Effect of TDCS in Children with Autism
Received: 25-Apr-2023 / Manuscript No. CNOA-23-96990 / Editor assigned: 28-Apr-2023 / PreQC No. CNOA-23-96990 (PQ) / Reviewed: 15-May-2023 / QC No. CNOA-23-96990 / Revised: 26-Jun-2023 / Manuscript No. CNOA-23-96990 (R) / Published Date: 04-Jul-2023 DOI: 10.4172/CNOA.1000195
Abstract
Introduction: The three basic signs of Autism Spectrum Disorder (ASD) include limited or repetitive interests and activities, poor language and communication, and trouble interacting with others. People with autism have a broken cerebellum prefrontal brain connection. The functional and anatomical specialization of cortical areas important in motor control, language, and social interaction is hampered by the disruption of specific cerebral-cerebellar networks. Seizures, somatosensory irregularities, sleep issues, and gastrointestinal symptoms are just a few of the ailments that autism is often linked to.
Objectives: The goal of this study is to determine the effects of tDCS therapy on children with autism.
Methodology: A tiny hand held device is used to provide a very low electrical current to certain brain areas during tDCS, a non-invasive brain stimulation treatment. Specific areas of the brain are covered by two sponges that are positioned on the skull, and electricity is sent through them via electrodes. The electrodes are linked to a portable device that produces a steady weak current of 0.5 mA-2 mA, about equivalent to the output of a 9 volt battery.
Assessment method: Evaluation of the Childhood Autism Rating Scale (CARS), Autism Treatment Evaluation Checklist (ATEC), and Children's Global Assessment Scale (CGAS) before and after therapy. Children with autism should undergo tDCS therapy for an average of 5 days per week. To investigate the effects of tDCS, an average of 7 sessions will be conducted.
Scope of research and implications: One of the most promising treatment options for a variety of medical and neurodevelopmental disorders, tDCS is affordable, simple to use, and has a very good safety profile.
The therapeutic effects of tDCS in the brain may go much beyond its ability to modulate synaptic activity since all of the cells and tissues in the brain and nervous system are susceptible to electric fields. It is anticipated that tDCS will have an impact on brain glial cells, endothelium and other cells that form brain blood vessels since it has been shown to modify both brain inflammation and brain blood perfusion.
Keywords
Autism spectrum disorder; Neurodevelopmental disorders; Brain; Endothelium; Electric fields
Introduction
Autism is a neurodevelopmental disorder also known as autism spectrum disorder which appears at the early developmental stage of children which limits them in everyday functioning. It can be detected at 12 to 18 months or even earlier, but usually the diagnosis takes place when children reach 3 to 7 years old [1]. Social impairment, stereotyped behaviors and repeated interest characterize ASD [2]. The informative core of this disorder is lack of communication, non contactness, non-communicability, especially when they are exposed to public or any social places, they misbehave if they have trouble communicating [3]. Autism is frequently linked to a number of additional abnormalities, such as seizures, somatosensory abnormalities, sleep problems, and gastrointestinal complaints, in addition to communication difficulties [4]. As a result, children with ASD have drastically diminished quality of life and overall functioning, which has a negative emotional impact on both the individuals with the diagnosis and their families. Even though genetics and environmental variables play a crucial role in the development of ASD, its etiology and pathophysiology are yet unknown. One hypothesis holds that some children are more genetically prone to specific environmental pollutants that can cause autism, while another holds that the higher the amounts of testosterone in the womb, the more likely the baby will develop into an ASD individual [5].
Numerous topics have been studied in research, including genetics, fetal injuries, brain function, neurochemicals, and immunological aspects. A quarter of ASD cases are linked to genetic diseases such as congenital rubella or the genetic condition fragments of X syndrome [6]. ASD may be caused by abnormal central nervous system functioning because most patients exhibit signs of normal brain function. In morphometric brain imaging investigations, it was discovered that ASD patients had hemispheric asymmetry and had more volume in various right hemispheric structures than in homologous contralateral structures, particularly in areas associated to language and social skills. Additionally, compared to neurotypical children, children with ASD showed hypoactivation in the left hemisphere's amygdala and fusiform gyrus, while a protonic magnetic resonance spectroscopy study discovered a reduced chemical ratio in the left but not the right dorsolateral prefrontal cortex in patients with ASD. This chemical ratio is N-acetyl aspartate/creatin/ phosphocreatine [7,8].
The primary symptoms of social impairment and communication have not yet been successfully treated with medication. TDCS is a non-invasive, secure, and affordable neuromodulation method that affects cortical excitability using anode and cathode electrodes positioned on the surface of the scalp to deliver low intensity electrical stimulation (0.5 mA-2.0 mA). It has been used to help people with ASD feel better. There is proof that delivering tDCS to certain brain areas, such as the frontal cortex, especially the Dorsolateral Prefrontal Cortex (DLPFC), dramatically modifies perceptions of learning, memory, alertness, brain activity/dynamics, and neurotransmitter levels. Evidence shown that tDCS applying to certain brain regions such as frontal cortex, especially targeted brain region is Dorsolateral Prefrontal Cortex (DLPFC), significantly modulates recognition on learning, memory, vigilance, brain activity/dynamics and neurotransmitters levels. tDCS subthreshold changes in resting membrane potential of targeted neurons. The positively charged current increases cortical excitability from anode and negatively charged decrease the excitability [9,10].
Multiple sessions of tDCS can result in a higher and better improvement than a single session, which may be gradual and frequently have a minor inconsistent effect. Numerous studies have examined the impact of transcranial Direct Current Stimulation (tDCS) on the DLPFC on autistic symptoms, Electroencephalogram (EEG) resting state connectivity, executive functioning, working memory, and syntax acquisition. These investigations have made tDCS a promising treatment option for people with ASD.
