Effect of a Short-term Corrective Exercise Program on Chronic Knee and Hip Pain
Received: 29-Nov-2018 / Accepted Date: 17-Jan-2019 / Published Date: 18-Jan-2019 DOI: 10.4172/2165-7025.1000404
Abstract
The objective of this study was to determine the acute effect following one corrective exercise treatment and the short-term effect of a home-based two-week corrective exercise program on chronic knee and hip pain. Forty participants with chronic knee and/or hip pain (defined as pain on most days of the week for at least the past 12 weeks) were recruited as a convenience sample and randomly assigned to either an exercise treatment group and a control group. All participants were instructed to maintain their current lifestyle for the duration of the study; however, the exercise treatment group also completed an Egoscue Method corrective exercise routine at least five days per week for two weeks. All participants kept a daily log of their average pain levels at rest and during movement using a visual analog scale (VAS). Additionally, subjects completed the Western Ontario and McMaster Universities Arthritis Index (WOMAC) and scores were recorded at baseline, week 1, and week 2. The exercise treatment group experienced a trend of reduced daily pain during movement (p=0.019) as reported in VAS logs. After controlling for age, BMI, past surgeries, arthritis status, and location of pain, there was a significant group x time interaction in WOMAC scores (p=0.015). At week 2, total WOMAC scores were significantly lower in the exercise treatment group (p=0.001) but not the control group (p>0.05). In conclusion, two weeks of corrective exercises significantly reduced knee and hip pain and improved function in the exercise treatment group.
Keywords: Therapeutic exercise; Musculoskeletal pain; Posture
Introduction
Chronic musculoskeletal pain is a major cause of reduced quality of life [1-3]. It is estimated that each year 25% of people over 55 y have a persistent episode of knee pain [4]. Approximately 9.5% of men and 11.2% of women have hip osteoarthritis [5], while about 9.3% of the U.S. population is diagnosed with symptomatic knee osteoarthritis by age 60 [6].
It has been suggested that posture plays a major role in the development of chronic pain [7]. The misalignment of body segments as a result of improper posture leads to compensatory effort by other segments, resulting in excess muscular strain [8] and wear on the joints [9]. Postural abnormalities are deviations from the ideal posture as defined by the Kendall and McCreary method [10]. Research has shown that more severe postural abnormalities result in significantly greater incidence of pain in the thoraco-cervical-shoulder region [11]. Other research has shown that ideal posture results in less lumbar back pain compared to postural misalignments [12].
Corrective exercise has been used to improve posture by bringing body segments closer to an ideal alignment [13-17]. When combined with traditional treatments the effectiveness of postural corrective exercise, ultrasound, and infrared radiation compared to ultrasound and radiation alone revealed significant reduction in neck pain and forward head angle [18].
A meta-analysis of eight randomized controlled studies investigating the effect of strengthening and/or aerobic exercise on chronic hip pain in participants with hip osteoarthritis found a pooled effect size of exercise on hip pain was 0.46 compared to a control group [19]. Similarly, another large meta-analysis of 32 studies, which included data on 3616 patients with knee osteoarthritis found a beneficial treatment effect for exercise with an effect size of 0.40 for knee pain [20].
While there are many types of corrective exercise used in chiropractic, physiotherapy, and personal fitness training, the Egoscue Method (EM) of corrective exercise is the focus of this study. The EM uses corrective exercises designed to improve whole-body postural alignment and reduce musculoskeletal pain by improving joint mobility and stability [7]. This involves evaluating a patient’s posture, and prescribing a personalized corrective exercise program (e.g., E-cise menu) based on their unique postural deviations. The E-cise menu consists of 10-20 E-cises, which may take 45-75 min to complete, preferably on a daily basis. Although the EM is reported to be effective from an observational perspective in a clinical setting [21], it has not been objectively studied in a research setting.
