Research Article Open Access
Effect of Capacitive and Resistive Electric Transfer on Tissue Temperature, Muscle Flexibility, and Blood Circulation
Yuki Yokota1, Yuto Tashiro1, Yusuke Suzuki1, Seishiro Tasaka1, Tomohumi Matsushita1, Keisuke Matsubara1, Mirei Kawagoe1, Takuya Sonoda1, Yasuaki Nakayama1, Satoshi Hasegawa1 and Tomoki Aoyama1*
1Depertment of Human Health Sciences, Graduate School of Medicine, Kyoto University, Kyoto, Japan
- *Corresponding Author:
- Dr. Tomoki Aoyama
Depertment of Human Health Sciences
Graduate School of Medicine, Kyoto University
53 Kawahara-cho, Shogoin,
Sakyo-ku, Kyoto 606-8507, Japan
Tel: +81-75-751-3952
Fax: +81-75-751-3909
E-mail: blue@hs.med.kyoto-u.ac.jp
Received date: December 09, 2016; Accepted date: December 24, 2016; Published date: January 01, 2017
Citation: Yokota Y, Tashiro Y, Suzuki Y, Tasaka S, Matsushita T, et al. (2017) Effect of Capacitive and Resistive Electric Transfer on Tissue Temperature, Muscle Flexibility, and Blood Circulation. J Nov Physiother 7: 325. doi:10.4172/2165-7025.1000325
Copyright: © 2017 Yokota Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Introduction: The differences between Capacitive and Resistive electric transfer (CRet) and hot pack (HP) in their effects on tissue temperature, muscle flexibility, and blood circulation are unknown. This study aimed to clarify the effect of CRet and HP on tissue temperature, muscle flexibility, and blood circulation. Methods: The participants were 13 healthy adults. They randomly performed three 15-minute interventions: (1) CRet, (2) HP, and (3) without powered CRet (sham). The intervention and measurement were applied to the right hamstring muscle. INDIBA® activ ProRecovery HCR902 was used in the CRet trial. The moist heat method was used in the HP trial. The measurement indexes were superficial temperature (ST), 10-mm deep temperature (DT), and 20-mm DT; the passive straight leg raise (SLR) test; and oxygenated (oxy), deoxygenated (deoxy), and total (total) hemoglobin (Hb) concentrations. Each index was measured for 30 minutes after the intervention and the amount of change (Δ) from the pre-intervention value was calculated. Results: ΔST, Δ10 mmDT, Δ20 mmDT, Δoxy-Hb, and Δtotal-Hb were significantly higher in the CRet and HP trials than in the sham trial for 30 minutes after the intervention (p<0.05). ΔSLR was significantly higher in the CRet trial than in the HP trial from 15 to 30 minutes after the intervention (p<0.01) Conclusion: Our results indicate that CRet is an efficient method for preventing and treating musculoskeletal injuries and improve muscle flexibility. In addition, it can improve blood circulation as well as HP can.
Keywords
Diathermy; Thermotherapy; Flexibility; Blood circulation
Introduction
Adequate muscle flexibility is an important physical ability because poor muscle flexibility increases the risk of various musculoskeletal injuries such as muscle strain and low back pain, which are common in athletes [1-6]. Thus, maintenance and improvement of muscle flexibility is important. In order to maintain and improve muscle flexibility, athletes and therapists use various methods such as stretching and thermotherapy. Many studies have reported the effect of thermotherapy combined with stretching on muscle flexibility, and they indicated that this combination is more effective for improving muscle flexibility than stretching alone [7-9]. However, it is unclear how thermotherapy alone influences muscle flexibility.
Thermotherapy is the therapeutic application of heat to the body resulting in increased tissue temperature [10]. By increasing tissue temperature, thermotherapy brings various benefits, including an increase in soft tissue extensibility [10]. This change in the physiological characteristics of muscle may lead to improve muscle flexibility. An increase in tissue temperature can also improve blood circulation by causing vasodilation [10]. Insufficient blood circulation causes hypoxic conditions in tissues, the production and release of algesic substances and tissue fibrosis, which lead to pain, muscle spasm, and joint contracture [11]. These conditions may reduce muscle flexibility. In addition, improvement of blood circulation can promote tissue repair and healing by supplying protein, nutrients, and oxygen at the injured site [12]. Thus, it is meaningful to evaluate the effect of thermotherapy on muscle flexibility and blood circulation to treat muscles.
Thermotherapy is usually classified into superficial and deep thermotherapy. In general, superficial thermotherapy increases temperature only in the skin and superficial tissue [10]. On the other hand, deep thermotherapy increases the temperature in deep tissue [10]. Heat conducted by superficial thermotherapy cannot reach muscle [10]. Earlier studies indicated that deep thermotherapy devices such as ultrasound and diathermy can increase the temperature at deep tissues more than superficial thermotherapy [13-15]. Draper et al. reported that increases in temperature at 30mm below the skin surface of the triceps surae muscle were 3.9°C after 15 minutes ultrasound intervention and 3.5°C after 20minutes pulsed short-wave diathermy intervention [13,14]. Therefore, deep thermotherapy seems more suitable for the treatment of muscle than superficial thermotherapy does.
