Effect of an Educational Program concerning Oral Assessment and Healthcare on Nurses’ Performance of Oral Health Checkups in a Hospital.
Received: 12-Dec-2017 / Accepted Date: 27-Dec-2017 / Published Date: 10-Jan-2018 DOI: 10.4172/2332-0702.1000232
Abstract
Objectives: The purpose of this study was to investigate the effect of a group-based educational program on the awareness, attitudes, and confidence of nurses in the performance of oral health checkups.
Materials and methods: The subjects (n=184) were nurses who worked in a hospital and an affiliated long-term care facility in Fukuoka Prefecture, Japan. The subjects were divided to an intervention group and a control group. The intervention group participated in the program, which was a combination of a lecture and training program on oral assessment and oral healthcare. To investigate the effect of the program on their awareness, attitudes, confidence, and performances of oral health checkups, questionnaire surveys were conducted before and one month after the intervention.
Results: Sixty-two nurses participated in the program. Fifty-five (88.7%) in the intervention group and 68 (84.0%) in the control group who completed both surveys were employed for the analysis. In the intervention group, there were significant differences between the baseline and follow-up in their awareness of detecting oral cancer and confidence in examining oral cleanliness (p<0.05). However, there were no positive changes in their attitudes toward and performance of oral health checkups in either group.
Conclusion: These results suggest in addition to the continuous participation of nurses in the program, the introduction of oral assessment tools into their oral healthcare protocols might be needed to promote the performance of oral health checkups in their facilities. We believe that these findings will help promote the performance of oral health checkups in hospitals and long-term care facilities.
Keywords: Oral health checkup; Oral assessment; Oral health education
Introduction
In Japan, as in many countries, the population is aging. The population ≥ 65 years of age have been growing rapidly in recent decades; it was 26.0% in 2014 and will approach 40% by 2055. In addition, the number of elderly patients who require long-term care almost doubled from 2.2 million in 2000 to 4.2 million in 2014.
The percentage of Japanese older adults aged 80 years who have 20 or more of their own teeth increased from 40.2% in 2011 to 51.2% in 2016. However, the prevalence of caries and periodontal disease in older adults also increased. Therefore, it is expected that the number of older adults with dental problems will increase in the future. However, there are many barriers to providing routine oral care to frail older adults because of their impaired mobility, illness, economic status, and poor access to dental services [1,2].
Regular oral health checkups are important for detecting earlystage oral diseases, providing dental health services, and maintaining oral health [3]. In Japan, there are 7,251 long-term care facilities for elderly individuals requiring long-term care, and the estimated number of elderly inpatients in medical institutes was approximately 902,000 in 2014. A previous study in Japan reported that the oral health status of older adults who lived in long-term care facilities was very poor [4,5]. Therefore, it may be important for older adults in those facilities to receive oral health checkups and dental health services.
However, it may be difficult for dentists to regularly perform oral health checkups in facilities without a dental department. A previous survey in Japan reported that only 26.8% of hospitals in 1,952 hospitals have a dental department [6]. The inability to perform regular oral health checkups for elderly people may be a major barrier to the provision of appropriate dental services to them.
To resolve this problem, healthcare workers such as nurses, who usually provide medical care for elderly patients, will play an important role in performing regular oral health checkups. Nurses can be a good bridge for referring elderly patients with oral problems to appropriate oral health services. If nurses’ performance of oral health checkups can be developed, there will be more opportunities for oral health professionals to provide oral health services to frail older patients in these facilities. In addition, nurses’ performance of oral health checkups is necessary for elderly patients who cannot afford dental examinations by dentists, who live in areas where there are no dentists [7], or who live in countries progressing toward an aging society.
Oral assessment tools for non-oral health professionals’ performance of oral health checkups have been developed to identify the need for dentist referral [8-10]. Oral health screenings by nonoral professionals (nurses) have been shown to be valid and reliable. However, a previous study regarding nurses’ performance of oral health checkups in a hospital reported that only 51.7% of 143 nurses had performed oral health checkups for elderly patients, and only 1 of them used an oral assessment tool for their oral health checkups [11].
It has been suggested that oral health professionals, especially dentists, should encourage and educate non-oral health professionals in the performance of oral health checkups through educational training programs. However, there are no studies regarding the development or efficacy of such programs. Therefore, it is necessary to develop efficient educational program to promote the performance of oral health checkups. Some studies have reported the effects of such educational programs on non-oral health professionals’ knowledge and attitudes towards oral healthcare [12-14]. In addition, there have been some studies concerning educational programs on oral heath checkups for small numbers of non-oral health professionals [15-17]. However, it is suggested that group-based educational programs are needed to develop nurses’ performance of oral health checkups because approximately 1.1 million nurses are reported to work in hospitals and long-term care facilities in Japan in 2016.