Definition and pathophysiology of autism
Asperger's syndrome a neurodevelopmental condition caused by differences in the brain that has a prevalence of 1 in 68 children in the United States of America (US CDC data from 2014). Its core component is social functioning deficits, i.e., how they think and behave, along with how they communicate and interact, which represents a quality of life concern not only for an individual with autism but also for their families as well as loved ones! [11-13].
Autism and autism spectrum disorder are the same, but ASD is a term that is used to diagnose autism. Some autistic people prefer not to use the word disorder because of its negative meaning. Hence, they prefer autism over autism spectrum disorder. But ASD is a rather preferred term in the medical field [14].
ASD was introduced in the subgroup of PDD, i.e., pervasive developmental disorders, which in turn are a group of disorders that were launched in the Diagnostic and Statistical Manual of mental disorders, edition III (DSM-III) in the year 1980 to convey the idea of a border spectrum of social communication deficits.
Because of ambiguity between the PDDs and the difficulty in differentiating between them, the latest diagnostic systems were launched! Which are ICD-11, i.e., international classification of diseases, 11th revision, as well as DSM-5, i.e., diagnostic and statistical manual of mental disorders, edition 5.
The DSM-5 and ICD-11 norms for ASD comprise five symptom bundles stated as follows.
Social communication as well as social interaction. They must have proof in many contexts of all of the following stated domains, either present or by past: Non-verbal communication, social reciprocity developing, maintaining, and understanding relationships is key. Constricted, recurrent behaviors and interests must have 2 of 4 of the below domains, either currently or by history: Demand on similarity stereotypes, repetitive behaviors oversensitivity or under sensitivity, or interest in sensory inputs moored, highly restricted interest signs be required to be present in initial development but may not be completely manifested there upon or maybe masked later in life by learned strategies. Signs should cause medically significant impairment in the present run. Neither intellectual disability nor global developmental delay provides a better explanation [15].
The pathophysiology of ASD is unknown as of now, but it turns out there has been several factors that are indicated in the pathogenesis of ASD. Among the indicated ones, the most prominent one is the genetic, which has been indicated to have a strong evidence based etiology in cases of a few concurrence or related conditions such as fragile X syndrome, tuberous sclerosis, etc. Along with that, brothers or sisters of autistic offspring have a greater occurrence of autism than those of the normal population. The findings of numerous genes, and interactions of multiple genes in one individual, epigenetic factors, as well as effects of environmental modifiers on these genes in ASD, suggesting that genetic causes, which includes diagnosable medical conditions, single gene defects, and cytogenetic problems, comprise 25% of the ASD patients till now! henceforth, the amount of clinical phenotypes and linked comorbidities has turned into the characteristic feature of ASD. Few studies have also shown the role of mitochondrial DNA mutations in ASD, which might lead to disability of the energy metabolism in mitochondria.
Individuals with ASD can have countless biomedical factors which can affect brain functioning as follows.
Nutritional deficiencies like (omega-3 fatty acids), zinc, magnesium, vitamin A and D, B vitamins.
Opiate like byproducts from gluten and casein, poor detoxification, poor methylation, food sensitivities or intolerances inflammation of the intestine or brain and excessive pro-inflammatory cytokines insufficient cytotoxin oxidative stress mitochondria/metabolic dysfunction immune imbalance, etc. [16].
Brain imaging of a normal person shows the volume of the right brain, which is the center for social function and language, is higher in the right hemisphere than in the left. In patients with ASD, under activation in the left hemisphere compared to that of the right hemisphere has been noticed. As well as, brain connectivity, abnormal synaptic maturation, and mirror neuron dysfunction have been proposed as neurophysiological elements which might be the key signs correlated with ASD.
A report by the CDC estimates that 46% of individuals with ASD have standard intelligence. They have psychiatric comorbidities of mood disorders such as depression, anxiety, hyperactivity disorder, OCD, chronic tic disorders, and substance related disorders. Grownups with ASD show a low level of acquirement for meaningful relationship partners along with a high level of underemployment even though they have high intelligence and education.
Materials and Methods
Diagnostic tools of autism
ASD is usually diagnosed in early childhood. However, because symptoms and severity differ greatly, ASD can sometimes be difficult to diagnose. Some individuals aren’t diagnosed until adulthood. A team of psychologists or neuropsychologists, a developmental pediatrician, a neurologist, and/or a psychiatrist look at the child’s developmental history and behaviour to make an official diagnosis. There are several steps in this process.
Developmental monitoring
Developmental monitoring is a proactive, continuing practise that involves observing a child's development and promoting discussions between parents and other adults about the child's skills and potential. Participation in developmental monitoring is permitted from every member of the family. To see whether the kid is growing and achieving age milestones, the doctor asks developmental questions like.
Did the baby still smile at six months? Did your child replicate facial expressions and sounds by the age of nine months? Do they respond when someone tries to catch their eye? Are they speaking in a "flat" tone? Do they interact with others and exchange stories? Were they babbling and cooing at 12 months? Do they readily become angry or offended? Are there any chances that any of their behaviours are peculiar or monotonous? Do they have difficulty making eye contact? Are they aware of what others are doing? Are they impacted by temperature, sound, or light? Do you have any digestive or sleep problems?
You will be sent to a specialist for further testing if your kid displays developmental difficulties or the doctor has concerns.
Any family members who have had mental health problems, such as Attention Deficit/Hyperactivity Disorder (ADHD), learning difficulties, intellectual impairment, or Autism Spectrum Disorder (ASD), must be disclosed to the doctor (ADHD).
