Research Article Open Access
Effect of Antifungal Drugs against Candida Isolates from Diabetic Women with Vaginitis
Rajalakshmi R1*, Sangeetha D1 and Udhaya V2
1Department of Microbiology, Faculty of Science, Annamalai University, Annamalai Nagar, Tamil Nadu, India
2Department of Medical Microbiology, Faculty of Medicine, Rajah Muthiah Medical College & Hospital, Annamalai University, Annamalai Nagar, Tamil Nadu, India
- *Corresponding Author:
- Rajalakshmi Ramachandran
Department of Microbiology, Annamalai University
Annamalai Nagar, Tamil Nadu, India
E-mail: rajalakshmi8478@gmail.com
Received date: July 31, 2017; Accepted date: August 14, 2017; Published date: August 17, 2017
Citation: Rajalakshmi R, Sangeetha D, Udhaya V (2017) Effect of Antifungal Drugs against Candida Isolates from Diabetic Women with Vaginitis. J Infect Dis Ther 5:331. doi: 10.4172/2332-0877.1000331
Copyright: © 2017 Rajalakshmi R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Diseases & Therapy
Abstract
Vaginitis is an inflammation of the vagina characterized by a whitish or whitish gray discharge, often with a curd-like appearance, odor, itching and irritation. Yeasts are always present in the vagina in small numbers, and symptoms only appear with overgrowth. The vaginal swab specimens were collected from the diabetic women with signs and symptoms of vaginitis. The isolated Candida species were identified by the morphological and cultural characteristics. The isolated and identified Candida strains were included C. albicans, C. dubliniensis, C. krusei, and C. tropicalis from diabetic women with signs and symptoms of vaginitis. The isolates were subjected to determine the in vitro anticandidal activity against antifungal drugs. All Candida strains isolated from diabetic women with vaginitis were 100% sensitive to Amphotericin-B and C. krusei strains showed 100% sensitivity to ketaconazole drug. Overall 32% of Candida strains showed multidrug resistance against the antifungal drugs we used.
Keywords
Antifungal drugs; Candida; Germ tube production; Multidrug resistance; Vaginitis
Introduction
Vaginitis, also known as vaginal infection and vulvovaginitis, is an inflammation of the vagina and possible vulva. It can result in discharge, itching, and pain, and is often associated with an irritation or infection of the vulva. The discharge may be excessive in amounts or abnormal in color (such as yellow, gray, or green). One of the problems of women with diabetes is resistant vulvovaginitis, which is related to some factors such as hyperglycemia, allergy, and atopy. Diabetes is a known predisposing factor of vulvovaginal candidiasis, primarily because of hyperglycemia-induced alterations, including decreased random motion of neutrophils, chemotaxis, phagocytosis, and microbial killing. In addition, increased glucose levels in genital tissues enhance yeast adhesion and growth. Several factors are associated with increased symptomatic infection in women, including pregnancy, iron deficiency anaemia, uncontrolled diabetes mellitus, and the use of oral contraceptives or antibiotics [1,2]. Diabetes is a proven predisposing factor for vulvovaginal candidiasis, along with pregnancy, use of broad – spectrum antibiotics, high- estrogen-dose oral contraceptives, obesity and drug addiction [3]. Symptomatic vulvovaginal candidal infections have been shown to be more prevalent in patients with diabetes than in the general population [4] and are usually attributed to “yeast infection” by the women themselves [5].In clinical settings, candidiasis is commonly treated with antimycotics-the antifungal drugs commonly used to treat candidiasis are topical clotrimazole, topical nystatin, fluconazole, and topical ketoconazole. It is possible for Candida albicans to develop a resistance to the drugs used to treat it, as seen from research done involving fluconazole, one of the drugs that is used to treat candidiasis and noted about the emergence of fluconazole resistant Candida species and quite remarkable percentage of yeasts and molds developed multidrug resistance [6]. In this study, the effect of antifungal drugs against Candida isolates from diabetic women with vaginitis was assessed.
Materials and Methods
Selection criteria
The inclusion criteria for the study, Patients with signs and symptoms of diabetic women (n=170) and Non diabetic normal healthy women without any signs and symptoms of vaginitis as control (n=50) were selected and took part in this study.
Specimen collection and transportation
The vaginal swab specimens were collected from the diabetic women with signs and symptoms of vaginitis. The specified routine procedure was followed; two vaginal swabs were collected from the posterior fornix of the vagina. One swab was used for smear preparation for gram staining and 10% KOH examination and the second swab were used for culture. Care was taken to avoid the collection of specimen from the diabetic women undergone any prior antibiotic therapy for atleast one week. The samples were safely transported to the laboratory under aseptic conditions for further proceedings.