The purpose of this study was to investigate the effect of a groupbased educational program concerning oral assessments and oral healthcare on nurses’ awareness, attitudes, confidence, and performance of oral health checkups.
Materials and Methods
Study design and study sample
This was an interventional study of nurses who worked in a hospital in Fukuoka Prefecture, Japan. The hospital was located in the center of a mid-sized city. The number of hospital beds was 320, and the hospital had an affiliated long-term care facility. Therefore, the nurses working there had many opportunities to perform oral health checkups on elderly patients.
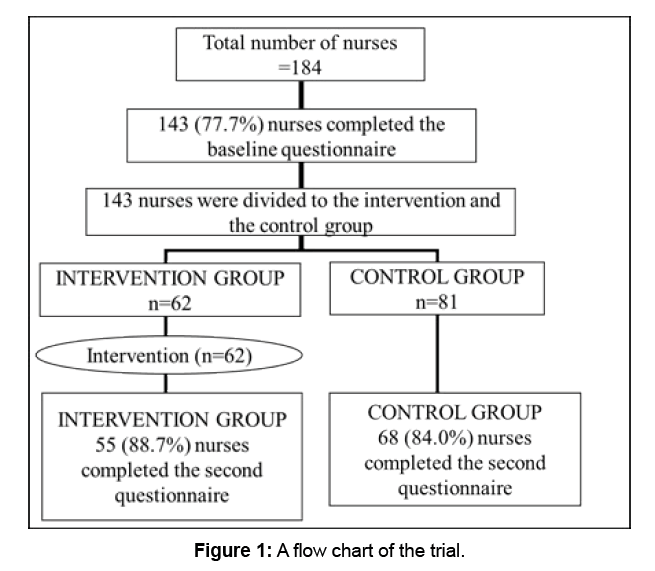
Figure 1 shows a flow chart of the study participants. All 184 nurses in the facility were employed as subjects without performing a power calculation because of the pilot nature of the study. The baseline questionnaires were distributed to the nurses in September 2016. The questionnaires were collected by staff members of the hospital and long-term care facility from September to October 2016. A total of 143 (77.7%) nurses completed the baseline questionnaire. The participants were divided into an intervention group and a control group. The selection of the intervention group depended on the nurses’ working schedule. Sixty-two nurses were ultimately invited to the educational program, which was held three times from November to December 2016. All invited nurses participated in one of the programs. The other 81 nurses were employed as the control group.
The second questionnaire was distributed to both groups one month after the intervention. Fifty-five nurses (88.7%) in the intervention group and 68 (84.0%) in the control group completed the second questionnaire and were employed for the analysis (Figure 1).
Questionnaires
The questionnaire was based on a previously-developed questionnaire that was used to investigate the practices, attitudes, and confidence of nurses in performing oral health checkups [11]. The examination of oral categories by non-oral professionals (nurses) was shown to be valid and reliable in a previous study [9-10].
The questionnaire consisted of 4 parts: socio-demographic (3 items); performance of oral health checkup (6 items); awareness (2 items) and attitude (3 items) in relation to oral health checkups (5 items); and confidence of oral examination (8 items).
The socio-demographic information that was collected included the respondent’s gender, age, and workplace. The workplaces were divided into three categories: a) the inpatient ward in the hospital; b) the long-term care facility; and c) other departments of the hospital (including the outpatient department, the department of radiology, the department of neuropsychiatry, the dialysis unit, and the operating room).
The term, “oral health checkup” was used in the questionnaire to describe the performance of oral screening to detect oral diseases or oral symptoms. Regarding the subjects’ awareness and attitude in relation to the performance of oral health checkups, they were asked whether they felt that a) dental caries or periodontal disease can be detected in oral health checkups performed by non-oral health professionals; b) oral cancer can be detected in oral health checkups performed by non-oral health professionals; c) they want to perform oral self-examinations every day; d) they want to perform oral health checkups for the elderly patients in their care; and e) all health workers should perform oral health checkups for elderly patients in their care. A four-point Likert scale was used for “Strongly agree”, “Somewhat agree”, “Somewhat disagree”, or “Strongly disagree”, giving scores from 0 (Strongly disagree) to 3 (Strongly agree). Regarding the respondents’ confidence in the oral examinations, they were asked how confident they felt examining each oral category. A four-point Likert scale was used for “Very confident”, “Somewhat confident”, “Somewhat unconfident”, or “Not at all confident”, giving scores from 0 (Not at all confident) to 3 (Very confident). Higher scores meant more awareness, more positive attitudes, or more confidence in the performance of oral health checkups. These scores were summed as the total score of the awareness and attitudes variables (Min=0, Max=15) or the confidence variables (Min=0, Max=24).
