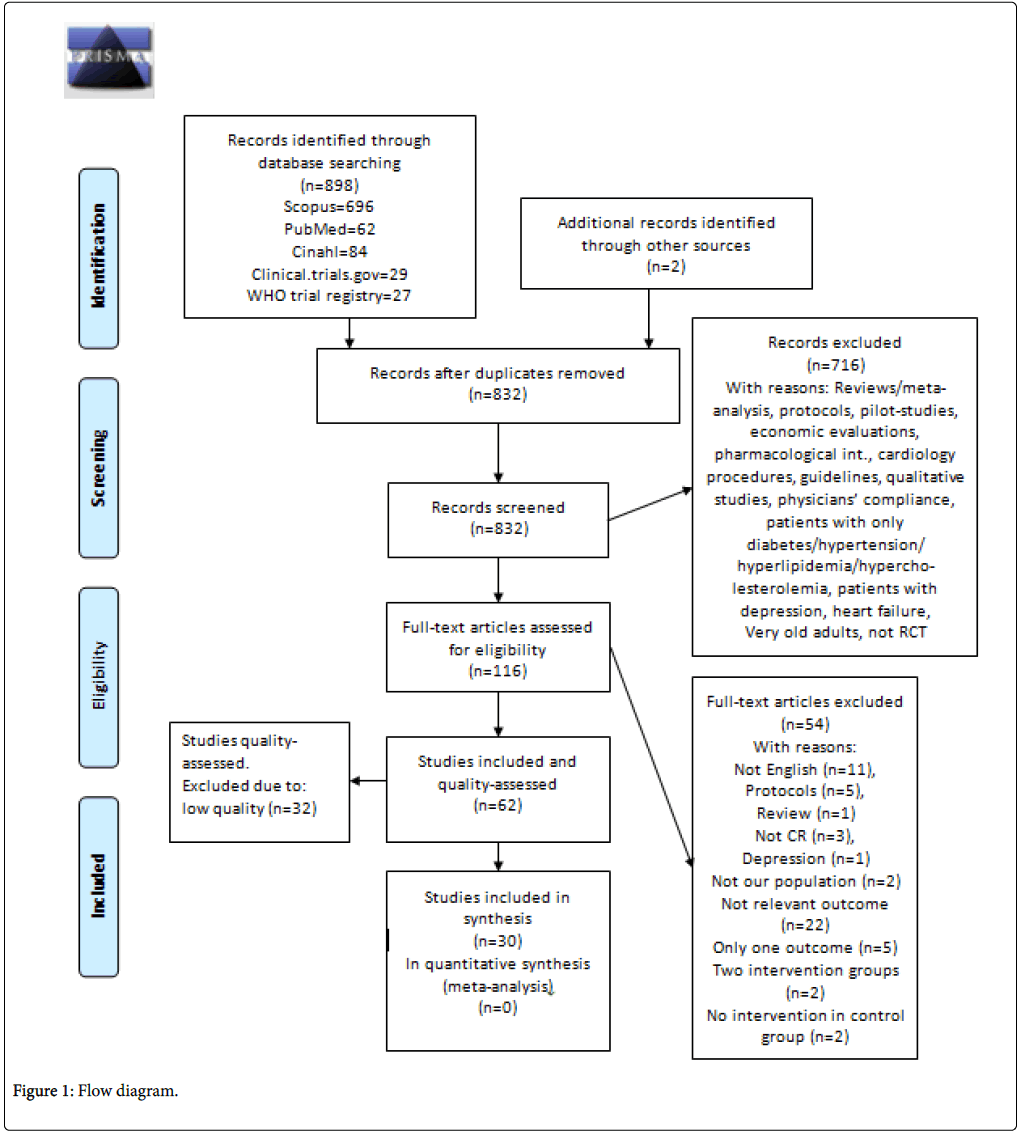
The database search identified 898 papers and two papers were identified through other resources (Figure 1). At relevance screening by reading the title and abstract by two independent reviewers, a total of 716 RCTs were excluded for not meeting the inclusion criteria due to the following reasons: reviews/meta-analysis, protocols, pilot-studies, economic evaluations, pharmacological interventions, cardiology procedures, guidelines, qualitative studies, studies on physicians’ compliance, no abstract. RCTs with CHD patients focusing on diabetes, hypertension, hyperlipidemia, hypercholesterolemia, depression, heart failure or very old adults were also excluded. Consequently, full text was sought for the 116 RCTs which were assessed for eligibility of which 54 were excluded, with reasons. Consequently 62 RCTs were included and underwent critical appraisal. The majority of exclusions were due to not fulfilling the criteria “truly randomized”.
After quality assessment the review included a total of 30 high quality RCTs (total N=12,206) with median follow-up 23 months (1 month-5 years). Details of included papers with characteristics of the CHD patients, settings and types of expanded CR interventions are presented in Table 1. Two papers reported on the same RCT and only reported on cholesterol level after two different follow-up periods [15,16]. Houle et al. reported on cholesterol, BMI, hypertension, and smoking [17], and in a later paper from the same RCT on physical activity only [18]. A mapping of the contents and types of intervention is presented in table 2. RCTs with shorter follow-up time than prescribed in CR [19,20], and sample sizes below 100 participants are indicated by footnotes [18,21,22]. Twenty of the expanded interventions were based on individual case management (e.g. personcentred advice coached by health professionals). Of the individualized interventions three different RCTs were based on mobile technology case-management [23-25], and in four RCTs [15,16,26,27] the intervention was delivered partly based on mobile technology. Six RCTs were home-based of which two expanded CR interventions showed significant increase in physical activity compared to standard CR [18,19]. However, the sample size was small in the study by Houle et al. [18], and the follow-up time was shorter than the usually prescribed 3 months in Peixoto et al.´s study [19].