Strengthening and aerobic exercise can be beneficial for people suffering from chronic hip [19,22,23] or knee pain [20,24,25]. Nevertheless, most exercise prescriptions are not based on whole-body posture assessment. To date, there are no published studies investigating the relationship between whole-body posture assessment and chronic hip and/or knee pain. Furthermore, to the best of our knowledge, it has not been established that that a corrective exercise prescription based on improving whole-body posture can reduce chronic hip and/or knee pain. The EM, which employs corrective exercise, seeks improve posture and reduce chronic pain. Because the EM E-cises is designed to be performed at home and do not require the use of expensive equipment, this type of therapy may be a costeffective approach for people suffering from chronic knee and/or hip pain.
This study sought to determine the acute effect following one corrective exercise treatment and the short-term effect of a homebased two-week corrective exercise program on chronic knee and hip pain. We hypothesized that: 1) knee and hip pain would not significantly decrease pain rating scores following one corrective exercise treatment, and 2) knee and hip pain would be significantly lower following a two-week corrective exercise program.
Materials And Methods
This study was a simple randomization design. Participants were a convenience sample who were randomly assigned to either the exercise treatment group, which performed corrective exercises for two weeks, or the control group, which did not perform any exercise treatment for two weeks. Group assignment was determined by each participant drawing a group assignment out of an envelope and accordingly being assigned by either the intervention or control groups. Group assignment/randomization was conducted by the same person who was a trained research assistant. Aside from the added exercise treatment, all participants were instructed to maintain their current habitual lifestyle for the duration of the study.
The relatively short study duration was chosen because the EM suggests that significant reductions in pain can be made after a single exercise session [7]. At the beginning of the study, pain and posture were assessed before and after a single bout of corrective exercises in the exercise group, while the control group was assessed before and after 45 minutes of rest. All participants recorded their level of pain daily, and their function and posture were assessed at one- and twoweek intervals. All study methods and procedures were approved by University Institutional Review Board for the use of Human Subjects prior to any data collection. Subject recruitment and data collection continued for a total of 4 months. All participants provided written informed consent prior to participation in this study.
Participants
Participants for this study were recruited from the university community via email announcements and flyers. Participants were adults (18-71 y, mean 47.4 ± 15.5 y) with chronic knee and/or hip pain. An age-diverse sample was selected to evaluate the pain-reducing effects of an individualized corrective exercise protocol across a variety of ages. Chronic pain was defined as pain on most days of the week for at least 12 weeks [24]. Individuals were excluded from the study if they (a) had undergone a knee or hip surgery or had sustained a knee or hip injury in the past 12 months, (b) were currently receiving any form of pain treatment such as physiotherapy, chiropractic, intra-articular injections, or prescription pain medications, (c) exhibited a severe lack of mobility, (d) reported an initial pain level <3 cm on the Visual Analog Scale (VAS) scale, (e) were pregnant, or (f) were unable to understand English. Individuals were allowed to take non-prescription medications, such as non-steroidal anti-inflammatory medications, during the study; however, they were required to refrain from taking any non-prescription pain medication during the 12 hours preceding the first and second assessments. A power analysis using a power level of 80% and alpha set at 0.05 indicated a sample size of 40 participants (20 in the control group and 20 in the exercise group). A large effect size (0.80) was assumed because this has been reported in the literature [26] for differences in Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores following an at-home exercise program. Forty-two eligible participants were originally recruited.
Intervention
All participants completed a pre-participation questionnaire that included questions about age, gender, injuries, previous joint-related surgery, the likelihood of a future joint-related surgery, and current non-prescription pain medication use. Participants completed two versions of the VAS for knee and/or hip pain: one for pain at rest and one for pain during movement. If participants had pain in multiple joints, they were told to record their overall level of pain. Participants were told to indicate their “usual pain” over the past seven days. Participants needed to have a VAS pain score of at least 3 cm (either at rest or during movement) in order to participate in the study [27]. The VAS method [28,29] exhibits a high test-retest reliability (r=0.94, P<0.001). Participants also completed the WOMAC questionnaire [30,31] which has been shown to be a valid and reliable arthritis index in patients with knee and hip osteoarthritis. Participants’ body mass was also measured to the nearest 0.1 kg and height to the nearest 0.5 cm using a digital scale and a stadiometer, respectively.