Regarding the performance of oral health checkups, participants were asked how many times they performed oral self-health checkups each week, utilizing a four-point scale (“Every day”, “4-6 times”, “1-3 times”, or “Very rarely”). If they answered “Every day”, “4-6 times”, or “1-3 times”, they were asked which oral examination categories they performed in their checkups.
They were then asked whether or not they had performed oral health checkups for elderly patients (≥65 years of age) in their care within the previous month. If they answered “Yes”, they were asked: a) how many times they had performed oral health checkups within the previous month, b) which oral examination categories they performed, and c) whether or not they used oral assessment tools, such as the oral assessment guide (OAG) or the oral health assessment tool (OHAT), in their oral health checkups [8,9].
The oral examination categories, which were defined based on the OHAT, were as follows: a) the lip (swelling, bleeding, and ulceration); b) the tongue and tongue coating; c) the gingiva and oral mucosa (swelling, bleeding, and ulceration); d) saliva (quality and quantity); e) the present teeth (decayed or broken teeth); f) removable dentures (broken areas); g) oral cleanliness (food residue, calculus, and plaque); and h) dental pain (verbal and/or non-verbal signs of pain). The oral examination categories of “Dental pain” were excluded in the oral selfhealth checkups.
The second questionnaire included the same content as the baseline questionnaire.
Intervention procedures
The lecture and practice for oral assessment and oral healthcare were conducted in the intervention group by the facilitator (T.N), who was a dentist specializing in gerodontology. A lecture regarding oral disease, oral assessment, and oral healthcare was conducted with using Microsoft PowerPoint slides for 40 minutes. The slides included images of plaque, calculus, and oral disease (xerostomia, dental caries, periodontal disease, and oral cancer).
In order to facilitate practicing oral checkups for elderly adults in their work, three fold-pocket sized OHAT sheets were distributed. The participants were instructed on how to use the sheets and asked to examine oral categories in 10 minutes. After the lecture, pairs of participants practiced mutual training in oral assessments and oral healthcare for 40 minutes. One member of each pair practiced performing an oral assessment and oral healthcare on the other, who played the role of an elderly patient with hemiplegia. They practiced oral assessment using a dental mirror and compact flashlight. They then practiced tooth brushing and cleaning the tongue and oral mucosa with a sponge brush. Each participant’s practice time was 20 minutes. The total time of the program was 1.5 h. The OHAT sheets used in the program were given to all participants, and they were instructed to use the sheets in their performance of oral health checkups for the elderly patients in their care.
Statistical analyses
A chi-squared test was used to explore the differences between the intervention and control groups in characteristic at baseline and to explore the differences between the performance of oral health checkups at baseline and follow-up. The group mean and median values were calculated for the awareness, attitude, and confidence variables. Mann-Whitney’s U test was used to explore the differences between the intervention and control groups in their awareness, attitudes, and confidence at baseline. Wilcoxon’s signed-rank test was used to explore the differences in the awareness, attitudes, and confidence variables between the baselines and follow-up. Data were analyzed with 5% significance. The statistical analyses were performed using the IBM SPSS Statistics software program (Version 21.0, IBM Corporation, Armonk, NY, USA).
Ethical considerations
This study was approved by the Ethics Committee of Fukuoka Dental College, Fukuoka, Japan (Approved #309). The front page of the questionnaire explained the aim of the project and the voluntary nature of the study. If nurses agreed to participate, they then answered the questionnaire.
Disclosure statement
All the authors have no conflict of interests to declare.
Results
A total of 143 nurses completed the baseline questionnaire. The total response rate was 77.7%. The majority (90.2% in the intervention group and 87.8% in the control group) of the participants was female. The mean age of the intervention group and the control group was 46.6 years (standard deviation [SD]=9.6) and 45.4 years (SD=11.8) respectively; the most common age group was 40-49 years. There were no significant differences between the intervention and control groups in characteristics, awareness and attitudes variables, confidence variables, or the performance of oral health checkups at baseline (Table 1).