Direct microscopic examination
10% KOH wet mount: A small portion of vaginal specimen was placed on clean glass slide, one or two drops of 10% Potassium hydroxide (KOH) solution was added and allowed to stand after 10-15 minutes and then examined for the presence of budding yeasts with or without pseudohyphae.
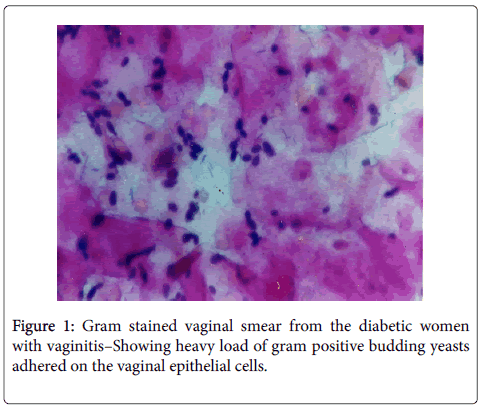
Gram stain: The smear made on the glass slide was allowed for air and heat fixation and submitted for gram staining procedure. Presence of gram-positive budding yeasts with or without pseudohyphae, number/grades of the yeast cells and the adherence pattern of the yeast cells on the epithelial cells were noted and recorded.
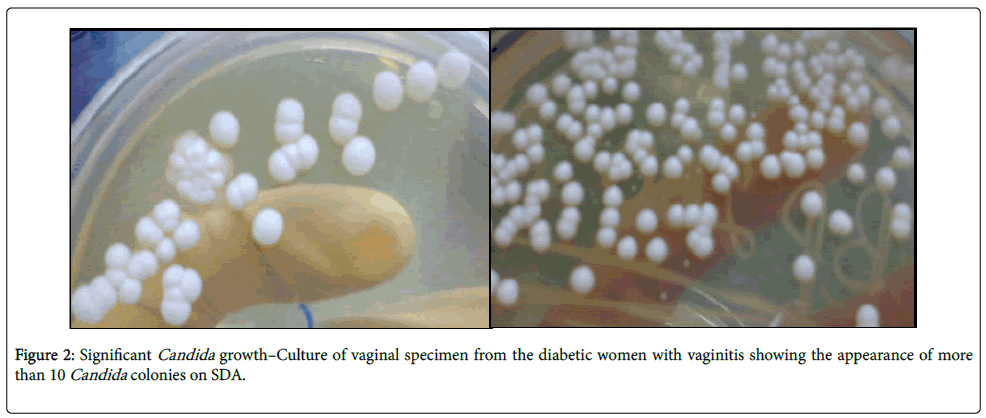
Isolation of Candida
The Vaginal specimen collected from the diabetic patients and normal healthy women were cultured on Sabouraud’s Dextrose Agar (SDA) with antibiotic Chloramphenicol (50µg/ml) and incubated at 37°C for one week. Candida growth on Sabouraud’s Dextrose Agar (SDA) was examined from second day onwards and recorded.
Identification of Candida species
The isolated Candida species were identified by the routine methods [7] i.e., Colony morphology in Sabouraud’s Dextrose Agar (SDA), Growth characteristics in Sabouraud’s Dextrose Broth (SDB), Germ tube production, Chlamydospore formation on corn meal agar, Sugar fermentation and Sugar assimilation [7-11]. The isolated and identified Candida strains from the patients and controls were included C. albicans, C. dubliniensis, C. krusei, and C. tropicalis were subjected to determine the in vitro anticandidal activity of antifungal drugs.
In vitro antifungal drug susceptibility testing
Inoculum preparation: Candida species/strains inoculum was prepared by suspending several colonies of grown cultures on Sabouraud’s Dextrose Agar (SDA) in phosphate buffered saline pH 7.2. Inoculum standardization was done using standard procedure in which the fungal suspensions were adjusted spectrophotometrically to an absorbance of 0.6 at 530 nm, which corresponds with the 0.5 McFarland standards.