Developmental screening
A more thorough examination of a child's development is provided via developmental screening.
Compared to developmental monitoring, the screening procedure is more formal. It is a typical component of many well child checks, even when there is no known issue. All children should undergo developmental and behavioural testing at 9, 18, and 30 months of age, respectively, according to the American Academy of Pediatrics (AAP). Additionally, between the ages of 18 and 24 months, the AAP advises that all children be evaluated for ASD during routine well child visits. A child's mobility, language, mental capacity, behaviours, and emotions may be compared to those of other children who are developing properly in screening questionnaires [17].
Developmental diagnosis
The Modified Checklist for Autism in Toddlers (M-CHAT), the Autism Behaviour Checklist (ABC), and the autism spectrum screening questionnaire are a few examples of screening tools that experts may use. Screening instruments determine if a kid is progressing along the proper developmental path. A thorough developmental assessment may be necessary if the screening tool reveals a problem area. This assessment is carried out by a professional who closely observes the child, conducts a series of tests on the child, conducts questionnaires with the parents or caregivers, and interviews the child. The outcomes of this formal assessment emphasize a child's assets and liabilities and may determine whether they satisfy the requirements for a developmental diagnosis. The expert may sometimes recommend genetic counselling and test the youngster [18,19].
Formal assessment tools
The majority of experts agree that formal evaluation methods are preferable since they are more systematic and repeatable when it comes to fulfilling the necessary diagnostic criteria. Among these are the Autism Diagnostics Interview-Revised (ADI-R), the Gilliam Autism Rating Scale (GARS), the Childhood Autism Rating Scale (CARS), and the Autism Diagnostic Observation Schedule (ADOS). A diagnostic instrument for autism spectrum disorder, the INCLEN Diagnostic Tool for Autism Spectrum Disorder (INDT-ASD), has been standardised and validated using the cars. Interviews with the caregivers and contact with the youngster are encouraged. This tool also indicates if the information being delivered conflicts with the child's opinions. It is a quick analysis. It can identify youngsters who have severe autism [20].
Management of autism-pharmacologic interventions and non-pharmacologic interventions
Pharmacology approaches to ASD management: ASD cannot presently be treated with medicine. The only way that currently available drugs work is in combination with behavioural therapy. When behavioural treatments do not work to address maladaptive behaviour or comorbidities such sleep difficulties, anxiety disorders, or ADHD, pharmaceutical therapy is employed. Only aripiprazole and risperidone have been scientifically shown to effectively treat irritability in ASD kids.
Non-pharmacological approaches to ASD management: The most popular form of treatment for those with ASD is speech and language therapy. It enhances a person's comprehension and verbal and written communication skills. While some ASD sufferers utilize verbal communication, others use signs, gestures, pictures, or technological tools.
A person may live as independently as possible with the support of occupational therapy, which teaches activities like dressing, eating, and bathing.
Included in occupational therapy are the following:
• Physical therapy aids in enhancing physical capabilities like mobility.
• Improved responsiveness to sensory input that may be constricting or overpowering is the goal of sensory integration treatment.
Approaches to education: In a classroom context, educational therapies are offered, and a teacher looks into ways to change the classroom environment and enhance academic and other results. Oral instructions may be supplemented by visual cues.
Social-relational approaches: Social skill development and emotional bonding are key components of social relational therapies. In order to improve communication chances, parents and therapists might follow the patient's interests by using the developmental, individual differences, and relationship based models.
"Social tales" provide a succinct description of what to anticipate in a social context.
The relationship development intervention model comprises exercises that boost one's enthusiasm, drive, and capacity to engage in social interactions with others.
People with ASD may practise social skills in a structured setting by participating in social skills groups.
Mechanism of tDCS in autism
Recently, transcranial Direct Current Stimulation (tDCS) has become one of the therapeutic modalities with the greatest potential for reducing the symptoms of autism. The most current study was published in July of this year and was prepared by a group of French researchers and clinicians. This study confirmed and expanded on previous research's findings that tDCS may significantly increase some people's quality of life and autonomy of autistic people by improving cognition, behavior, and physical health. Following this study, a different article detailed how tDCS treatment significantly improved the motor skills of a small group of autistic children.
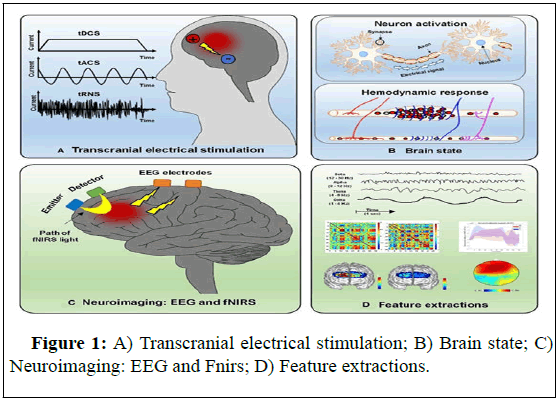
To modify neuronal excitability and change connections, the transcranial Direct Current Stimulation (tDCS) approach injects a small electrical stimulation into the brain. It enables the facilitation and stabilization of the corresponding training effects when combined with particular cognitive activities. Consequently, a promising treatment strategy for ASD involves using tDCS in social cognition relevant brain regions in conjunction with specialized cognitive training (Figure 1).
Possible mechanisms of action of tDCS for ASD treatment
We give an overview of the potential mechanisms of action by which tDCS is effective in the treatment of ASD. But further modes of action need to be found, as the precise pathophysiology of this complicated condition is still unknown. Neuronal polarity and neural circuitry appear to be involved in the overall effects of tDCS.
