Research Article Open Access
Effectiveness of Atomized Methadone on the Buccal Mucosa in the Last Days of Life: An Innovative Delivery Route When Patients Can No Longer Swallow
Maureen Ann Allen1*, Rosemary MacDougall2, Matthew Murphy2 and Shelley Robertson21Dalhousie University, St. Martha's Regional Hospital, Chronic pain and Palliative care, Canada
2St. Martha's regional Hospital, Canada
- *Corresponding Author:
- Maureen Ann Allen
Assistant Professor Dalhousie University, St. Martha's Regional Hospital
Chronic pain and Palliative care, Antigonish, Nova Scotia B2G 2M5, Canada
Tel: 902 870-0853
E-mail: jimandmoe@eastlink.ca
Received date: January 21, 2016, Accepted date: February 15, 2016, Published date: February 19, 2016
Citation: Allen MA, MacDougall R, Murphy M, Robertson S (2016) Effectiveness of Atomized Methadone on the Buccal Mucosa in the Last Days of Life: An Innovative Delivery Route When Patients Can No Longer Swallow. J Palliat Care Med 6:250. doi:10.4172/2165-7386.1000250
Copyright: © 2016 Allen MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: Methadone is an effective long acting opioid analgesic used to manage nociceptive and neuropathic pain. Its unique lipophilic properties, absence of active metabolites and high volume of distribution allows for delivery routes that are distinct and innovative enabling patients uninterrupted and effective pain control in the last days of life. Objective: The purpose of this study was to explore the effectiveness and ease of administration of atomized methadone solution on the buccal mucosa when alternative routes including rectal and sublingual were seen as less desirable by families and health care providers in patients in the last days of life who could no longer swallow medications. Methods: The charts of thirty patients who took methadone solution at the end of life were retrospectively reviewed and data collected regarding the various transmucosal delivery routes used. Satisfaction questionnaires were completed by families and health care providers after death looking at the effectiveness of pain control and ease of administration when methadone solution was given sublingual, rectal or atomized on the buccal mucosa. Conclusion: All 30 patients remained on methadone solution until their death. Of the twenty-two patients (73%) who had methadone solution atomized buccally, one was switched to rectal administration due to bitter taste and one to sublingual due to family preference. All families surveyed reported that methadone solution was effective in controlling pain and easy to administer.
Keywords
End of life; Atomized; Methadone solution; Rural community; Pain control; Ease of administration
Introduction
Methadone is a potent long acting synthetic opioid analgesic with mu, delta and kappa receptor agonist effects. It differs from more conventional opioids by way of reuptake inhibition of serotonin and norepinephrine and through its antagonistic effect on N-methyl-Daspartate (NMDA) receptors making it an effective opioid analgesic for nociceptive and neuropathic pain [1-3].
It has a high volume of distribution and is highly lipophilic which allows for delivery routes that are unique and innovative, enabling its use in patients at the end of life when oral ingestion is no longer possible due to progression of disease or when protective airway reflexes such as coughing and swallowing are no longer present [4-7]. When taken orally, methadone reaches a peak plasma level after 2.5-3 hours with excellent oral bioavailability of 67-95%. These unique properties of methadone and the absence of active metabolites make it an attractive and inexpensive option for patients who have been unable to tolerate other conventional opioids [5,8].
There are however numerous clinical challenges with methadone use including its wide inter-individual variability in pharmacokinetics, risk of accumulation, drug-drug interactions as well as the lack of consensus regarding equianalgesic dosing.
Methadone: Routes of delivery
Numerous innovative delivery routes of methadone have been cited in the literature [4,9-12]. The most reliable and preferred route is the oral route however rectal administration of methadone is also viewed as acceptable and effective [4-6]. Other delivery routes including intravenous, intramuscular, intrathecal, subcutaneous and transmucosal (mucosal linings of the rectal, nasal and oral cavity) have all been cited as possible delivery routes each posing their own challenges and benefits [4,9,10,12].
