Effect of Glucose and Fructose on Non-Alcoholic Fatty Liver Disease (NAFLD)- A Review
Received: 27-Feb-2023 / Manuscript No. JCMHE-23-90308 / Editor assigned: 01-Mar-2023 / PreQC No. JCMHE-23-90308 (PQ) / Reviewed: 15-Mar-2023 / QC No. JCMHE-23-90308 / Revised: 03-May-2023 / Manuscript No. JCMHE-23-90308 (R) / Published Date: 10-May-2023
Abstract
The liver is a large organ in the abdomen that is responsible for many vital functions in the body. Liver diseases will cause a gradual loss of liver function and result in inflammation and destruction of renal parenchyma. Non-Alcoholic Fatty Liver Disease (NAFLD) has been a public health concern since diabetes and obesity are more prevalent than ever. Non-Alcoholic Fatty Liver Disease (NAFLD), the most common chronic liver condition, increases the risk of other comorbidities such as type 2 diabetes and cardiovascular disease, as well as liver related morbidity and death. Insulin resistance is the primary cause of NAFLD, but other complex factors such as lifestyle, hormones and genetics also play a role in its development. High carbohydrate consumption is major stimulants to NAFLD by concerning the involvement of carbohydrate induced De Novo Lipogenesis (DNL) pathway and the gut microbiome in NAFLD. The increased consumption of fructose rich sweeteners, such as High Fructose Corn Syrup (HFCS), in the diet caused mitochondrial dysfunction and increased apoptotic activity in the liver. In this reviews we focus on how fat, carbohydrates, glucose and sugar substances accumulate and affect the liver, in addition how to keep them under control.
Keywords: Non-alcoholic fatty liver disease, Liver disease; Glucose, Fructose, High Fructose Corn Syrup (HFCS), Intermittent fasting, Carbohydrates, Low carbs diet, Obesity
Keywords
Non-alcoholic fatty liver disease; Liver disease; Glucose; Fructose; High Fructose Corn Syrup (HFCS); Intermittent fasting; Carbohydrates; Low carbs diet; Obesity
Introduction
The liver is a large organ in the abdomen that is important in carbohydrate homeostasis because it controls glucose levels by synthesizing and degrading glycogen and producing glucose via gluconeogenesis. Furthermore, it has been widely believed that the liver is the primary site of fructose metabolism. Liver performs a variety of vital bodily functions such as blood filtering, toxins are removed from the blood, removes old red blood cells, produces bile and a fluid that aids the body’s digestion breaking down of food, proteins, carbohydrates and fats are metabolized by this organ so that your body can use them, produces substances that aid in blood clotting, it controls the amount of blood in the body, glycogen (an energy source) and vitamins are stored for later use by the body. It is also classified as a gland because it produces chemicals that the body requires. Certain diseases and lifestyle choices can harm the liver. Chronic liver disease occur as a gradual loss of liver functions which is lasts for more than six months and results in inflammation, destruction and regeneration of the liver parenchyma, leading to fibrosis and cirrhosis. Cirrhosis is the end stage of chronic liver disease that results in liver organ disruption. Usually individual with chronic liver disease present with no symptoms, by taking the patient’s history to find out long term consuming of nephrotoxic drugs or alcohol use and as well as measuring the serum concentrations of AST, ALT which is mild to moderately increased can indicate the liver disease. The underlying cellular mechanism of fibrosis and cirrhosis is the enrollment of stellate cells and fibroblasts tends to result in fibrosis, whereas parenchymal regeneration is dependent on hepatic stem cells [1,2].
Literature Review
Non-Alcoholic Fatty Liver Disease (NAFLD)
Non-Alcoholic Fatty Liver Disease (NAFLD) is the most common chronic liver disease, which refers to abnormal fat accumulation in the liver that is not due to excessive alcohol consumption [3]. NAFLD is very common in children and adolescents, particularly in obese patients and has even been detected in newborn babies from mothers with gestational diabetes. NAFLD encompasses both Nonalcoholic Fatty Liver (NAFL) and Nonalcoholic Steatohepatitis (NASH). NAFL is defined as having more than 5% steatosis of the liver’s parenchyma in the absence of significant inflammation or fibrosis (scarring). NASH, on the other hand, typically exhibits lobular inflammation and hepatocyte ballooning histologically with injured hepatocytes in a background of steatosis and is associated with faster fibrosis progression than NAFLD. While the majority of cases are benign and asymptomatic, some people may go to develop liver inflammation a condition which is diagnosed when steatotic liver tissue exhibits inflammatory activity and hepatocyte injury and lead to the destruction of liver tissues, severe damage may cause scarring resulting in liver cirrhosis and eventually liver failure [4]. Most people with NAFLD have no symptoms although some present with fatigue, malaise or pain or discomfort in the upper right abdomen. When NASH develops symptoms may include jaundice, weakness, itchy skin, loss of appetite, and nausea. Obesity, saturated fat rich foods, type 2 diabetes mellitus or hyperinsulinemia, hypertension and dyslipidemia are all strongly linked to the development of NAFLD. NAFLD is not only the manifestation of metabolic syndrome but may also be the beginning of the metabolic syndrome [5].