| Methods Country | Participants | Intervention A Expanded CR in addition to usual care | Intervention B Usual care/Standard care | Notes | Study Year |
|---|---|---|---|---|---|
| Nurse case management USA | Patients with CHD recruited during hospitalization after coronary revascularization. N=228 | Case management CR by a nurse for 1 year after discharge. Nurse and GP/cardiologist participated in partnership of managing the patients´ lipids. 1 outpatient visit 4-6 weeks after discharge. Follow-up 1 year (telephone) |
Standard discharge teaching and physical therapy instructions. Included guidelines for activity, monitoring pulse, temperature, diet and personal exercise instructions for the first weeks after discharge. Observed by GP or cardiologist. Written results of lipid profile at 4 weeks, 6 and 12 months after discharge. Received recommendations about diet and physical activity again at follow-up. | Control of hypercholesterolemia in patients who have undergone coronary revascularization can be improved by a nurse case-management program. Favourable changes in lipids and lipoproteins were accompanied by significant improvements in dietary and exercise patterns in the intervention group. | Allen JK [33] |
| Intensive lifestyle programme Sweden | Women <65 years with CHD. N=130 | Intensive lifestyle programme (physical exercise, smoking cessation, dietary advice) including stress management. Year 1: 10 days+5 days+2 days in-patient CR. Year 2-5: 2 days in-patient CR twice a year. Year 0-5: Baseline+yearly medical and psychosocial examinations. Follow-up 5 years. |
Conventional post-hospitalization which depended on the hospital. The most common was physiotherapy (bicycling or aerobics) twice a week for about four weeks and information on healthy food and adverse effects of nicotine. Year 0-5: Baseline + yearly medical and psychosocial examinations. | This extensive intervention programme reduced visits at emergency wards and numbers of in-patient days, which in the long run may have beneficial effects on public finances and the patient's quality of life. | Andersson A [30] |
| University hospitals Netherlands | CHD patients, 35-68 years, who felt exhausted after PCI. N=710 | Group based behavioural therapy focusing on stressors leading to exhaustion and on support for recovery by promoting rest. Groups of 6 patients met weekly during the first 10 weeks, and once a month the following 4 months. Sessions lasted 2 h. Follow-up 1½ year | Routine check-ups in all four centres and referral to a physical rehabilitation in one centre. | A group based behavioural intervention focusing on stressors did not reduce the risk of new CHD events. However, it had a beneficial effect on patients' feelings of exhaustion. | Appels A [49] |
| Prolonged secondary prevention program on recurrent hospitalization Australia | CHD patients with private health insurance N=602 | Usual post discharge care (UC) with nurse-led, home-based intervention. Comprehensive home-visits 1-2 weeks after discharge. Screening into three groups (low, medium, high risk). Visits, telephone coaching, referral to other health professionals accordingly to screening. Repeated home visits if readmitted. Follow-up 2 years | Usual post discharge care: Typically ongoing care by the treating specialist physician and a family physician with specialist follow-up as clinically indicated. | Special group of CPs (privately insured), no reduction in readmissions. Gender difference | Carrington MJ [50] |
| TEXT ME (tobacco, exercise and diet messages). Large tertiary hospital Australia | Patients with proven CHD (prior myocardial infarction or proven angiographically) N=710 | 4 text messages per week for 6 months. Text messages provided advice, motivational reminders, and support to change lifestyle behaviours. Messages for each participant were selected from a bank of messages according to baseline characteristics (e.g. smoking) and delivered via an automated computerized message management system. The program was not interactive. Follow-up 6 months | Generally community follow-up with the majority referred to inpatient CR as determined by their GP. | TEXT ME showed significant improvement regarding blood pressure, LDL-C, physical activity, smoking, and the majority >86% found TEXT ME useful, easy to understand, and appropriate in frequency. Messages were based on baseline data. | Chow CK [23] |
| Falkirk and District Royal Infirmary Scotland | Inpatients and outpatients >60 years attending secondary care, with angina or AMI N=320 | Mentoring groups for 1 year, meeting monthly for 2 h, each led by two trained lay health mentors in addition to standard care. Trained senior lay health mentors. Follow-up 1 year | Standard care (no more information) | Mentoring by lay trained seniors significantly improves diet, exercise score, SF-36 PF and use of health care. Attention rate was high, socio- economic grouping did not alter participation | Coull AJ [39] |
| Two hospital sites, follow-up at cardiac clinic and primary care centres Sweden | Patients with acute coronary syndrome <75 years. N=199 | Person-centred care process, emphasising the patient as a partner in care. Care was co-created in collaboration between patients, physicians, registered nurses and other health care professionals and documented in a health plan. A team-based partnership across three health care levels included transparent knowledge about the disease and medical state to achieve agreed goals during recovery. Follow-up 6 months |
When assessed as medically stable, patients were referred to their regular primary care centre, where medication and rehabilitation was planned by the primary care physician (where appropriate, with other health care professionals). Medical referrals and discharge notes were shared by health care professionals at the units but not necessarily with patients. Followed guideline-directed care. After hospital discharge patients underwent two standard individual cardiac check-ups at an out-patient cardiac clinic, one led by a registered nurse after 2-3 weeks and one by a physician after 4-6 weeks, where they were given advice and informed about the condition. | Person-centred care approach emphasising the partnership between patients and health care professionals throughout the care chain improves general self-efficacy without causing worsening clinical events. There was no difference between groups on re-hospitalisation or death, return to work or prior activity level | Fors A [40] |
| 3-month outpatient CR program. Followed by randomization Italy | Patients with recent AMI. N=52 | 3-month outpatient CR program. Followed by 2 years, multifactorial continued educational and behavioural intervention implemented into a cardiac rehabilitation setting. Follow-up 2 years | 3-month outpatient CR program, exercise 3 times/week (a cardiologist, a nurse and a physiotherapist supervised the training), risk factor assessment, life style management. | Long-term, multifactorial educational and behavioural intervention maintained for 2 years in a multi-comprehensive CR setting represents a valid strategy for improving long-term cardiovascular functional capacity and cardiovascular risk profile in post infarction patients. | GiallauriaF [21] |
| A long-term, relatively intensive rehabilitation strategy after MI Italy | Patients with recent MI. | Multifactorial, continued educational and behavioral program performed by a CR team: specialist cardiac nurse, physiotherapist, cardiologist (supervisor). A clinical psychologist and occupational therapist could be recruited. An informing letter was sent to patients' GP and inviting their collaboration. Comprehensive CRCR sessions with one-to-one support were held monthly from 1 to 6 months, then every 6 months for 3 years. Each session consisted of 30 min of supervised aerobic exercise, plus lifestyle and risk factor counseling lasting at least 1 h and reinforcement of preventive interventions lasting 30 min. To improve adherence and help patients adopt a positive role in the care of their own health, a booklet explaining how to deal with exercise, diet, smoking cessation, and stress management was distributed. The mutual support of family members was encouraged in ad hoc meetings together with the patients. Follow-up 3 years |
Standard CR lasting approximately 1 month and consisting of supervised exercise sessions and comprehensive lifestyle and risk factor management along with optimization of medical therapy. Thereafter a letter was sent to GP recommending secondary prevention goals. After the standard, post-MI CR, patients in the usual care group reported to their reference center only to undergo the 6-month and then annual scheduled assessments. After each assessment, a copy of the results of laboratory and exercise tests was forwarded to the GP who was responsible for any further medical decisions. |
The GOSPEL Study is the first trial to our knowledge to demonstrate that a multifactorial, continued reinforced intervention up to 3 years after rehabilitation following MI is effective in decreasing the risk of several important CV outcomes, particularly nonfatal MI, although the overall effect is small. | Giannuzzi P [9] |