In general, transmucosal routes of drug delivery offer distinct advantages over swallowed drugs. These advantages include bypass of hepatic first pass effect, avoidance of pre-systemic elimination within the GI tract and depending on the drug, a better enzymatic flora for drug absorption [13-15]. The nasal cavity specifically has been investigated extensively with several drugs including fentanyl and midazolam used in various clinical settings for pain and sedation [10,15,16]. Attempts at using methadone intranasal however have not been promising due to mucosal irritation of the nose with repeat dosing [10].
The mucosal oral cavity on the other hand is highly acceptable as an alternative route for drug delivery by patients and health professionals [13,14,17]. No studies or clinical trials to date have been done to explore the efficacy of atomized methadone on the buccal mucosa with respect to its tolerability and ease of administration however anecdotal evidence use suggests that the administration of atomized methadone holds great potential for end of life care in patients needing to be rotated to another delivery route when they are no longer able to swallow their medication.
Methadone’s qualities of high lipid solubility, high potency and long half-life make this delivery route attractive. A recent case series published in the Journal of Palliative Medicine by Spaner (2014) suggested that methadone administration via buccal mucosa route was reliable and effective [17].
Atomized methadone on the buccal mucosa surface as an alternative routes of drug delivery
The buccal mucosal surface offers several advantages for controlled drug delivery when drug administration is needed for extended periods of time. The mucosa is well supplied with both vascular and lymphatic drainage and first-pass metabolism in the liver and presystemic elimination in the gastrointestinal tract are avoided as previously mentioned. Gastric acidity and enzymatic action of the gastric proteases are also avoided. The buccal mucosa has a large surface area of 200 cm2 which promotes the absorption of more liposoluble drugs that are only slightly ionized by the pH of the mouth [14].
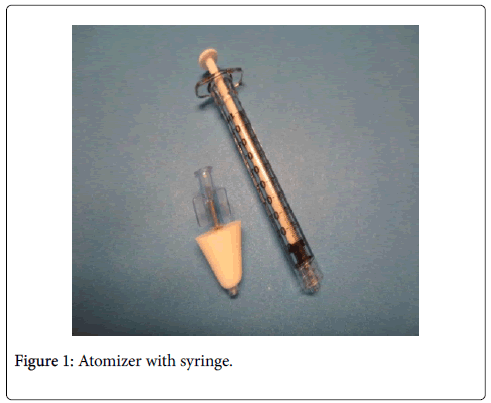
Studies looking at atomized drugs intranasal show that drug particles are rapidly absorbed into the blood stream with rates comparable to those seen with intravenous administration [10,15]. Commercially available atomized pumps which are attached to a preloaded syringe are capable of atomizing drug particles to 2-10 micrometers and can distribute these particles across a broad area of mucosa (Figure 1). These atomized pumps offer a needleless delivery system that is safe and effective which allows for controlled administration of drugs [13,15].
Factors that influence the rate of absorption on the oral mucosal surface include the volume of solution delivered, excessive salivation, extreme dryness as well as the integrity of the oral mucosa which can be altered by tumor or infection.
The ideal environment for administering drugs into the oral mucosa is a mucosal surface that is relatively dry without debris or excessive mucus [13,14]. At the time of publication, the maximum volume of atomized drug particles that can be delivered onto the buccal mucosa is unknown.
Methods
Participants
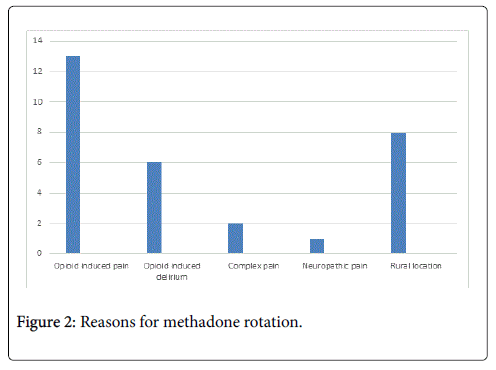
Case series data was collected retrospectively using a list of thirty patients followed by our palliative care team who were rotated to methadone due to ineffective pain control, complications from previous opioid analgesic such as opioid induced pain and delirium or rural location which limited timely access to community based nursing services and continuous analgesic pumps. Reasons for methadone rotation can be seen in Figure 2. The average age of participants was 72.3 years with a male to female ratio of 17 to 13.