As a method of superficial thermotherapy, hot packs (HP) are widely used in clinical practice because of their convenience. Recently, a Capacitive-Resistive electric transfer (CRet) system, which is one of the diathermy methods, has been developed as a form of deep thermotherapy [16]. This device delivers radiofrequency (RF) energy that passes between active and inactive electrodes, and generates heat in the human body [17-19]. CRet can treat larger area than ultrasound because CRet has no limit in treatment area unlike ultrasound, which can treat an area only twice the size of the ultrasound transducer. In addition, CRet does not require a polus and surface-cooling system because it uses 448 kHz, which is lower than conservative diathermy, as it does not cause excessive heat generation between the skin and the electrode. Thus CRet is more convenient and safer than other devices. A previous study revealed changes of skin temperature occurred using the device; however, the changes in deep tissue temperature and the direct physiological effect on changes in muscle flexibility and blood circulation were not shown [19]. In addition, the differences between CRet and HP in their effects on tissue temperature, muscle flexibility, and blood circulation are unknown. Thus, the aim of the present study was to evaluate the effects of CRet and HP on tissue temperatures, muscle flexibility, and blood circulation.
Materials and Methods
Participants
Thirteen health adults participated in this study (5 women and 8 men, mean ± standard deviation; age 22.0 ± 0.8 years, height 166.7 ± 0.1 cm, body weight 60.9 ± 9.9 kg, body mass index 21.8 ± 1.6 kg/m2). The participants were non-athletes, and did not currently perform any excessive exercise. Participants with a history of orthopedic or nervous system disease in their lower limbs were excluded. All participants were instructed not to consume alcohol and avoid smoking and performing intense activities at least 24 hours before the experiment. The study protocol was approved by the ethical committee of Kyoto University Graduate School of Medicine (the chairperson: Shinji Kosugi, the protocol number: C1150, the date of approval: February 16, 2016). After receiving an explanation of the study protocol, all participants provided informed consent.
We calculate the sample size needed for two-way analysis of variance (ANOVA) with repeated measures (effect size=0.40, α error = 0.05, power=0.8, number of groups=3, number of measurement=8) using G* power 3.1 software (Heinrich Heine University, Dusseldorf, Germany). The result showed that 13 subjects were required.
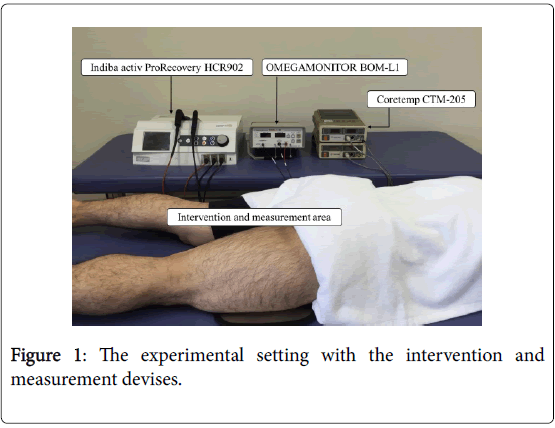
Design
The participants randomly received the following three interventions: (1) Capacitive and Resistive electric transfer (CRet trial), (2) hot pack (HP trial), and (3) CRet without power (sham trial). The intervention order was randomized, and each experiment was conducted more than 24 hours apart. The intervention and measurement were applied to the right hamstring muscle. We chose hamstring muscle as the target muscle because poor flexibility of hamstring muscle increase the risk of various musculoskeletal injuries [1-6] and hamstring injuries are common in athlete [3]. The participants were requested to lie in a prone position on a bed whilst receiving the intervention and measurement, with the right hamstring muscle exposed. The experiment was conducted in a controlled environment with the temperature maintained between 22 and 25 (Figure 1).
Instruments and measurements
Interventions: Indiba® activ ProRecovery HCR902 (Indiba S. A., Barcelona, Spain) was used for the CRet intervention. This device operates at a frequency of 448 kHz. A rigid, circular, metallic electrode with a diameter of 65 mm was used as the active electrode, and a large, flexible, rectangular metallic plate (measuring 200 × 260 mm) was used as the inactive electrode. It delivers RF energy in two modes as active electrodes: capacitive (CAP) and resistive (RES). The CAP electrode has a polyamide coating which acts as a dielectric medium, insulating its metallic body from the skin surface; therefore, it generates heat near the superficial skin of the body. The RES electrode is uncoated and passes RF energy directly through the body into the inactive electrode; therefore, it generates heat in the deep part of the body. There are several contraindications to CRet intervention, e.g. pregnancy, deep vein thrombosis, hypoesthesia, damaged skin, and implanted pacemaker. The participants underwent the intervention for 15 minutes (5 minutes in CAP and 10 minutes in RES). The active electrode was continually moved in the circular motion on the skin of posterior thigh and the inactive electrode was placed under the thigh. A manufacturer-supplied conductive cream was used as a coupling medium between the active electrode and the skin surface during the intervention. The intensity was defined as 6 or 7 on a subjective analog scale which is an 11-point, participant self-reported scale of thermal sensing (0: no thermal sensing, 10: worst possible thermal sensing). The duration and intensity of the CRet intervention were based on the manufacturer’s recommending method, which were considered to be the most effective without feeling discomfort or pain [19]. The sham intervention was unpowered CRet but otherwise performed using the same method and conditions as those in the CRet intervention. In the HP trial, 15 minutes of moist heat with an HP was applied to the participants. The HP (S-PACK: SAKAI Medical Co., Ltd., TOKYO, Japan) was heated to 80 in a hydro-collator tank (PACKWARMER CL-15: SAKAI Medical Co., Ltd., Tokyo, Japan) and wrapped in towels in eight layers. This intensity of the HP is considered to be most effective without feel discomfort or pain.