| Secondary prevention in primary health care project Sweden | 75 years or younger who were discharged from the hospital after a CHD event within the past 12 months N=362 | Psychosocial factor intervention (cognitive behavioural therapy (CBT): stress management) 20 2-h session during 1 year. Group sessions with 5-9 participants divided by gender. Follow-up 2 year | Traditional risk factor optimization efforts during follow-up. | CBT decreases risk of recurrent CVD and MI. After 2 years patients' smoking habits, blood pressure, lipid levels, exhaustion, coping, credence significantly changed. | Gulliksson M [29] |
| CR centre Canada | Patients with an acute coronary syndrome. N=65 | Socio-cognitive intervention associated with a pedometer-based program on physical activity, cardiovascular risk factors and self-efficacy expectation during one year. Clinician nurse specialist-led, home-based intervention an access to rehabilitation centre. Assesment at 3, 6, 9 and 12 months. Follow-up 1 year. | Standard advice, access to rehabilitation centre | Same study population as Houle 2012. Study supports development of the home-based CR program using socio-cognitive intervention associated with a pedometer | Houle J [17] |
| CR centre Canada | Patients with acute coronary syndrome event N=65 | 6 consultations with a clinical nurse specialist during 1 year. Pedometer-based program associated with a socio-cognitive intervention on physical activity behaviour, cardiovascular risk factors, and quality of life during the year after an acute coronary syndrome event. Follow-up 1 year | Usual care at discharge regarding physical activity, diet and medication. Patients had no restrictions to go to a centre-based CR program or to consult a health care professional such as a nutritionist, an exercise specialist or a psychologist. All patients received usual medical follow-up by their own GP or cardiologist. | Consultations every two month during a year, self-monitoring pedometry and socio-cognitive intervention improves physical activity and quality of life | Houle J [18] |
| Intensive nursing monitoring and follow-up China | CHD patients undergoing PCI. N=807 | Standard secondary prevention+close nurse-led monitoring and electronic follow-up check by nurse. Follow-up 1 year. | Standard secondary prevention according to guidelines with conventional follow-up. | Intensive nursing care by the electronic follow-up system may lead to an improvement in quality of secondary prevention after PCI, including risk factor control, the use of medication, and self-management abilities. | Hu X [34] |
| Home walking intervention Australia | Women with CHD, recruited by telephone interview. N=154 | 12-week home walking intervention after completion of outpatient CR on HRQL and maintenance of physical activity. Assessment with questionnaire at 3, 6 and 12 months. Follow-up 1 year | Usual care (attendance once weekly for 6 weeks with no other support or follow-up) | For women a mini intervention and follow-up with self-reported questionnaire increased their maintenance of 30 min. walking three times a week | Johnson NA [38] |
| Multicentre trial in secondary and tertiary health care-setting Netherlands | Patients admitted for acute coronary syndrome. N=754 | Nurse-coordinated prevention program. 4 out-patient nurse clinic visits, focus on healthy lifestyles, risk factors and medication adherence. Follow-up 1 year | Outpatient clinic visits to treating cardiologists and other relevant specialists. Included referral to CR according to national guidelines. Consisted typically of 12 weeks programme including physical exercise and education. | Hospital-based, nurse-coordinated programme results in sustained lowering of cardiovascular risk. Data suggest the counseling component prevents readmissions | Jorstad, Harald T [36] |
| Secondary prevention programme. Inpatient rehabilitation. Germany | Middle-aged (58 years) CHD patients of low educational level. N=600 | 3-week comprehensive cardiovascular inpatient rehabilitation programme at the beginning. One further rehabilitation session in hospital after 6 months and regular telephone reminders over a period of 36 months. Follow-up 3 years | 3-week comprehensive cardiovascular inpatient rehabilitation programme at the beginning. Authors report that there is no information on the frequency and quality of usual care. | Telephone reminders during 3 years following usual CR had positive impact on risk in a low-education (predominantly male), middle-aged cohort | Mayer-Berger W [26] |
| Home-based training Norway | Patients undergoing coronary artery bypass surgery (CABS). N=26 | 4 weeks of home-based aerobic interval training 3 times/week for 6 months. Offered 60 min theoretical background on the intervention, the benefits of the intervention and practical information at first. Follow-up 6 months | 4 weeks of residential rehabilitation. Exercise, diet counselling, smoking cessation programme, lectures on healthy life style in general. | AIT patients reported good adherence to exercise training. Even though these first data indicate positive effects of home-based AIT in patients undergoing bypass surgery, more studies are needed to provide supporting evidence. | Moholdt T [22] |
| Heart rate monitored exercise for 1 year after outpatient CR rehabilitation USA | Patient with a recent cardiac event (MI, CABG, angioplasty). N=250 | 5 small-group cognitive-behavioural change counselling sessions. Participants are taught self-efficacy enhancement, problem-solving skills, and relapse prevention strategies to address exercise maintenance problems. 3 times/week in 1 ½ h in the last 3 weeks of the CR plus 2 sessions 1 and 2 months after completing CR. Free. The costs for nurse salary and teaching material were about 30 dollars. Follow-up 1 year | Usual care (No more information) | Usual-care group were 76% more likely than those in the CHANGE group to stop exercising during the year following a CR program | Moore SM [37] |
| Secondary prevention Spain | Patients with acute coronary syndrome or stroke. N=247 | Health education by a trained nurse. Comprehensive and intensive treatment of cardiovascular risk factors. Visits 2, 5, 12, 24 months after the acute episode. Follow-up 3 years | Follow-up in cardiology or neurology and/or primary care consulting offices, annual consulting to monitor lifestyle factors, treatment etc. | After the intervention the absolute risk of cardiovascular morbidity and mortality was reduced after 3 years in high risk population | Moreno-Palanco MA [28] |
| Hospital-based secondary prevention program USA | Women hospitalized with CHD. N=304 | Education and counseling by a prevention facilitator/educator during hospitalization and during phone visits at 2, 4, and 12 weeks and a phone or clinic visit at 6 weeks post-discharge. Prevention facilitators were non-physician, non-nurse health professionals who had formal training in health education, nutrition, medical technology, or public health and underwent standardized training by the New York-Presbyterian Hospital Preventive Cardiology Program professional staff. The initial educational session included: 1 h of structured counseling before discharge that reviewed smoking, exercise, nutrition, weight, blood pressure and cholesterol goals based on the AHA/ACC guidelines, information on how to achieve them based on social learning theory and the five A's construct (ask, advise, agree, assist, arrange). Prevention facilitators and participants agreed on specific, achievable goals and developed action plans. Participants received feedback on their goals and health behaviors, and advice on recommendations for behavior change personalized to their specific needs. Dates and times for follow-up visits and phone calls were arranged at the end of the initial educational session. Follow-up 6 months. |
Patients were encouraged to attend CR and to exercise a minimum of 3-5 days/week. The facilitator instructed the patient on heart rate guidelines and Borg perceived exertion levels based on treadmill test results as outlined by the American College of Sports Medicine's Guidelines for Exercise Testing and Prescription. Nutrition counseling was based on the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Patients were encouraged to stop smoking and avoid secondhand smoke and were referred to formal smoking cessation programs as appropriate. All subjects were informed that use of beta-blockers, aspirin or antiplatelet agents, and ACE inhibitors often is recommended for patients with CHD, and criteria for contraindications were reviewed. |
After 6 months minority women were 2.4 times more likely to reach the blood pressure goal, and white women were 2.86 times more likely to report use of beta-blockers compared with minority and white women, respectively in usual care | Mosca L [31] |
