Dynamic Postural Instability in Individuals with High Body Mass Index
Received: 15-Mar-2018 / Accepted Date: 06-Apr-2018 / Published Date: 11-Apr-2018 DOI: 10.4172/2165-7025.1000387
Abstract
Objective(s): To evaluate and compare static and dynamic balance between individuals with high body mass index (BMI) and normal BMI.
Methods: This case-control study included 19 individuals with high BMI and 7 individuals with normal BMI. It was conducted at a regional level university setting. The center of pressure (COP) changes during double limb stance and single limb stance were obtained using a force plate (Brazil Do). The main COP outcome measures included total displacement, area of sway, amplitude, velocity, and mean power frequency changes in anteroposterior (AP) and mediolateral (ML) directions.
Results: During single limb stance, there was a significant difference in COP amplitude (cm) (p=0.015) and velocity (cm/s) (p=0.012) between the 2 groups in the AP direction. However, there were no significant differences found in the ML direction for amplitude (cm) (p=0.155) or velocity (cm/s) (p=0.186). There was no significant difference in the COP outcome measure for double limb stability for both the eyes closed and eyes opened conditions.
Conclusion: Individuals with high BMI have impaired dynamic balance control in the AP direction reflected through higher COP amplitude and velocity. They have preserved stability in the ML direction during single limb stance stability. The COP changes during the double limb stance are unimpaired, both with eyes opened and closed.
Keywords: Body mass index; Balance; Center of pressure; Posture
Introduction
Many health issues are linked to individuals with high body mass index (BMI). The BMI is a measure of an individual’s body fat when comparing height to weight. An individual is considered overweight with a BMI of 25-29.9 kg/m2 and obese if the BMI is ≥30 kg/m2. Higher BMI is associated with type 2 diabetes, high blood pressure, heart disease and stroke, some types of cancer, and kidney and liver diseases [1]. Evidence suggests that individuals with high BMI are more likely to have functional mobility impairments [2], impairments of gait [3], risk of falls [4] and impaired quality of life [5]. Fall-related injuries requiring medical care are experienced at a rate up to 79% greater for individuals with high BMI compared to those with normal BMI [6].
Postural stability is a primary factor in predicting fall risk and refers to one’s ability to maintain body position in time and space despite external forces [7,8]. Factors affecting postural stability include certain medications, vision, proprioception, strength, fatigue, levels of physical activity, and BMI [9,10]. When using the Berg Balance Scale (BBS) and Timed-Up and Go (TUG) as indicators of balance and functional mobility, no significant differences were found when comparing BMI and balance [11,12]. However, when looking specifically at postural stability, force plate analysis has been shown to be a better indicator of fall risk when compared to functional balance assessments [13,14]. Most studies use functional assessment tests rather than force plate analysis, limiting the amount of data available to assess postural stability. It has been suggested that center of pressure (COP)-based assessment can provide more detailed evidence of balance deficits than functional asssessments [13] and can identify a subclinical balance impairment [15]. Detailed information about biomechanical and neuromuscular components of postural stability can be gathered using force plate analysis of COP sway [14]. Increased COP sway in anteroposterior (AP) and mediolateral (ML) directions were reported when an additional weight was added to the subject using a backpack [16]. If increasing the weight of a backpack can increase COP displacement, it is possible that the same would be true for people with higher BMIs.
High BMI is one of the key factors contributing to falls due to its impact on balance, posture and mobility impairment [17], therefore, affecting the quality of life [5]. Higher prevalence of falls, stumbling in walking and decreased physical activity were found in individuals with obesity [5]. It was postulated that obese individuals have deficits in utilizing proprioceptive information for postural control [18]. In addition to muscle weakness and impaired mobility, the risk of falling increases with age and with higher BMI [19]. It is reported that plantar mechanoreceptors are impaired in obese individuals due to the continuous pressure of supporting a large mass, eventually contributing to the impairment of balance [20].
Since obesity has a strong association with decreased mobility, increased postural sway, and falls, this proposal explored the potential relationship of balance impairment and BMI. The purpose of this study to evaluate and compare static and dynamic balance between individuals with higher BMI and normal BMI controls. It was hypothesized that people with higher BMI’s would have significantly decreased postural stability as reflected by increases in COP sway.