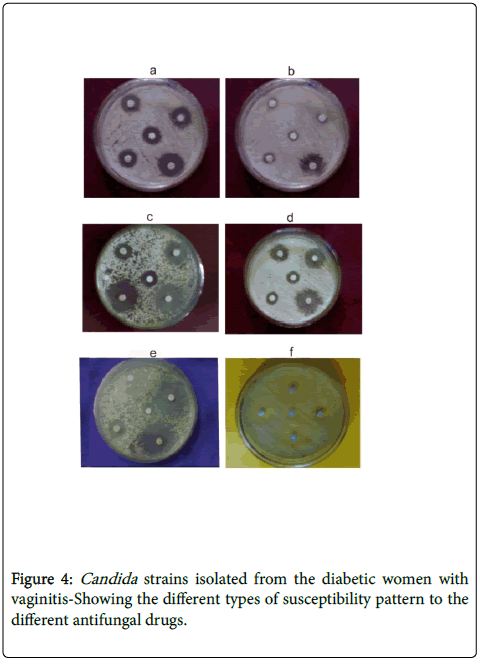
Disk diffusion method: The commercially available following antifungal discs were Clotrimazole, Ketaconazole. Fluconazole, Nystatin and Amphotericin-B were used in this study. Each SDA plate was inoculated with the standard inoculum suspensions by soaking a swab and rotating it over the agar plate. The antifungal discs were placed over the inoculated agar. After 48 hours of incubation at 31°C zone of inhibition of growth was measured and recorded. A duplicate was also carried out [7]. The Candida strains resistant to four or more antifungal drugs were considered as multidrug resistant strains.
Results
Direct microscopic examination
10% KOH wet mount examination: All 170 (100%) vaginal specimens of patients showed the presence of either budding yeasts alone or with pseudohyphae. Only 15 (30%) of control specimens showed only budding yeasts.
Gram staining: Among 170 patients vaginal specimens, 85% (n=145) of them showed gram positive budding yeasts heavily adhered on vaginal epithelial cells (Figure 1) and 9% (n=15) of the smear showed the presence of pseudohyphae along with the gram positive budding yeasts and 6% (n=10) of the smear showed less number of yeast cells adhered on vaginal epithelial cells. Only 12% (n=6) of the vaginal smear of the controls showed the presence of gram positive budding yeasts (rare cells) without pseudohyphae and non-adherent to the vaginal epithelial cells.
Culture results
All the 170 patients vaginal specimens yielded 100% Candida growth whereas only 24% (n=12) k growth observed in the control specimens (50).
Significant and insignificant Candida growth
All 170 vaginal samples from patients yielded 100% significant Candida growth (more than 10 colonies) on SDA (Figure 2). Among 50 control specimens, 24% (n=12) yielded Candida growth on SDA. Among which 8% (n=4) showed significant Candida growth, 16% (n=8) showed insignificant Candida growth (less than 10 colonies) and 76% (n=38) showed no growth.
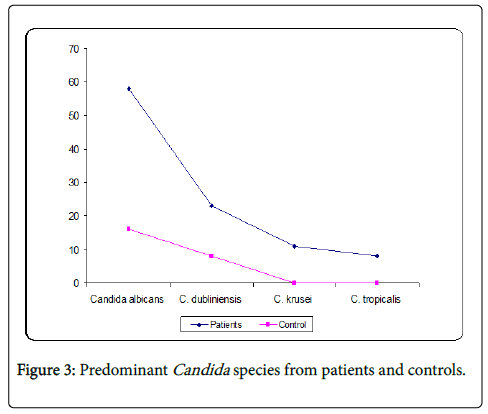
Predominant Candida species identification
The isolated Candida strains from patients were identified as Candida albicans (58%), Candida dubliniensis (23%), Candida krusei (11%) and Candida tropicalis (8%). Candida strains isolated from controls were identified as C. albicans (16%) and C. dubliniensis (8%) (Figure 3).
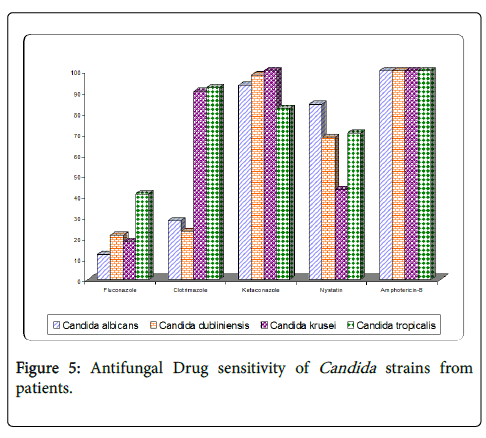
Antifungal drug sensitivity test
Totally 170 Candida strains (different species) from patients and 50 strains from healthy controls were subjected to anti-fungal sensitivity test. Out of 170 Candida strains, 26% (n=45) of them showed resistance to more than three or four anti-fungal drugs used (Figure 4). C. albicans (n=12) 12%, C. dubliniensis (n=24) 60%, C. krusei (n=6) 33%, C. tropicalis (n=3) 21%, showed multidrug resistance to five antifungal drugs used. All Candida species/ strains isolated from diabetic women with vaginitis were 100% sensitive to Amphotericin-B and C. krusei strains (all) showed 100% sensitivity to ketaconazole drug (Table 1 and Figure 5). Overall 32% of Candida strains showed multidrug resistance against the antifungal drugs we used.