| Multicentre trial in general practices Ireland | Patients with established CHD. N=664 | Tailored care plans for practices (practice based training in prescribing and behaviour change, administrative support, quarterly newsletter), and tailored care plans for patients (motivational interviewing, goal identification, and target setting for lifestyle change) with reviews every four months at the practices. Follow-up 1½ year | Control practices provided usual care consisting of annual review of blood pressure, cholesterol concentration, smoking status and prescribed drugs in accordance with the criteria specified within the NHS GP contract quality and outcomes framework for the management of coronary heart disease. | Hospital-admission was reduced after the complex intervention, but no clinical benefits were shown after 18 months, possibly due to ceiling effect, and the study may be underpowered | Murphy AW [32] |
| Medium intensity case-management program. Switzerland. | Patients with coronary artery disease. N=201 | An hour of counselling by a clinician during hospitalization and two short reminders by phone and mail 3 and 6 months later. Treatment decisions were left to patients and their primary care physicians. Follow-up 1½ year | Usual care. During hospitalization patients were treated by the regular house staff of the department of internal medicine. Information about cardiovascular risk factors were given solely by the treating physicians and no structured counseling programme was offered. 9 months follow-up. | The authors conclude that this hospital-based case-management and outreach program, limited to counselling by a clinician, did not substantially improve cardiovascular risk factor control among patients hospitalized for coronary events. | Nordmann A [27] |
| Early CR Brazil. | Patients who recently experienced an acute myocardial infarction (AMI) N=88 | After the same inpatient care plan, low-risk patients who experienced an AMI were randomized into 2 groups. The intervention group entailing outpatient (unsupervised) CR primarily cantered on a progressive walking program. Follow-up 1 month | Supervised exercise program with early mobilization beginning 12 h after an AMI. | A CR program based on early progressive exercises, initiated by supervised inpatient training and followed by an unsupervised outpatient program, improved HRQL and functional capacity in patients at low cardiovascular risk. This CR program took place very early, short time after patients experienced CR. Difficult to compare with Danish CR in phase 2. | Peixoto TCA [19] |
| Expanded CR Sweden | Patients with recent acute MI or CABG. N=224 | 1 year stress management programme, increased physical training, staying at a "patient-hotel" for 5 days after the event and cooking sessions. Follow-up 5 years. | Physical training 60 min 2 times/week for 3 months, counseling with cardiologist, heart school 2 x 90 min. (performed by nurse, dietician, physiotherapist or welfare officer), smoking cessation in group or individual. | Reduced number of cardiac events and days in hospital in expanded group. Non-significant difference in death. | Pluss CEC [10] |
| The CardioFit internet-based expert system Canada and England | Patients with acute coronary syndromes. N=223 | The patients received a personally tailored physical-activity plan upon discharge from the hospital and access to a secure website for activity planning and tracking. They completed five online tutorials over a 6-month period and were in email contact with an exercise specialist. Follow-up 1 year. | Physical activity guidance from an attending cardiologist. | Using an internet-based activity prescription with online coaching increased physical activity at follow up. Use of the CardioFit program could extend the reach of rehabilitation and secondary-prevention services. The system was designed to promote physical activity in CHD patients who were not participating in CR. | Reid RD [24] |
| Exercise training Portugal | Patients with a first AMI. N=38 | Patients participated in an 8-week aerobic exercise programme. 3 times/week for 8 weeks. Follow-up 2 months | Standard medical care and follow-up(No more information) | Exercise training improved autonomic function, assessed by heart rate recovery, resting heart rate and systolic blood pressure, in the absence of changes in diet or medication. The study is not regarding CR as a whole, but only about exercise. | Ribeiro F [20] |
| Coronary Artery RIsk MAnagement Programme. Day-hospital Italy | Patients with acute coronary events. N=168 | CARIMAP delivered by the rehabilitation day-hospital. Individualized management program. Programme lasted 3-7 months and the patients were assessed in the end according to risk profile and drug therapy. Follow-up 9 months | After intensive rehabilitation patients were referred to their GP and cardiologist. Assessed after 9 months. | Sturchio A [35] | |
| Coaching (COACH) study Australia | CHD patients N=219 | The Coaching patients On Achieving Cardiovascular Health (COACH) Program: Regular personal coaching via telephone and mailings to achieve the target levels for their particular coronary risk factors. There was one coach per hospital either dietician or nurse. Follow-up 2 years. | When discharged a 1-page chart of risk factor targets for the secondary prevention were sent to GP. Patients were contacted after 24 months to arrange follow-up. | Vale MJ [16] | |
| Coaching intervention and telephone follow-up Australia | CHD patients <75 years who had been hospitalized for CABG or PCI. N=245 | Coaching intervention. Performed by a dietician with background as educator and working with cardiovascular disease. Telephone contact 2 weeks after first coaching session. 3 telephone calls with 6 weeks interval. Telephone contact after 24 weeks – Follow-up 6 month (telephone). | Offered information about a CR-programme and encouraged to participate (the same as intervention A). Contacted by telephone 2 weeks after randomization. Offered information about a CR-programme and encouraged to participate. Contacted by telephone after 24 weeks-before 6 month follow-up. | Coaching had no impact on total cholesterol levels, but to being prescribed lipid-lowering drug therapy (P<0.001). The effectiveness is best explained by both adherence to drug therapy and to dietary advice given. Coaching may be an appropriate method to reduce the treatment gap in applying evidence-based medicine to the "real world". | Vale MJ [15] |
| Internet based vascular risk factor management Netherlands | Patients with clinically manifest vascular disease. N=330. | Personalised website with an overview and actual status of patients' risk factors and mail communication via the website with a nurse practitioner for 12 months; the intervention combined self-management support, monitoring of disease control, and drug treatment. Follow-up 1 year. | Asked to contact their treating physician at the hospital or GP for risk factor management. The treating physician at the hospital or the GP was also informed about of the risk factor status in writing. | An internet based, nurse led treatment programme on top of usual care for vascular risk factors had a small effect on lowering vascular risk and on lowering of some vascular risk factors in patients with vascular disease. Be aware that at baseline, the Framingham heart risk score was higher in the intervention group than in the usual care group. No information on N in each randomization group. | Vernooij JW [25] |
Table 1: Included studies. AMI: Acute Myocardial Infarction; CABG: Coronary Bypass Graft Surgery; CHD: Coronary Heart Disorder; CR: Cardiac Rehabilitation, GP: General Practitioner; MI: Myocardial Infarct; PCI: Percutaneous Coronary Intervention.
| Individual case management | Group-based | |
|---|---|---|
| Home-based | Carrington [50], Houle, b [17], Houle* , b [18] | |
| Johnson [38], Moholdt, b [22], Peixoto* , a [19] | ||
| Mobile technology | Chow* [23], Reid* [24], Vernoij* [25] | |
| Partly by mobile technology | Mayer-berger* [26], Nordmann [27], Vale* [15], Vale* [16] | |
| Coaching by health professionals Coaching by lay people | Fors* [40], Hu [34], Moreno-Palenco* [28] | Jorstad* [36], Sturchio [35], Coull [39] |
| Educational/behavioral/cognitive | Murphy* [22] | Gialluiari* , b [21], Mosca* [31] |
| Life-style based Stress-management and life-style based |
Allen* [33], Anderson* [30] | Ribeiro, a [20] |
| Giannuzzi* [14] | Appels [20], Gullikson* [29], Moore* [37], Pluss [10] |
Table 2: Contents and types of interventions. *Significant effect of expanded versus standard cardiac rehabilitation, p<0.05. a, follow-up time<3 months b, sample size<100 participants.
Due to heterogeneity among the health professionals involved in interventions, the settings, and time to follow-up statistical pooling was not possible, and a meta-analysis was not performed. Therefore, the findings are presented in narrative form. Table 3 presents available details of the data (mean values of outcomes, standard deviations) on the following outcomes: mortality, readmission, cholesterol, BMI, hypertension, smoking status, physical activity, dietary habits and measures of self-management, e.g. self-efficacy and risk score.