| Socio-demographic data | Total (n=143) | Intervention (n=61) | control (n=82) |
|---|---|---|---|
| Gender | |||
| Male (n [%]) | 16 (11.2) | 6 (9.8) | 10 (12.2) |
| Female (n [%]) | 127 (88.8) | 55 (90.2) | 72 (87.8) |
| Age (years) | |||
| 20-29 (n [%]) | 8 (5.6) | 1 (1.6) | 7 (8.5) |
| 30-39 (n [%]) | 35 (24.5) | 14 (23.0) | 21 (25.6) |
| 40-49 (n [%]) | 42 (34.1) | 20 (36.4) | 22 (32.4) |
| 50-59 (n [%]) | 31 (25.2) | 16 (29.1) | 15 (22.1) |
| ≥60 | 17 (11.9) | 7 (11.5) | 10 (12.2) |
| Workplace | |||
| Inpatient ward (n [%]) | 98 (68.5) | 40 (65.6) | 58 (70.7) |
| Long-term care facility (n [%]) | 12 (8.4) | 5 (8.2) | 7 (8.5) |
| Other (n [%]) | 33 (23.1) | 16 (26.2) | 17 (20.7) |
| Total score of the awareness and attitude variables (Min=0, Max=15) | |||
| Mean (SD) | 10.3 (2.4) | 10.6 (2.6) | 10.1 (2.2) |
| Total score of the confidence variables (Min=0, Max=24) | |||
| Mean (SD) | 12.7 (3.8) | 13.2 (4.1) | 12.2 (3.6) |
| Performance of oral heal checkups: Performed oral self-health checkups within the previous week |
|||
| Yes (n [%]) | 118 (82.5) | 50 (82.0) | 68 (82.9) |
| No (n [%]) | 25 (17.5) | 11 (18.0) | 14 (17.1) |
| Performed oral health checkups for elderly patients in care within the previous month. | |||
| Yes (n [%]) | 74 (51.7) | 30 (49.2) | 44 (53.7) |
| No (n [%]) | 69 (48.3) | 31 (50.8) | 38 (46.3) |
Table 1: Baseline characteristics, awareness, attitudes, and confidence toward oral health checkups, and performance of oral health checkups between nurse groups.
Table 2 shows the comparison of scores for the awareness and attitudes variables and the confidence variables between baseline and follow-up. In the intervention group, the score for awareness that nonoral health professionals could detect oral cancer in their oral health checkups increased significantly (p<0.05). In addition, the score for confidence in the examination of oral cleanliness increased significantly (p<0.05). There were no significant differences between baseline and follow-up in the score of attitudes variables. In the control group, the score for attitudes concerning willingness to perform oral health checkups for elderly patients decreased significantly (p<0.05). There were no significant differences between the baseline and follow-up in the scores of awareness and confidence variables.
The score for confidence in examining present teeth and the total score of confidence variables increased slightly in the intervention group, although not to a significant degree (p=0.085 and p=0.073, respectively) (Table 2).
| Awareness and attitudes variables |
Intervention group (n=55) | Control group (n=68) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | p* | Baseline | Follow-up | p* | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Non-oral health professionals can detect tooth decay or gum disease in their oral health checkups. | 2.3 ± 0.7 | 2.4 ± 0.5 | 0.290 | 2.0 ± 0.7 | 2.0 ± 0.6 | 0.623 |
| Non-oral health professionals can detect oral cancer in their oral health checkups. | 1.7 ± 0.8 | 2.1 ± 0.7 | 0.006 | 1.6 ± 0.7 | 1.5 ± 0.7 | 0.155 |
| I want to perform oral self-checkups every day. | 2.3 ± 0.7 | 2.3 ± 0.6 | 0.847 | 2.1 ± 0.7 | 2.2 ± 0.6 | 0.369 |
| I want to perform oral health checkups for elderly patients in my care. | 2.2 ± 0.6 | 2.2 ± 0.6 | 0.983 | 2.2 ± 0.6 | 2.0 ± 0.6 | 0.039 |
| I believe that all health workers should perform oral health checkups in elderly patients in their care. | 2.4 ± 0.7 | 2.4 ± 0.6 | 0.725 | 2.2 ± 0.6 | 2.1 ± 0.6 | 0.269 |
| Total score (Min=0, Max=15) | 10.9 ± 2.4 | 11.4 ± 2.1 | 0.188 | 10.1 ± 2.1 | 9.9 ± 2.3 | 0.451 |