NAFLD linked to diabetes mellitus
NAFLD is estimated to affect more than 70% of obese adults with type 2 diabetes. Diabetes type 2 is the most significant predictor of NAFLD related hepatic fibrosis and cirrhosis. However, it was only in the last few decades that it was recognized that people with obesity and prediabetes could develop NAFLD. NAFLD is nearly always associated with insulin resistance and type 2 diabetes mellitus. Many patients with NAFLD exhibit metabolic syndrome like characteristics, such as elevated plasma triglycerides, low HDL cholesterol, impaired fasting glucose levels, an increased waist circumference and high blood pressure [6]. The pathogenesis between NAFLD and type 2 diabetes is not fully understood, but insulin resistance appears to be a major contributor, with obesity being the most common cause of insulin resistance. As calorie intake increases and obesity progresses, changes in lipid metabolism, combined with inflammation in adipose tissue and ectopic sites of fat deposition, lead to insulin resistance, which is primarily caused by post receptor abnormalities in insulin signalling pathways.
According to Leon A Adams, et al., compared NAFLD patients to control subjects, none of whom had diabetes at the beginning; those with NAFLD were more likely to have diabetes and metabolic syndrome when they were re-evaluated eleven years later. In other study included 400 adult patients with NAFLD who are at high risk of developing advanced fibrosis, noticed that diabetes and aminotransferase levels are distinct predictors of moderate to severe fibrosis. As a result, the presence of diabetes in NALFD is critical because NAFLD can progress to NASH [7].
Prevalence: NAFLD is quite prevalent; according to a recent study, its global prevalence is predicted to be 32.4%, men had a noticeably higher frequency of NAFLD than women did, although the prevalence of NAFLD is increasing over the time.
Etiology: Nonalcoholic fatty liver can develop for many reasons, the causes are complex and mainly involve: Hormonal such as ghrelin, leptin, insulin as well as sexual hormones (polycystic ovary syndrome, estrogen deficiency/menopause and male hypogonadism) lifestyle (nutrition, inactivity), environmental and genetics. However the condition seems to associate with metabolic risk factors that also define metabolic syndrome, namely; being overweight or obese especially in the abdomen, having high triglycerides or Low Density Lipoprotein (LDL) levels in the blood, having high blood pressure or having insulin resistance or glucose intolerance. There is also an evidence of when high fructose diet can cause fatty liver even when there is no weight gain [8,9].
Pathophysiology: In 1998, Day and James proposed the most widely used and accepted model "two hit hypothesis". The first hit is caused by insulin resistance, which causes fat droplets to accumulate in the cytoplasm of hepatocytes, leading to the development of steatosis. Insulin resistance causes an increase in the delivery of free fatty acids and triglycerides to the liver as well as a decrease in excretion, resulting in accumulation. Excess carbohydrates also stimulate fatty acid synthesis in the liver. The “first hit” makes the liver more vulnerable to many of the “second hit” factors that promote hepatic injury, inflammation and fibrosis. These factors include oxidative stress and subsequent lipid peroxidation, proinflammatory cytokines, adipokines and mitochondrial dysfunction [10]. The second hit is multifactorial, resulting in hepatocellular injury and the development of NASH. Excess fatty acids in the liver make it more susceptible to injury. The injury is thought to be caused by peroxisomal fatty acid oxidation, Reactive Oxygen Species (ROS) production from the mitochondrial respiratory chain, cytochrome P450 fatty acid metabolism and hepatic metabolism of gut derived alcohol. Obesity also contributes to the second hit by releasing inflammatory mediators such as leptin, Tumour Necrosis Factor (TNF)-alpha and Interleukin (IL)-6, which cause hepatocyte damage. The second hit also includes insulin resistance. NASH develops and progresses as a result of sinusoidal collagen deposition caused by hepatic stellate cell activation and portal fibrosis caused by ductular proliferation. These changes have been linked to insulin resistance, which is now thought to be the cause of steatosis progressing to NASH and progressive fibrosis [11].