While cathodic stimulation decreases neural excitability, anodic stimulation boosts it. At least when considered in light of the tDCS's immediate side effects, this polarization shift most likely results from the displacement of resting potential. Modifications in synapse function are assumed to be the cause of the long term effects of tDCS, specifically through modifications in the activity of N-methyl-Daspartate and aminobutyric acid receptors, resulting in long lasting changes in regions with lower activity. Through the use of neurotrophic substances derived from the brain, tDCS may also modify neuroplasticity. The early etiology of autism is greatly influenced by the hyperactivity of just this one trophic factor. The overall effect of tDCS appears to affect other areas and is not limited to particular sites of treatment.
To encourage and improve brain plasticity, a small hand held device delivers a very modest electrical current to specific brain regions during tDCS, a non-invasive neurostimulation procedure. Two sponges are positioned on the skull over particular brain regions, and electrodes are used to deliver the current through them. The electrodes placed are connected to a portable appliance that produces a weak current that is constant and ranges between 0.5 mA-2 mA, matching the power of a 9 volt battery. Therefore, the impact of tDCS is limited; a small bit of the current that reaches the scalp gently "nudges" and modifies neuron-axonal excitability.
One of the highly promising treatments for a range of neurological and medical conditions, tDCS is affordable, simple to use, and has a very good safety profile.
tDCS's mechanisms of action relevant to autism
Brain function modulation-tDCS in the enhancement of neuronal plasticity: The ability of the brain to change continually during a person's life is referred to as neuroplasticity, also known as brain plasticity. A healthy brain remodels itself to respond to shifting environmental demands by altering itself structurally, functionally, and through "neuronal wiring" (the means by which neurons exchange information). In order for the brain to recover from an insult or injury and be able to adjust to the environment's changing demands and challenges, such changes must take place continuously.
For healthy brain function, cognition, and behavior, brain plasticity is crucial. Autism and other neuropsychiatric disorders are significantly influenced by pathological alterations in the brain's neuroplasticity, or, to put it another way, the brain's inability to adapt to changing demands.
The capacity of both healthy and neurologically impaired people has been found to improve with tDCS in a variety of cognitive and executive function areas. By stimulating brain regions involved in working memory and attention, scientists and medical professionals have produced significant improvements in cognitive function, processing speed, arithmetic processing, behavior control, multitasking, focus shifting, and many other areas.
The fundamental action of tDCS is typically thought to entail altering neurons' electrical charge or resting membrane potential (neurons are essentially "electrical devices").
How much calcium and other signaling chemicals are transported into and out of neurons depend on their membrane potential. This in turn affects gene expression, neuronal energy consumption, connection and communication between neurons, as well as the creation and release of other signaling molecules, including endocannabinoids, GABA, serotonin, dopamine, and others.
The therapeutic benefits of tDCS in the brain may go much beyond its regulation of synaptic activity since cells and tissues in many areas of the brain and nervous system are receptive to electric fields. It is assumed that tDCS would affect brain glial cells in addition to endothelial and other cells that construct brain blood vessels since it has been proven to impact both brain inflammation and brain blood perfusion.
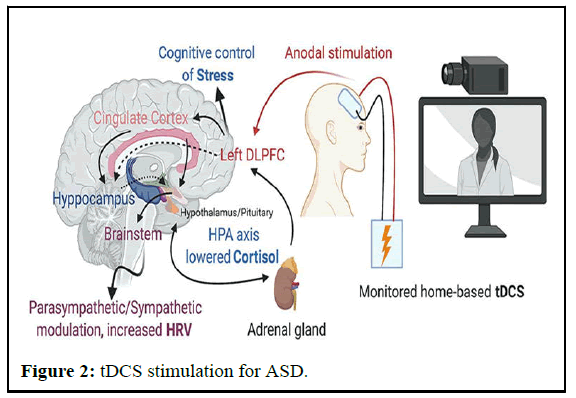
In summary, several disease mechanisms and pathological cascades in the nervous system can be affected by tDCS (Figure 2).
tDCS modulation of auditory processing and languagerelated brain areas
An increasing corpus of research demonstrates that tDCS can modulate linguistic ability in both healthy people and patients who experience aphasia, or language loss. Single tDCS sessions have been demonstrated to have significant impacts on healthy adults across all linguistic tests, sometimes even after only one session. In certain situations, the reported advancements in non-verbal patients were astounding.
There is speculation that tDCS induced changes in excitability and neuroplasticity in the areas of the brain that process language, greater connectivity between other brain regions, and general gains in cognition or working memory are what cause changes in language comprehension and speech.
Auditory sensory processing is likely a second mechanism underlying tDCS related gains in communication and language. It has been demonstrated that the capacity to selectively focus on a target speaker of attention in a difficult aural environment is impacted by tDCS.
Since autism is known to have poor "speech discrimination" and problems encoding speech at the brainstem, the potential of tDCS therapy to improve background noise filtering may be especially significant for people with autism.
tDCS for autism subclinical seizures and epilepsy
Compared to the general population, people with autism have a much greater prevalence of seizure disorders, and epilepsy is the main cause of premature mortality in this community. Most autistic people have been discovered to exhibit subclinical epileptiform activity, even in the absence of a clinical seizure disorder.
Autism and epilepsy probably have similar pathophysiologies. Autism alone is less likely to cause serious social difficulties and lifelong dependency than autism combined with epilepsy. Autism typically manifests in epilepsy related diseases such Dravet syndrome, Landau-Kleffner syndrome, and tuberous sclerosis complex.