| Mortality All cause, Cardiac (n) | Readmission to hospital All cause, Cardiac (days/group) | Cholesterol Total, HDL, LDL (mmol/ml) | Body Mass Index | Hypertension Systolic pressure (mmHg) (n) >130/140 | Smoking Yes/No (%) | Physical activity | Dietary habits and self-management (n), (n%) | |
|---|---|---|---|---|---|---|---|---|
| Total 4.1 (0.7)/4.6 (0.6) p<0.0001 LDL: 2.2 (0.57)/2.67 (0.57) p<0.0001 HDL: 1.11 (0.31)/1.06 (0.24) p=0.15 | 6 MET h/week (>30 min moderate ex. 3 times/week): 40%/26% p=0.02 | Sat. fat: 10 (2.2)/11 (2.3) p=0.004 | Allen [33] | |||||
| Hosp.days/pt: 0.41 (2.43)/0.77 (1.86) p=<0.01 Emergency visits 0.10 (0.35)/0.52 (1.85) p=<0.05 | Andersson [30] | |||||||
| Card.adm: 81/69 p=0.44 Recurr. AMI: 4/11 p=0.07 N=366/344 |
Appels [49] | |||||||
| All cause: 8.8%/5.1 p=0.283 | Rate of all cause: 0.17/0.15 p=0.802 Card.adm: 148/147 | >130: 107/115>130: 42%/44% N=257/262 | At risk for future event 61%/72% | Carrington [50] | ||||
| p=0.158 Hospital activity: 1197/1200; NS | ||||||||
| Total: 3.9/4.1 p<0.001 HDL: 1.1/1.1 p=0.55 LDL: 2.04/2.17 p=0.04 | 29/30.3 p<0.001 | 128/135.8 p<0.001 | 26/43 p<0.001 | MET min/week: 936 (70)/643 (68) p=0.003 Inactive <600 MET min/week: 37.4%/68.8% p<0.001 |
Chow [23] | |||
| Hosp.days/pt: 1.81/2.46 Card.days/pt: 0.99/1.25 NS |
15/14 NS |
MET: 843/767 NS |
Sat. fat: 10.5%/11.4% p<0.05 |
Coull [39] | ||||
| All cause: 0.04 (0.203)/0.02 (0.137) 4/2 NS |
Card.readm:0.15 (0.36)/0.13 (0.34) 14/14 NS |
Composite score (PA, SE, RTW, readm.) p=0.015 Self-efficacy 30.9 (5.1)/30.5 (5.3) 21/10 p=0.018 | Fors [40] | |||||
| Total: 4.2/5.7 p<0.001 HDL: 1.3/0.9 p<0.001 LDL: 2.3/3.9 p<0.001 | 26.7 (2.5)/28.3 (2.9) p<0.001 | 120/130.6 p<0.001 | Giallauria [21] | |||||
| All cause: 34/43 p=0.29 Cardiac: 18/24 p=0.35 | Recurr. AMI: 23/44 p=0.01 | Total: 4.0/4.7 p=0.4 LDL: 2.7/2.7 NS HDL: 1.3/1.3, NS | Increase 1.7%/2.1% p=0.03 | NS | NS | PA high level 23.8%/18.8% p=0.01 | Life style habits diet p<0.001 Self/stress management p<0.001 | Giannuzzi [9] |
| All cause: 23/25 NS Cardiac: 1/3 | Fatal/non-fatal CVD event: 69/77 p=0.002 Recurr. AMI: 41/50 p=0.007 | Gulliksson [29] | ||||||
| LDL:1.7 (0.40)/1.9 (0.9) NS HDL: 1.2 (0.3)/1.2 (0.3) NS | 126 (13)/ 123 (16) p=0.335 | 4 (21)/27 (46) p=0.166 | Houle [17] | |||||
| 7500 steps: 83/55 p=<0.05 | Houle [18] | |||||||
| Total: 3.76 (0.98)/3.99 (1.08) p=0.002 LDL: 2.42 (0.81)/2.72 (1.01) p=0.0001 |
24.2 (6.2)/25.1 (5.1) p=0.025 |
135.7 (14.6)/142.4 (11.5) p=0.0001 |
30-45 min 4-5 days/w:254 (62.6)/155 (38.7) p=0.0001 |
Dietary control: 226 (55.6)/105 (26.2) p=0.0001 |
Hu [34] | |||
| % regular PA: 77/56 MacNew score: 6.38/6.31 p=0.51 | Johnson [38] | |||||||
| Total >4,5: 254/251p=0.74 HDL>1:243/237 p=0.99 N=359/348 | >25: 77/94 p=0.09 |
>140: 264/211 p<0.001 |
Smoking status: 83/85 p=0.72 |
30 min/5 days: 239/192 p=<0.001 |
veg.>200 g: 286/244 p=0.007>2 fruits/day: 332/292 p<0.001 |
Jorstad [36] | ||
| All cause 8 (2.6)/9 (2.4) N=271/329 NS | Recurr. AMI 34/54 p=NS Other card. events 28/62 p<0.05 | Hours/week: 13.25/7 p=0.083 N=211/272 | Maye-Berger [26] | |||||
| N=211/272 | ||||||||
| Total 4.3 (0.7)/4.3 (1.0) NS HDL 1.2 (0.4)/1.4 (0.4) NS | Heart rate recovery 1 min. 24.8 (11.5)/24.8 (13.3) | Moholdt [22] | ||||||
| Exercise times/month 7.6 (7.0)/7.1 (8.2) Controls 76% more likely to stop exercising during the year following CR p=0.02 | Self-efficacy-adherence 69.4 (37)/70 (36.3) | Moore [37] | ||||||
| 4/17 N=121/126 Survival rate 97.4%(1.5)/85.5% (3.1) p=0.003 | Cardio event 16.1%/44.6%26/54 N=118/121 p<0.05 | HDL 1.39/1.30 p=0.14 LDL 2.05/2.42 p<0.005 | 28.82 (4.26)/29.39 (5.31) NS | 123.2 (15.1)/128.5 (20.4) NS | Moreno-Palanco [28] | |||
| Persons 0.4 (0.7)/0.5 (1.0) N=415/435 p=0.03 Persons 0.14 (0.5)/0.23 (0.7) N=425/444 p=0.04 | LDL >2,5 54/50 N=94/84 NS | 18-25 & waist<90 22/20 N=108/109 NS | 42%/45% N=116/111 NS2,5 more likely to reach blood pressure goal |
15/6 N=112/108 S (p not reported) | 30 min, 3d/week: 41%/32% N=108/105 NS | [31] Mosca | ||
| Persons 0.4 (0.7)/0.5 (1.0) N=415/435 p=0.03 Persons 0.14 (0.5)/0.23 (0.7) N=425/444 p=0.04 | Total 4.2 (0.9)/4.2 (0.9) N=342/391 NS | 28.4 (5)/28.7 (4.8) N=351/399 NS | 133.8 (17)/137.9 (19.3) N=360/405 NS | Murphy [32] | ||||
| 28/20 NS | Nordmann [27] | |||||||
| 6-min-walk test 519.7 (79.3)/452.1 (111.2) p<0.001 | Peixoto [19] | |||||||
| AMI: 5/15 All cause hosp./person: Reduction intervention group p=<0.01 Total hosp.days/person: 6/10 p=0.02 | Pluss [10] | |||||||
| Total 5.2/5.4, NS | 122.5 (13.0)/ 121 (14.1), NS | Ribeiro [20] | ||||||
| Steps/day: 7392 (3365)/6750 (3366) p=0.023 vigorous PA: 201.4 (169.6)/179.8 (152.6) p=0.047 | Reid [24] | |||||||
| Total 4.53 (1.09)/5.52 (1.19) p<0.05 LDL 2.67 (0.98)/3.37 (1.17) NS | 125 (19)/130 (45) p<0.05 | 20/57 p<0.05 | Sturchio [35] | |||||
| Total 4.48/4.72 p<0.0001 | Vale [16] | |||||||
| Total 5.0/5.54 (N=107/112) p=0.0001 LDL 3.11/3.57 (N=96/105) p=0.0004 HDL 1.12/1.16 (N=98/106) p=0.4035 | Vale [15] | |||||||
| Total 4.3 (0.9)/4.5 (1.0) NS HDL 1.3 (0.4)/1.3 (0.4) NS LDL 2.3 (0.7)/2.6 (0.9) LDL <2.5: 18.4%/30.9% p=0.004 | 28.6 (4.1)/27.9 (4.2) NS | 137 (18)/140 (19) >140: 101/105 NS | 77/87 p=0.038 | Framingham risk score: -12%/-8% | Vernooij [25] |
Table 3: Results of the interventions. HDL: High-Density Lipoprotein; LDL: Low-density Lipoprotein; MET: Metabolic Equivalent of Task; NS: Non-Significant.
Results on mortality (due to all causes and cardiac events) were included in six RCTs, of which only one attained significant results on mortality after the expanded CR intervention [28] and Gullikson et al reported significantly 41% fewer CVD events compared to the control group (hazard ratio 0.59, 95% CI 0.42-0.83), p=0.002 [29].
