Research Article Open Access
Effect of 12-Week Lifestyle Intervention on Behavioral, Anthropometry and Biochemical Profile of School Children in Chandigarh, India
Prabhushankar T1, Thakur JS1*, Jaswal N1, Bharti B2 and Bhansali A31School of Public Health, Postgraduate Institute of Medical Education and Research, Chandigarh, India
2Advanced Pediatric Center, Postgraduate Institute of Medical Education and Research, Chandigarh, India
3Department of Endocrinology, PGIMER, Chandigarh, India
- *Corresponding Author:
- Jarnail Singh Thakur, Professor
School of Public Health
Postgraduate Institute of Medical Education and Research
Chandigarh, India
Tel: +91-946-360-2173
E-mail: jsthakur64@gmail.com
Received date: July 01, 2015 Accepted date: September 16, 2015 Published date: September 29, 2015
Citation: Prabhushankar T, Thakur JS, Jaswal N, Bharti B, Bhansali A (2015) Effect of 12-Week Lifestyle Intervention on Behavioral, Anthropometry and Biochemical Profile of School Children in Chandigarh, India. J Community Med Health Educ 5:367. doi: 10.4172/2161-0711.1000367
Copyright: © 2015 Prabhushankar T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Objective: The present study assessed the effect of a 12 weeks lifestyle intervention program on health behavior, anthropometric measures and biochemical profile in selected schools.
Study Design: A community-based intervention study. 8 schools were randomly allotted to control or intervention group. Sample size of 180 students in each group were assessed for health behavior, anthropometry and biochemical profile. Students in intervention group were subjected to lifestyle intervention comprising of life skill sessions, lifestyle diary, physical activity period daily, healthier option in school canteen, etc., followed by post assessment.
Results: 384 students were enrolled (191 from intervention and 193 from control schools). 97% of them were evaluated at the end of the intervention. A significant increase in the behavior of children playing out in free time was found (p<0.05). Significant number of children started watching television for <2 hours (p<.0001.)Proportion of children who opted for fruits in case food was not prepared at home increased from 57.4% to 67.9% (p<.05). No significant changes in the biochemical and anthropometric parameters were found.
Conclusions: 12-week lifestyle intervention is feasible in school settings and helped in changing health behavior of the students. Longer duration of intervention may be required for change in anthropometry and biochemical profile.
Keywords
Lifestyle; Intervention; Behavioral; Anthropometry; Biochemical
Introduction
Early interventions are critical to improve health, nutrition and development of young children. This fact is substantiated in the World Development Report 2007 while focusing on ages 12-24 years which states that ‘decisions during five youth transitions have the biggest long term impact on how human capital is kept safe, developed and deployed…’ and that ‘policies and institutions affect the risks, the opportunities and the outcomes of youth and their families’[1].
There are over 1.2 billion adolescents aged 10–19 years in the world, constituting 18 per cent of world population. Worldwide, at least 12% of the adolescents are living with a chronic condition both as a function of the increasing incidence and improving survival after childhood and adolescent illnesses [2]. The Global School Health Survey (2007) in CBSE schools across India revealed that 1.5% of the students aged 13-15 years were overweight and around 7-8% of them were at risk of being overweight. It also revealed that only 30% of the students were physically active for at least 60 minutes per day on all 7 days of a week. Around 4% of the students use some form of tobacco, of which 1.5% of students were known to smoke [3].
School settings have long been recommended as an excellent health promoting environment where promoting healthy eating can be an integral and acceptable component of school curriculum [4]. Various strategies have been adopted like office based motivational interviewing by pediatricians, hospital based interventions and school based interventions [5-7]. A lot of school based lifestyle intervention programs have been successful in many parts of the world and a new framework for health promoting schools has been prepared by WHO India and Central Board of Secondary Education. ‘Trim and Fit’ program is a school based lifestyle intervention program implemented throughout Singapore and has successfully resulted to decrease in the prevalence of obesity among school children [8].