| Confidence variables Oral examination categories |
||||||
| Lip | 2.2 ± 0.6 | 2.1 ± 0.6 | 0.414 | 1.9 ± 0.6 | 1.9 ± 0.5 | 0.564 |
| Tongue and tongue coating | 1.8 ± 0.7 | 1.9 ± 0.6 | 0.564 | 1.6 ± 0.6 | 1.7 ± 0.6 | 0.495 |
| Gingiva and oral mucosa | 1.8 ± 0.7 | 1.9 ± 0.6 | 0.340 | 1.6 ± 0.6 | 1.6 ± 0.6 | 0.670 |
| Saliva | 1.2 ± 0.8 | 1.4 ± 0.7 | 0.152 | 1.2 ± 0.7 | 1.1 ± 0.7 | 0.590 |
| Present teeth | 1.5 ± 0.7 | 1.7 ± 0.6 | 0.085 | 1.4 ± 0.6 | 1.4 ± 0.6 | 0.827 |
| Removable dentures | 1.5 ± 0.7 | 1.7 ± 0.7 | 0.107 | 1.4 ± 0.7 | 1.5 ± 0.7 | 0.157 |
| Oral cleanliness | 1.7 ± 0.7 | 1.9 ± 0.6 | 0.047 | 1.6 ± 0.6 | 1.7 ± 0.6 | 0.336 |
| Oral pain | 1.7 ± 0.7 | 1.9 ± 0.6 | 0.088 | 1.4 ± 0.7 | 1.5 ± 0.6 | 0.220 |
| Total score (Min=0, Max=24) | 13.4 ± 4.2 | 14.5 ± 3.7 | 0.073 | 12.2 ± 3.7 | 12.5 ± 3.6 | 0.357 |
*Wilcoxon signed-rank test
Table 2: A comparison of scores for awareness and attitude variables and confidence variables between baseline and follow-up in the intervention and control groups.
Table 3 shows a comparison of the percentages performing oral health checkups between baseline and follow-up. About 80% of nurses in both groups performed oral health self-checkups more than once a week. More than half in both groups examined the lips, tongue and tongue coating, gingiva and oral mucosa, present teeth, and oral cleanliness in their performance of oral health self-checkups. There were no significant differences between baseline and follow-up for the performances in either group.
Variables |
Intervention group (n=55) | Control group (n=68) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||
| n (%) | n (%) | p* | n (%) | n (%) | p* | |
| Performance of oral health self-checkups | ||||||
| 45 (81.8) | 46 (83.6) | 0.801 | 57 (83.8) | 60 (88.2) | 0.458 | |
| Oral examination categories** | ||||||
| Lip | 32 (71.1) | 37 (80.4) | 0.299 | 36 (63.2) | 39 (65.0) | 0.836 |
| Tongue and tongue coating | 31 (68.9) | 34 (73.9) | 0.596 | 37 (64.9) | 35 (58.3) | 0.465 |
| Gingiva and oral mucosa | 35 (77.8) | 35 (76.1) | 0.848 | 35 (61.4) | 39 (65.0) | 0.687 |
| Saliva | 6 (13.3) | 9 (19.6) | 0.423 | 6 (10.5) | 3 (5.0) | 0.262 |
| Present teeth | 29 (64.4) | 28 (60.9) | 0.725 | 36 (63.2) | 38 (63.3) | 0.984 |
| Removable dentures | 1 (2.2) | 4 (8.7) | 0.175 | 3 (5.3) | 0 (0.0) | 0.072 |
| Oral cleanliness | 31 (68.9) | 32 (69.6) | 0.944 | 41 (71.9) | 35 (58.3) | 0.123 |
| Performance of oral health checkups for elderly patients | ||||||
| 26 (47.3) | 26 (47.3) | 1.000 | 37 (54.4) | 32 (47.1) | 0.391 | |
| Oral examination categories** | ||||||
| Lip | 21 (80.8) | 19 (73.1) | 0.510 | 22 (59.5) | 24 (75.0) | 0.172 |
| Tongue and tongue coating | 16 (61.5) | 13 (50.0) | 0.402 | 21 (56.8) | 20 (62.5) | 0.450 |
| Gingiva and oral mucosa | 18 (69.2) | 15 (57.7) | 0.388 | 21 (56.8) | 16 (50.0) | 0.575 |
| Saliva | 3 (11.5) | 6 (23.1) | 0.271 | 3 (8.1) | 4 (12.5) | 0.547 |
| Present teeth | 9 (34.6) | 8 (30.8) | 0.768 | 11 (29.7) | 13 (40.6) | 0.343 |
| Removable dentures | 15 (57.7) | 13 (50.0) | 0.578 | 21 (56.8) | 16 (50.0) | 0.575 |
| Oral cleanliness | 16 (61.5) | 15 (57.7) | 0.777 | 22 (59.5) | 24 (75.0) | 0.172 |
| Oral pain | 11 (42.3) | 14 (53.8) | 0.405 | 7 (18.9) | 10 (31.3) | 0.236 |
*: Chi-squared test
**: The percentages indicate the ratio of the number of nurses examining oral categories to the number of nurses performing oral health checkups
Table 3: A comparison of the percentages of participants performing oral health checkups between baseline and follow-up in the intervention and control groups.