Measurement
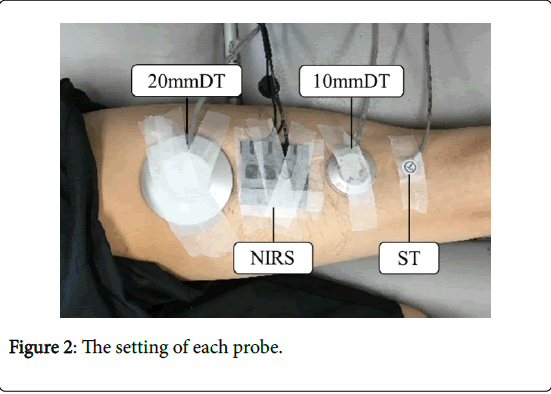
Tissue temperature was measured using a Coretemp CTM-205 (Termo Co., Ltd., Tokyo, Japan). This instrument is an electronic thermometer for noninvasive measurement of body temperature. We measured 3 depths (skin superficial temperature [ST], and deep temperatures [DT] 10 mm and 20 mm below the superficial skin) simultaneously. ST was measured with a thermistor probe, PD-K161, and DTs (10 mm DT and 20 mm DT) were measured with temperature-compensative probes, PD-11 and PD-51, which measure the temperature 10 mm and 20 mm below the skin surface, respectively. Each probe was attached with elastic tape to the skin on the hamstring muscle confirmed by palpation (Figure 2). The probes were attached by one therapist and placed in the same order.
The passive straight leg raise (SLR) test was used to determine changes in the hamstring muscle’s flexibility. Two therapists used a universal goniometer to measure the passive SLR. One therapist performed the passive SLR test by keeping the participants’ knee in full extension and the ankle in neutral plantar flexion-dorsiflexion. The second therapist placed the axis of the goniometer over a mark on the greater trochanter of the femur. The stationary arm of the goniometer was placed parallel to the bed and checked with a level, and the moving arm was placed in line between the head of the greater trochanter of the femur and the lateral epicondyle of the femur. In order to minimize errors, the landmarks where the axis and arm of goniometer were placed were confirmed by palpation. The degree of elevation of the straightened leg was recorded every 1 degree.
Blood circulation was measured with near-infrared spectroscopy (NIRS) using an OMEGAMONITOR BOM-L1 TR W (Omegawave Co., Ltd., Tokyo, Japan). This device’s two photo detectors absorb three wavelengths of light (780, 810, 830 nm) from a light source. The absorbance is analyzed using a modified version of the Lambert-Beer law, yielding a hemoglobin (Hb) content under the photo detectors. The two photo detectors were placed 15 mm and 30 mm away from the light source. The distance between the two detectors reflected the measurement depth. Thus, blood circulation around 15 mm below the skin surface was measured in this study. The measurement indexes of blood circulation were oxygenated (oxy-), deoxygenated (deoxy-), and total (total-) Hb concentrations. The total-Hb is the sum of oxy-Hb and deoxy-Hb. The NIRS probe was attached with elastic tape to the center of the belly of the right biceps femoris muscle, which is a component of the hamstring muscle, defined as the midpoint of the femur from the greater trochanter to the lateral epicondyle of the femur and confirmed with palpation (Figure 2). The placement of the NIRS probe was conducted by one therapist and the midpoint of femur was measured with a tape measure and marked by a pen.
Experimental procedure
The duration of the experiment was 50 minutes: 5 minutes before the intervention (rest), the 15-minute intervention, and 30 minutes after the intervention (rest). Tissue temperature, muscle flexibility, and blood circulation were measured 5 minutes before and 30 minutes after the intervention. Tissue temperature data were measured at 5- minute intervals (T1: before the intervention and T2-T8: after the intervention) and analyzed and compared among the trials. Muscle flexibility was measured before (T1), immediately after, 15 minutes after, and 30 minutes after the intervention (T2, T5, and T8), and the data were analyzed and compared among the trials. The blood circulation data were divided into 5-minute intervals, and the average of the 5-minute intervals were recorded (I1: before the intervention and I2-I7: after the intervention) (Figure 3).