The present study aimed to implement a 12 weeks long, short-term, school-based lifestyle intervention program among selected school children and assess its effect on their changing health behavior and various anthropometric measures.
Materials and Methods
This community-based intervention study was carried out in UT Chandigarh (India) from July 2008 to March 2009 including a 12-week long health promotion intervention program.
Union Territory of Chandigarh has a total of 187 schools (107 public, 72 private, 7 aided schools and 1 Jawahar Navodhaya Vidhalaya) in Chandigarh [9-13]. A written permission was taken from the DPI, Schools and School Health Program Officer, UT Chandigarh to undertake the study. Short listing of schools (10 governments and 10 private) was done according to their proximity to the field practice area of the School of Public Health, PGIMER. First eight schools (4 governments and 4 private) that consented were enrolled for the study. These schools were then randomly allotted to control or intervention group by toss of coin.
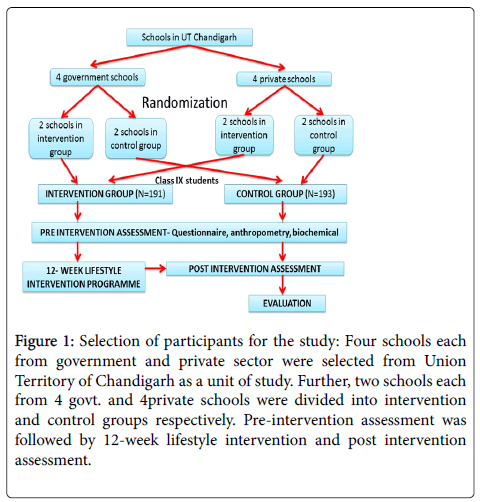
The prevalence of unhealthy lifestyle pattern in urban adolescents is 75% [14]. At the end of the intervention program, this prevalence is expected to reduce to 50%. Taking 95% confidence interval and 0.05 as allowable level of error, the sample size required in each group was 60. As it was a randomized cluster, thrice the calculated sample was taken to minimize the bias. So sample size decided was 180 for each group. So, a class IX or a section containing 45-50 students (13-15 yrs.) was selected from each school. Figure 1 shows the flowchart of selection of participants for the study. A baseline assessment of behavioral, anthropometric and biochemical measurements was taken before the intervention.
Figure 1: Selection of participants for the study: Four schools each from government and private sector were selected from Union Territory of Chandigarh as a unit of study. Further, two schools each from 4 govt. and 4private schools were divided into intervention and control groups respectively. Pre-intervention assessment was followed by 12-week lifestyle intervention and post intervention assessment.
Modified version of Questionnaire for Health Behavior Survey developed under the WHO India framework was used for data collection before and after the intervention period. WHO BMI growth charts for children was used to study the nutritional status of the children.
Lifestyle intervention
The intervention group was subjected to 12 week long lifestyle intervention program. Fortnightly sessions on life skills education and health education were organized. Total of 6 interactive sessions were held pertaining to sensitization session for parents; food and nutrition, physical fitness and know your body; avoiding tobacco and alcohol and being responsible and safe; awareness on personal hygiene and environment and behavior and life skills.
A lifestyle diary was developed by the investigator in which the child’s daily diet and physical activity was self-recorded for a period of three months and monitored by class teacher on weekly basis. 10% of the diaries were checked by the investigator on a monthly basis.
The school administration was requested to arrange for one physical activity period daily for the participating children. On holidays, the children were encouraged physical activity at home. The menu in the school canteen was replaced with healthier food options like milk and milk products, lasi, fruit chats, sprouts. During sensitization session of the parents, they were advised to motivate their children to reduce TV watching hours.
All the study subjects were re-assessed for behavioral, anthropometric and biochemical indicator after 12 weeks.
Ethical approval
This study was approved by the Institute’s Ethics Committee. Permission was taken from the respective schools and informed consent was taken from the parents/guardians of all school students.
Analysis
SPSS 16 software was used to analyze the data. For categorical variable, chi-square test was used. For continuous variable, z test was used to compare two means. Prevalence rates were given in percentages. All the p values were two tailed and considered significant when values are less than 0.05.