An EM corrective exercise protocol was followed and a postural alignment specialist trained in postural evaluation conducted all assessments. To reduce possible inter-rater error, the same researcher conducted all postural evaluations. An individualized exercise program (E-cise menu) was generated using the ePeteTM software (version 4.4.3) based on the noted postural deviations. To ensure that all exercise treatment participants were prescribed the same volume of exercise, the E-cise menus were adjusted by adding or removing exercises so the time required completing the exercises was approximately 45 minutes. Typical corrective exercises employed as part of the E-cise menu are listed on Table 1, along with an internet web link that can be accessed to view each corrective exercise protocol, and common exercise requirements (sets, repetitions, and hold times).
| Exercise name | Internet web link to exercise protocol | Common exercise requirement* |
|---|---|---|
| Standing windmill | http://www.egoscue.com/WebMenus/ECiseHTML/30000.html | 10 repetitions x 4 sets |
| Standing arm circles | http://www.egoscue.com/WebMenus/ECiseHTML/13.html | 20 repetitions x 6 sets |
| Static back | http://www.egoscue.com/WebMenus/QTVideo/30.html | 5-minute hold |
| Hip crossover stretch | http://www.egoscue.com/WebMenus/ECiseHTML/383.html | 1-minute hold (each side) |
| Cats and dogs | http://www.egoscue.com/WebMenus/ECiseHTML/19.html | 10 repetitions (both directions) |
| Sitting femur rotations | http://www.egoscue.com/WebMenus/QTVideo/18.html | 10 repetitions x 4 sets |
| Static back abdominal contractions | http://www.egoscue.com/WebMenus/QTVideo/349.html | 20 repetitions x 3 sets |
| Hooklying gluteal contractions | http://www.egoscue.com/WebMenus/ECiseHTML/28.html | 20 repetitions x 3 sets |
| Hooklying knee squeezes | http://www.egoscue.com/WebMenus/QTVideo/26.html | 20 repetitions x 3 sets |
| Airbench | http://www.egoscue.com/WebMenus/ECiseHTML/27.html | 1-minute hold |
| Supine groin stretch (modified) | http://www.egoscue.com/WebMenus/ECiseHTML/31.html | 5-minute hold |
| Supine foot circles-point/flexes | http://www.egoscue.com/WebMenus/ECiseHTML/3.html | 10 repetitions x 8 sets |
*Total time of E-cise routine=about 45 minutes; with minimal rest between sets (0-30 seconds)
Table 1: Examples of typical egoscue corrective exercises.
Participants in the exercise treatment group were led through their complete E-cise menu by the researcher to ensure competency on the exercises. Participants in the control group did not perform any exercises for 45 minutes. Immediately following the exercise session or 45 minutes of rest, participants completed the VAS again for their current knee and/or hip pain at rest and with movement.
All participants were given logs (one for each day of the week), which they were to fill out every evening before retiring to bed. These logs contained questions about their compliance to the E-cise menu (for those in the exercise group) and a VAS for pain at rest and during movement. All participants were instructed to maintain their current lifestyle for the duration of the study; however, the exercise treatment group also completed an EM corrective exercise routine at least five days per week for two weeks. In addition, participants in the exercise treatment group were scheduled for a return visit the following day so that E-cises could be observed for competency and any adjustments could be made to the E-cise menu if participants were experiencing pain during an E-cise. Participants in the exercise treatment group were instructed to complete their E-cise menu at home on at least five days of the week, but preferably every day, for the next two weeks. Forty-two participants were originally recruited for this study. Contact was lost with one participant from the exercise treatment group and a participant from the control group was excluded for receiving additional pain therapy during the study, leaving 40 participants for analysis (20 in exercise group, 20 in control group). All participants in the exercise treatment group reported performing their E-cise menu at least five days per week for the duration of the study.