Diagnosis: Non-Alcoholic Fatty Liver Disease (NAFLD), it ranges from simple fatty liver (steatosis) to Nonalcoholic Steatohepatitis (NASH), a state of hepatocellular inflammation and damage caused by fat accumulation. Diagnosis of NAFLD is typically given to patients who have not consumed alcohol in amounts considered harmful to the liver [12]. There is no fixed biochemical marker that can be used to differentiate the stages of NAFLD (simple steatosis, NASH, and cirrhosis), although there are some tests which can be used include: Magnetic Resonance Imaging (MRI), Computed Tomography (CT) and ultrasounds however, Al-Busafi SA, et al., reported that Xenon-133 liver scan (Xe-133 gas) proved to be safe, inexpensive, dependable, noninvasive method for diagnosing and quantifying hepatic steatosis, outperforming ultrasound [13].
NAFLD induced Hepatocellular Carcinoma (HCC)
Hepatocellular Carcinoma (HCC) has been shown to be the most common type of cancer in type 2 diabetes and obesity nearly doubles the risk of HCC. As a result, mostly in near future, a rapidly increasing incidence of NAFLD-HCC is possible, up to 50% of NAFLD-HCCs occurring in patients without cirrhosis and being detected at a late stage [14]. Nonalcoholic Steatohepatitis (NASH) is a well-known cause of cirrhosis that is linked to the development of HCC [15]. Mostly in 10 years after the onset of Steatohepatitis (NASH), up to 30% of patients may develop cirrhosis and Hepatocellular Carcinoma (HCC), and the abnormal DNA methylation is what causes NAFLD to progress to cancer [16].
Role of glucose in the fatty liver: So fatty liver starts when fat gets deposited in the liver and it gets progresses through four stages; the first stage is just inflammation that get slowly progresses to form scar tissue called stage two and in stage three fibrosis occur when persistent inflammation causes scar tissue around the liver and as well as blood vessels, but the liver is still able to function normally and eventually we end up in a final stage called cirrhosis which is the most severe stage, it happens when normal liver tissues are replaced by fibrosis to the extent that the structure and function of the liver is affected and can lead to liver failure and liver cancer [17,18].
In fact, fats are not a bad thing, we need fats for our energy and the fat is produced by the liver using the food that we eat by involving the De Novo Lipogenesis (DNL) pathway. De Novo Lipogenesis (DNL) is an endogenous pathway in which excess dietary starch, sugar, protein and alcohol are converted into specific Fatty Acids (FAs). Although elevated DNL levels have been linked to a variety of metabolic abnormalities [19].
The fat in the liver is not obtained from the fat we consume, but rather from the sugar and carbohydrates that accumulate in the liver. Carbohydrates are mostly made up of glucose. Consumed carbohydrates are a major stimulant for hepatic de Novo Lipogenesis (DNL) and are associated with highly probable than dietary fat to directly contribute to NAFLD, The main cause of fatty liver is sugar, which are all carbohydrates that we consume [20]. In fatty liver patients, the liver is literally sugar coated. Sugar contains two molecules glucose and fructose. Glucose can be metabolized by organs other than liver such as gut, muscle and brain, but fructose can get metabolized extensively by the liver, where it stimulates fat synthesis. Indeed, some experts believe that our bodies are not designed to cope with excessive fructose. The liver metabolizes almost 70% of fructose consumed by humans. Fructose is catabolized way quicker in the liver and is even more lipogenic than glucose. Ouyang X, et al., and colleagues compare NAFLD patient without cirrhosis who were age, gender and BMI matched, subjects with NAFLD consumed 2 times to 3 times more fructose from sugary sweetened beverages than controls, which was linked to increased expression of fructokinase (KHK) in the liver, an important enzyme for fructose metabolism and fatty acid synthase, an important enzyme for lipogenesis. Justus von Liebig, a German chemist, discovered that simple carbohydrates increased fat accumulation in the liver. Indeed, by the 1960's, numerous scientists reported that fructose was distinct from glucose in its ability to raise both plasma triglycerides and liver fat.