Increasing amounts of data are gathering together to suggest the possibility of using tDCS and other forms of neurostimulation to treat drug resistant, or refractory, epilepsy.
Experimental animal research demonstrates that tDCS can lessen the frequency and severity of seizures, and preliminary human trials suggest that it may be helpful for at least a subgroup of patients.
The Russian academy of medical sciences carried out one of the earliest investigations into people, which was then published in 2001. 18 minors with drug-resistant epilepsy, including 13 with cerebral palsy and 5 with organic CNS abnormalities, received transcranial micro polarization, a type of tDCS. The frequency and severity of seizures significantly and permanently decreased in all children, and improvements in EEG parameters were also evident.
The Khon Kaen university team in Thailand was among the first to look at the effectiveness of cathodal tDCS for treating pediatric seizures. They discovered that a single 20 minutes therapy significantly reduced epileptiform discharges up to two days after it. The 36 subjects all responded favorably to the therapy.
The same researchers also investigated how 22 individuals with Lennox-Gastaut syndrome, a severe refractory epileptic disease, responded to tDCS. The primary motor cortex was subjected to cathodal tDCS for five days in a row, and the results were sustained at the 3 weeks follow-up inquiry in terms of seizure frequency and epileptic discharges. The data demonstrate an increase in (cortical activity) around the stimulation site, which offers circumstantial support for a potential mode of action of tDCS on a parameter previously connected to autistic severity in individuals with ASD.
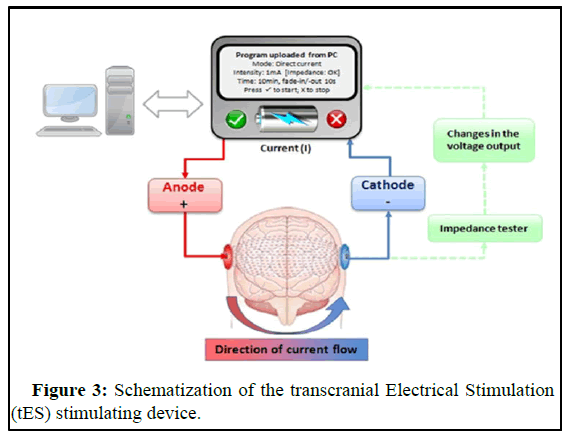
The technique involves the delivery of a low level intensity (1 mA-2 mA) current by a battery driven stimulator between two electrodes (anode and cathode) that are placed on the scalp. The electrodes are typically large, conductive rubber sheets inserted in saline soaked sponges (20 cm2-35 cm2). The current passes through the scalp and crosses the extracortical layers to reach the cortex, which modulates the membrane polarity of the neurons with a region of underlying neural tissue. In the case of direct current delivery the current flow direction is from the anode to cathode. This current induces changes in the electrical activity of the neurons and it consequently modifies the neurons synaptic efficiencies. This modification is insufficient to induce action potentials; however, it is adequate to introduce variation in the response threshold of the stimulated neurons. To maintain a constant current the impedance is regularly verified by an impedance tester to establish whether it is necessary to vary the voltage delivered from the stimulator (Figure 3).
Modulation of physiological response to stress by tDCS
Autism sufferers react to stress exaggeratedly. They frequently overreact when a threat is deemed to exist and struggle to cope with uncertainty. Compared to the general population of healthy people, the sympathetic "fight or flight" stress response lasts longer in autism.
Many of the other problems that people with autism frequently experience, such as anxiety, avoidance of unfamiliar situations, rigid and/or challenging behaviours, including irritability and violence, are made worse by this excessive reactivity to stressful stimuli, which corresponds with deficiencies in adaptive functioning.
Due to their heightened stress response and altered regulation of the HPA axis in reaction to stress, individuals with autism may be prone to a number of mental and physical health issues. Autism has a dramatically higher incidence of several medical conditions, including anxiety, severe depressive disorder, and suicide.
The physiological reaction to stress has been seen to be modulated by tDCS. Data from numerous researches demonstrates that tDCS treatments can successfully lower cortisol and heart rate, which could be hazardous in both healthy people and those with anxiety disorders.
In addition to minimizing the detrimental effects of stress on physical health, one study found that tDCS also decreases stress induced working memory deficits, suggesting a "potential novel route to avoid stress induced cognitive deficits." Additionally, under experimental conditions, tDCS greatly lowers pathological fear and modifies the memory of fear, suggesting that it may be an effective therapy option for anxiety, post-traumatic stress disorder, and other emotional regulation problems.
Hyperalgesia, or heightened pain sensitivity, is linked to chronic stress. Because of alterations in neurological pain pathways brought on by stress, those with heightened or extended stress responses frequently have lower pain thresholds. Recent data indicates that pain sensitization caused by stress may be controlled by tDCS treatment.
Effects of tDCS on sensory dysfunction and pain processing
Autism sufferers frequently have aberrant pain sensitivity and sensory impairment. Compared to the general population, autism affects both children and adults at higher rates of both acute and chronic pain. The faulty interpretation of pain stimuli by the brain and nervous system is assumed to be at least partly responsible for the mechanisms underlying greater pain sensitivity in autism.
In addition to localized inflammation, maladaptive alterations in brain excitability in the central nervous system are hypothesised to be signaled by chronic pain. Most studies done to date have shown that tDCS may lessen pain brought on by improper peripheral and central nervous system pain signal processing. Regardless of inflammation or disease activity, tDCS has been shown to be effective in reducing chronic stomach pain in people with inflammatory bowel disease in studies on chronic back pain and fibromyalgia. Changes in the levels of brain neurochemicals linked to pain processing, such as glutamate, dopamine, serotonin, and endogenous opioids, have been hypothesised as one of the processes behind the pain relieving effects of tDCS. This is because most earlier experiments stimulated the primary motor cortex region of the brain with anodal currents.