About half of nurses in both groups had performed oral health checkups for elderly patients in the previous month. However, no participants in the intervention group and only one in the control group used oral assessment tools at baseline. Only one in each group used oral assessment tools one month after the intervention. More than half of participants in both groups examined the lip, tongue and tongue coating, gingiva and oral mucosa, and removed dentures in their performance of oral health checkups for elderly patients. However, only 30%-40% of nurses examined the present teeth, and only 10%- 20% examined saliva in their performances. There were no significant differences between baseline and follow-up for the performances in either group (Table 3).
Discussion
This is the first report to investigate the effect of an educational program concerning oral assessments and oral healthcare on nonoral professionals’ awareness, attitudes, confidence, and performances of oral health checkups. There have been no program specialized for the education of non-oral professionals in oral health checkups. We therefore created a new educational program combining lectures on oral assessment and oral healthcare. One reason for adding the oral healthcare lecture to the oral assessment program was to promote attendance. As a result, all invited nurses attended the program. The facilitator for the intervention group had substantial experience in conducting oral healthcare programs for non-professionals and understood the purpose of this study.
At baseline, the participants’ awareness of their ability to detect oral cancer during their oral health checkups was low. In Japan, the number of cases of oral cavity and oropharyngeal cancer has steadily increased, from 2,497 cases in 1975 to 15,716 cases in 2011. However, the incidence of oral cancer is lower than that of other cancers [18]. It seemed that the main reason for their low level of awareness was that they had no experience seeing patients with oral cancers. A previous study reported that electronic presentations with images of oral and maxillofacial cancer were good tools for sharing information with a variety of clinical and non-clinical audiences [19]. It has been suggested that a presentation with image slides of oral cancer may be effective in improving awareness among nurses. Further studies are needed to investigate whether or not improvement in their awareness will help improve their performance of oral health checkups for oral cancer.
Most subjects had positive attitudes toward oral health checkups at baseline, and the program therefore could not improve their attitude. A previous study regarding oral healthcare education reported that the supervised implantation of an oral healthcare program could not improve participants’ attitudes [14]. These studies suggest that it might be difficult to improve participants’ attitudes toward oral health. Other studies have suggested that having the opportunity to discuss their feeling about oral health after the education session might be effective in improving non-oral professionals’ attitudes toward oral health. Therefore, if there is enough time, discussion time should be added to the program to improve attitudes toward the performance of oral health checkups. In the control group, participants’ attitudes toward willingness to perform oral heath checkups for elderly patients decreased one month after the intervention compared with baseline. New Year’s holidays (4-5 days) fell in the period between the intervention and the second survey. These holidays might have contributed to an increased workload during this period, and the nurses in the control groups might therefore have felt more negatively about performing even more work via checkups, leading to negative attitudes. This result also suggests that the attitudes in the intervention group remained positive even during this period of increased work and stress.
The present study showed that confidence in performing oral health checkups, especially in examining oral cleanliness, improved in the intervention group. A previous study revealed that confidence in relation to the performance of oral examinations was significantly associated with the performance of oral health checkups for elderly patients [11]. Furthermore, previous studies regarding smoking cessation counseling have found that a health provider’s confidence was important for modifying their counseling abilities and that training in counseling increased their confidence [20,21]. Therefore, the training in oral assessment and oral healthcare included in the program might have contributed to the improvement in their confidence.
The main purpose of the present study was to promote nurses’ performance of oral health checkups for elderly adults. However, this program could not improve their performance of oral health selfcheckups or oral health checkups for elderly patients. Pocket-sized OHAT sheets were given to all 55 nurses (the intervention group) in the program. However, only one nurse used the sheet one month after the intervention. Those results showed that participation in the group-based program only once and the distribution of oral assessment tools was not effective in promoting the performance of these checkups in nurses. Further improvement of the program tailored to the performance of checkups may therefore be needed to promote oral health checkup performance. In addition, continued participation in the program may help nurses gain confidence, which may in turn promote their performance of oral health checkups.
Another possible reason for the lack of change in their performance of oral health checkups is the lack of financial support, such as national health insurance; furthermore, nurses are not tasked with performing oral health checkups and dentist referral in Japan. Although most nurses reported that they felt that they should perform oral health checkups and use oral assessment tools in their usual care, it might be difficult to encourage them to do so with group-based educational programs alone. It is therefore suggested that in addition to the introducing such a program, it might be necessary to provide environmental support, such as the improvement of the care system. For example, the introduction of oral assessment tools in the oral healthcare protocol for elderly patients in their facilities might be effective [15].