Twenty-three patients (77%) had a cancer diagnosis with prostate and lung cancer the most common. Seven patients (23%) had a noncancer diagnosis which included end stage heart, lung or renal disease. Patients already on methadone prior to coming to the palliative care program as part of their previous pain management strategy were also added to the database. Data was collected between January 2013 and October 2015.
Inclusion criteria included the following:
Presence of a life–limiting illness.
Patients admitted to the palliative care program.
Methadone solution taken where methadone may have been the primary opioid, an adjuvant opioid, or a combination opioid.
Methadone was used for pain.
No patients who used methadone at the end of life were excluded from the case series data base.
Procedure
Ethics approval was obtained from the Guysborourgh-Antigonish- Strait Health Authority ethics board prior to beginning the case series. Data was collected on patients either admitted to the program on methadone or rotated to methadone during admission to the palliative care program. Demographic data collected regarding study participants and their methadone use was reviewed retrospectively.
Satisfaction questionnaires regarding effectiveness of pain control using methadone solution and ease of administration of the delivery route selected were done by telephone with families while nursing questionnaires were distributed to the various clinical settings by palliative care personnel.
The medication administration records were reviewed in each chart to collect information about opioid dose changes and break through requirements in the last 48 hours of life. Palliative care patients were seen in the hospital and community setting in a rural Nova Scotia community practice. There was no formal palliative care unit.
When patient’s protective airway reflexes diminished and they were no longer able to swallow, methadone was switched to a solution. Our usual practice was to use sublingual and rectal administration as alternative routes of methadone administration for 15 years due to cost and unavailability of parenteral methadone in a timely manner.
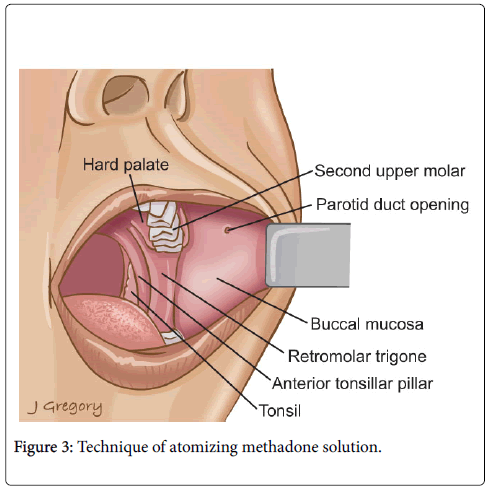
Health care providers in the community and hospitals had received on-going education regarding the unique characteristic of methadone and its use in end of life care. Methadone oral solution and a commercially available atomizer device that could be attached to a preloaded syringe was supplied to nursing staff and families to facilitate the delivery of methadone over a broad area of the buccal mucosa (Figure 3).
Staff and families were given a brief demonstration on how to deliver the methadone solution using this route. They were directed to place their index finger at the oral commissure of the patient’s lip and pull in an outward direction, atomizing the solution along the buccal mucosa of the inner cheek. Families were also shown how to deliver methadone solution using the sublingual or rectal route.
Methadone solution was offered in a 10 mg/ml or 50 mg/ml concentration with a total dosing of 0.75 mL placed in each mucosal space to a combined maximum of 1.5 mL. An equivalent dosing ratio of oral to rectal to buccal was used.
Families and nursing staff had access to the support of a palliative care team which included a nurse consultant and physician dedicated to providing palliative care support. Patients who wanted to die at home or in an alternative care setting such as a nursing home were followed by the palliative care team and offered 24 hour telephone support by a physician skilled in methadone administration.
Results
Thirty patients took methadone in the Palliative care program between January 2013 and October 2015. Our district palliative care program provides service to 45, 515 patients in 5 small communities within a catchment area of 8000 km2. Timely access to community based nursing services varies depending on the location of the community.