Regarding readmission (due to all causes and cardiac events) 12 RCTs in total reported this outcome, of which eight RCTs reported significant effect on reduction of readmission after the expanded CR intervention [9,10,26,28-32]; i.e. Gullikson et al reported 38% fewer recurrent AMI events, p=0.02 [29].
At time for follow-up cholesterol level was the most included outcome. Cholesterol (level of total, HDL, and LDL) was reported in 17 RCTs of which nine of the expanded CR interventions reported significant decreases in total cholesterol, HDL and/or LDL-level, respectively [15,16,21,23,25,28,33-35]. However, in two studies the sample size was small; therefore the effect estimation is less robust [21,22].
BMI was reported with favourable effect in four of 10 RCTs of the expanded CR intervention compared to standard CR [9,21,23,34] of which two RCTs included a small sample size [21,22].
Hypertension measured by systolic blood pressure was included in 13 RCTs of which five reported significant differences between the expanded CR and standard CR [21,23,34-36]. Besides Jorstad et al. reported the percentage of participants with blood pressure>140 mm Hg, which in the groups compared were 264% vs. 211%, p<0.001 [36].
In total 14 RCTs reported on physical activity/exercising by a number of different outcome measures (hours/week of exercise, daily steps, heart rate recovery, 6-min-walk test, and the Metabolic Equivalent of Task (MET). In nine of these the expanded CR resulted in significantly better outcomes compared to standard CR [9,18,19,23,24,33,34,36,37]. Five RCTs were exercise-only programs focusing on physical activity promotion [18,19,24,37] and only the study by Johnson et al. resulted in a non-significant difference, between groups [38]. One RCT found that the number of participants defined as inactive (by <600 MET minutes/week) was significantly less in the expanded CR compared to the standard CR group, 37.4% vs . 68.8%, p<0.001 respectively [23]. Another RCT found that participants receiving standard CR were 76% more likely to stop exercising during the year following CR than participants receiving expanded CR, p=0.02 [37].
Among the five RCTs including dietary habits all reported significant intervention effect of the expanded CR compared to standard CR; e.g. decreased intake of saturated fat [33,39], healthier diet [9,34], and recommended daily intake of >200 g vegetables and >2 fruits, was reported among 286 vs . 244, 332 vs . 292 participants, respectively, p<0.01 [36].
A few RCTs reported significant effects on self-management (e.g. stress or self-efficacy in in a risk score) [9,25,40].
Discussion
Cardiac rehabilitation is the standard of care for CHD patients. This review demonstrated that expanded CR showed positive treatment effect compared to standard CR although narrow beneficial effects. The majority of the expanded CR was individual case management of which seven were based on mobile technology for coaching, feed-back and surveillance. The interventions were delivered in different settings (in patients´ homes, rehabilitation centers, or hospital-based).
This review found among the 30 included RCTs several significant reductions regarding clinical primary outcomes (e.g. death and nonfatal AMI), and favorable effect on several CHD lifestyle risk factors. The effects found were irrespective of patient case mix (i.e. % of AMI patients), characteristics of RCTs (i.e. sample size, location, length of intervention and follow-up), or year of publication. However, compared to an updated Cochrane review including 23 RCTs [41], this review only found effect on physical activity in two RCTs.
Two thirds of the RCTs did not report on readmission; mortality was even less often reported, and only one RCT found a significant difference between the groups. This finding is in accordance with a recent Cochrane review, which found only few RCTs reporting clinical effects and no effect on all-cause mortality and non-fatal AMI from interventions based on internet [42]. A new Cochrane review on education-based CR found some evidence of a reduction in events, but based on only two studies [43]. However, reductions on these clinical outcomes are important to evaluate in future studies on effect of CR; considering their significant impact on the patients´ QoL and on health care cost.
The effect on adherence to recommendations in secondary prevention guidelines could be explained by some of the multiple risk factors, CR usually target. For behavior changes regarding lifestyle risk factors, it was the intervention groups´ actual level at the time for follow-up which was compared to standard CR. However, management of adherence to healthy lifestyle recommended in secondary prevention such as dietary habits and exercise attendance was not reported except in Moore et al.´s study which focused on participants´ self-efficacy enhancement, problem-solving skills, and relapse prevention strategies addressed exercise maintenance, and found favourable intervention effect [37].
A majority of the expanded CR interventions were focusing on multiple life style risk factors, as seen in an overview of reviews [5]. However, cholesterol was the most common reported outcome, and most RCTs reported only few outcomes. Our findings on cholesterol, BMI, hypertension and smoking status are similar to those in a recent Cochrane review, which found some evidence for internet-based interventions on lifestyle behaviors; however no firm conclusions could be made [42]. Like in the present review the outcomes measured differed, there was incomplete reporting, studies reported at different follow-up times, therefore the interpretations of findings are very complex [42].
Although exercise therapy has been identified as a central element in guidelines for CR comprehensive programs, and are recommended by both the American and the European societies of cardiology [44], only some of the RCTs measured physical activity outcomes. Thus, the expanded CR often included exercise therapy but reported other outcome measures (readmissions, lifestyle habits). A recent metaanalysis on effect from exercise-based CR showed reductions from cardiovascular mortality, readmissions and improvements in health related QoL across patients and interventions types [44]. Only one RCT measured heart rate recovery, although it is more highly associated with overall risk than are physical activity and exercise therapy. Cardiorespiratory fitness is directly influenced by the maintenance of regular training, and a faster heart rate recovery after training has been shown to be associated with a decrease in cardiac events and mortality [20]. It seems that a home-based intervention is sufficiently effective regarding physical activity [18,19]. However, the adherence to daily activity was not reported on.
Our findings indicated that expanded CR may provide treatment benefit compared to standard CR. However, to determine whether the effect was sustained after the interventions´ follow-up, measures of adherence to lifestyle behavior is needed. A recent intervention with mobile technology-delivered CR program showed a lifestyle behavior change after 3 months compared to standard CR [45]. The adherence to healthy lifestyle behaviors was measured by a composite behavior score.
This review showed that an individual case management intervention based on mobile technology was seen to have significant impact on several lifestyle factors [15,16,23-25]. In one RCT text messages were tailored to the individual needs of the patient according to baseline lifestyle characteristics [23].
A new review including seven interventions delivered in part by mobile phone text messaging found that simple text appeared to most effective. Three of the interventions improved adherence to medication, and two studies significantly increased physical activity behavior [46]. In our review one of the expanded CR interventions present significant favourable results on a composite score based on physical activity, perceived self-efficacy and rate of return to work [40].
Strengths and Limitations
Our review included 30 RCTs fulfilling a strict quality assessment, thus the findings may be evident and not violated by bias. However, in some of the RCTs the sample size was small. Due to more variation than expected a meta-analysis could not be performed, which is a limitation.
The comparison groups in all RCTs were to be described as standard or usual care following guidelines. Thus, we excluded a study which compared the intervention with no intervention [47]. However, it was a limitation that the content of the usual care/standard CR were not thoroughly described, and that the studies were heterogeneous in terms of follow-up time.
Effect sizes were relatively modest, and due to variation of expanded CR components performing meta-analysis was impossible. In general, the lack of blinding resulted in a risk of performance bias. However, blinding of participants in CR or non-medical interventions in general is not possible.
Outcomes such as self-management (e.g. self-efficacy enhancement, problem-solving skills, and a composite score of self-efficacy, physical activity, and return to work were seldom reported. Stress management is not routinely included as a component of standard CR, despite considerable evidence that high stress is associated with health outcomes. In the present review one study reported effect on stress management after 3 years CR intervention [9], and a recent study showed that this component may benefit CHD participants in regard to heart disease biomarkers [48].