A previous study reported that the salivary flow rates were significantly reduced in older adults compared with younger adults [22]. Saliva is important for maintaining the oral health [23]. In Japan, there is no specific license given for examining saliva like there is for evaluating blood or urine test findings. Nurses are instructed to observe the oral condition, such as the dryness of the oral cavity or contamination of the saliva flow. However, the present study showed that only about 10% of nurses examined the saliva at baseline, and only 20% in the intervention group examined it at 1 month after the intervention. Therefore, the development of tools for the easy assessment of the saliva status may be important for promoting the examination of saliva.
Less than half of nurses examined the present teeth of elderly patients, with no significant differences in this examination between baseline and follow-up in either group. This result might indicate that nurses do not feel such an examination is important, or they may feel this examination is difficult without a dental mirror. Several reports have suggested that impaired mastication ability due to tooth loss might be a risk factor for cardiovascular and gastrointestinal diseases and other health problems [24,25]. Therefore, examinations of the present teeth are becoming more important for sustaining the teeth. Further lectures on the relationship between malnutrition and the oral condition or oral health and aspiration pneumonia are needed to improve the rate of examination performance.
Several limitations associated with the present study warrant mention. First, the subjects were divided into intervention and control groups, taking account into their working schedule. This might have caused selection bias. However, there were no significant differences between the two groups in their characteristics, awareness and attitudes variables, confidence variables, or performance of oral health checkups at baseline. Second, the study population was limited to nurses who worked at a single hospital and long-term care facility in Japan. There may be some differences in the performance of oral health checkups by other health workers or at other facilities.
However, despite these limitations, we feel that the present study will provide a foundation for further studies investigating non-oral professionals’ performance of oral health checkups and the development of educational training programs for non-oral professionals, medical students, and nurse students.
Conclusion
This is the first report to investigate the effect of a group-based educational program concerning oral assessment and oral healthcare on non-oral professionals’ awareness, attitudes, confidence, and performance of oral health checkups in Japan.
The present study showed that the educational program improved participants’ awareness and confidence toward oral health checkups. However, their attitudes and performance of oral health checkups for elderly patients were not improved by the program. Thus, in addition to ensuring the continuous participation of nurses in the program, environmental support such as the introduction of oral assessment tools into their oral healthcare protocols might be needed to promote the performance of oral health checkups in this population.
The findings of the present study will provide a foundation for developing a group-based educational oral health checkup training program for non-oral health professionals and promoting the performance of oral health checkups for elderly patients in long-term care facilities and hospitals.
Eating, speaking, and smiling all require good oral health, which is essential for the general health and well-being of all people, especially the elderly. Oral assessment tools for non-professionals may work as effective communication tools between non-oral health professionals and oral health professionals. We hope the enhancement of oral care for older adults by multi-occupational collaboration will lead to a reduction in the risk of developing oral diseases and associated systemic consequences.
Acknowledgements
The authors are grateful to Juzabu Jinnouchi, the president of Sasaguri hospital, Yoko Sanda, a director of nurse service department of Sasaguri Hospital, and the staff members of Sasaguri Hospital, Fukuoka, Japan. This work was supported by JSPS KAKENHI, grant number JP 25463277 and 17K12001.
References
- Nitschke I, Müller F, Hopfenmüller W (2001) The uptake of dental services by elderly Germans. Gerodontology 18: 114-120.
- Ohi T, Sai M, Kikuchi M, Hattori Y, Tsuboi A, et al. (2009) Determinants of the utilization of dental services in a community-dwelling elderly Japanese population. Tohoku J Exp Med 218: 241-249.
- Giannobile WV, Braun TM, Caplis AK, Doucette-Stamm L, Duff GW, et al. (2013) Patient stratification for preventive care in dentistry. J Dent Res 92: 694–701.
- Berg R, Berkey DB, Tang JM, Baine C, Altman DS (2000) Oral health status of older adults in Arizona: Results from the Arizona Elder Study. Spec Care Dentist 20: 226-233.
- Kikutani T, Yoshida M, Enoki H, Enoki H, Yamashita Y, et al. (2013) Relationship between nutrition status and dental occlusion in community-dwelling frail Older adults. Geriatr Gerontol Int 13: 50-54.