ST and DT were measured one (T1) and seven times (T2 to T8) before and after the interventions, respectively. The NIRS measured changes in Hb during 10 minutes (I1) before the intervention in CRet, HP, and sham trial. Then the interventions for CRet, HP, and sham trials were performed for 15 minutes. After the interventions, the NIRS measurement was performed continuously for 30 minutes, and it was devided into six intervals; from 12 to 17. The passive SLR teast was performed one (T1) and three times (T2, T5, and T8) before the intervention, respectively.
Statistical analysis
For each index that was measured, the amount of change (Δ) from the first value was calculated and compared at each time point after the interventions in order to investigate how long the effects of each intervention last. Statistical analysis was performed using two-way analysis of variance (ANOVA) with 3 × 8 repeated measurement on the changes in ST/DT for comparisons among the trials. The changes of muscle flexibility were analyzed with two-way ANOVA with 3 × 4 repeated measurement. The changes in each Hb index were analyzed with two-way ANOVA with 3 × 7 repeated measurement. A Sidak post hoc multiple comparison test was performed to clarify the differences in detail among the three trials. The statistical analysis were performed using the SPSS version 20.0 (IBM Corp., Armonk, NY), with a significance threshold of 0.05 (Figure 4).
Results
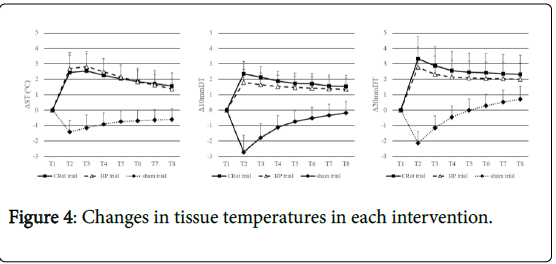
Changes in tissue temperatures
There was a significant interaction in ΔST (F=48.6, p<0.01), Δ10 mmDT (F=82.5, p<0.01), and Δ20 mmDT (F=50.5, p<0.01). The Sidak post hoc test revealed that ΔST, Δ10 mmDT and Δ20 mmDT were significantly higher in the CRet and HP trials than in the sham trial between T2 and T8 (ST, 10 mmDT: CRet, HP vs. sham T2 to T8 p<0.01, 20 mmDT: CRet vs. sham T2 to T6 p<0.01, T7, T8 p<0.05, HP vs. sham T2 to T7 p<0.01, T8 p<0.05). There were no significant differences between the CRet and HP trials in Δ10 mmDT and Δ20 mmDT; however, they tended to be higher in the CRet trial than in the HP trial between T2 and T8 (table 1).
| CRet trial | HP trial | Sham trial | ANOVA | ||
| ST | T1 | 0 | 0 | 0 | F=48.6 |
| T2 | 2.4 ± 1.1** | 2.7 ± 1.0†† | ?1.4 ± 0.7 | ||
| T3 | 2.5 ± 1.1** | 2.8 ± 1.0†† | ?1.2 ± 0.8 | ||
| T4 | 2.2 ± 1.1** | 2.5 ± 0.8†† | ?0.9 ± 0.7 | ||
| T5 | 2.0 ± 0.9** | 2.1 ± 0.8†† | ?0.7 ± 0.7 | ||
| T6 | 1.9 ± 0.9** | 1.8 ± 0.7†† | ?0.7 ± 0.7 | ||
| T7 | 1.7 ± 0.9** | 1.6 ± 0.7†† | ?0.6 ± 0.7 | ||
| T8 | 1.5 ± 0.9** | 1.4 ± 0.7†† | ?0.6 ± 0.7 | ||
| 10mmDT | T1 | 0 | 0 | 0 | F=82.5 |
| T2 | 2.3 ± 0.8** | 1.8 ± 0.9†† | ?2.7 1.1 | ||
| T3 | 2.1 ± 0.7** | 1.6 ± 0.8†† | ?1.8 ± 0.9 | ||
| T4 | 1.9 ± 0.7** | 1.5 ± 0.7†† | ?1.1 ± 0.8 | ||
| T5 | 1.7 ± 0.7** | 1.5 ± 0.7†† | ?0.8 ± 0.7 | ||
| T6 | 1.7 ± 0.7** | 1.4 ± 0.8†† | ?0.5 ± 0.7 | ||
| T7 | 1.6 ± 0.7** | 1.4 ± 0.8†† | ?0.3 ± 0.7 | ||
| T8 | 1.5 ± 0.7** | 1.3 ± 0.7†† | ?0.2 ± 0.7 | ||
| 20mmDT | T1 | 0 | 0 | 0 | F=50.5 |
| T2 | 3.3 ± 1.4** | 2.8 ± 1.3†† | ?2.1 ± 0.7 | ||
| T3 | 2.9 ± 1.3** | 2.3 ± 1.2†† | ?1.2 ± 0.8 | ||
| T4 | 2.6 ± 1.3** | 2.1 ± 1.1†† | ?0.5 ± 0.7 | ||
| T5 | 2.5 ± 1.3** | 2.1 ± 1.1†† | ?0.008 ± 0.7 | ||
| T6 | 2.4 ± 1.2** | 2.0 ± 1.1†† | 0.3 ± 0.8 | ||
| T7 | 2.4 ± 1.3* | 2.0 ± 1.1†† | 0.5 ± 0.8 | ||
| T8 | 2.3 ± 1.2* | 2.0 ± 1.0† | 0.7 ± 0.8 |
**p<0.01 CRet trial vs. sham trial; *p<0.05 CRet trial vs. sham trial; ††p<0.01 HP trial vs.sham trial; †p<0.05 HP trial vs. sham trial; The chronological changes in ST, 10mmDT, and 20mmDT in the CRet, HP and sham trials are shown. From T2 to T8, ST, 10mmDT, and 20mmDT were significantly higher in the CRet and HP trials than in the sham trial. No significant differences were observed between the CRet and HP trials.