The most common reason for a methadone rotation was opioid induced pain. Two patients had entered the palliative care program on methadone because of complex pain prior to their cancer diagnosis as shown in Figure 2. Eight patients in rural communities who had requested death at home were rotated to methadone due to the unavailability of a continuous analgesic pump and timely access to specialized nursing care to monitor the pump. All eight patients remained at home until death.
The average dose of methadone received in all thirty patients in 24 hours was 37.5 mg. One patient continued to swallow medications until death precluding a rotation to methadone solution. Fifteen patients who requested to die at home or in their home community, whether it was a nursing home or a rural hospital were able to stay within their community with palliative care team involvement. None required transfer to the regional hospital (Table 1).
| Patient Characteristics | |
|---|---|
| Demographic variable | Value |
| Number of patients | 30 |
| Mean age | 72.3 years (range, 40-94 years) |
| Gender (m/f) | 17/13 |
| Primary diagnosis | |
| Cancer diagnosis | |
| Lung | 5 |
| Gastrointestinal | 3 |
| Genitourinary | 2 |
| Prostate | 7 |
| Breast | 1 |
| Unknown primary | 4 |
| Endometrial | 1 |
| Non-cancer diagnosis | |
| Inoperable hip fracture (Dementia and end stage heart disease) | 2 |
| Renal Failure | 3 |
| End stage heart disease | 1 |
| Stroke | 1 |
Table 1: Case series demographics in patients who had received methadone solution.
Twenty-two patients (73%) used atomized methadone solution buccally which was the preferred method of delivery. Six patients (20%) had used a sublingual delivery route. One patient was switched from atomized to rectal administration after complaining of bitterness from the solution and one family switched from atomized to sublingual due to preference. The family who preferred the sublingual route stated that the low volume of solution delivered was their reason for switching while the patient who was changed to rectal administration had used atomized methadone solution early in his clinical course during a brief period of decreased level of consciousness and found the solution unpleasant.
The use of breakthrough pain medication in the last two days of life was reviewed. The average number of breakthrough doses was 3.4. Twenty nine patients (97%) used an alternative parenteral short-acting opioid for breakthrough pain. The most common opioid used was subcutaneous hydromorphone, followed by subcutaneous fentanyl and morphine. Only one patient had used methadone solution for breakthrough pain medication due to opioid induced confusion when other conventional opioids were used.
Patients received methadone suspension for a median duration of 4 days with use ranging from 1 day to 12 days. Regular dosing of Methadone solution was three times a day. No patient required an increase to four times daily. All patients remained under the 1.5 mL of delivered suspension. All thirty patients remained on methadone throughout the course of their illness. Three patients required an increase of methadone in the last 48 hours of life after needing more than 5 doses of breakthrough pain medication. All required less than 3 doses of breakthrough pain medication at the time of their death.
Thirty satisfaction questionnaires were sent to nursing staff within the district. Twenty-five (83%) were returned and completed with three nurses indicating they had not administered methadone solution. Of the twenty-two nurses (73%) who had dispensed methadone solution thirteen (60%) had used more than one delivery route. Of the ten families contacted by phone, eight were reached successfully. Two of the families (25%) surveyed had used more than one delivery route. A summary of the results from the satisfaction questionnaire can be found in Table 2.
| Hospital | |
| Regional Hospital (89 beds) | 15 |
| Rural Hospital (<15 beds) | 4 |
| Family Home | |
| Town 4000-5000 population | 1 |
| Rural <3000 population | 8 |
| Nursing Home | |
| Town | 1 |
| Rural | 1 |
Table 2: Location in the district health authority where death occurred.
Families and nursing staff that cared for patients in these settings felt the patient’s pain was well controlled and that methadone solution delivered by the atomized route was convenient and minimally intrusive.