Materials and Methods
Participants
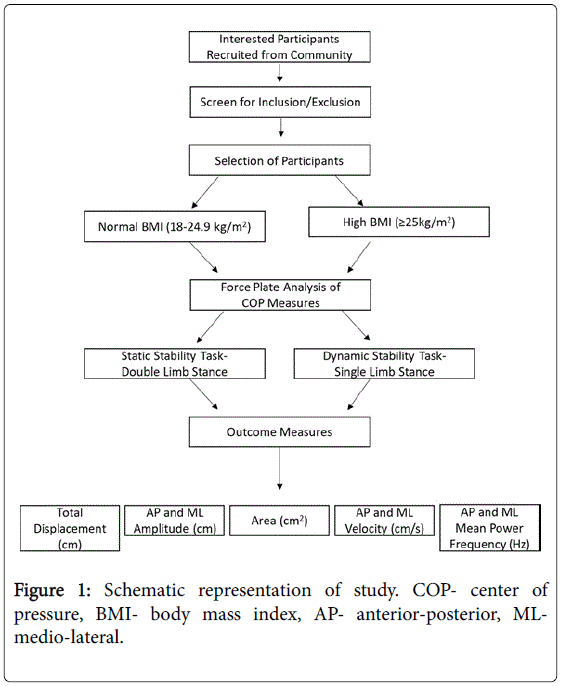
Nineteen individuals with high BMI and seven with normal BMI participated in this study (Figure 1).
The study was approved by the Institutional Review Board and written informed consent was obtained from each participant. Participants were recruited from the community after screening for the exclusion criteria and classified in either a high BMI group or normal BMI group. Participants were excluded if they had recent lower extremity injury/trauma/surgery within the last 6 months, lower extremity total joint replacement, neurologic conditions (including but not limited to stroke, multiple sclerosis, and neuropathy), or inability to walk 30 feet without an assistive device. The clinical characteristics of the participants were obtained (Table 1).
| Normal BMI group (mean ± SD) | High BMI group (mean ± SD) | p-value | |
|---|---|---|---|
| Age (yrs) | 63.0 ± 16.2 | 71.9 ± 8.2 | 0.07 |
| Height (cm) | 167.5 ± 7.6 | 162.6 ± 8.8 | 0.196 |
| Weight (kg) | 65.3 ± 7.5 | 81.9 ± 11.4 | 0.002 |
| BMI (kg/m2) | 23.2 ± 1.1 | 30.9 ± 3.6 | ˂0.001 |
| Gender | 1:06 | 3:16 | 1 |
| (male: female) | 1:6 | 3:16 | 1.00 |
BMI- body mass index; Normal 18- 24.9, High ≥ 25. Fisher exact test was used for gender distribution; t-test was used for continuous variable.
Table 1: Demographics and anthropometric details of the participants.
Experimental setup and procedure
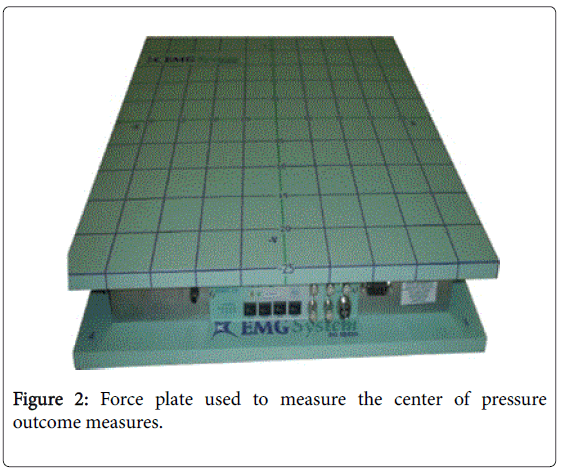
Static and dynamic balance was tested using COP changes during double limb stance and single limb stance for 10 seconds with a sampling frequency of 500 Hz using a force plate (Figure 2) (BIOMEC V16, Synergy Applied and Medical Research Inc., Brazil). The technical details of the force plate are published elsewhere [14]. The force plate contains load cells with an internal circuit that changes electrical resistance upon the application of a force.