Table 1: Changes in tissue temperatures in each intervention.
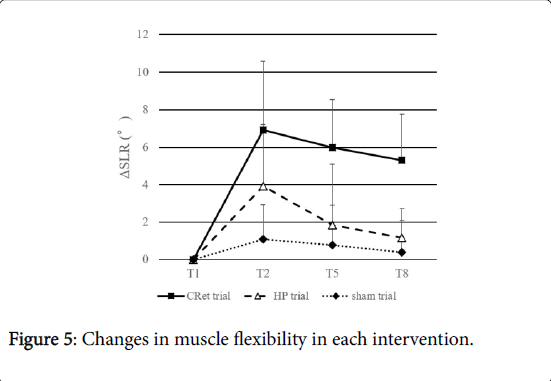
Changes in muscle flexibility
There was a significant interaction in ΔSLR (F=10.1, p<0.01). The Sidak post hoc test revealed that ΔSLR was significantly higher in the CRet trial than in the sham trial between T1 and T8 (p<0.01), moreover, it was significantly higher in the CRet trial than the HP trial between T5 and T8 (p<0.01). There was no significant difference between the HP and sham trials (Figure 5).
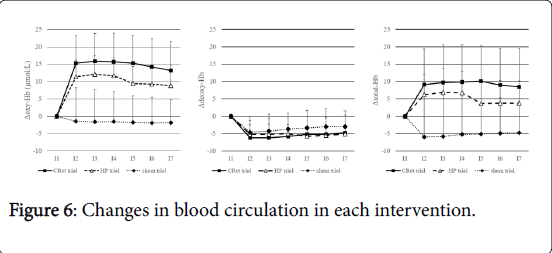
Changes in blood circulation
There was a significant interaction in Δoxy-Hb (F=12.2, p<0.01) and Δtotal-Hb (F=5.9, p<0.01). Δdeoxy-Hb did not differ significantly among the three trials. The Sidak post hoc test revealed that Δoxy-Hb and Δtotal-Hb were significantly higher in the CRet and HP trials than in the sham trial between I2 and I7 (oxy-Hb: CRet, HP vs. sham I2 to I7 p<0.01, total-Hb: CRet vs. sham I2 to I7 p<0.01, HP vs. sham I2, I5 to I7 p<0.05, I3,I4 p<0.01). In each trial, Δdeoxy-Hb tended to decrease after the intervention (Table 2).
| CRet trial | HP trial | Sham trial | ANOVA | |
| T1 | 0 | 0 | 0 | F=10.1 |
| T2 | 6.9 ± 3.7** | 3.9 ± 3.3 | 1.1 ± 1.8 | |
| T5 | 6.0 ± 2.5§ | 1.8 ± 3.2 | 0.8 ± 2.1 | |
| T8 | 5.3 ± 2.5§ | 1.2 ± 1.6 | 0.4 ± 1.7 |
**p<0.01 CRet trial vs. sham trial
§p<0.05 CRet trial vs. HP, sham trial
The chronological changes in the passive SLR test in the CRet, HP and sham trials are shown. From T2 to T8, the passive SLR test was significantly greater in the CRet trial than in the sham trial. Moreover, the passive SLR test at T5 and T8 was significantly greater in the CRet trial than in the HP trial. No significant difference was observed between the HP and sham trials.
Table 2: Changes in muscle flexibility in each intervention.
Discussion
We examined the effects of CRet and HP on muscle flexibility using the passive SLR test. The changes in the passive SLR test were significantly greater in the CRet trial than in the sham trial for 30 minutes after the intervention. This suggests that CRet could improve muscle flexibility. There are two possible factors for the change in muscle flexibility. The first factor is the increase in the extensibility of the soft tissue, including connective tissue composed primarily of collagen fibers [20-22] (Figure 6).