Additionally, tDCS can lessen levels of TNF and other proinflammatory chemicals in the brain, as well as some of the negative consequences of chronic stress on pain sensitivity.
There has long been speculation that tDCS and other neuromodulation techniques have effects that go well beyond those of the neurological system and the brain. Numerous research conducted on animals and in living organisms has demonstrated that tDCS affects immunological and inflammatory responses in the central and peripheral nervous systems, including the gut enteric nervous system.
There have not yet been any clinical trials that translate these findings. Active tDCS lowers levels of proinflammatory cytokines IL-6, IL-10, and TNF-a in individuals with severe arthritis when compared to placebo sham treatment. These results imply that, in addition to lowering pain sensitivity, active tDCS therapy may have additional therapeutic advantages in patients with pro-inflammatory diseases.
Inflammation and distorted immune responses are linked to autism as well as the majority of neurological and psychiatric problems, in addition to traditional neuroinflammatory diseases like multiple sclerosis.
Therefore, tDCS may represent a promising therapeutic approach for such illnesses due to its potential impact on the inflammatory response.
There is a need for more research on the ideal sites for electrode attachment, as well as on the frequency, intensity, and duration of tDCS stimulation.
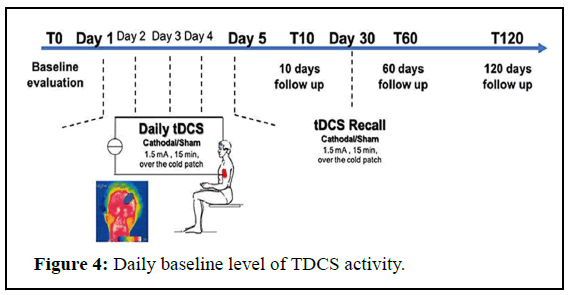
The baseline level of neuronal activity in each person, variations in the skull, and even hair density, which affects how much current can pass through the skull, are additional aspects to take into account that may have an impact on the results of tDCS application (Figure 4).
Effect of tDCS on Autism Spectrum Disorder (ASD)
A painless, secure, and easy technique called transcranial Direct Current Stimulation (tDCS) has been shown to increase performance in a variety of social and cognitive activities. As a consequence, by focusing on certain underlying brain issues, tDCS has the ability to enhance cognitive, motor, and social communication capacities in clinical groups like ASD patients.
People with autism have a broken cerebellum-prefrontal brain connection. Disruptions in certain cerebral-cerebellar networks that interfere with the functional and anatomical specialization of cortical areas responsible for motor control, language, and social interaction are the root cause of Autism Spectrum Disorder (ASD). A number of neurophysiological and neuroimaging investigations have shown that the Prefrontal Cortex (PFC) of people with ASD has an E: I (Excitation-Inhibition) imbalance in various locations. According to MRS research, ASD individuals have a larger E: I ratio because their left frontal brain has more glutamate than their right frontal cortex, but not the other way around. By causing subthreshold alterations in the resting membrane potentials of the targeted neuronal group, tDCS modulates cortical excitability.
Greater E: I ratios in the right vmPCF (ventromedial Prefrontal Cortex) and left DL-PFC (Dorsolateral Prefrontal Cortex) in ASD may be brought on by higher levels of glutamate and lower levels of GABA (Gamma-Aminobutyric Acid) in the brain. According to research, tDCS cathodal stimulation of the left DL-PFC reduces cortical excitability by increasing local excited glutamate levels, whereas tDCS anodal stimulation of the right vmPCF increases cortical excitability by increasing local GABA concentrations, thereby enhancing processing and cognitive flexibility in ASD.
By reducing hyperactivity and social withdrawal and improving processing speed, linguistic ability, and cognitive flexibility in patients with ASD, tDCS has been demonstrated to benefit neurologically wounded people. Two studies that were released in 2015 suggested that tDCS therapy had substantial and enduring impacts on a range of parameters. In the first study, 12 young adults with autism and intellectual disabilities who were only moderately talkative received tDCS 10 times daily. Eight out of ten research participants reduced their aberrant behaviors, resulting in an average ABC score decline of 26.7%. The subscale measuring hyperactivity and disobedience had the most dramatic and statistically significant decline.
A case study of a 14 years old girl with ASD and drug resistant catatonia revealed long term improvement in the second publication. The patient's rigidity, impulsivity, stereotyped behaviors, and unwillingness to eat or drink were entirely reversed after 28 sessions of tDCS. There was some improvement in the expressions of grimacing, low mood, gazing, and oppositional and confrontational behaviors. The child steadily made improvements to her grip reflex and motor planning. By the time the therapy was through, she had started eating and was able to feed herself.
According to certain research, tDCS helped ASD patients with repetitive and limited behaviors. It has task-dependent effects on EF (Executive Functioning) performance and enhances the therapeutic benefits of behavioral therapy. Micro current treatment enhanced speaking and listening abilities in kids with speech impairments and developmental delays. It alters the alpha and theta band activity in significant brain regions and promotes the development of motor skills. A single 30 minutes therapy session significantly improved vocabulary and syntax learning. Additionally, it improves working memory.
Results and Discussion
Corresponding too many studies, it is clearer to distinguish autism spectrum disorder symptoms that considered as roadblock in communication. The symptoms are summarized in non-communication behavior with respect to other symptoms were mentioned as sleep disturbance or epilepsy gastrointestinal symptoms.