Results
A total of 384 students were enrolled in the study (191 from intervention schools and 193 from control schools). A total of 371 students (97% of the baseline) were evaluated at the end of the intervention. The age and sex distribution of the study participants is given in Table 1.
| Age (in yrs.) | Intervention group | Control group | ||||
|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | |
| 13 yrs. | 16 (8.4%) | 19 (10%) | 35 (18.4%) | 18 (9.3%) | 22 (11.4%) | 40 (20.7%) |
| 14 yrs. | 65 (34.2%) | 54 (28.4%) | 119 (62.6%) | 55 (28.5%) | 52 (27.5%) | 108 (56%) |
| 15 yrs. | 26 (13.3%) | 11 (5.7%) | 37 (19%) | 30 (15.5%) | 15 (7.8%) | 45 (23.3%) |
| Total | 107 (55.9%) | 84 (44.1%) | 191 (100%) | 103 (53.3%) | 90 (46.7%) | 193 (100%) |
Table 1: Age and sex distribution of the students in intervention and control groups.
The age of the students ranged from 13-15 years in both the groups. 55.9% and 53.3% of the students were males in intervention and control groups respectively. Most of the students were 14 years old (62.6% in the intervention group and 56% in the control group).
Table 1 gives the age-wise as well as sex-wise distribution of the students enrolled in the intervention group as well as the control group in the present study.
Table 2 shows the change in the health behavior of the school children in both the groups after the intervention. There was a significant increase in the behavior of children to play outside when they had free time from 33% to 45% (p<0.05). This is in contrast to the control group where there was a reduction in the number of children opting to play outside during free time. There was 20% increase from the baseline in the proportion of children who did some kind of physical activity (p<0.0001). In the intervention group, 18% of the children started watching television for less than 2 hours after intervention (p<0.0001). The health behavior of school children regarding food and nutrition has shown a significant rise in the proportion of children who never skipped their breakfast from 56% to 68.5% (p<0.05) contrary to no change in the control group (p=0.6). The proportion of children who opted for fruits in case food was not prepared at home also increased from 57.4% at baseline to 67.9% (p<0.05) in intervention group against reduction in fruit intake among the school children in the control group. About 16.3% of the students in the intervention group had also restricted their frequency of intake of fast foods to once a month (p<0.001). Regarding behavior and life skills 22% of the children no more found it difficult to handle things that resulted from their body (p<0.0001).
| Theme | Health behavior improved | Intervention group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-intervention (N=191) | Post-intervention (N=184) | Change% (Post-Pre) | P value | Pre-intervention (N=193) | Post-intervention (N=187) | Change% (Post-Pre) | P value | ||
| Physical activity | Playing outside in free time | 63 (33%) | 83 (45.1%) | 12.10% | <0.05 | 68 (35.2%) | 51 (27.3%) | -7.90% | 0.1 |
| Do some kind of physical activity | 42 (22.5%) | 68 (37.5%) | 20% | <0.0001 | 50 (25.9%) | 54 (28.9%) | 3% | 0.6 | |
| Television watching hours (<2 hrs.) | 107 (56%) | 136 (73.9%) | -17.90% | <0.0001 | 102 (52.8%) | 106 (56.7%) | 3.90% | 0.2 | |
| Food and nutrition | Never skip breakfast | 107 (56%) | 126 (68.5%) | 12.50% | <0.05 | 106 (54.9%) | 108 (57.8%) | 2.90% | 0.6 |
| Prefer fruits when food not prepared at home | 109 (57.4%) | 125 (67.9%) | 10.50% | <0.05 | 118 (61.2%) | 113 (60.4%) | -0.80% | 0.9 | |
| Fast food intake less than once a month | 55 (28.8%) | 83 (45.1%) | 16.30% | <0.001 | 39 (20.2%) | 44 (23.5%) | 3.30% | 0.4 | |