During the static stability task, the participants were instructed to stand with their arms hanging loosely by their sides, with their palms oriented toward the body. During the tests, the subjects were instructed to maintain an upright stance while standing barefoot on the force platform with their feet shoulder-width apart. During double limb stance, COP data were collected with eyes open and eyes closed. During the dynamic stability task, the participants were instructed to stand on one leg based on their preference and continue using the same leg for each trial and task. In single limb stance, the data was collected with eyes open, only. The main COP outcome measures included total displacement (cm), area of sway (cm2), amplitude (cm), velocity (cm/sec), and mean power frequency (Hz) changes in AP and ML directions. Participants were guarded by the researchers for safety. Three trials of 10 seconds in duration were collected for each condition.
Data Processing and Analysis
The moments of forces were digitized with an analogue-to-digital converter and customized software (National Instruments, Austin TX, USA). MATLAB R2017a software (MathWorks, Natick, MA, USA) was used to analyze the COP data. Custom-made software was used to obtain COP outcome measures. The software includes low-pass filtering of COP data at 10 Hz with a Butterworth filter. After filtering, the COP total displacement, amplitude, sway area, mean velocity and mean power frequency in AP and ML directions were obtained. The COP total displacement was defined as the maximal displacement of the COP in all direction. The COP area was estimated by fitting an ellipse to the COP data that encompasses 95% of the data. The velocity of COP was derived by total COP displacement divided by the measurement time. The mean power frequency spectral density was calculated using the Welch periodogram method with a resolution of 0.039 Hz. The validity and reliability of all these parameters computed with this BIOMEC force platform have been established earlier [14].
Demographic information was assessed using descriptive statistics. An independent sample t-test was performed to see the difference between the individuals with high BMI and normal BMI. Statistical analyses were performed using IBM SPSS Version 24 (IBM, NY, USA) and the significance levels were set at p<0.05.
Results
Static standing stability
All the participants were able to perform all the trials of the static standing stability task. The results of COP analysis during double limb stance did not show any significant difference in the COP outcome measures for the eyes closed or eyes open conditions (Table 2).
| COP outcome measures | Static stability (double limb stance) | Dynamic stability (single limb standing) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Eyes opened | Eyes closed | Eyes opened | |||||||
| Normal BMI group | High BMI group | p-value | Normal BMI group | High BMI group | p-value | Normal BMI group | High BMI group | p-value | |
| Total Displacement (cm) | 12.49 ± 6.5 | 13.23 ± 5.5 | 0.775 | 13.56 ± 7.8 | 18.43 ± 7.8 | 0.17 | 49.75 ± 10.3 | 62.13 ± 18.6 | 0.12 |
| AP Amplitude (cm) | 1.15 ± 0.6 | 1.11 ± 0.4 | 0.871 | 1.1 ± 0.6 | 1.33 ± 0.8 | 0.479 | 2.84 ± 0.3 | 4.77 ± 2.6 | 0.015 |
| ML Amplitude (cm) | 1.49 ± 0.5 | 1.61 ± 0.3 | 0.467 | 1.54 ± 0.6 | 1.99 ± 0.6 | 0.086 | 3.6 ± 0.8 | 5.01 ± 2.5 | 0.155 |
| Area (cm2) | 1.97 ± 1.5 | 1.73 ± 0.9 | 0.622 | 1.61 ± 1.3 | 2.64 ± 3.0 | 0.395 | 8.55 ± 2.9 | 23.32 ± 18.5 | 0.011 |
| AP Velocity (cm/s) | 0.63 ± 0.3 | 0.63 ± 0.3 | 0.999 | 0.65 ± 0.3 | 0.76 ± 0.3 | 0.454 | 3.3 ± 0.9 | 4.43 ± 0.9 | 0.012 |
| ML Velocity (cm/s) | 0.97 ± 0.5 | 1.04 ± 0.5 | 0.72 | 1.07 ± 0.6 | 1.53 ± 0.7 | 0.129 | 3.32 ± 0.9 | 4.27 ± 1.7 | 0.186 |
| AP Mean Power Frequency (Hz) | 0.40 ± 0.06 | 0.44 ± 0.1 | 0.274 | 0.44 ± 0.1 | 0.48 ± 0.2 | 0.529 | 0.89 ± 0.2 | 0.91 ± 0.2 | 0.843 |
| ML Mean Power Frequency (Hz) | 0.44 ± 0.2 | 0.49 ± 0.2 | 0.521 | 0.5 ± 0.1 | 0.62 ± 0.2 | 0.097 | 0.9 ± 0.3 | 0.82 ± 0.3 | 0.496 |
COP- center of pressure; AP- anterior-posterior; ML- medio-lateral. Significant p values are shown in bold.