According to the study high fructose diet stimulates hepatic de novo fatty acid synthesis and lead to enhance oxidative stress, inflammation, hyperuricemia, hypertriglyceridemia, higher systolic blood pressure, and insulin resistance. Fructose has been proposed as a key factor in the development of NASH. Studies suggest that fructose which is present in sugar and beverages are highly responsible to induce metabolic syndrome in humans. Experimental animal study conducted by Ackerman Z, et al., and colleagues by using long term fructose administration to rats resulted to cause a hepatic macro and microvesicular steatosis, with an increase in hepatic triglycerides of 198% and an increase in hepatic cholesterol concentration of 89%.
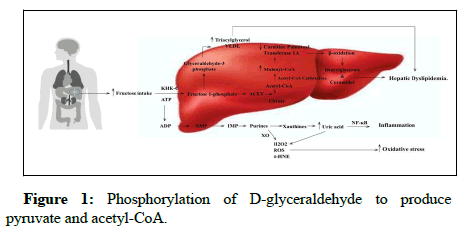
When fructose enters the stomach, it goes into the liver, where it is converted to fat and exported to the intestine, where it can be digested. High fructose intake activates the aldolase B enzyme, which converts fructose to dihydroxyacetone phosphate and D-glyceraldehyde. Triokinase then promotes lipid dysregulation by stimulating the phosphorylation of D-glyceraldehyde to produce pyruvate and acetyl-CoA (Figure 1). So, when the fructose is in minimal quantities it doesn’t harm the body but when is in excessive amount it gets converted into fat and deposited in the liver rather than exporting into the intestine and promotes lipogenesis, oxidative stress, uric acid production, inflammation and dysbiosis in the gut, all of which contribute to necrosis and fibrosis in Nonalcoholic Steatohepatitis (NASH).
In the liver, fructose is broken down. Fructose enters the hepatocytes and is phosphorylated by Ketohexokinase-C to fructose 1-phosphate (KHK-C). Fructose 1-phosphate is converted to glyceraldehyde-3 phosphate, which is used to make triacylglycerols and Very Low Density Lipoproteins (VLDL). Fructose consumption can promote citrate breakdown to acetyl-CoA by upregulating the ATP Citrate Lyase (ACLY) enzyme. Acetyl-CoA carboxylase converts acetyl-CoA to malonyl-coenzyme-A (malonyl-CoA) (ACC-1). Malonyl-CoA levels are elevated, which inhibits oxidation by limiting carnitine palmitoyl transferase 1A, promoting the accumulation of diacylglycerols and ceramides and causing hepatic dyslipidemia. Furthermore, increased KHK-C activity depletes Adenosine Triphosphate (ATP), resulting in Adenosine Diphosphate (ADP), which is then converted to Adenosine Monophosphate (AMP). In turn, AMP is converted to Inosine Monophosphate (IMP), which increases purine production. Xanthine Oxidoreductase (XO) generates oxygen Reactive Species (ROS), Hydrogen peroxide (H2O2), 4-Hydroxynonenal (4-HNE) and xanthine. The xanthine is then metabolized, resulting in the overproduction of uric acid and ROS, both of which cause oxidative stress. Uric acid activates Nuclear Factor-B (NF-B), causing inflammation.
When carbs enter the body breakdown of carbohydrates begins in the mouth with salivary amylase, the stomach acid breaks them down into glucose and activates the hormone insulin. Insulin then transports the glucose into the body’s cells, where it provides energy for ordinary everyday activities. When blood glucose levels fall, the pancreas produces glucagon, which stimulates the liver to release stored glucose. When there is more glucose than needed, the liver stores it as glycogen, which the body uses when food is unavailable. Since glycogen gets deposited in the body it gets converted in fat or triglycerides. Often the high amount of fructose administration has an ability to increase the uric acid level, Nakagawa T, et al., experiment reported that fructose fed rats had increased hepatic uric acid production, systolic blood pressure, and fasting insulin levels.
In a study done by Maersk M, et al., and colleagues showed that there was a great change in liver fat and skeletal muscle fat in a group who were consumed of 1 L of sugary beverages (e.g. regular cola) versus daily consumption of 1 L of isocaloric semiskim milk, diet cola (0 calories) or water after 6 months.
A study of administration of high fructose diet for seven years in cynomologus monkeys, resulting in both an increase in liver fat and hepatic fibrosis, with the degree of fibrosis correlating with the time of fructose exposure, also noticed that number and diameter of the lipid droplets increased as the fructose containing diet was consumed for a longer period of time.