| Behavior and skills | Handling things resulting from body changes | 41 (21.5%) | 80 (43.5%) | 22% | <0.0001 | 73 (37.8%) | 55 (29.4%) | -8.40% | 0.08 |
| Supporting a friend with HIV | 124 (64.9%) | 169 (91.8%) | 26.90% | <0.0001 | 141 (73.4%) | 159 (85%) | 11.60% | <0.01 | |
| Know your body | Never Attributing any wrong thing to themselves | 25 (13.1%) | 59 (32.1%) | 19% | <0.0001 | 41 (21.2%) | 42 (22.4%) | 1.20% | 0.8 |
| Knowledge about risk factors | Formula for calculating BMI | 48 (25.1%) | 139 (75.5%) | 50.40% | <0.0001 | 46 (23.8%) | 45 (24.1%) | 0.30% | 0.8 |
| Other name for NCDs | 58 * | 162* | +104* | * | 13* | 10* | -3* | * | |
| Naming the NCDs | 300* | 417* | +117* | * | 343* | 364* | +21* | * | |
| Risk factors of NCDs | 284* | 384* | +100* | * | 231* | 129* | -102* | * | |
*Scores were computed for these parameters
Table 2: Changes in the health behavior of the school children in both the groups after the intervention.
Table 2 presents the knowledge of the students on the indicators of physical activity, health and nutrition, behavior and skills, body and risk factors before and after the intervention and relative change in the health behavior of both intervention and control group of school children.
The intervention also resulted in a significant change in the attitude of the students towards HIV/AIDS. At baseline, 30.4% of the students reported that they would stop talking to their friend if they knew that he had HIV/AIDS, but post-intervention only 4.4% of the children reported the same (p<0.0001). Also those children now said that they would provide all possible support to their friend with HIV/AIDS. In the control group too, there was an increase in the same attitude but the significance level was lesser as compared to the intervention group (p<0.05). The intervention produced a significant change in the attitude of the children towards their body. At baseline, only 13.1% children thought that when anything wrong happened to you, it was not because of them which increased to 32.1% post-intervention (p<0.0001). Regarding knowledge of school children about risk factors, MCQs on risk factors were asked from the children, a scoring pattern was assigned to analyze these questions.
A score of +1 was given to each right option, -1 to each wrong option, a net score of 0 was given to that student and so on. The children were asked to choose the correct formula for BMI. At baseline, only 25.1% of the children knew the correct formula for BMI which tripled after the intervention to 75.5% in the intervention group. But it remained the same as in baseline among the control group children. The score of school children on naming of risk factors increased from 300 before intervention to 417 after the intervention. In the intervention group, the scores of students on the knowledge about risk factors of NCDs improved from 284 to 384 after the intervention. However, this score decreased in the control group. It was 231 before the intervention and decreased to 129 after the intervention.
The anthropometric parameters of the study children were compared before and after study (Table 3). In the intervention group, a reduction in the mean weight of children by 0.62 kg was observed, though this reduction was insignificant. But in the control group, the mean weight of the children increased by 0.97 kg. Similarly, the mean BMI of the school children also reduced from 18.96 to 18.76 in the intervention group, and this reduction was again insignificant. In the control group, the mean BMI increased from a baseline level of 18.71 to 19.02 after the intervention. The waist hip ratio of the intervention children showed a slight insignificant rise from a mean level of 0.70 to 0.80, while it remained the same at 0.86 in the control group, before and after the intervention period.