As the temperature increases, the collagen extensibility increases, and the connective tissue viscosity and viscoelasticity of muscle fiber are reduced [23-25]. Subsequently, the extensibility of soft tissue increased, and muscle flexibility was improved. The second factor is the increase in the participants’ tolerance to the pain from muscle stretching. Some previous studies reported that local thermotherapy increased the pain threshold [26,27,28]. This analgesic effect caused by thermotherapy is considered to be due to the gate control theory of pain proposed by Melzack and Wall [29]. According to the theory, pain perception is modulated in the dorsal column by competing inputs from large-diameter non-nociceptive Aβ nerves transmitting information from cutaneous thermal, mechanical or electrical stimulation, and smaller-diameter nociceptive Aδ nerves and C-nerves transmitting painful information [29]. The Aβ nerves activated by the thermal stimulation of the CRet intervention reduce the transmission of pain; therefore, the tolerance of pain from muscle stretching increased.
The changes in the passive SLR test were significantly greater in the CRet trial than in the HP trial 15 and 30 minutes after the intervention, and no significant difference was observed between the HP and sham trials for the 30 minutes after the intervention. These results suggest that CRet is more effective for improving muscle flexibility than HP. We assume that this phenomenon was due to the increase in deep tissue temperature. In the present study, the mean changes in temperature were 2.3 and 1.8 at 10 mm and 3.3 and 2.8 at 20 mm below the superficial skin immediately after the CRet and HP interventions, respectively. There was no significant difference between the CRet and HP trials in 10 mmDT and 20 mmDT; however, they tended to be higher in the CRet trial than in the HP trial for 30 minutes after the intervention. These results suggest that CRet could warm deep tissue more effectively than HP. HP is classified as superficial thermotherapy [10], and superficial heat modalities do not sufficiently raise the temperatures of deeper muscles [30]. Previous studies reported that HP did not increase the muscle flexibility and that short wave diathermy classified as deep thermotherapy, which is similar to CRet, was more effective for improving tissue extensibility than HP [31,32]. In the present study, the intervention and measurement were applied to the right hamstring muscle. The hamstring muscle is comprised of three muscles: the biceps femoris, semitendinosus, and semimembranosus [33]. The semimembranosus is situated deep to the biceps femoris and semitendinosus [33]. All of them influence the degree of the passive SLR test. We assumed that CRet could reach the whole hamstring muscle and warm not only the biceps femoris and semitendinosus but also the semimembranosus enough to change the degree of the passive SLR test; on the other hand, HP could not warm the deep muscle sufficiently. Thus, the change in the passive SLR was significantly greater in the CRet trial than in the HP trial. In other words, CRet is more effective for improving muscle flexibility than HP (Table 3).
| CRet trial | HP trial | Sham trial | ANOVA | ||
| Oxy-Hb | I1 | 0 | 0 | 0 | F=12.2 |
| I2 | 15.3 ± 8.0** | 11.4 ± 4.7†† | ?1.4 ± 9.6 | ||
| I3 | 15.9 ± 8.0** | 12.1 ± 5.4†† | ?1.6 ± 9.2 | ||
| I4 | 15.7 ± 8.2** | 11.7 ± 5.1†† | ?1.6 ± 8.7 | ||
| I5 | 15.3 ± 7.9** | 9.4 ± 4.9†† | ?1.7 ± 7.6 | ||
| I6 | 14.2 ± 8.1** | 9.3 ± 5.5†† | ?1.9 ± 7.4 | ||
| I7 | 13.2 ± 8.4** | 8.9 ± 5.7†† | ?1.8 ± 6.6 | ||
| Deoxy-Hb | I1 | 0 | 0 | 0 | n.s. |
| I2 | ?6.2 ± 5.0 | ?5.1 ± 2.7 | ?4.5 ± 4.4 | ||
| I3 | ?6.1 ± 5.6 | ?5.1 ± 2.8 | ?4.2 ± 4.8 | ||
| I4 | ?5.7 ± 5.0 | ?4.9 ± 2.6 | ?3.6 ± 4.6 | ||
| I5 | ?5.2 ± 5.1 | ?5.7 ± 2.8 | ?3.3 ± 5.1 | ||
| I6 | ?5.2 ± 4.8 | ?5.5 ± 2.9 | ?2.9 ± 5.3 | ||
| I7 | ?4.7 ± 5.1 | ?5.1 ± 2.4 | ?2.9 ± 4.6 | ||
| Total-Hb | I1 | 0 | 0 | 0 | F=5.9 |
| I2 | 9.1 ± 10.3** | 6.2 ± 5.9† | ?5.9 ± 11.8 | ||
| I3 | 9.7 ± 10.9** | 7.0 ± 6.7†† | ?5.8 ± 11.9 | ||
| I4 | 9.9 ± 10.7** | 6.8 ± 6.3†† | ?5.2 ± 11.1 | ||
| I5 | 10.1 ± 10.3** | 3.7 ± 6.1†† | ?5.1 ±10.2 | ||
| I6 | 9.0 ± 10.5** | 3.8 ± 6.5† | ?4.9 ± 10.2 | ||
| I7 | 8.4 ± 11.1** | 3.8 ± 6.4† | ?4.7 ± 9.1 |
Table 3: Changes in blood circulation in each intervention.