Transcranial Direct Current Stimulation (tDCS) a noninvasive neurological method was found effective in changing of cortical excitability mainly by applying electrodes (anode and cathode) on the scalp with two sponges. This neuromodulation tool was found promising method for treating ASD symptoms according to its effective function in motor and sensory regions as poor/non-communication, language, memory and motor control disturbance.
According to studies, tDCS had shown effective in ASD patients by frequent sessions in 3 weeks. Studies had shown effective in real tDCS groups compared with sham tDCS group in reducing of CARS scores and CSHQ score in tDCS group with constant CARS, ABC and RSB scores in sham tDCS groups in ASD patients. With these facts, it was clear that real tDCS have effective impact in reducing CARS and ABC scores in ASD patients. With this decrease, left DLPFC stimulation had reduced ABC scores in autistic patients. These methods had shown significant link between CARS and ABC in pre/post-treatment in ASD patients in that the more the symptoms are severing the more the tDCS is effective in reducing the symptoms in ASD patients.
The CARS scale is 15 item the distinguish and identify children or adults with autism. Besides that, it acts as measurement of severity in autism spectrum disorder. CARS scale is distinguished and specialized more from ABC or even RSB scale in that CARS scale is assessed by trained clinical compared to ABC and RSB that measured by guardians of the children with ASD.
Study tools detected that CARS scale is significantly important in distinguish autistic patients from normal children especially in the 15th item according to the detected reduced rate in CARS 15 item while applying real tDCS tool in ASD patients with respect to the other 14 items. With combining and summarizing the results, its acceptable to use tDCS tool with CARS and other scale id distinguish ASD.
Despite the fact that the informative of these findings, other anatomical and pathophysiological changes that may be detected should give more clear understanding in autism spectrum disorder. Physiological changes in left DLPFC prefrontal cortex had should great impact in the cause of sleep disturbances in autistic patients according to its control in sleep physiology and dreaming. This fact had confirmed by the confirmation of the physiology and function of prefrontal cortex in sleep control. One of these studies that confirm that, non-rapid-eye-movement during sleep had noticed to be due the activity of the prefrontal cortex in high voltage and slow brain wave with respect to other cortical regions.
Corresponding to tDCS studies, it is important beside the study to know the motor and sensory change in ASD patients after each session of tDCS tool. Questions should be asked to the parents according their autistic child behavior after the tDCS treatment as well in case of new autistic or non-autistic symptoms that appeared after the treatment. This evaluation will give more accurate results in the safety of tDCS as treatment to ASD patients as well confirmation to its impressive effects in reducing symptoms with autism. Parents detected that after frequent one week of tDCS hyperactivity behavior had been noticed. Restrict 3 weeks in tDCS treatment had shown no significant new symptoms as well reduced in their suffering symptoms had been noticed.
Contributing to these well effects of tDCS as treatment in reducing ASD symptoms, the exact mechanism of tDCS is yet unknown. Developmental screenings and tools had given more understandable results of tDCS method. Correspond to history taking before and after treatments, results shows that frequent stick to tDCS as treatment gives better results in improving as reducing symptoms. Besides that, it had shown that it is safe treatment according to no evidence or new symptoms had been detected.
Radiological screening as fMRI wasn’t a promising tool in ASD. EEG had shown great impact in ASD according its safety and ease on children as a method. Beside the safety, EEG is impressive tool as it had discovered changes in brain waves in autistic patients. EEG detected Peak Alpha Frequency (PAF) as a marker in ASD. According to these finding autistic patients had been compared before and after tDCS treatment shown that increase in PAF stimulation as improvement in the two domains of ATEC impacted by tDCS. Beside other findings and results of tDCS impact on autism as pre/ post-treatment behavioral improvements impressively.
Last but not least, tDCS in frequent sessions not less than 3 weeks had great impact in behavioral improvements and reducing autistic symptoms with safety of children with noticing no evidence of new symptoms according its effect on left DLPFC.
Conclusion
last but not least, to summarize the impressive effects on tDCS neuromodulation method as treatment to be used in autism spectrum disorder, had need many studies to understand its best way and time to use to give its best results. Involving studies with tDCS treatment with autism had shown that mainly it was preferable to be used in frequency not less than 3 weeks according its effect by more than one session. It had shown its safety on autistic children with no noted issues or new autistic symptoms. Correspond to these facts, tDCS is well neuromodulation tool that shows promising of reducing and control symptoms in autism spectrum disorder.
Limitations
Limitation to these studies had done to evaluate the best effective way in using tDCS as treatment. Limitations are using tDCS, had started between sham and real tDCS group with one session only to evaluate the tDCS effectiveness without comparing the frequency impact of it. Second limitation was main goal to determine the apparent of difference effects of tDCS before and after treatment without using any scale tools as Autism Behavior Checklist (ABC), Social Communication Questionnaire (SCQ), Social Responsiveness Scale (SRS), and clancy behavior scale. This limitation was disappointed due to its far goal from the main goal which is tDCS treatment effectiveness on ASD.
Corresponding to these limitations, evaluating symptoms before and after tDCS treatment in autistic patients to determine the safety and main symptomatic effects as well as studies had shown limitations in the frequency impact on autism.
To conclude limitations, responding to many study limitations it has been detected that the more the tDCS session up to 3 weeks had shown great impact than one session, correlate to this, severity have great role in tDCS results that the more autism symptoms is severe the more the effect of tDCS result will detect.
References
- Trottier G, Srivastava L, Walker CD (1999) Etiology of infantile autism: A review of recent advances in genetic and neurobiological research. J Psychiatry Neurosci 24 :103-115.