| Theme | Health behavior improved | Intervention group | Control group | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-intervention (N=191) | Post-intervention (N=184) | Change% (Post-Pre) | P value | Pre-intervention (N=193) | Post-intervention (N=187) | Change% (Post-Pre) | P value | ||
| Anthropometry | Weight (Kg) [Mean(SD)] | 47.25 (11.02) | 16.63 (10.92) | -0.62 | 0.6 | 46.35 (8.98) | 47.32 (9.33) | 0.97 | 0.3 |
| Body Mass Index [Mean(SD)] | 18.96 (2.91) | 18.76 (2.83) | -0.2 | 0.6 | 18.71 (2.82) | 19.02 (2.99) | 0.3 | 0.3 | |
| Waist Hip Ratio [Mean(SD)] | 0.79 (0.12) | 0.80 (0.05) | 0.01 | 0.5 | 0.86 (0.07) | 0.86 (0.06) | 0 | - | |
| Biochemical measurements | Pre-intervention (n=81) | Post-intervention (n=184) | Change% (Post-Pre) | P value | Pre-intervention (N=193) | Post-intervention (N=187) | Change% (Post-Pre) | P value | |
| Total Cholesterol | 148.11 (25.54) | 152.38 (29.51) | 4.2 | 0.3 | 145.76 (19.42) | 149.22 (32.99) | 3.46 | 0.6 | |
| [Mean(SD)] | |||||||||
| HDL | 37.62(5.85) | 39.23(6.05) | 1.6 | 0.1 | 40.65 (6.66) | 39.18 (7.31) | -1.37 | 0.3 | |
| [Mean(SD)] | |||||||||
| LDL | 90.99(22.64) | 90.83(25.82) | -0.16 | 0.96 | 89.97 (14.81) | 94.18 (31.29) | 4.19 | 0.4 | |
| [Mean(SD)] | |||||||||
| VLDL | 19.5(9.59) | 21.85(11.6) | -2.35 | 0.06 | 15.14 (7.08) | 15.48 (3.23) | 0.34 | 0.8 | |
| [Mean(SD)] | |||||||||
| Triglycerides | 97.5(47.93) | 96.99(26.42) | -0.51 | 0.9 | 75.69 (35.41) | 78..48 (18.3) | 2.78 | 0.7 | |
| [Mean(SD)] | |||||||||
Table 3: Changes in the anthropometric and biochemical parameters of the school children in both groups after the intervention.
Table 3 shows the mean scores of the school children on anthropometry and biochemical parameters before and after the intervention in the present study and relative change in the parameters both among the intervention and control group.
Changes in the biochemical parameters of children are shown in Table 3. The intervention produced a rise in the mean HDL levels from 37.62 mg to 39.23 mg albeit statistically insignificant (p=0.1). The mean triglyceride level also showed reduction in the intervention group. All other parameters showed a slight increase in the intervention group, however they were not statistically significant. In the control group, it was observed that all the biochemical measurements showed an increase except HDL which was reduced by 1.47 mg, although the difference was not statistically significant.
Discussion
The study was a community-based intervention study to assess the effect of a short term, school based lifestyle intervention program on the health behavior and anthropometric measurements of school going adolescents and determine the factors influencing adoption of healthy lifestyle practices among the school going adolescents. A total of 384 students were enrolled in the study (191 in intervention group and 193 in control group. The age of the participating children varied from 13-15 years in both the groups. 371 participants were evaluated after the intervention. This reduction was due to the daily variation in the attendance of the school children. However, the follow up rate of 96.6% was achieved.
Awareness was created among the children after the intervention that physical activity can be routinely implemented in daily life. There was a statistically significant increase in the behavior of children to play outside when they had free time (p<0.05). The children were encouraged by the parents at home as they had been explained the beneficial effects of physical games and harmful effects of playing computer games. There was 20% increase from the baseline in the children who did some kind of physical activity, of which 15% did it regularly. The children had also been taught simple physical exercises. The children had also been taught simple physical exercises during the sessions which could be easily done at home.
A similar increase in physical activity was observed in CATCH study [15], where the time spent in moderate physical activity in physical education classes increased from 40% to 50% after the intervention. In the intervention group, 20% of the children started watching television for less than 2 hours after intervention. Another school health program-Planet Health also produced similar reduction in television watching and this was possible due to efforts of the parents [6]. This shows that parents are also vital stakeholders in a school based intervention program. But behavior change should be facilitated in children regarding TV watching rather than through enforcement by parents. Substitution of this leisure time with outdoor games should be promoted and caution should be taken that parents might very well exploit their children to academic activities and shun their leisure activity.