The present study revealed that the changes in total-Hb were significantly greater in the CRet and HP trials than in the sham trial for 30 minutes after the intervention. Oxy-Hb, which is a component of total-Hb, increased in the CRet and HP trials, whereas the deoxy-Hb decreased. This result shows that the change in total-Hb was due to the increase in oxy-Hb. An increase in oxy-Hb indicates an increase in the volume of fresh blood supplied by the arteries [34]. The mechanism of thermal effects improving blood circulation can be attributed to the direct reflective activation of vascular smooth muscles via skin temperature receptors, suppression of the sympathetic nerve system through indirect activation of local spinal reflexes, and increases in the local release of inflammatory chemical mediators such as histamine and prostaglandin, and the compound effect would result in vasodilation and increase in blood flow [35,36]. Some previous studies reported that blood circulation was improved by thermotherapy techniques such as ultrasound, shortwave diathermy, and HP [11,34,37]. These studies concluded that increases in tissues temperature caused vasodilation; hence, blood circulation was improved. In our study, the blood circulation was improved after intervention with both CRet and HP. Therefore, the present study agrees with those previous studies.
The results of this study indicated that CRet improved muscle flexibility. Maintenance and improvement of muscle flexibility is the key to prevent and treat musculoskeletal injuries. Various studies have investigated the effect of thermotherapy on muscle flexibility; however, many of them reported the effect of thermotherapy applied concomitantly with stretching [7-9]. In contrast, the present study indicated that CRet alone could improve muscle flexibility. However, further studies should compare the effect of combined CRet and stretching on muscle flexibility.
The present study had some limitations. First, the intensity of CRet intervention was determined using a subjective analog scale. Thus, the amount of increased temperature due to the difference of applied energy is unknown. Further experiments using various intensities of the CRet intervention is needed. Second, the measurement time was limited. In the present study, the changes in ST, 10 mmDT, 20 mmDT, oxy-Hb, and total-Hb were significantly greater in the CRet and HP trials than in the sham trial, and the changes in the passive SLR were greater in the CRet trial than in the sham trial for the 30 minutes after the interventions. However, it is unknown how long the effects of CRet last. A prolonged effect after more than 30 minutes should be researched. Third, we could not objectively conclude whether the changes in muscle flexibility were due to the increase in soft tissue extensibility or the increase in the participants’ tolerance to the pain from muscle stretching because we did not measure the physiological index which objectively reflect soft tissue extensibility such as muscle length and stiffness and the participants’ subjective pain sensation such as visual analog scale. Fourth, it is unclear that how deeply CRet conducts heat and affects the deeper tissue because we did not measure deeper tissue temperature than 20 mm deep. Despite these limitations, the results of the present study provide valuable information on the effects of CRet.
Conclusions
The effect on muscle flexibility was higher in the CRet trial than in the HP trial. Additionally, CRet could improve the blood circulation as well as HP. The findings of this study suggest that CRet could be an effective means as thermotherapy.
Acknowledgement
We would like to thank to the students of the Human Health Sciences as Kyoto University for their help with data collection.
References
- Feldman DE, Shrier I, Rossignol M, Abenhaim L (2001) Risk factors for the development of low back pain in adolescence. Am J Epidemiol 154: 30-36.
- Witvrouw E, Danneels L, Asselman P, D'Have T, Cambier D (2003) Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players. A prospective study. Am J Sports Med 31: 41-46.
- Worrell TW, Perrin DH (1992) Hamstring muscle injury: the influence of strength, flexibility, warm-up, and fatigue. J Orthop Sports Phys Ther 16: 12-18.
- Bradley PS, Portas MD (2007) The relationship between preseason range of motion and muscle strain injury in elite soccer players. J Strength Con Res 21:1155-1159.
- Kujala UM, Salminen JJ, Taimela S, Oksanen A, Jaakkola L (1992) Subject characteristics and low back pain in young athletes and nonathletes. Med Sci Sports Exerc 24: 627-632.
- Mierau D, Cassidy JD, Yong-Hing K (1989) Low-back pain and straight leg raising in children and adolescents. Spine (Phila Pa 1976) 14: 526-528.
- Draper DO, Anderson C, Schulthies SS, Ricard MD (1998) Immediate and residual changes in dorsiflexion range of motion using an ultrasound heat and stretch routine. J Athl Train 33: 141-144.
- Draper DO, Castro JL, Feland B, Schulthies S, Eggett D (2004) Shortwave diathermy and prolonged stretching increase hamstring flexibility more than prolonged stretching alone. J Orthop Sports Phys Ther 34: 13-20.
- Nakano J, Yamabayashi C, Scott A, Reid WD (2012) The effect of heat applied with stretch to increase range of motion: a systematic review. Phys Ther Sport 13: 180-188.
- Cameron MH (2009) Physical Agents in Rehabilitation from Research to Practice, (4th edn) Philadelphia, PA: Saunders.
- Morishita K, Karasuno H, Yokoi Y, Morozumi K, Ogihara H, et al. (2014) Effects of therapeutic ultrasound on intramuscular blood circulation and oxygen dynamics. J Jpn Phys Ther Assoc 17: 1-7.