ePeteTM software
The ePeteTM software is a computer program designed by the Egoscue clinic for creating personalized corrective exercise programs. Postural deviations (as noted in the posture assessment) are entered into the program, from which an EM corrective exercise menu can be derived. This menu is specific to the unique postural deviations of the participant and is designed to improve misalignments. The E-cise menu is fully customizable. The software has a database of approximately 600 corrective exercises, of which 60-70 are drawn from to create E-cise menus.
Data analysis
Statistical Analysis Software (SAS), version 9.3 (Cary, North Carolina) was used for data analysis. VAS and WOMAC scores were analyzed using analysis of covariance. Age, gender, BMI, location of pain, non-prescription pain medication use, history of joint surgery, arthritis, likelihood of future surgery, and pain at baseline were all covariates used in analysis. The daily VAS pain data were analyzed using residual maximum likelihood.
Participant demographics were analyzed to determine frequencies, means, and standard deviations in order to describe the sample. Statistical significance was set at p<0.05.
Results
At baseline, participants’ age, BMI, likelihood of joint replacement surgery, VAS pain, and WOMAC scores were not significantly different between groups (Table 2).
| Variable | Treatment (n=20) |
Control (n=20) |
p value |
|---|---|---|---|
| Age (y) | 43.2 ± 3.7 | 51.6 ± 3.2 | 0.09 |
| BMI (kg/m2) | 29.0 ± 1.5 | 27.4 ± 1.4 | 0.45 |
| Surgery likelihood (Likert 1-7) | 3.7 ± 0.5 | 3.2 ± 0.4 | 0.44 |
| VAS pain during movement (cm) | 5.5 ± 1.8 | 5.9 ± 1.6 | 0.56 |
| VAS pain at rest (cm) | 2.4 ± 1.9 | 2.7 ± 1.7 | 0.74 |
| Total WOMAC score | 26.8 ± 3.6 | 24.2 ± 3.8 | 0.52 |
| WOMAC function score | 15.5 ± 2.4 | 13.9 ± 2.5 | 0.59 |
| WOMAC pain score | 6.6 ± 0.8 | 6.4 ± 0.8 | 0.84 |
Results are described as mean ± standard error
Table 2: Participant characteristics at baseline.
Unexpectedly, at baseline, non-prescription pain medication use was greater in the control group compared to the exercise group (p=0.04). However, non-prescription pain medication use was not a significant covariate in any of the statistical analyses. Additionally, there were no significant changes in non-prescription pain medication use from baseline and after weeks 1 and 2 in either group (p=0.29). VAS pain scores in the exercise treatment group did not significantly change after a single corrective exercise routine, after controlling for location of pain, past surgery, and age, at rest (p=0.49; for group x time interaction) or pain during movement (p=0.69; for group x time interaction).
Resting VAS pain scores decreased by 1.40 ± 0.34 cm in the exercise group and 0.48 ± 0.32 cm in the control group, although the difference between groups did not reach statistical significance (p=0.06). After controlling for initial pain level, location of pain, past surgery, and arthritis, there was no significant decrease over time for pain at rest as measured by daily resting VAS pain scores (p=0.52).