Discussion
The results of this case series suggests that when patients are switched from oral methadone to a transmucosal delivery route, they continue to receive safe, effective pain control. This did not increase the care burden on health professional and families who cared for them regardless of whether the place of death was at home or hospital setting. Transmucosal delivery route’s provided families with an effective long acting opioid when a continuous analgesic pain pump or 24 hour nursing care was limited. Methadone solution atomized on the buccal mucosa was the preferred delivery route in the community (75%) whereas both sublingual (72%) and atomized methadone on the buccal mucosa (68%) were utilized equally in the hospital setting. Although interpretation of this difference is limited due to the low numbers of participants, it is possible this trend may be a reflection of our district’s comfort with delivering methadone solution either sublingually or rectally previously which was our approach prior to the introduction of the atomizer whereas families had not been exposed to sublingual or rectal administration beforehand. Health professionals and families however reported all routes were effective in controlling pain and effortless to administer. Of the eight families who chose the atomized delivery route in the rural community, all felt that this route was both effective in controlling pain and easy to administer. None of the patients who were switched from an oral route of methadone to a transmucosal route were transferred to hospital when they wanted to die at home. Families and community based nurses caring for patients expressed gratitude at having access to an effective long acting opioid that was easy to administer without the use of a continuous analgesic pumps or frequent dosing of a parenteral opioid to keep loved ones comfortable.
None of the patients who received sublingual or atomized methadone required more than a total of 1.5 ml per dose. The maximum concentration of methadone used was a 50 mg/ml concentration. The decision to split the dosing and deliver only 0.75 ml on each cheek was based on a clinical judgment and not guided by evidence. Nursing staff found that there was less pooling with this technique.
One could have also considered a split dosing of four times a day lowering the total volume needing to be delivered at any time or switch the patient to a rectal route of administration. Families found atomizing methadone solution less intimidating than dripping a solution of methadone into the sublingual space in a patient who could no longer swallow as evidenced by the fact most families chose the atomized route. There is no evidence to objectively determine what the aspiration risk is when solution is delivered by an atomized or dripped route into the oral mucosa in a patient with blunted airway reflexes.
Limitations with this case series and questionnaire interpretation included the low numbers of participants enrolled, the inability of patients to report their pain experience due to decrease level of consciousness and maintaining consistency in the delivery of methadone solution when a broad group of health professionals and families were involved in providing care.
Although family members who provided care remained unchanged, nursing staff turnover in the various health care settings was challenging warranting on-going education, instruction and support from health professionals skilled in delivering methadone to ensure methadone solution was not inadvertently stopped in a patient who could no longer swallow medication which was the typical practice of our nursing colleagues.
We addressed this by standardizing our written instructions to include alternative delivery routes for methadone. For example, Methadone solution (10 mg/ml) 5 mg (0.5 ml) three times a day oral, rectal, sublingual or atomized buccally. As well if patients unexpectedly lost the ability to swallow but were still on a tablet form of methadone, families and nurses were instructed to use the methadone tablets at the same dose rectally or sublingual until methadone solution could be obtained ensuring the continued delivery of methadone [18].
Another challenge was the interpretation and distribution of the satisfaction questionnaire (Table 3). Questionnaires were delivered to nursing units within the health care district and collected at a later date whereas families were contacted by phone which may have influenced their viewpoint. All family members surveyed however indicated that they were satisfied with the use of methadone solution regardless of how it was delivered and were grateful to keep their loved one at home.
| Nursing: 30 questionnaires sent Families: 10 contacts made 25 completed (83%) 8 interviewed (80%) 22 had used methadone solution (73%) | |||
|---|---|---|---|
| Delivery route used to administer methadone solution | |||
| Atomized buccally | Sublingual | Rectal | |
| Nurses | (15/22) 68% | (16/22) 72% | (5/22) 22% |
| Families | (6/8) 75% | (1/8) 12% | (1/8) 12% |
| Satisfaction with ease of administration (Satisfied or very satisfied) No families or nurses expressed dissatisfaction | |||
| Atomized buccally | Sublingual | Rectal | |
| Nurses | (14/15) 93% | (14/16) 87% | (3/5) 60% |
| Families | (6/6) 100% | (1/1) 100% | (1/1) 100% |
| Satisfaction with pain control (Satisfied or very satisfied) No families or nurses expressed dissatisfaction | |||
| Atomized buccally | Sublingual | Rectal | |
| Nurses | (11/15) 73% | (13/16) 81% | (2/5) 40% |
| Families | (6/6) 100% | (1/1) 100% | (1/1) 100% |
Table 3: Results of satisfaction questionnaire’s.