Table 2: Force plate analysis of center of pressure outcome measures during static and dynamic standing task in individuals with normal BMI and high BMI groups.
Dynamic standing stability
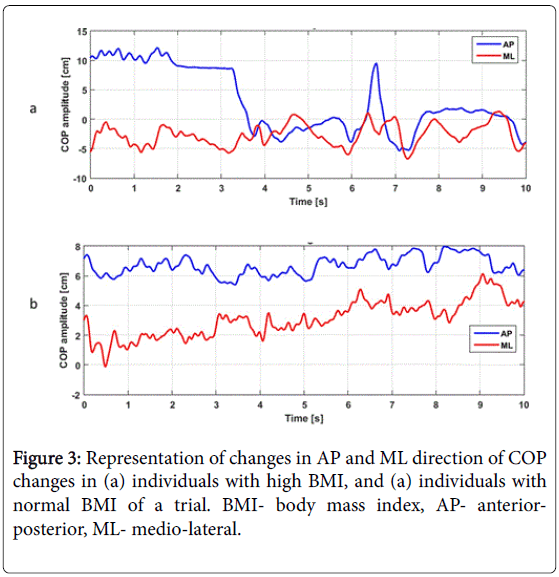
During single limb stance conditions, five individuals with higher BMI could not perform the single limb standing task due to task difficulty. A representative COP sway in AP and ML direction of one participant with high BMI and one with normal BMI is shown in Figure 3.
The COP analysis during single limb stance (Table 2) showed a significant difference in COP amplitude (cm) (p=0.015) and velocity (cm/s) (p=0.012) in the AP direction. In addition, the COP sway area was significantly different between the groups (p=0.011). There were no significant differences found in the ML direction for amplitude (cm) (p=0.155) or velocity (cm/s) (p=0.186).
Discussion
This study demonstrated that individuals with higher BMI have impaired dynamic balance reflected through increased COP displacement and velocity during single limb stance. Findings of the current study are in line with studies reporting increased COP displacement in individuals with higher BMI [20-23]. However, those studies did not include static and dynamic tasks for postural control nor did they include individuals who were overweight (BMI 25-29.9 kg/m2).
The current study did not find any significant change in COP during double limb stance. However, COP significantly increased during single limb stance, suggesting individuals with high BMI have impaired dynamic postural stability with preserved static stability. Yang et al. reported dynamic postural instability in individuals with obesity in line with the current findings. However, the outcome of the study is based on response to treadmill induced slip and no COP measures were included [24].
Politti et al. documented increased COP in AP and ML directions when additional weight was attached to the body through a backpack [16]. However, this mechanically added weight was placed on the posterior aspect. In contrast, individuals with high BMI tend to have an accumulation of fat in the abdomen and thigh regions which relatively shift the COM anteriorly and superiorly [25,26]. In the current study, significant differences were only observed in an AP direction, not in the ML direction, suggesting direction-specific balance instability in the AP direction.
Postural instability in the AP direction for those with high BMI may stem from a different distribution of body mass compared to those with normal BMI, including a greater distribution of mass in the trunk, abdomen and anterior thigh [20,26,27] in the AP direction. Obese individuals demonstrate both an increase in the magnitude and velocity of postural sway when compared to non-obese individuals [28]. Improvements in postural stability have been shown to be related in a linear fashion with the magnitude of weight loss [20].