| S.No | Candida isolates n=170 |
Antifungal drugs | ||||
|---|---|---|---|---|---|---|
| Fluconazole | Clotrimazole | Ketaconazole | Nystatin | Amphotericin-B | ||
| 1. | C. albicans (n=98) | 12% S | 28% S | 93% S | 84% S | 100% S |
| 2. | C. dubliniensis (n=40) | 21% S | 23% S | 98% S | 68% S | 100% S |
| 3. | C. krusei (n=18) | 18% S | 90% S | 100 % S | 43% S | 100% S |
| 4. | C. tropicalis (n=14) | 41% S | 92% S | 82% S | 70% S | 100% S |
Table 1: Antifungal drug sensitivity tests of Candida isolated from the diabetic women with signs and symptoms of vaginitis.
Discussion
Candidiasis is the general term used to indicate the different types of Candida infections and the vaginal candidiasis is the condition in which the Candida involves and cause vaginitis. Hyperglycemia is the major cause of increased susceptibility of the diabetic patients to vulvovaginal candidiasis. In our study all (100%) vaginal specimens showed either budding yeasts or budding yeasts with pseudohyphae. This indicates the association of Candida in vaginitis and the presence of pseudohyphae indicates the diseased status of the patients and the involvement of the Candida in vaginitis. It has been published that the production of germ tube and the pseudomycelium is due to the virulent and pathogenic nature of the Candida [6].
Udhaya et al. in their study note that the only 78% of the vaginal specimens (collected from the cancer cervix cases) and yielded Candida growth on SDA. But in our study we could able to get different results that, all vaginal specimens (100%) yielded Candida growth on SDA. Our result gains the support of the earlier publications that it is not uncommon the presence and the colonization of these Candida yeasts in the hyperglycemic conditions [12-17]. And the earlier study of Janani et al. confirms and supports our result evidently that she could able to isolate 100% Candida growth from the vaginal specimens of the asymptomatic diabetic women.
Janani et al. stated that the Candida strains isolated from asymptomatic diabetic women with vaginal candidiasis showed 57% of them resistance to more than three or four antifungal drugs used. C. albicans (92%) showed multidrug resistance. C. krusei (33%) and C. dubliniensis (42%) showed multidrug resistance. But our study result indicates that the C. albicans (12%), C. dubliniensis (60%), C. krusei (33%) and C. tropicalis (21%) showed the multidrug resistance against the antifungal drugs we used. It was quite obvious to note that the resistance towards clotrimazole and fluconazole was seems to be more when compare to other antifungal drugs we used (Table 1). There was another distinguishable result, we obtained that all C. krusei strains were sensitive to the drug ketaconazole (100%) (Table 1).
In our study, we also state that all vaginal specimens of the diabetic women with vaginitis yielded 100% significant Candida growth and the predominating species noted were C. albicans (58%) and 32% of multidrug resistance was noted to the multidrug resistant Candida strains. Most study data indicates that overall yeast carriage and infection rates increase in diabetes patients and correlate with degree of glucose control. Thus, good control of blood glucose and treatment with an appropriate antifungal agent are important in the management of vaginal candidal infections in diabetic women. Because most of the oral and topical azoles used to treat vulvovaginitis result in comparable efficacy rates, selection of therapy should be based on factors such as causative organisms, safety and side effects, the potential for drug interactions, and patient preferences.
Since the risk of infection and healing process with diabetic patients are more, the prophylactic measures and frequent assessment of the therapy regimen is seems to be much more essential. For which the regular and revised study of the antibiotic or antimicrobial sensitivity is essential. And to overcome the problem of multidrug resistance, the search for the new antimicrobial is also need in this field.
