Drug Abuse and Perivascular Changes of the Brain
Received: 13-Jun-2016 / Accepted Date: 28-Jun-2016 / Published Date: 29-Jun-2016 DOI: 10.4172/2161-0681.1000281
Abstract
Drug abuse is a major health problem worldwide with severe socioeconomic consequences. Numerous drugs are widely abused but most common are heroin, cocaine, amphetamines and cannabis. Various cerebrovascular events associated with drug abuse have been reported in the literature but a systematic study of the perivascular changes occuring in human brains is lacking. We present a post-mortem, comparative, pathology study of the perivascular areas in the brain of drug abusers and healthy controls.
Keywords: Drug abuse; Perivascular changes; Brain; Pathology
314856Introduction
Drug abuse has significantly increased over the last decades throughout the world. Various socioeconomic factors including poverty, unemployment and stressful conditions of modern life have contributed to this trend. The number of available drugs abused has grown accordingly. Most commonly abused ones are heroin, cocaine, amphetamines and cannabis, but other chemically produced substances such as “ecstasy” and lysergic acid diethylamide (LSD) are also widely abused.
Abuse of multiple substances by the same person is a common practice and most of these drugs contain various contaminants in the form of particles. Moreover, sterile precautions are seldom taken by the addicts. All these factors contribute to the development of vascular and perivascular changes throughout the body, but those observed in the brain are the most detrimental (in terms of neurological dysfunction).
Materials and Methods
We have conducted a comparative pathology study on the brains of drug addicts and healthy controls. Exclusion criteria were neurological disorders not related to drug abuse (stroke, epilepsy etc.), vascular diseases (hypertension, coronary artery disease, diabetes mellitus etc.) and causes of death that are known to induce cerebrovascular changes (drowning, traumatic brain injury etc.). Overall, 37 human brains (20 drug addicts and 17 healthy controls of similar ages) were examined. Mean age of death of drug addicts was 30.3 years, while mean age of death of healthy controls was 27 years. All 20 drug addicts died of drug overdose. Among healthy controls, 4 (24%) died after a fall from height and the rest 13 (76%) died at motor vehicle accidents. There were 19 males and only 1 female in the drug addicts' group, while in the control group there were 11 males and 6 females.
The aim of our study was to determine the pathological changes of the perivascular areas in the brain due to drug abuse. Examined areas include the frontal cortex, basal ganglia, hippocampus, cerebellum and pons. Anatomic specimens were painted with hematoxylin eosin and studied under the microscope.
Statistical analysis was conducted using Student's t test and statistical significance was set to p<0.05.
Results
Toxicological analysis of drug addicts' blood and urine revealed heroin use in 19/20 (95%), benzodiazepines in 10/20 (50%), cannabis in 8/20 (40%), cocaine in 4/20 (20%) and amphetamines in 2/20 (10%) (Table 1). Toxicological analysis of all controls was negative for drugs (Table 2).
| Case | Sex | Age at death | Toxicology | Cerebellum | Hippocampus | Frontal lobe | Pons | Basal ganglia |
|---|---|---|---|---|---|---|---|---|
| 1 | Male | 18 | Heroin, cannabis | B | B | B | B-C | B |
| 2 | Male | 34 | Heroin, benzodiazepines | B | B | B | B-C | A-B-C |
| 3 | Male | 24 | Heroin, cannabis | A-B-C | B-C | - | B-C | A-B-C |
| 4 | Male | 34 | Heroin, cannabis, benzodiazepines | A-B | B-C | C | A-B | A-B-C |
| 5 | Male | 27 | Heroin, benzodiazepines | A-B-C | B-C | B-C | B-C | - |
| 6 | Male | 20 | Heroin | B | A-B-C | B-C | B | B-C |
| 7 | Male | 26 | Heroin, cannabis, cocaine | B-C | B-C | - | B-C | B-C |
| 8 | Male | 26 | Heroin, cannabis, cocaine | B | A-B-C | B-C | A-B-C | A-B-C |
| 9 | Male | 37 | Heroin | A-B-C | A-B-C | - | - | B-C |
| 10 | Male | 35 | Heroin, cocaine | - | B | A-B | A-B-C | A-B |
| 11 | Male | 42 | Heroin, cocaine | - | A-B-C | A-B-C | B-c | A-B-C |
| 12 | Male | 49 | Heroin, benzodiazepines, amphetamine | B | - | - | B-C | B-C |
| 13 | Male | 16 | Heroin, cannabis, benzodiazepines | A-B-C | - | B | B-C | A-B-C |
| 14 | Male | 32 | Heroin | A-B-C | B-C | A-B-C | B | B-C |
| 15 | Male | 21 | Heroin, cannabis, benzodiazepines | - | B-C | B-C | B-C | B-C |
| 16 | Male | 38 | Cannabis, benzodiazepines | B-C | - | B-C | B-C | B-C |
| 17 | Male | 48 | Heroin | B-C | B | B-C | A-B-C | B-C |
| 18 | Male | 40 | Heroin, benzodiazepines | A-B | B-C | A-B-C | A-B-C | B-C |
| 19 | Male | 20 | Heroin, benzodiazepines | B | B-C | B | B | B |
| 20 | Female | 19 | Heroin, benzodiazepines | A-B-C | B | B-C | A-B-C | A-B-C |
Table 1: Drug abusers' group data. A – Infiltration by inflammatory cells, B – Edema, C – Hemorrhage.