When participants with high BMI were asked to stand on a single leg, they possibly exhibited increased COP changes in the AP directions to maintain anteriorly and vertically shifted COP in the small base of support. Mechanical and metabolic workload must increase to maintain the anterior and vertical displacement of Center of Mass (COM) in a smaller base of support. This may be a possible reason why individuals with higher BMI get early fatigue while performing dynamic tasks.
During prolonged standing, postural sway increases at a faster rate for obese individuals compared to those of normal weight [20]. When considering the inverted pendulum model of postural control [27], the control of posture in single leg standing not only decreases the base of support but adds additional workload to the ankle strategies. Most likely, decreased range of motion (ROM) and impaired proprioceptive input can also contribute to the increased COP. The current study did not include measurements of ROM and proprioception. However, in the eyes closed position, the individuals with high BMI were able to maintain the COP similar to that of the normal BMI group, indicating that proprioceptive inputs were available. Thus, it seems a decrease in ankle strategy may be the primary factor increasing COP in the high BMI group.
Mean power frequency of the high BMI group was similar to that of the normal BMI group, indicating that somatosensory components of postural control [29,30] with eyes open and eyes closed is similar for both groups. On the contrary, it was postulated that people with high BMI have difficulties in utilizing somatosensory and proprioceptive information for postural control [18]. Due to the combination of the overweight and obese group, it is possible that the current study caused a ceiling effect.
The study is limited since BMI cannot make the distinction between an elevated body weights due to high levels of lean vs. fat body mass. Since the increase in body fat is more frequently associated with abnormalities found in obesity than a lean body mass, further studies categorizing the participants based on body fat and subcategories of the overweight and obese category will help identify the effect of excess fat on postural stability. The study outcome is limited to lack of clinical measures of balance. The generalizability of the study outcome is limited due to small sample size. Further studies including biochemical, neurological, and clinical and instrumental assessment of postural stability would strengthen the outcome of the current findings.
In conclusion, this study found that individuals with high BMI have preserve static stability but impaired dynamic balance control in the AP direction reflected through higher COP amplitude and velocity. This information may assist with development of balance rehabilitation strategies for individuals with high BMI.
Acknowledgement
The authors thank Dr. Jennifer Mai for her help with the IRB submission. We also thank Dr. Mimi Vaassen and Clarke University DPT students for their help with data collection.
Conflict of Interest
None of the authors have conflict of interest.
References
- Pi-Sunyer FX (2002) The Obesity Epidemic: Pathophysiology and Consequences of Obesity. Obes Res 10: 97S-104S.
- Hills AP, Parker AW (1991) Gait characteristics of obese children. Arch Phys Med Rehabil 72: 403-407.
- McGraw B, McClenaghan BA, Williams HG, Dickerson J, Ward DS (2000) Gait and postural stability in obese and nonobese prepubertal boys. Arch Phys Med Rehabil 81: 484-489.
- Wu X, Lockhart TE, Yeoh HT (2012) Effects of obesity on slip-induced fall risks among young male adults. J Biomech 45: 1042-1047.
- Fjeldstad C, Fjeldstad AS, Acree LS, Nickel KJ, Gardner AW (2008) The influence of obesity on falls and quality of life. Dyn Med 7: 4.
- Finkelstein EA, Chen H, Prabhu M, Trogdon JG, Corso PS (2007) The relationship between obesity and injuries among U.S. adults. Am J Health Promot 21: 460-468.
- Maki BE, Holliday PJ, Topper AK (1994) A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol 49: M72-M84.
- Melzer I, Benjuya N, Kaplanski J (2004) Postural stability in the elderly: a comparison between fallers and non-fallers. Age ageing 33: 602-607.
- Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL (1992) Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil 73: 1073-1080.
- Chapman S, Thomas S (2017) Falls and the rise of the GP contract: An EMIS web protocol and template to help identify frail patients. Br J Community Nurs 22: 554-556.
- Kurup M, Felix JW (2015) Balance status of the elderly people and factors associated with it. Ind J Phys Occup Ther 9: 113-11.
- Haripriya S, Anjana B, George S, Roshan PSB (2017) The Influence of Body Mass Index on Functional Mobility and Balance in Elderly Individuals. Ind J Phys Occup Ther 11: 6-10.