Although health-related QoL is another relevant factor in all patients´ lives, there is no universally accepted single measure used. Therefore the concept was not included. However, standard CR has been shown to improve QoL in CHD patients [48], and an updated Cochrane review on education-based CR also found evidence of improved QoL [43].
The review did not include risk scores, which is a limitation. Although these categorizations are arbitrary, they may be indicator of the likely benefits of prevention of future cardiac events and useful for both the individual patient and for the clinician in helping decide at which risk the patient belong and whether lifestyle modifications are needed. Only a few RCTs included risk scores such as the Framingham risk score [25].
Most often the RCTs did not include a detailed description of the content of the interventions in standard CR. Future RCTs ought to improve their quality of reporting, particularly in terms of risk of bias [8], details of the intervention and also content of standard CR. Furthermore, expanded CR should be tailored to sustainable lifestyle behavior changes measured by adherence to healthy lifestyle, and include outcomes of functioning not solely mortality and readmission [49,50].
The population included may be regarded as representative of CHD patients, and the results therefore used for minor groups of patients. Future RCTs may recruit patients who are less representative of the broader CHD population, both including those with stable angina and those at higher risk, e.g. with major comorbidities and disabilities.
Furthermore, the RCTs included relatively small study groups as well as varied outcome measures and follow-up times. It is a limitation that the findings of the RCTs are reported at different follow-up times. RCTs were generally of short duration (beyond 12 months) and the duration of interventions varied between 2 months and up to 5 years.
For future practice it is recommended that CR interventions are delivered by individualized mobile technology and tailored to the individual patient´s needs. Before this, there is a need for development of a standardized risk score instruments to help the clinician in decision of treatment.
Conclusion
In summary, this review found effect primarily on lifestyle risk factors of expanded CR compared to standard CR. Only few RCTs found effect on mortality and readmission outcomes. Thus, there was some evidence to suggest that expanded CR (e.g. person-centred mobile based interventions) have potential for use in CHD population and may be more beneficial than only standard CR following guidelines.
However, expanded CR should be tailored to sustainable lifestyle behavior changes measured by adherence to healthy lifestyle and outcomes of functioning. There is need for large scale and longer term studies of lifestyle behavior changes and complete reporting of management and adherence to lifestyle behaviour.
The review confirmed that expanded CR showed positive treatment effect compared to standard CR on lifestyle risk factors, whereas only few RCTs reported the mortality and readmission outcomes.
Conflict of Interest
There are no conflicts of interest to declare.
Acknowledgements
We thank the librarian from the Aarhus University Library, Hanne Caspersen for assistance in the search of literature.
References
- The Danish Heart Foundation (2007) Cardiac rehabilitation after the structural reform: rehabilitation and coherent patient courses for chronically ill: Inspiration for municipalities, regions, general practice, hospitals and others. Network of health promoting hospitals in Denmark.
- Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, et al. (2012) European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The fifth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur Heart J 33: 1635-1701.
- National institute for health and clinical excellence (NICE) (2010) Cardiovascular disease prevention.
- Scottish intercollegiate guidelines network (SIGN) (2002) Cardiac rehabilitation. A national clinical guideline.
- Anderson L, Taylor RS (2014) Cardiac rehabilitation for people with heart disease: An overview of cochrane systematic reviews. Cochrane Database Syst Rev 12: CD011273.
- Chatziefstratiou AA, Giakoumidakis K, Brokalaki H (2013) Cardiac rehabilitation outcomes: Modifiable risk factors. Br J Nurs 22: 200-207.
- de Vries H, Kemps HM, van Engen-Verheul MM, Kraaijenhagen RA, Peek N (2015) Cardiac rehabilitation and survival in a large representative community cohort of dutch patients. Eur Heart J 36: 1519-1528.
- Authors/Task Force Members, Piepoli MF, Hoes AW, Agewall S, Albus C, et al. (2016) 2016 European guidelines on cardiovascular disease prevention in clinical practice: The sixth joint task force of the european society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts): Developed with the special contribution of the european association for cardiovascular prevention & rehabilitation (EACPR). Eur J Prev Cardiol 23: NP1-NP96.
- Giannuzzi P, Temporelli PL, Marchioli R, Maggioni AP, Balestroni G, et al. (2008) Global secondary prevention strategies to limit event recurrence after myocardial infarction: Results of the GOSPEL study, a multicenter, randomized controlled trial from the italian cardiac rehabilitation network. Arch Intern Med 168: 2194-2204.
- Pluss CE, Billing E, Held C, Henriksson P, Kiessling A, et al. (2011) Long-term effects of an expanded cardiac rehabilitation programme after myocardial infarction or coronary artery bypass surgery: A five-year follow-up of a randomized controlled study. Clin Rehabil 25: 79-87.
- Nielsen KM, Meillier LK, Larsen ML (2013) Extended cardiac rehabilitation for socially vulnerable patients improves attendance and outcome. Dan Med J 60: A4591.
- Momsen AH, Hald K, Nielsen CV, Larsen ML (2017) Effectiveness of expanded cardiac rehabilitation in patients diagnosed with coronary heart disease: A systematic review protocol. JBI Database System Rev Implement Rep 15: 212-219.
- Balady GJ, Ades PA, Comoss P, Limacher M, Pina IL, et al. (2000) Core components of cardiac rehabilitation/secondary prevention programs: A statement for healthcare professionals from the American heart association and the American association of cardiovascular and pulmonary rehabilitation writing group. Circulation 102: 1069-1073.
- Giannuzzi P, Saner H, Bjornstad H, Fioretti P, Mendes M, et al. (2003) Secondary prevention through cardiac rehabilitation: Position paper of the working group on cardiac rehabilitation and exercise physiology of the European society of cardiology. Eur Heart J 24: 1273-1278.
- Vale MJ, Jelinek MV, Best JD, Santamaria JD (2002) Coaching patients with coronary heart disease to achieve the target cholesterol: A method to bridge the gap between evidence-based medicine and the "real world"-randomized controlled trial. J Clin Epidemiol 55: 245-252.
- Vale MJ, Jelinek MV, Best JD, Dart AM, Grigg LE, et al. (2003) Coaching patients on achieving cardiovascular health (COACH): A multicenter randomized trial in patients with coronary heart disease. Arch Intern Med 163: 2775-2783.
- Houle J, Doyon O, Vadeboncoeur N, Turbide G, Diaz A, et al. (2011) Innovative program to increase physical activity following an acute coronary syndrome: Randomized controlled trial. Patient Educ Couns 85: 237-244.
- Houle J, Doyon O, Vadeboncoeur N, Turbide G, Diaz A, et al. (2012) Effectiveness of a pedometer-based program using a socio-cognitive intervention on physical activity and quality of life in a setting of cardiac rehabilitation. Can J Cardiol 28: 27-32.
- Peixoto TC, Begot I, Bolzan DW, Machado L, Reis MS, et al. (2015) Early exercise-based rehabilitation improves health-related quality of life and functional capacity after acute myocardial infarction: A randomized controlled trial. Can J Cardiol 31: 308-313.
- Ribeiro F, Alves AJ, Teixeira M, Miranda F, Azevedo C, et al. (2012) Exercise training enhances autonomic function after acute myocardial infarction: A randomized controlled study. Rev Port Cardiol 31: 135-141.
- Giallauria F, Lucci R, D'Agostino M, Vitelli A, Maresca L, et al. (2009) Two-year multicomprehensive secondary prevention program: Favorable effects on cardiovascular functional capacity and coronary risk profile after acute myocardial infarction. J Cardiovasc Med (Hagerstown) 10: 772-780.