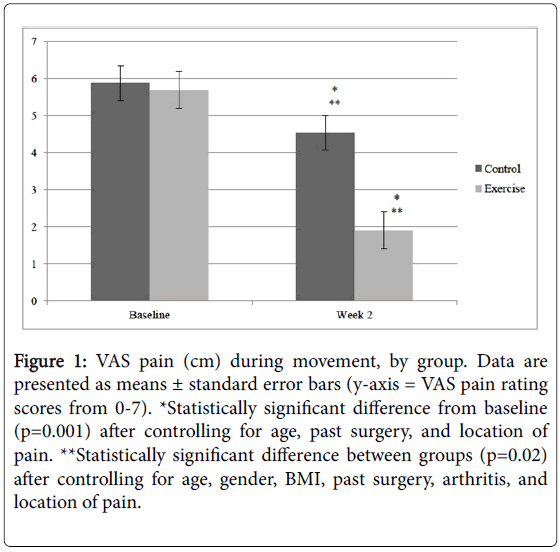
On the other hand, movement VAS pain scores (Figure 1) decreased on average by 0.11 ± 0.03 cm/d in the exercise group (p=0.002), while there was a non-significant decrease of 0.02 ± 0.03 cm/d in VAS pain scores in the control group (p=0.47). The difference between the groups was statistically significant (p=0.02) after controlling for significant covariates (initial pain level, location of pain, past surgery, arthritis). Compared to baseline, pain during movement at the end of the second week decreased by 3.77 ± 0.49 cm in the exercise group and 1.34 ± 0.46 cm in the control group (p=0.001 for group x time interaction).
Figure 1: VAS pain (cm) during movement, by group. Data are presented as means ± standard error bars (y-axis = VAS pain rating scores from 0-7). *Statistically significant difference from baseline (p=0.001) after controlling for age, past surgery, and location of pain. **Statistically significant difference between groups (p=0.02) after controlling for age, gender, BMI, past surgery, arthritis, and location of pain.
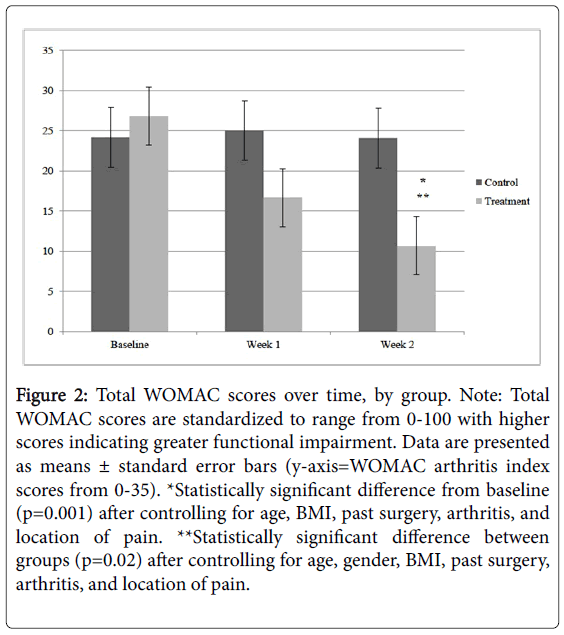
Total WOMAC scores decreased significantly in the exercise treatment group over time, while total WOMAC scores in the control group did not change significantly (Table 3, Figure 2). Although, there were non-significant decreases in total WOMAC (p=0.11), function (p=0.09), and pain subscores (p=0.54) in the exercise treatment group after the first week; by the end of week 2, decreases in total WOMAC (p=0.001), function (p=0.002), and pain (p=0.008) subscores were statistically significant (Table 3). Total WOMAC, function, and pain subscores were significantly lower (p=0.02, p=0.03, p=0.01, respectively) in the exercise treatment group compared to the control group at the end of week 2. Compared to baseline, the exercise group showed a 60%, 67%, and 51% relative decrease in total WOMAC, function, and pain subscores, respectively at the end of week 2.
Figure 2: Total WOMAC scores over time, by group. Note: Total WOMAC scores are standardized to range from 0-100 with higher scores indicating greater functional impairment. Data are presented as means ± standard error bars (y-axis=WOMAC arthritis index scores from 0-35). *Statistically significant difference from baseline (p=0.001) after controlling for age, BMI, past surgery, arthritis, and location of pain. **Statistically significant difference between groups (p=0.02) after controlling for age, gender, BMI, past surgery, arthritis, and location of pain.