After the intervention, there has been significant rise in the proportion of children who never skipped breakfast from 56% to 68.5%. During the session on diet, it was found that most children were skipping breakfast to reduce weight and having an excuse of getting late to school. But the importance of taking breakfast was clearly explained during the sessions. The proportion of children who opted for fruits in case food was not prepared at home also increased from 57.4% at baseline to 67.9% and fruit intake among children. About 16.3% of the students in the intervention group had also restricted their frequency of intake of fast foods to once a month and this change in the behavior being very significant. This change could be attributed to the intervention in the schools’ canteen, support from the parents and the awareness generated among the children regarding harmful effects of junk food. Other studies have also resulted in increased fruit intake in children like Be Smart [16], CATCH [15], and APPLES [17].
In the intervention group, 22% of the children no more found it difficult to handle things that resulted from their body in adolescent changes and this change was statistically significant. This was one area which had not been studied in any other study. The intervention also resulted in a significant change in the attitude of the students towards HIV/AIDS. At baseline, 30.4% of students reported that they would stop talking to their friend with HIV/AIDS and post-intervention only 4.4% reported the same and this change was statistically significant. This could be attributed to external factors like the mass media where a lot of advertisements of National AIDS Control Program reflect the same things. The intervention produced a significant change in the self-reported attitude of children towards their body. At baseline, only 13.1% of children thought that when anything wrong happened to them, it was not because of them which increased to 32.1% after the intervention, being a significant change. This area needs a lot of intervention and the children need more counseling on personality.
There was improvement in the score of the children on knowledge regarding risk factors of chronic NCDs in the intervention group while compared to the control group, where knowledge level either remained the same or decreased. After the intervention, children atleast had known as to how NCDs were otherwise known as and the common NCDs and the associated risk factors. This awareness on lifestyle diseases among school children is very essential as it would help them figure out NCDs from fever and infections and they would be able to incorporate healthy lifestyle practices into their daily lives [18]. There was a significant increase in the proportion of children knowing the correct formula of calculating BMI. It was 25.1% at baseline and increased to 75.5% after the intervention. It was primarily because of the lifestyle diary where the children were asked to calculate their own BMI and plot on charts.
Blood sampling was done in 50% of the intervention group and 25% of the control group. As a pleasant surprise, almost all the parents consented to blood sampling in their children, in contrary to the popular myth that consent rates would be low due to apprehensions among the parents. A proper explanation and advantages of biochemical testing always helps to meet the objective. But there was no significant change in the biochemical parameters like lipid profile and blood sugar in the children after the intervention. The Kids N Fitness Program was a family centered lifestyle intervention which evaluated the effect of the program on 8-16 year old children and it produced significant changes in some parameters like total cholesterol, LDL and triglycerides, thus showing that even family-centered programs which are very intensively structured have lesser impact on such parameters [19].
There was no significant change in the anthropometric indicators like weight, BMI and waist hip ratio after the intervention. It is the short time period of intervention that could be attributed to the insignificant change achieved in all these parameters. Various studies have shown that most of the studies with shorter intervention periods have been ineffective in reducing the mean BMI of the children [20,21]. It clearly outlines the role of other factors in producing change in such parameters.
The present study concludes that 12-week lifestyle intervention is feasible in school settings and helped in changing health behavior of the students. Longer duration of intervention may be required for change in anthropometry and biochemical profile.
Conclusion
12-week lifestyle intervention is feasible in school settings and helped in changing health behavior of the students. Longer duration of intervention may be required for change in anthropometry and biochemical profile.
Acknowledgements
The authors would like to acknowledge the support of School Health Program Officer and Chandigarh Administration in planning as well as implementation of the study.
Authors’ Contributions
PT contributed by preparing study design, data collection, data analysis and report writing. JS contributed to conceptualizing the proposal and developing, writing and editing the final draft of the paper. NJ contributed to data analysis and writing of paper. BB and AB participated in implementing, supervising and editing the paper.