[Google Scholar] [PubMed]
- Garcia-Gonzalez S, Lugo-Marin J, Setien-Ramos I, et al. (2021) Transcranial direct current stimulation in autism spectrum disorder: A systematic review and meta-analysis. Eur Neuropsychopharmacol 48: 89-109.
[Crossref] [Google Scholar] [PubMed]
- Qiu J, Kong X, Li J, Yang J, Huang Y, et al. (2021) transcranial Direct Current Stimulation (tDCS) over the left dorsal lateral prefrontal cortex in children with Autism Spectrum Disorder (ASD). Neural Plast 2021: 6627507.
[Crossref] [Google Scholar] [PubMed]
- Luckhardt C, Schutz M, Muhlherr A, Mossinger H, Boxhoorn S,et al. (2021) Phase-IIa randomized, double-blind, sham-controlled, parallel group trial on anodal transcranial Direct Current Stimulation (tDCS) over the left and right tempo-parietal junction in autism spectrum disorder-StimAT: Study protocol for a clinical trial. Trials 22: 1-6.
[Crossref] [Google Scholar] [PubMed]
- Samsam M, Ahangari R, Naser SA (2014) Pathophysiology of autism spectrum disorders: Revisiting gastrointestinal involvement and immune imbalance. World J Gastroenterol 20: 9942–9951.
[Crossref] [Google Scholar] [PubMed]
- Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J (2018) Autism spectrum disorder. Lancet 392: 508-520.
[Crossref] [Google Scholar] [PubMed]
- Compart PJ (2013) The pathophysiology of autism. Glob Adv Health Med 2: 32-37.
- Ha S, Sohn IJ, Kim N, Sim HJ, Cheon KA (2015) Characteristics of brains in autism spectrum disorder: Structure, function and connectivity across the lifespan. Exp Neurobiol 24: 273–84.
[Crossref] [Google Scholar] [PubMed]
- Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, et al. (2006) Autism from 2 to 9 years of age. Arch Gen Psychiatry 63: 694-701.
[Crossref] [Google Scholar] [PubMed]
- Freeth M, Sheppard E, Ramachandran R, Milne E (2013) A cross-cultural comparison of autistic traits in the UK, India and Malaysia. J Autism Dev Disord 43: 2569-2583.
[Crossref] [Google Scholar] [PubMed]
- Juneja M, Mishra D, Russell PS, Gulati S, Deshmukh V, et al. (2014) INCLEN Diagnostic Tool for Autism Spectrum Disorder (INDT-ASD): Development and validation. Indian Pediatr 51: 359-365.
[Crossref] [Google Scholar] [PubMed]
- Geier DA, Kern JK, Garver CR, Adams JB, Audhya T, et al. (2009) Biomarkers of environmental toxicity and susceptibility in autism. J Neurol Sci 280: 101-108.
[Crossref] [Google Scholar] [PubMed]
- Jackson MP, Rahman A, Lafon B, Kronberg G, Ling D, et al. (2016) Animal models of transcranial direct current stimulation: Methods and mechanisms. Clin Neurophysiol 127: 3425-3454.
[Crossref] [Google Scholar] [PubMed]
- Zheng Z, Zhu T, Qu Y, Mu D (2016) Blood glutamate levels in autism spectrum disorder: A systematic review and meta-analysis. PLoS One 11: e0158688.
[Crossref] [Google Scholar] [PubMed]
- Clark VP, Coffman BA, Trumbo MC, Gasparovic C (2011) transcranial Direct Current Stimulation (tDCS) produces localized and specific alterations in neurochemistry: A 1H magnetic resonance spectroscopy study. Neurosci lett 500: 67-71.
[Crossref] [Google Scholar] [PubMed]
- Zhao X, Ding J, Pan H, Zhang S, Pan D, et al. (2020) Anodal and cathodal tDCS modulate neural activity and selectively affect GABA and glutamate syntheses in the visual cortex of cats. J Physiol 598: 3727-3745.
[Crossref] [Google Scholar] [PubMed]
- D’Urso G, Toscano E, Sanges V, Sauvaget A, Sheffer CE, et al. (2021) Cerebellar transcranial direct current stimulation in children with autism spectrum disorder: A pilot study on efficacy, feasibility, safety, and unexpected outcomes in Tic disorder and epilepsy. J Clin Med 11: 143.
[Crossref] [Google Scholar] [PubMed]
- Fehring DJ, Illipparampil R, Acevedo N, Jaberzadeh S, Fitzgerald PB, et al. (2019) Interaction of task related learning and transcranial direct current stimulation of the prefrontal cortex in modulating executive functions. Neuropsychologia 131: 148–159.
[Crossref] [Google Scholar] [PubMed]
- Luckhardt C, Boxhoorn S, Schuetz M, Fann N, Freitag CM (2021) Brain stimulation by tDCS as treatment option in autism spectrum disorder-A systematic literature review. Prog Brain Res 264: 233-257.
[Crossref] [Google Scholar] [PubMed]
- Tu Y, Cao J, Guler S, Chai-Zhang T, Camprodon JA, et al. (2021) Perturbing fMRI brain dynamics using transcranial direct current stimulation. NeuroImage 237: 118100.
[Crossref] [Google Scholar] [PubMed]
Citation: Srijamya, Kumar H, Mishra B, Khan MW, Nair MJM, et al. (2023) Topic: Effect of TDCS in Children with Autism. Clin Neuropsycho 6: 205. DOI: 10.4172/CNOA.1000195
Copyright: © 2023 Srijamya, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 691
- [From(publication date): 0-2023 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 483
- PDF downloads: 208