Thus, the results of this study support our initial hypotheses and demonstrated that: 1) knee and hip pain did not significantly decrease pain rating scores following one corrective exercise treatment, and 2) knee and hip pain was significantly lower following a two-week corrective exercise program.
Discussion
This study evaluated the effect of a corrective exercise program on pain and function in participants with chronic knee and/or hip pain after one treatment, at one week and after two weeks of performing exercises. The resulting data showed a significant decrease in pain over the two weeks, as well as a significant improvement in functional capacity in the exercise group compared to the control group. To date, this appears to be the first study to investigate the effectiveness of EM corrective exercises in a research setting.
Research on the effect of corrective exercise on pain and posture is limited. The studies that have examined corrective exercise have focused primarily on isolated locations of the spine or shoulders. Two studies [17,18] found that corrective exercises can significantly reduce neck pain. Corrective exercises have also been shown to reduce forward head angle [13] and forward shoulder angle [14]. One study [15] suggested that Pilates exercises may improve both standing and sitting sagittal plane posture. No studies were found which evaluated a corrective exercise approach based on a whole-body postural assessment.
The EM is based on the premise that in most instances musculoskeletal pain can be attributed to improper posture [7]. The EM shares the belief with others [10,32] that misaligned posture is a result of underuse or overuse of skeletal muscles, which results in inadequate muscular control or imbalances. These imbalances can alter the alignment of the skeletal system, which puts excess stress on joints and leads to chronic pain. Several cross-sectional studies support this hypothesis. Griegel-Morris et al. [11] found that participants with more severe postural abnormalities had significantly increased incidence of pain in the thoraco-cervical-shoulder region. They also noted that postural abnormalities were quite common, with 66% of participants exhibiting forward head posture, 38% having kyphosis, and 73% and 66% of the participants showing right and left rounded shoulders, respectively. Guimond and Messrieh [12] also discovered that those with ideal posture had significantly less cervical, thoracic, and lumbar spine pain. Another study found a positive correlation between neck pain and forward head and rounded shoulders [33].
The purpose of the EM is to use corrective exercises to bring the whole body closer to “ideal” posture and thus reduce pain. A key characteristic of the EM is the premise that postural misalignments of a given joint can lead to pain at the same or another joint, which is why the whole-body postural alignment should be considered when treating pain [34]. Others have suggested that misaligned posture can have negative effects on various locations in the body [35]. The E-cises are designed to influence all the major joints of the body. Data from our study show that EM corrective exercises can significantly reduce knee and hip pain, as well as improve perceived physical function.
Our data show a significant decrease in pain in the exercise treatment group, as reported in participants’ daily logs, over the course of this two-week study. This suggests that these corrective exercises have a relatively quick effect on decreasing knee and hip pain. Although it has been suggested that the EM corrective exercises can provide immediate pain relief, [21] we did not note a significant reduction in pain at rest or pain during movement after the first exercise session. There was large variation in reported pain using the VAS which, combined with the relatively small sample size, may have been the reason a statistically significant change was not detected. It is also possible that the corrective exercise prescription may not have been ideal for every participant in the study. For example, in a clinical setting, it is customary for an EM exercise therapist to add or remove exercises from a patient’s E-cise menu based on effectiveness and feedback from the patient. In our study, participants were given an unmodified E-cise menu that was generated by the ePeteTM software.
The results of this study agree with the majority of research on the effect of therapeutic exercise on chronic knee and hip pain. A metaanalysis of eight randomized control studies showed favorable results on hip pain for the exercise group over the control group (effect size=0.46; 95% CI=0.64-0.28) [19]. Similarly, a meta-analysis of 32 studies on exercise and knee pain produced an effect size of 0.40 (95% CI=0.30-0.50) for pain and 0.37 (95% CI=0.25-0.49) for function [20]. In our study, the exercise group showed reduced WOMAC scores with effect sizes of 0.93 (95% CI=1.58-0.28) for pain and 0.80 (95% CI=1.48-0.19) for function. These changes were statistically significant after controlling for potential confounding variables such as age, gender, BMI, past joint surgery, arthritis, and location of pain.