References
- (2007) World Bank Report. Development and the next generation. Oxford University Press, New York, USA.
- Sawyer SM, Drew S, Yeo MS, Britto MT (2007) Adolescents with a chronic condition: Challenges living, challenges treating. The Lancet 369: 1481-9.
- World Health Organization. India (CBSE) 2007 Fact Sheet. Global School-based Student Health Survey.
- WHO Consultation on obesity (1998) Special Issues in the management of obesity in childhood and adolescence. In: Obesity preventing and managing the global epidemic. Geneva; WHO, 231-247.
- Schwartz RP, Hamre R, Dietz WH, Wasserman RC, Slora EJ, et al. (2007) Office based motivational interviewing to prevent childhood obesity. Arch paediatr Adolesc Med. 161:495-501.
- Luepker RV, Percy CL, Mckinlay SM, Nader PR, Parcel GS, et al. (1996) Outcomes of a field trial to improve children’s dietary pattern and physical activity. The child and adolescent trial for cardiovascular health. CATCH collaborative group. JAMA 275:768-76.
- Reilly JJ, Kelly L, Montgmery C, Williamson A, Fisher A, et al. (2006) Physical activity to prevent obesity in young children: cluster randomized controlled trial. BMJ 333:1041.
- Toh CM, Cutter J, Chew SK (2002) chool based interventions has reduced obesity in Singapore. BMJ 324: 427.
- (2011) Census of India. Census Data: Chandigarh, Office of the Registrar General and Census Commissioner. New Delhi: Logic Soft International.
- (2011) Sample Registration System. (2011) SRS Bulletin (December, 2011). New Delhi, India: Office of the Registrar General of India.
- Jaiswal A (2011) Referral cases jack up maternal deaths at GMCH. The Tribune.
- Official website of Chandigarh Administration. Department of Education Chandigarh Administration. Schools.
- Dhingra V, Chatterjee A, Guleria R, Sharma R, Pandey RM, et al. (2002) Adverse physical activity pattern in urban adolescents. J Assoc Phys India 50:1521.
- Golan M, Weizman A, Apter A, Fainaru M (1998) Parents as exclusive agents of change in the treatment of childhood obesity. American Journal of Clinical Nutrition 67, 1130-1135.
- Nader PR, Stone EJ, Lytle LA, Perry CL, Osgnanian SK, et al. (1999) Three-year maintenance of improved diet and physical activity: The CATCH cohort. Child and adolescent trial for cardiovascular health. Arch Pediatr Adolesc Med 153: 695-704.
- Gary DF, Sherman S, Kelly EB, Karen MG, Stephanie VVS, et al. (2008) A policy-based school intervention to prevent overweight and obesity. Pediatrics 121:e794-802.
- Divakaran B, Muttapillymyalil J, Sreedharan J, Shalini K (2010) Lifestyle risk factors of non-communicable diseases: awareness among school children. Indian J Cancer 47 Suppl 1:9-13.
- Monzavi R, Dreimane R, Geffner ME, Braun S, Conrad B, et al. (2006) Improvement in risk factors for metabolic syndrome and insulin resistance in overweight youth who are treated with lifestyle intervention. Pediatrics 117: 1111-8.
- Dyer T, Coonan WE, Leitch DR, Hetzel BS, Baghurst RA (1983) An investigation of the effects of daily physical activity on the health of primary school students in South Australia. Int J Epidemiol 12: 308-313.
- Harrell JS, McMurray RG, Bangdiwala SI, Frauman AC, Gansky SA, et al. (1996) Effects of a school-based intervention to reduce cardiovascular disease risk factors in elementary-school children: the cardiovascular Health in Children (CHIC) study. J Pediatr 128: 797-805.
- McMurray RG, Harrell JS, Bangdiwala SI, Bradley CB, Deng S, et al. (2002) A school-based intervention can reduce body fat and blood pressure in young adolescents. J Adolesc Health 31:125-132.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 15024
- [From(publication date):
October-2015 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 10348
- PDF downloads : 4676