- Japanese Dental Association, Japanese Agency for Dental Research (2011) Survey on dental involvement in team approach at hospital (in Japanese). Japanese Dental Association, Tokyo.
- Azodo CC, Ezeja EB, Ehizele AO, Ehigiator O (2013) Oral assessment and nursing interventions among Nigerian nurses-knowledge, practices and educational needs. Ethiop J Health Sci 23: 265-270
- Eilers J, Berger AM, Petersen MC (1988) Development, testing, and application of the oral assessment guide. Oncol Nurs Forum 15: 325-330.
- Chalmers JM, King PL, Spencer AJ, Wright FA, Carter KD (2005) The oral health assessment tool -validity and reliability. Aust Dent J 50: 191-199.
- Tsukada S, Ito K, Stegaroiu R, Shibata S, Ohuchi A (2017) An oral health and function screening tool for nursing personnel of long-term care facilities to identify the need for dentist referral without preliminary training. Gerodontology 34: 232-239.
- Haresaku S, Aoki H, Makino M, Monji M, Kansui A, et al. (2018) The practices, attitudes, and confidence of nurses in the performance of oral health checkups for elderly patients in a Japanese hospital. Oral Health Prev Dent.
- Frenkel H, Harvey I, Needs K (2002) Oral health care education and its effect on caregivers' knowledge and attitudes: a randomised controlled trial. Community Dent Oral Epidemiol 30: 91-100.
- Le P, Dempster L, Limeback H, Locker D (2012) Improving residents' oral health through staff education in nursing homes. Spec Care Dentist 32: 242-250.
- Janssens B, De Visschere L, van der Putten GJ, de Lugt-Lustig K, Schols JM, et al. (2016) Effect of an oral healthcare protocol in nursing homes on care staffs' knowledge and attitude towards oral health care: a cluster-randomized controlled trial. Gerodontology 33: 275-286.
- Amerine C, Boyd L, Bowen DM, Neill K, Johnson T, et al. (2014) Oral health champions in long-term care facilities-a pilot study. Spec Care Dentist 34: 164-170.
- Saensom D, Merchant AT, Wara-Aswapati N, Ruaisungnoen W, Pitiphat W (2016) Oral health and ventilator-associated pneumonia among critically ill patients: a prospective study. Oral Dis 22: 709-714.
- Deutsch A, Siegel E, Cations M, Wright C, Naganathan V, et al. (2017) A pilot study on the feasibility of training nurses to formulate multicomponent oral health interventions in a residential aged care facility. Gerodontology 34: 469-478.
- No Authors Listed (2016) Cancer statistics in Japan 2015. Foundation for Promotion of Cancer Research, Tokyo.
- Carvalho FS, Chaves FN, Soares EC, Pereira KM, Ribeiro TR, et al. (2016) Educational utilization of microsoft powerpoint for oral and maxillofacial cancer presentations. Asian Pac J Cancer Prev 17: 2337-2339.
- Pinto BM, Goldstein MG, DePue JD, Milan FB (1998) Acceptability and feasibility of physician-based activity counseling. Am J Prev Med 15: 95-102.
- Hudmon KS, Kroon LA, Corelli RL, Saunders KC, Spitz MR, et al. (2004) Training future pharmacists at a minority educational institution: Evaluation of the Rx for Change Tobacco Cessation Training Program. Cancer Epidemiol Biomarkers Prev 13: 477-481.
- Affoo RH, Foley N, Garrick R, Siqueira WL, Martin RE (2015) Meta-analysis of salivary flow rates in young and older adults. J Am Geriatr Soc 63: 2142-2251.
- Dodds MW, Johnson DA, Yeh CK (2005) Health benefits of saliva: A review. J Dent 33: 223-233.
- Hung HC, Colditz G, Joshipura KJ (2005) The association between tooth loss and the self-reported intake of selected CVD-related nutrients and foods among US women. Community Dent Oral Epidemiol 33: 167-173.
- Yoshihara A, Watanabe R, Nishimuta M, Hanada N, Miyazaki H (2005) The relationship between dietary intake and the number of teeth in elderly Japanese subjects. Gerodontology 22: 211-218.
Citation: Haresaku S, Aoki H, Makino M, Monji M, Kansui A, et al. (2018) Effect of an Educational Program concerning Oral Assessment and Healthcare on Nurses’ Performance of Oral Health Checkups in a Hospital. J Oral Hyg Health 6: 232. DOI: 10.4172/2332-0702.1000232
Copyright: © 2018 Haresaku S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5728
- [From(publication date): 0-2018 - Apr 26, 2025]
- Breakdown by view type
- HTML page views: 4821
- PDF downloads: 907