- Gil AW, Oliveira MR, Coelho VA, Carvalho CE, Teixeira DC, et al. (2011) Relationship between force platform and two functional tests for measuring balance in the elderly. Br J Phys Ther 15: 429-435.
- Da Silva RA, Bilodeau M, Parreira RB, Teixeira DC, Amorim CF (2013) Age-related differences in time-limit performance and force platform-based balance measures during one-leg stance. J Electromyogr Kinesiol 23: 634-639.
- Ganesan M, Pal PK, Gupta A, Sathyaprabha TN (2010) Dynamic posturography in evaluation of balance in patients of Parkinson’s disease with normal pull test: concept of a diagonal pull test. Parkinsonism Relat Disord 16: 595-599.
- Politti F, de Oliveira Gonzalez T, de Paula Gomes CAF, El Hage Y, Amaral AP, et al. (2012) Effect of the Usual Weight of a Backpack on Body Sway during Quiet Standing. J Phys Ther Sci 24: 1079-1082.
- Friedmann JM, Elasy T, Jensen GL (2001) The relationship between body mass index and self-reported functional limitation among older adults: a gender difference. J Am Geriatr Soc 49: 398-403.
- Dutil M, Handrigan GA, Corbeil P, Cantin V, Simoneau M, et al. (2013) The impact of obesity on balance control in community-dwelling older women. Age (Dordr) 35: 883-890.
- Mitchell RJ, Lord SR, Harvey LA, Close JC (2015) Obesity and falls in older people: mediating effects of disease, sedentary behavior, mood, pain and medication use. Arch Gerontol Geriatr 60: 52-58.
- Teasdale N, Simoneau M, Corbeil P, Handrigan G, Tremblay A, et al. (2013) Obesity alters balance and movement control. Curr Obes Rep 2: 235-240.
- Menegoni F, Galli M, Tacchini E, Vismara L, Cavigioli M, et al. (2009) Gender-specific effect of obesity on balance. Obesity (Silver Spring) 17: 1951-1956.
- Lee AJ, Lin WH (2007) The influence of gender and somatotype on single-leg upright standing postural stability in children. J Appl Biomech 23: 173-179.
- Hue O, Simoneau M, Marcotte J, Berrigan F, Dore J, et al. (2007) Body weight is a strong predictor of postural stability. Gait posture 26: 32-38.
- Yang F, Kim J, Yang F (2017) Effects of obesity on dynamic stability control during recovery from a treadmill-induced slip among young adults. J Biomech 53: 148-153.
- Cereda E, Malavazos AE, Caccialanza R, Rondanelli M, Fatati G, et al. (2011) Weight cycling is associated with body weight excess and abdominal fat accumulation: a cross-sectional study. Clin Nutr 30: 718-723.
- Ellabban M, Hart N (2004) Body contouring by combined abdominoplasty and medial vertical thigh reduction: experience of 14 cases. British journal of plastic surgery 57: 222-227.
- Alonso AC, Mochizuki L, Silva Luna NM, Ayama S, Canonica AC, et al. (2015) Relation between the sensory and anthropometric variables in the quiet standing postural control: is the inverted pendulum important for the static balance control? Biomed Res Int 2015: 985312.
- Son SM (2016) Influence of Obesity on Postural Stability in Young Adults. Osong Public Health Res Perspect 7: 378-381.
- Singh NB, Taylor WR, Madigan ML, Nussbaum MA (2012) The spectral content of postural sway during quiet stance: influences of age, vision and somatosensory inputs. J Electromyogr Kinesiol 22: 131-136.
- Kanekar N, Lee YJ, Aruin AS (2014) Frequency analysis approach to study balance control in individuals with multiple sclerosis. J Neurosci Methods 222: 91-96.
Citation: Ganesan M, Koos T, Kruse B, O’Dell B (2018) Dynamic Postural Instability in Individuals with High Body Mass Index. J Nov Physiother 8: 387. DOI: 10.4172/2165-7025.1000387
Copyright: © 2018 Ganesan M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4747
- [From(publication date): 0-2018 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 3906
- PDF downloads: 841