Summary and Conclusion
Totally 220 vaginal swabs were collected from the patients and controls were subjected in this study and categorized as diabetic women with signs and symptoms of vaginitis – 170 and non-Diabetic normal healthy women without signs and symptoms of vaginitis – 50. 100% of the diabetic women yielded Candida growth whereas only 24% of non-diabetic normal healthy women vaginal specimen yielded Candida growth on SDA. Significant Candida growth (more than 10 Candida colonies) was obtained from the both diabetic women with vaginitis and non-diabetic normal healthy women. Candida strains isolated from the patients were identified as Candida albicans (58%), Candida dubliniensis (23%), Candida krusei (11%) and Candida tropicalis (8%) and in controls the isolated Candida strains were identified as Candida albicans (16%) Candida dubliniensis (8%). Among the Candida species isolated, Candida albicans (58%) and Candida dubliniensis (23%) was the predominant Candida species isolated from the diabetic women with signs and symptoms of vaginitis.
All Candida species/strains isolated from diabetic women with vaginitis were 100% sensitive to Amphotericin-B and C.krusei strains (all) showed 100% sensitivity to ketaconazole drug. Overall 68% of Candida strains isolated from the diabetic women with vaginitis shown sensitivity towards antifungal drugs and 32% showed multidrug resistance against antifungal drugs we used.
References
- Fidel PL (2002) “Immunity to Candida”. Oral Dis 8: 69-75.
- Pappas PG (2006) “Invasive candidiasis”. Infect Dis Clin North Am 20: 485-506.
- Sobel JD (1993) Candidal vulvovaginitis. Clin Obset Gynecol 36: 153-165.
- Scudamore JA, Tooley PJ, Allcorn RJ (1992) The treatment of acute and chronic vaginal candidiasis. Br J Clin Pract 46: 260-263.
- Kalpan W, Kaufman L (1967) Sabouraudiz 1: 137.
- Udhaya V (2001) Role of Candida in Cervical Cancer - Association and Characterization of Candida, immuno diagnosis of Vaginal/cervical Candidiasis and anticandidal activity of certain medicinal plants.
- Abi-Said D, Anaissie E, Uzun O, Raad I, Pinzcowski H, et al. (1997) The epidemiology of hematogenous candidiasis caused by different Candida species. Clin Infect Dis 24: 1122-1128.
- Anil S, Samaranayake LP (2002) Impact of lysozyme and lactoferrin on oral Candida isolates exposed to polyene antimycotics and fluconazole. Oral Dis 2002 8 : 199-206.
- Baily GG, Moore CB, Essayag SM, De Wit S, Burnie JP, et al. (1997) Candida inconspicua, a fluconazole- resistant pathogen in patients infected with human immunodeficiency virus. Clin Infect Dis 25:161-163.
- Balbi C, Ajello DM, Balbi GC (1986) Treatment with ketoconazole in diabetic patients with vaginal candidiasis. Drug Exp Clin Res 12: 413-414.
- Bodey GP (1966) Fungal infections complicating acute leukemia. J Chron Dis 19: 667-687.
- Bodey G, Bueltmann B, Duguid W, Gibbs D, Hanak H, et al. (1992) Fungal infections in cancer patients: An international autopsy survey. Eur J Clin Microbiol Infect Dis 11: 99-109.
- Donders GG, Prenen H, Verbeke G, Reybrouck R (2002) Impaired tolerance for glucose in women with recurrent vaginal candidiasis. Am J Obstet Gynecol 187: 989-993.
- Fleury FJ (1982) Recurrent candidal vulvovaginitis. Chemotherapy 28: 48-54.
- Gibb D, Hockey S, Brown L, Lunt H (1995) Vaginal symptoms and insulin- dependent diabetes mellitus. N Z Med J 108: 252-253.
- Nyirjesy P, Peyton C, Weitz MV, Mathew L, Culhane JF, et al. (2006) Causes of chronic vaginitis: analysis of prospective database of affected women. Obstet Gynecol 108: 1185-1191.
- Rowe BR, Logan MN, Farrell I, Barnett AH (1990) Is candidiasis the true cause of vulvovaginal irritation in women with diabetes mellitus?. J Clin Pathol 43: 644-645.
Relevant Topics
- Advanced Therapies
- Chicken Pox
- Ciprofloxacin
- Colon Infection
- Conjunctivitis
- Herpes Virus
- HIV and AIDS Research
- Human Papilloma Virus
- Infection
- Infection in Blood
- Infections Prevention
- Infectious Diseases in Children
- Influenza
- Liver Diseases
- Respiratory Tract Infections
- T Cell Lymphomatic Virus
- Treatment for Infectious Diseases
- Viral Encephalitis
- Yeast Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 4487
- [From(publication date):
August-2017 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 3637
- PDF downloads : 850