Dysphagia with White Esophageal Exudates: An Eosinophilic Esophagitis Mimic Treated with a Proton-Pump Inhibitor
Received: 23-Feb-2021 / Manuscript No. JGDS-23-26661 / Editor assigned: 26-Feb-2021 / PreQC No. JGDS-23-26661(PQ) / Reviewed: 12-Mar-2021 / QC No. JGDS-23-26661 / Revised: 15-May-2023 / Manuscript No. JGDS-23-26661(R) / Published Date: 12-Jun-2023 QI No. / JGDS-23-26661
Abstract
Eosinophilic Esophagitis (EoE) is a major cause of dysphagia and food impaction. Recognition and diagnosis of EoE have been increasing rapidly, but the role of Proton Pump Inhibitors (PPIs) for the diagnosis of EoE and treatment of esophageal eosinophilia remains controversial. Initial diagnostic algorithms for EoE relied on a PPI trial to distinguish EoE from gastroesophageal reflux disease, a common cause of esophageal eosinophilia.
Keywords: Eosinophilic esophagitis; Proton pump inhibitors; Esophageal eosinophilia; Dysphagia
Keywords
Eosinophilic esophagitis; Proton pump inhibitors; Esophageal eosinophilia; Dysphagia
Introduction
This approach has become complicated by the recent recognition of PPI-Responsive Esophageal Eosinophilia (PPI-REE), a disorder characterized by clinicopathologic features similar to EoE but that resolve with high-dose PPI therapy.The mechanism of PPI action for treatment of esophageal eosinophilia may rely not only on acid suppression but also on novel anti-inflammatory effects of the PPIs themselves. Treatment with PPI therapy is now considered a required step before a formal diagnosis of EoE can be made, and continuing PPI therapy in patients with PPI-REE is a common strategy [1,2]. However, the role of continuing PPI monotherapy in patients with EoE remains a matter of debate. The decision to do so should hinge on improvement in symptoms and histology as well as the need for ongoing dilation.
Case Presentation
A 39-year-old woman presented with a one-year history of solid food dysphagia, food avoidance, weight loss, and one episode of food impaction. Physical examination was unremarkable. Laboratory evaluation revealed a microcytic, iron deficiency anemia with normal differential. An esophagram showed delayed passage of a 13 mm barium tablet at the gastroesophageal junction. An upper endoscopy showed linear furrows and white exudates throughout the proximal and distal esophagus without narrowing [3,4]. The clinical presentation and endoscopic appearance raised suspicion for eosinophilic esophagitis. Biopsies obtained from throughout the esophagus showed squamous mucosa with spongiosis and increased intraepithelial lymphocytes (up to 60 per HPF) in peripapillary and interpapillary zones consistent with severe lymphocytic esophagitis [5]. Gastric and duodenal biopsies and colonoscopy were unremarkable. She was started on twice daily proton-pump inhibitor and oral iron therapy with resolution of symptoms and anemia.
Endoscopy follow-up at 12 weeks showed normal mucosa and biopsies. She remains asymptomatic [6,7].
Results and Discussion
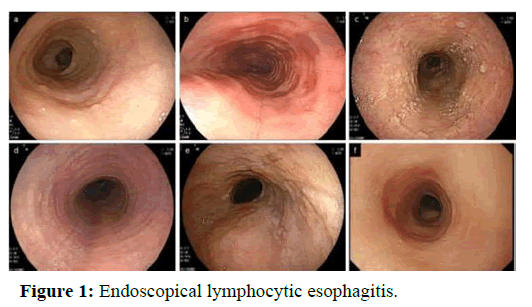
Lymphocytic esophagitis is a rare esophageal disorder that can clinically (dysphagia, food impaction) and endoscopically (white exudates, furrows) mimic eosinophilic esophagitis. Reported associations include esophageal motility disorders, medications, and inflammatory bowel disease. Proton pump inhibitors and topical corticosteroids have been invoked as therapies (Figure 1) [8].
Over the past several years, the approach to esophageal eosinophilia has become more complicated with the recognition of PPI-REE. This condition was first described in a series of 3 pediatric patients with clinical, endoscopic, and histologic features of EoE but who completely responded to a course of PPI treatment [9].
Since that time, retrospective and prospective studies in both children and adults consistently show that at least one-third of patients with esophageal eosinophilia respond to a course of high-dose PPIs. Although the mechanisms of this PPI response are currently being elucidated, the critical point is that patients with esophageal eosinophilia that responds to PPI therapy are currently not considered to have EoE. Specifically, guidelines require that patients undergo a PPI trial before they can receive a formal diagnosis of EoE. It is unclear, however, whether a patient has PPI-REE or GERD based on PPI response alone. It is also unclear if PPI-REE is a form of GERD, a subtype of EoE, a result of their interaction, or an independent condition. Adding to the confusion, PPI-REE can be a transient condition. Dohil and colleagues have presented a series of patients who had an initial response to PPI therapy, but on long-term followup, and in the absence of medication adherence issues, seasonality, changes in diet, or new allergen triggers, subsequently developed recurrent esophageal eosinophilia consistent with EoE in spite of ongoing PPI therapy for PPI-REE [10].
The role of proton pump inhibitor therapy for esophageal eosinophilia
In spite of the diagnostic uncertainty associated with EoE, GERD, and PPI-REE, there are benefits to PPI therapy in a subset of patients with esophageal eosinophilia. A review by Molina-Infante and colleagues indicated that the rate of symptom improvement in adults with esophageal eosino-philia who were treated with PPI therapy ranged from 25% to 80% and histologic remission from 33% to 61%, depending on the study design and patient population [11].