Discussion
Managing fatty liver caused by fructose and glucose
Maintaining an unhealthy lifestyle, eating excessive amounts of food high in calories and trans fats and drinking beverages high in fructose have all been identified as major contributors to the growing epidemic of obesity and its comorbidities. Sugar sweetened beverages have been linked to weight gain in adults and children, as well as chronic health consequences such as an increased risk of obesity, diabetes, cardiovascular disease and fatty liver disease. Although fructose is found in honey and fruits, sucrose and HFCS are the primary sources of fructose, particularly in sugary sweetened beverages. Therapeutic approaches for NAFLD is usually through following a healthy lifestyle, diet, weight loss and physical activity are recommended by both the American and European liver associations. The single most important way to prevent NAFLD is to achieve and maintain a healthy body weight. Furthermore, weight loss is the most effective way to reverse the course of established NAFLD in overweight or obese patients. Weight loss can be accomplished through caloric restriction from dieting by consuming at least 500 kcal-1000 kcal, as well as bariatric surgery in morbidly obese patients, increased physical activity and/or pharmacotherapeutic agents that reduce hepatic steatosis and insulin resistance. The EASL-NAFLD guidelines recommend energy restriction and the elimination of NAFLD promoting components (i.e. processed foods, products high in added fructose) and a "Mediterranean diet" should be recommended to all NAFLD patients. Identifying and treating metabolic syndrome such as diabetes, obesity, hypertension, hyperlipideamia and improving insulin resistance through weight loss, exercise or pharmacotherapy and using hepato protective agents such as antioxidants shown to be effective against NAFLD.
A meta-analysis of randomised controlled trials looked at the long term effects of low carbohydrate diets versus low fat diets on metabolic risk factors that low carbohydrate diets have been shown to facilitate in weight loss, lower intrahepatic triglyceride levels and improve metabolic parameters in obese patients. Low carbohydrate and low fat diets both helped people lose weight and improve their metabolic risk factors.
Sevastianova, et al., observed 16 subjects with a BMI=30.61.2, on a high carbohydrate diet (>1,000 Kcal) for 3 weeks had a >10 fold greater relative change in liver fat (27%) than in body weight (2%) and that increased liver fat was positively correlated with De Novo Lipogenesis (DNL). Moreover, a 6 month hypocaloric diet resulted in a decrease in body weight as well as a return to normal liver fat. This study indicate that fat accumulates in the human fatty liver during carbohydrate overfeeding and supports a role for DNL in the pathogenesis of NAFLD.
Conclusion
There is sufficient evidence to suggest that the fructose component of sugar and HFCS plays a significant role in development of fatty liver by both stimulating de novo lipogenesis and inhibiting fatty acid oxidation. These effects are caused by fructokinase's unique fructose metabolism, which results in a drop in ATP with nucleotide turnover and uric acid generation, resulting in hepatic dyslipidemia, inflammation and increased oxidative stress. While there are numerous causes of NAFLD, the consumption of fructose containing sugars is most likely to play a significant role due to the increased risk of metabolic syndrome and obesity. Reduced consumption of fructose, primarily in soft drinks, is beneficial in lowering the risk of NAFLD. Besides that maintaining a balanced lifestyle, low carbohydrates diet and engaging in physical activity help to reduce fat accumulation in the body. Although more evidence is required to support the low carbohydrate diet is effective in NAFLD.
Statement of Declaration
Funding: The authors declared that no funds, grants or other support were received during the ongoing preparation of the manuscript.
Competing interests: The authors declare that there is no conflict of interest.
References
- Marino L, Jornayvaz FR (2015) Endocrine causes of non-alcoholic fatty liver disease. World J Gastroenterol 21: 11053.
[Crossref] [Google Scholar] [PubMed]
- March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, et al. (2010) The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod 25: 544-551.
[Crossref] [Google Scholar] [PubMed]
- Sanyal AJ, Campbell-Sargent C, Mirshahi F, Rizzo WB, Contos MJ, et al. (2001) Non-alcoholic steatohepatitis: Association of insulin resistance and mitochondrial abnormalities. Gastroenterology 120: 1183-1192.
[Crossref] [Google Scholar] [PubMed]
- Al Shaalan R, Aljiffry M, Al-Busafi S, Metrakos P, Hassanain M (2015) Non-alcoholic fatty liver disease: Non-invasive methods of diagnosing hepatic steatosis. Saudi J Gastroenterol 21: 64.