There are several important differences between this study and previous studies. The average follow-up time in the studies included in the meta-analyses [19,20] was 8 weeks, while our study lasted 2 weeks. We employed a two-week study to specifically evaluate the immediate and short-term effects of EM corrective exercises. The type of exercise therapy employed in previous studies was also different than the EM used in this study. All the studies included in the meta-analyses [19,20] used strengthening exercises on the muscles surrounding the painful joint and some included range of motion, aquatic, and aerobic exercises as well. There are currently no published studies, which use corrective exercises (e.g., E-cises) that address whole-body postural alignment as it relates to knee and/or hip pain.
There were notable strengths to this study, including the study design. This was a randomized trial, which allows for the possibility of a causal relationship. The results of this study may be inferred to a similar population of that used in the study. Several potential covariates (e.g., age, gender, BMI, past surgery, arthritis, and location of pain) were controlled for in the analysis of the data. A single test administrator performed all of the posture evaluations, which eliminated potential inter-rater measurement error.
There were also three potential limitations of this study. First, the short duration of this study, while sufficient to assess the short-term effect of EM corrective exercises on pain and perceived physical function, may not have been long enough to observe actual changes in postural alignment. Indeed, changes in postural alignment were not assessed but should be considered in future studies. Second, participants were instructed to maintain their current habitual lifestyle, but since they were free-living and not supervised, it is not possible to know if some outside activity in their daily lifestyle may have inadvertently increased or decreased their musculoskeletal pain levels. Third, participants completed most of the corrective exercise sessions unsupervised under free-living conditions; therefore, the researchers could not verify that all exercise sessions were actually completed as reported.
In summary, this study found that a two-week program of corrective exercises significantly reduced knee and hip pain and improved perceived functional ability. These improvements were observed after adjusting for age, BMI, location of pain, history of joint surgery, and the presence of arthritis. The EM appears to be a safe and effective treatment for chronic knee and hip pain. Future research is warranted to investigate the effects of the EM corrective exercises on posture and pain in other locations of the body (e.g., back, neck, and shoulders).
Future studies that involve long-term follow-up should be employed to determine whether or not beneficial effects are sustained over time. In addition, it is important that future EM corrective exercise research measure changes in postural alignment, more effectively document and statistically control various lifestyle variables, and directly supervise EM corrective exercise routines to confirm participation.
References
- Hootman JM, Helmick CG, Barbour KE, Theis KA, Boring MA (2016) Updated projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults, 2015-2040. Arthritis Rheumatol 68: 1582-1587.
- Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM (2019) The global burden of musculoskeletal pain-where to from here? Am J Public Health 109: 35-40.
- Husky MM, Ferdous Farin F, Compagnone P, Fermanian C, Kovess-Masfety V (2018) Chronic back pain and its association with quality of life in a large French population survey. Health Qual Life Outcomes 16: 195.
- Peat G, McCarney R, Croft P (2001) Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 60: 91-97.
- Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A (2010) Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am 92: 1162-1169.
- Losina E, Weinstein AM, Reichmann WM, Burbine SA, Solomon DH, et al. (2013) Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res 65: 703-711.
- Egoscue P (1993) The Egoscue Method of health through motion: revolutionary program that lets you rediscover the body's power to rejuvenate it. HarperCollins Publisher, New York City, NY.
- Smith AJ, O'Sullivan PB, Campbell A, Straker L (2010) The relationship between back muscle endurance and physical, lifestyle, and psychological factors in adolescents. J Orthop Sports Phys Ther 40: 517-523.
- Twomey LT (1992) A rationale for the treatment of back pain and joint pain by manual therapy. Phys Ther 72: 885-892.
- Kendall FP, McCreary EK, Provance PG (1993) Muscles: Testing and function, Fourth edition. Lippincott Williams & Wilkins, Philadelphia, PA.
- Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA (1992) Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther 72: 425-431.
- Guimond S, Massrieh W (2012) Intricate Correlation between Body Posture, Personality Trait and Incidence of Body Pain: A Cross-Referential Study Report. PLoS One 7: 8.
- Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D (2010) The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br J Sports Med 44: 376-381.
- Kluemper M, Uhl T, Hazelrigg H (2006) Effect of stretching and strengthening shoulder muscles on forward shoulder posture in competitive swimmers. J Sport Rehabil 15: 58.
- Kuo YL, Tully EA, Galea MP (2009) Sagittal spinal posture after Pilates-based exercise in healthy older adults. Spine 34: 1046-1051.
- Scannell JP, McGill SM (2003) Lumbar posture - Should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living. Phys Ther 83: 907-917.
- Moustafa IM, Diab AA, Hegazy F, Harrison DE (2018) Does improvement towards a normal cervical sagittal configuration aid in the management of cervical myofascial pain syndrome: a 1- year randomized controlled trial. BMC Musculoskelet Disord 19: 396.
- Diab AA, Moustafa IM (2012) The efficacy of forward head correction on nerve root function and pain in cervical spondylotic radiculopathy: a randomized trial. Clin Rehabil 26: 351-361.
- Hernandez-Molina G, Reichenbach S, Zhang B, Lavalley M, Felson DT (2008) Effect of therapeutic exercise for hip osteoarthritis pain: results of a meta-analysis. Arthritis Rheum 59: 1221-1228.
- Fransen M, McConnell S (2008) Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev 4: 125.
- Wallis JA, Taylor NF (2011) Pre-operative interventions (non-surgical and non-pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery-a systematic review and meta-analysis. Osteoarthritis Cartilage 19: 1381-1395.
- Gill SD, McBurney H (2013) Does exercise reduce pain and improve physical function before hip or knee replacement surgery? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil 94: 164-176.
- Hasegawa M, Yamazaki S, Kimura M, Nakano K, Yasumura S (2013) Community-based exercise program reduces chronic knee pain in elderly Japanese women at high risk of requiring long-term care: A non-randomized controlled trial. Geriatr Gerontol Int 13: 167-174.
- Hurley MV, Walsh NE, Mitchell H, Nicholas J, Patel A (2012) Long-term outcomes and costs of an integrated rehabilitation program for chronic knee pain: A pragmatic, cluster randomized, controlled trial. Arthritis Care Res 64: 238-247.
- Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, et al. (2000) Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med 132: 173-181.
- Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, et al. (2005) Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis 64: 29-33.
- Ferraz MB, Quaresma MR, Aquino LRL, Atra E, Tugwell P, et al. (1990) Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol 17: 1022-1024.
- Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, et al. (1978) Studies with pain rating scales. Ann Rheum Dis 37: 378-381.
- Bellamy N (1989) Pain assessment in osteo-arthritis-Experience with the WOMAC osteo-arthritis index. Semin Arthritis Rheum 18: 14-17.
- Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to anti-rheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15: 1833-1840.
- Sahrmann S (2002) Diagnosis and treatment of movement impairment syndromes. St Louis, Mosby.
- Lau KT, Cheung KY, Chan KB, Chan MH, Lo KY, et al. (2010) Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Man Ther 15: 457-462.
- Egoscue P, Gittines R (1988) Pain free: A revolutionary method for stopping chronic pain. Bantam Books, New York.
- Shipp KM (2011) Actions and exercises to improve posture. International Council on Active Aging. Functional U 9: 1-13.
Citation: Vehrs Z, Hager RL, George JD, Myrer JW, Vehrs PR, et al. (2019) Effect of a Short-term Corrective Exercise Program on Chronic Knee and Hip Pain. J Nov Physiother 9: 404 DOI: 10.4172/2165-7025.1000404
Copyright: © 2019 Vehrs Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4330
- [From(publication date): 0-2019 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 3574
- PDF downloads: 756