- Moholdt T, Bekken Vold M, Grimsmo J, Sloerdahl SA, Wisloeff U (2012) Home-based aerobic interval training improves peak oxygen uptake equal to residential cardiac rehabilitation: A randomized, controlled trial. PLoS One 7: e41199.
- Chow CK, Redfern J, Hillis GS, Thakkar J, Santo K, et al. (2015) Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: A randomized clinical trial. JAMA 314: 1255-1263.
- Reid RD, Morrin LI, Beaton LJ, Papadakis S, Kocourek J, et al. (2012) Randomized trial of an internet-based computer-tailored expert system for physical activity in patients with heart disease. Eur J Prev Cardiol 9: 1357-1364.
- Vernooij JW, Kaasjager HA, van der Graaf Y, Wierdsma J, Grandjean HM, et al. (2012) Internet based vascular risk factor management for patients with clinically manifest vascular disease: Randomised controlled trial. BMJ 344: e3750.
- Mayer-Berger W, Simic D, Mahmoodzad J, Burtscher R, Kohlmeyer M, et al. (2014) Efficacy of a long-term secondary prevention programme following inpatient cardiovascular rehabilitation on risk and health-related quality of life in a low-education cohort: A randomized controlled study. Eur J Prev Cardiol 21: 145-152.
- Nordmann A, Heilmbauer I, Walker T, Martina B, Battegay E (2001) A case-management program of medium intensity does not improve cardiovascular risk factor control in coronary artery disease patients: The heartcare I trial. Am J Med 110: 543-550.
- Moreno-Palanco MA, Ibanez-Sanz P, Pablo CC, Pizarro-Portillo A, Rodriguez-Salvanes F, et al. (2011) Impact of comprehensive and intensive treatment of risk factors concerning cardiovascular mortality in secondary prevention: MIRVAS study. Rev Esp Cardiol 64: 179-185.
- Gulliksson M, Burell G, Vessby B, Lundin L, Toss H, et al. (2011) Randomized controlled trial of cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease: Secondary prevention in uppsala primary health care project (SUPRIM). Arch Intern Med 171: 134-140.
- Andersson A, Sundel KL, Unden AL, Schenck-Gustafsson K, Eriksson I (2010) A five-year rehabilitation programme for younger women after a coronary event reduces the need for hospital care. Scand J Public Health 38: 566-573.
- Mosca L, Christian AH, Mochari-Greenberger H, Kligfield P, Smith Jr. SC (2010) A randomized clinical trial of secondary prevention among women hospitalized with coronary heart disease. J Womens Health (Larchmt) 19: 195-202.
- Murphy AW, Cupples ME, Smith SM, Byrne M, Byrne MC, et al. (2009) Effect of tailored practice and patient care plans on secondary prevention of heart disease in general practice: Cluster randomised controlled trial. BMJ 339: 1186.
- Allen JK, Blumenthal RS, Margolis S, Young DR, Miller III ER, et al. (2002) Nurse case management of hypercholesterolemia in patients with coronary heart disease: Results of a randomized clinical trial. Am Heart J 144: 678-686.
- Hu X, Zhu X, Gao L (2014) Intensive nursing care by an electronic followup system to promote secondary prevention after percutaneous coronary intervention: A randomized trial. J Cardiopulm Rehabil Prev 34: 396-405.
- Sturchio A, Di Gianni A, Campana B, Genua M, Storti M, et al. (2012) Coronary artery RIsk MAnagement programme (CARIMAP) delivered by a rehabilitation day-hospital: impact on patients with coronary artery disease. J Cardiopulm Rehabil Prev 32: 386-393.
- Jorstad HT, von Birgelen C, Alings AM, Liem A, van Dantzig J, et al. (2013) Effect of a nurse-coordinated prevention programme on cardiovascular risk after an acute coronary syndrome: Main results of the RESPONSE randomised trial. Heart 99: 1421-1430.
- Moore SM, Charvat JM, Gordon NH, Pashkow F, Ribisl P, et al. (2006) Effects of a CHANGE intervention to increase exercise maintenance following cardiac events. Ann Behav Med 31: 53-62.
- Johnson NA, Lim LL, Bowe SJ (2009) Multicenter randomized controlled trial of a home walking intervention after outpatient cardiac rehabilitation on health-related quality of life in women. Eur J Cardiovasc Prev Rehabil 16: 633-637.
- Coull AJ, Taylor VH, Elton R, Murdoch PS, Hargreaves AD (2004) A randomised controlled trial of senior lay health mentoring in older people with ischaemic heart disease: The braveheart project. Age Ageing 33: 348-354.
- Fors A, Ekman I, Taft C, Bjoerkelund C, Frid K, et al. (2015) Person-centred care after acute coronary syndrome, from hospital to primary care - A randomised controlled trial. Int J Cardiol 187: 693-699.
- Anderson L, Sharp GA, Norton RJ, Dalal H, Dean SG, et al. (2017) Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev 6: CD007130.
- Devi R, Singh SJ, Powell J, Fulton EA, Igbinedion E, et al. (2015) Internet-based interventions for the secondary prevention of coronary heart disease. Cochrane Database Syst Rev 12: CD009386.
- Anderson L, Brown JP, Clark AM, Dalal H, Rossau HK, et al. (2017) Patient education in the management of coronary heart disease. Cochrane Database Syst Rev 6: CD008895.
- Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, et al. (2016) Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J Am Coll Cardiol 67: 1-12.
- Pfaeffli Dale L, Whittaker R, Jiang Y, Stewart R, Rolleston A, et al. (2015) Text message and internet support for coronary heart disease self-management: Results from the Text4Heart randomized controlled trial. J Med Internet Res 17: e237.
- Pfaeffli Dale L, Dobson R, Whittaker R, Maddison R (2016) The effectiveness of mobile-health behaviour change interventions for cardiovascular disease self-management: A systematic review. Eur J Prev Cardiol 23: 801-817.
- Naser A, Shahamfar J, Kumar GV, Daga MK, Hadi HS, et al. (2008) Cardiac risk factor changes through an intensive multifactorial life style modification program in CHD patients: Results from a two year follow up. J Biol Sci 8: 248-257.
- Blumenthal JA, Sherwood A, Smith PJ, Watkins L, Mabe S, et al. (2016) Enhancing cardiac rehabilitation with stress management training: A randomized, clinical efficacy trial. Circulation 133: 1341-1350.
- Appels A, Bar F, van der Pol G, Erdman R, Assman M, et al. (2005) Effects of treating exhaustion in angioplasty patients on new coronary events: Results of the randomized exhaustion intervention trial (EXIT). Psychosom Med 67: 217-223.
- Carrington MJ, Chan Y, Calderone A, Scuffham PA, Esterman A, et al. (2013) A multicenter, randomized trial of a nurse-led, home-based intervention for optimal secondary cardiac prevention suggests some benefits for men but not for women: The young at heart study. Circ Cardiovasc Qual Outcomes 6: 379-389.
Citation: Momsen AMH, Hald K, Nielsen CV, Larsen ML (2018) Effectiveness of Expanded Cardiac Rehabilitation on Mortality and Lifestyle Risk Factors in Patients Diagnosed With Coronary Heart Disease-A Systematic Review. J Card Pulm Rehabil 2: 120.
Copyright: © 2018 Momsen AMH, et al. This is an open-access article distributed under the terms of the creative commons attribution license, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 3641
- [From(publication date): 0-2018 - Nov 22, 2024]
- Breakdown by view type
- HTML page views: 2928
- PDF downloads: 713