[Crossref] [Google Scholar] [PubMed]
- Mehta SR, Thomas EL, Bell JD, Johnston DG, Taylor-Robinson SD (2008) Non-invasive means of measuring hepatic fat content. World J Gastroenterol 14: 3476.
[Crossref] [Google Scholar] [PubMed]
- Al-Busafi SA, Ghali P, Wong P, Novales-Diaz JA, Deschenes M (2012) The utility of Xenon-133 liver scan in the diagnosis and management of non-alcoholic fatty liver disease. Can J Gastroenterol 26: 155-159.
[Crossref] [Google Scholar] [PubMed]
- Chao HW, Chao SW, Lin H, Ku HC, Cheng CF (2019) Homeostasis of glucose and lipid in non-alcoholic fatty liver disease. Int J Mol Sci 20: 298.
[Crossref] [Google Scholar] [PubMed]
- Lonardo A, Nascimbeni F, Maurantonio M, Marrazzo A, Rinaldi L, et al. (2017) Non-alcoholic fatty liver disease: Evolving paradigms. World J Gastroenterol 23: 6571.
[Crossref] [Google Scholar] [PubMed]
- Ballestri S, Zona S, Targher G, Romagnoli D, Baldelli E, et al. (2016) Non-alcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J Gastroenterol Hepatol 31: 936-944.
[Crossref] [Google Scholar] [PubMed]
- Golob-Schwarzl N, Bettermann K, Mehta AK, Kessler SM, Unterluggauer J, et al. (2019) High keratin 8/18 ratio predicts aggressive hepatocellular cancer phenotype. Transl Oncol 12: 256-268.
[Crossref] [Google Scholar] [PubMed]
- Campo JAD, Gallego-Duran R, Gallego P, Grande L (2018) Genetic and epigenetic regulation in Non-Alcoholic Fatty Liver Disease (NAFLD). Int J Mol Sci 19: 911.
[Crossref] [Google Scholar] [PubMed]
- Sanders FW, Griffin JL (2016) De novo lipogenesis in the liver in health and disease: More than just a shunting yard for glucose. Biol Rev Camb Philos Soc 91: 452-468.
[Crossref] [Google Scholar] [PubMed]
- Muriel P, Lopez-Sanchez P, Ramos-Tovar E (2021) Fructose and the liver. Int J Mol Sci 22: 6969.
[Crossref] [Google Scholar] [PubMed]
- Jang C, Hui S, Lu W, Cowan AJ, Morscher RJ, et al. (2018) The small intestine converts dietary fructose into glucose and organic acids. Cell Metab 27: 351-361.
[Crossref] [Google Scholar] [PubMed]
- Ouyang X, Cirillo P, Sautin Y, McCall S, Bruchette JL, et al. (2008) Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J Hepatol 48: 993-999.
[Crossref] [Google Scholar] [PubMed]
- Jensen T, Abdelmalek MF, Sullivan S, Nadeau KJ, Green M, et al. (2018) Fructose and sugar: A major mediator of non-alcoholic fatty liver disease. J Hepatol 68: 1063-1075.
[Crossref] [Google Scholar] [PubMed]
- Brumbaugh DE, Tearse P, Cree-Green M, Fenton LZ, Brown M, et al. (2013) Intrahepatic fat is increased in the neonatal offspring of obese women with gestational diabetes. J Pediatr 162: 930-936.
[Crossref] [Google Scholar] [PubMed]
- Mosca A, Della Corte C, Sartorelli MR, Ferretti F, Nicita F, et al. (2016) Beverage consumption and paediatric NAFLD. Eat Weight Disord 21: 581-588.
[Crossref] [Google Scholar] [PubMed]
- Johnson RJ, Segal MS, Sautin Y, Nakagawa T, Feig DI, et al. (2007) Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease and cardiovascular disease. Am J Clin Nutr 86: 899-906.
[Google Scholar] [PubMed]
- Havel PJ (2005) Dietary fructose: Implications for dysregulation of energy homeostasis and lipid/carbohydrate metabolism. Nutr Rev 63: 133-157.
[Crossref] [Google Scholar] [PubMed]
Citation: Tom A, Zamanigerashi S, Nath HS (2023) Effect of Glucose and Fructose on Non-Alcoholic Fatty Liver Disease (NAFLD)-A Review. J Community Med Health Educ 13: 805.
Copyright: © 2023 Tom A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1816
- [From(publication date): 0-2023 - Mar 10, 2025]
- Breakdown by view type
- HTML page views: 1639
- PDF downloads: 177