One of the most fascinating areas of emerging data concerns the mechanism of PPI response in patients with esophageal eosinophilia. For example, several studies have suggested that PPIs may have novel anti-inflammatory effects that are independent of their acid suppression. PPIs can act as antioxidants, directly inhibit neutrophils and monocytes, decrease expression of proinflammatory cyto-kines, and inhibit or kill multiple bacteria and fungi. PPIs also have been shown to inhibit eosinophil recruitment from blood to tissue, not just into the gastrointestinal tract but also into lung tissue and secretions. Specifically applicable to esophageal eosinophilia are studies that show that PPIs block Interleukin (IL)-4-and IL-13-stimulated secretion of eotaxin-3 in esophageal cell lines from patients with EoE, likely by impacting STAT6 binding to the eotaxin-3 promotor.
This not only provides a direct mechanism of action for the clinical improvement noted in patients who have PPI-REE8, but also potentially explains why it is difficult to predict which patients with suspected EoE will have a PPI response. Interestingly, the same eotaxin-blocking effect is not seen when PPIs are applied to a fibroblast culture system. The similarities between patients with EoE and some with PPI-REE are further highlighted by the fact that the same genes, including eotaxin-3 and Th2 cytokines, are down regulated after treatment. Finally, use of PPIs can restore esophageal mucosal barrier function in patients with esophageal eosinophilia, potentially decreasing the route of exposure for allergen triggers to inflammation.
Conclusion
The PPI response goes beyond the effect on histology and improvement in esophageal eosinophilia and leads to other clinical improvements as well. PPI therapy may play a role in combination therapy with patients who require dilation. In a systematic review examining dilation in patients with EoE, Bohm and Richter found that inflammation was reduced in patients who underwent dilation and PPI therapy but not in patients who underwent dilation alone.
References
- Kaplan M, Mutlu EA, Jakate S, Bruninga K, Losurdo J, et al. (2003) Endoscopy in eosinophilic esophagitis:“Feline” esophagus and perforation risk. Clin Gastroenterol Hepatol 1: 433-437.
[Crossref] [Google Scholar] [PubMed]
- Kuzumoto T, Tanaka F, Sawada A, Nadatani Y, Otani K, et al. (2021) Vonoprazan shows efficacy similar to that of proton pump inhibitors with respect to symptomatic, endoscopic, and histological responses in patients with eosinophilic esophagitis. Esophagus 18: 372-379.
[Crossref] [Google Scholar] [PubMed]
- Destek S, Gul VO, Ahioglu S, Tatar Z, Erbil Y (2014) A rare cause of chronic dysphagia: Eosinophilic esophagitis. J Surg Case Rep 2014: rju096.
[Crossref] [Google Scholar] [PubMed]
- Tomomatsu Y, Yoshino J, Inui K, Wakabayashi T, Kobayashi T, et al. (2013) Clinical features of eosinophilic esophagitis: Ten Japanese cases. Dig Endos 25: 117-124.
[Crossref] [Google Scholar] [PubMed]
- Pentiuk SP, Miller CK, Kaul A (2007) Eosinophilic esophagitis in infants and toddlers. Dysphagia 22: 44-48.
[Crossref] [Google Scholar] [PubMed]
- Sawada A, Hashimoto A, Uemura R, Otani K, Tanaka F, et al. (2019) Association between endoscopic findings of eosinophilic esophagitis and responsiveness to proton pump inhibitors. Endosc Int open 433-439.
[Crossref] [Google Scholar] [PubMed]
- Fujiwara Y, Hashimoto A, Uemura R, Sawada A, Otani K, et al. (1963) Optimal biopsy protocol to evaluate histological effectiveness of proton pump inhibitor therapy in patients with eosinophilic esophagitis. Digestion 100: 64-71.
[Crossref] [Google Scholar] [PubMed]
- Hruz P, Straumann A, Bussmann C, Heer P, Simon HU, et al. (2011) Escalating incidence of eosinophilic esophagitis: A 20-year prospective, population-based study in Olten County, Switzerland. J Allergy Clin Immunol 128: 1349-1350.
[Crossref] [Google Scholar] [PubMed]
- Van Rhijn BD, van Ree R, Versteeg SA, Vlieg‐Boerstra BJ, Sprikkelman AB, et al. (2013) Birch pollen sensitization with cross‐reactivity to food allergens predominates in adults with eosinophilic esophagitis. Allergy 68: 1475-1481.
[Crossref] [Google Scholar] [PubMed]
- Sayej WN, Patel R, Baker RD, Tron E, Baker SS (2009) Treatment with high-dose proton pump inhibitors helps distinguish eosinophilic esophagitis from noneosinophilic esophagitis. J Pediatr Gastroenterol Nutr 49: 393-399.
[Crossref] [Google Scholar] [PubMed]
- Moawad FJ, Schoepfer AM, Safroneeva E, Ally, MR, Chen YJ, et al. (2014) Eosinophilic oesophagitis and proton pump inhibitor‐responsive oesophageal eosinophilia have similar clinical, endoscopic and histological findings. Aliment Pharmacol Ther 39: 603-608.
[Crossref] [Google Scholar] [PubMed]
Citation: Shaker A, O’Dell K, Chopra S (2023) Dysphagia with White Esophageal Exudates: An Eosinophilic Esophagitis Mimic Treated with a Proton-Pump Inhibitor. J Gastrointest Dig Syst 13: 737.
Copyright: © 2023 Shaker A, et al. This is an openaccess article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1818
- [From(publication date): 0-2023 - Nov 17, 2025]
- Breakdown by view type
- HTML page views: 1483
- PDF downloads: 335