- Nadler SF, Weingand K, Kruse RJ (2004) The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain Physician 7: 395-399.
- Draper DO, Harris ST, Schulthies S, Durrant E, Knight KL, et al. (1998) Hot-Pack and 1-MHz Ultrasound Treatments Have an Additive Effect on Muscle Temperature Increase. J Athl Train 33: 21-24.
- Draper DO, Knight K, Fujiwara T, Castel JC (1999) Temperature change in human muscle during and after pulsed short-wave diathermy. J Orthop Sports Phys Ther 29: 13-18.
- Lehmann JF, Stonebridge JB, deLateur BJ, Warren CG, Halar E (1978) Temperatures in human thighs after hot pack treatment followed by ultrasound. Arch Phys Med Rehabil 59: 472-475.
- Kato S, Saitoh Y, Miwa N (2013) Repressive effects of a capacitive-resistive electric transfer (CRet) hyperthermic apparatus combined with provitamin C on intracellular lipid-droplets formation in adipocytes. Int J Hypothermia 29:30-37.
- Hernandez-Bule ML, Paino CL, Trillo MA, Ubeda A (2014) Electric stimulation at 448 kHz promotes proliferation of human mesenchymal stem cells. Cell Physiol Biochem 34:1741-1755.
- Osti R, Pari C, Salvatori G, Massari L (2015) Tri-length laser therapy associated to tecar therapy in the treatment of low-back pain in adults: a preliminary report of a prospective case series. Lasers Med Sci 30: 407-412.
- Kumaran B, Watson T (2015) Thermal build-up, decay and retention responses to local therapeutic application of 448kHz capacitive resistive monopolar radiofrequency: A prospective randomised crossover study in healthy adults. Int J Hyperthermia 31:883-895.
- Lehmann JF, Warren CG, Scham SM (1974) Therapeutic heat and cold. Clin Orthop Relat Res: 207-245.
- Strickler T, Malone T, Garrett WE (1990) The effects of passive warming on muscle injury. Am J Sports Med 18: 141-145.
- Lentell G, Hetherington T, Eagan J, Morgan M (1992) The use of thermal agents to influence the effectiveness of a low-load prolonged stretch. J Orthop Sports Phys Ther 16: 200-207.
- Mutungi G, Ranatunga KW (1998) Temperature-dependent changes in the viscoelasticity of intact resting mammalian (rat) fast- and slow-twitch muscle fibres. J Physiol 508:253-265.
- Lehmann JF, Masock AJ, Warren CG, Koblanski JN (1970) Effect of therapeutic temperatures on tendon extensibility. Arch Phys Med Rehabil 51: 481-487.
- Warren CG, Lehmann JF, Koblanski JN (1976) Heat and stretch procedures: an evaluation using rat tail tendon. Arch Phys Med Rehabil 57: 122-126.
- Lehmann JF, Brunner GD, Stow RW (1958) Pain threshold measurements after therapeutic application of ultrasound, microwaves and infrared. Arch Phys Med Rehabil 39: 560-565.
- Benson TB, Copp EP (1974) The effects of therapeutic forms of heat and ice on the pain threshold of the normal shoulder. Rheumatol Rehabil 13: 101-104.
- Minton J (1993) 1992 Student Writing Contest-1st Runner-up: A Comparison of Thermotherapy and Cryotherapy in Enhancing Supine, Extended-leg, Hip Flexion. J Athl Train 28: 172-176.
- Melzack R, Wall PD (1965) Pain mechanisms: a new theory. Science 150: 971-979.
- Abramson DI, Mitchell RE, Tuck S Jr, Bell Y, Zays AM (1961) Changes in blood flow, oxygen uptake and tissue temperatures produced by the topical application of wet heat. Arch Phys Med Rehabil 42: 305-318.
- Taylor BF, Waring CA, Brashear TA (1995) The effects of therapeutic application of heat or cold followed by static stretch on hamstring muscle length. J Orthop Sports Phys Ther 21:283-286.
- Robertson VJ, Ward AR, Jung P (2005) The effect of heat on tissue extensibility: a comparison of deep and superficial heating. Arch Phys Med Rehabil 86: 819-825.
- Koulouris G, Connell D (2005) Hamstring muscle complex: an imaging review. Radiographics 25: 571-586.
- Karasuno H, Morozumi K, Fujiwara T (2005) Change in intramuscular blood volume induced by continuous shortwave diathermy. J Phys Ther Sci 17:71-79.
- Crockford GW, Hellon RF, Parkhouse J (1962) Thermal vasomotor responses in human skin mediated by local mechanisms. J Physiol 161: 10-20.
- Kellogg DL Jr, Liu Y, Kosiba IF, O'Donnell D (1999) Role of nitric oxide in the vascular effects of local warming of the skin in humans. J Appl Physiol 86: 1185-1190.
- Okada K, Yamaguchi T, Minowa K, Inoue N (2005) The influence of hot pack therapy on the blood flow in masseter muscles. J Oral Rehabil 32: 480-486.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 6785
- [From(publication date):
February-2017 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 5517
- PDF downloads : 1268