The use of atomized methadone on the buccal mucosa at the end of life offers great promise as an alternative delivery route to oral, sublingual, subcutaneous and rectal administration when a patient can no longer swallow at the end of life. It is both tolerable and acceptable and can offer an alternative delivery route to sublingual or rectal administration. Methadone’s potent long acting quality can help ease the care burden for families wanting to keep their loved ones at home who may not have access to a continuous analgesic pain pump or around-the-clock community based nursing. The ease of atomized oral mucosal administration and its cost-effectiveness make it a promising addition to end of life use of methadone.
References
- Haroutiunian S, McNicol ED, Lipman AG (2012) Methadone for chronic non-cancer pain. Cochrane data base of systemic reviews 11.
- Morley JS, Miles JB, Bridson J, Nash TP, White S, et al. (2003) Low-dose methadone has an analgesic effect in neuropathic pain: a double-blind randomized controlled crossover trial. Palliative Medicine 17: 576-587.
- Lynch ME (2005) A review of the use of methadone for the treatment of chronic Noncancer pain. Pain Res Manag autumn 10: 133-144.
- Neron A (2009) Care Beyond Cure: Management of Pain and Other Symptoms. Can J Hosp Pharm 62: 178.
- Taube AW (2003) Methadone: What is its Role in Cancer Pain Control? The Canadian Journal of CME 15: 90-99.
- Davis MP, Walsh D (2001) Methadone for relief of cancer pain. A review of pharmacokinetics, pharmacodynamics, drug interactions and protocols of administration. Support care cancer 9: 73-83.
- Nicholson AB (2013) Methadone for Cancer pain. Cochrane database of systemic Reviews 6.
- Dickerson ED (2001) Methadone: The question or the answer for US opioid therapy and pharmaco-economics? Support Care Cancer 9: 646-648.
- Kestenbaum MG, Vilches AO, Messersmith MS, Connor SR, Fine PG, et al. (2014) Alternative Routes to oral opioid administration in Palliative Care: A Review and Clinical Summary. Pain Medicine 15: 1129-1153.
- Dale O, Hoffer C, Sheffels P (2014) Disposition of nasal, intravenous, and oral methadone in healthy volunteers. Clinical Pharmacology & Therapeutics pp: 536-544.
- Centeno C, Vara F (2005) Intermittent subcutaneous methadone administration in the management of cancer pain. J Pain palliate Care Pharmacotherapy 19: 7-12.
- Rao S, Song Y, Peddle F, Evans AM (2011) Particle size reduction to the nanometer range; a promising approach to improve buccal absorption of poorly water-soluble drugs. Int J nanomedicine 6: 1245-1251.
- Admir HS (1998) Buccal Mucosa as a route for systemic drug delivery: A review. Faculty of Pharmacy and Pharmaceutical Sciences. University of Alberta, Edmonton. J Pharm Pharmaceutics Sci 1: 15-30.
- Sliva S, Barton E (2014) Intranasal use of drugs in the Emergency room and pre-hospital arenas.
- Grassin-Delyle S, Buenestado A, Naline E, Faisy C, Blouquit-Laye S (2012) Intranasal Drug Delivery: an efficient and non-invasive rout for systematic administration: focus on opioids. Phamacol Ther 134: 366-379.
- Squier CA (1991) The permeability of oral mucosa. Critical reviews in oral biology and Medicine 2: 13-32.
- Spaner D (2014) Effectiveness of the Buccal Mucosa Route for Methadone Administration at the End of Life. Journal of palliative Medicine 17: 1262-1265.
- Product Monograph (2014) Metadol. Paladin Lab Inc. Saint-Laurent Quebec.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 12422
- [From(publication date):
March-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 11517
- PDF downloads : 905