| Case | Sex | Age at death | Toxicology | Cerebellum | Hippocampus | Frontal lobe | Pons | Basal ganglia |
|---|---|---|---|---|---|---|---|---|
| 1 | Male | 24 | Negative | - | - | B | - | - |
| 2 | Male | 22 | Negative | - | B-C | B-C | B-C | - |
| 3 | Female | 23 | Negative | - | - | B | - | - |
| 4 | Male | 28 | Negative | B | B | B | - | - |
| 5 | Male | 26 | Negative | - | - | - | B-C | B-C |
| 6 | Male | 24 | Negative | - | - | - | - | - |
| 7 | Female | 35 | Negative | - | B-C | B-C | - | - |
| 8 | Male | 24 | Negative | B | - | - | B | - |
| 9 | Female | 21 | Negative | - | - | - | B | B |
| 10 | Male | 19 | Negative | B-C | B-C | B-C | B-C | - |
| 11 | Male | 26 | Negative | - | - | - | - | - |
| 12 | Male | 34 | Negative | B-C | - | - | - | B-c |
| 13 | Male | 35 | Negative | - | B | B-C | B-C | - |
| 14 | Female | 19 | Negative | - | B | B-C | B-C | B-C |
| 15 | Female | 34 | Negative | - | - | - | - | - |
| 16 | Male | 35 | Negative | B-C | - | - | - | - |
| 17 | Female | 27 | Negative | - | - | B | B | - |
Table 2: Control group data. A – Infiltration by inflammatory cells, B – Edema, C – Hemorrhage.
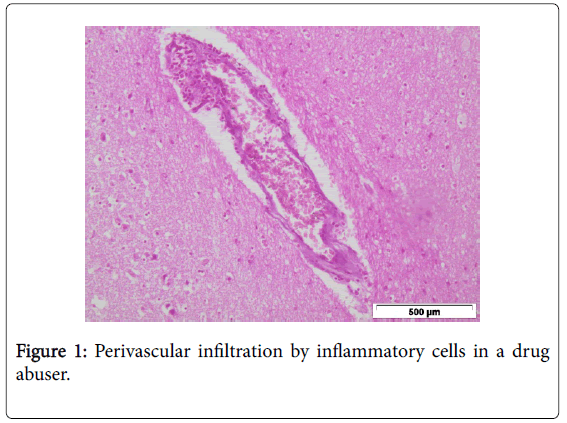
Small diameter cerebral vessels (especially small cortical and meningeal vessels) were perivascularly infiltrated by inflammatory cells (neutrophils, macrophages and lymphocytes) in drug abusers compared to healthy controls (p < 0.05) in all areas examined.
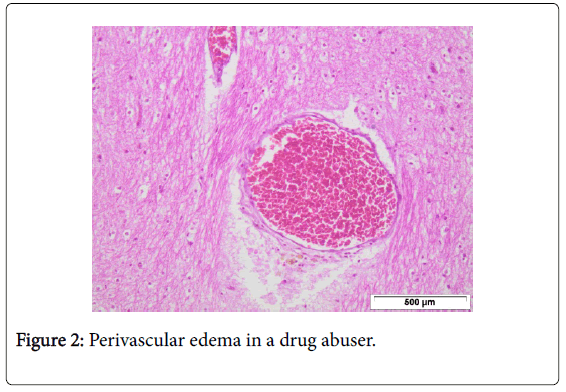
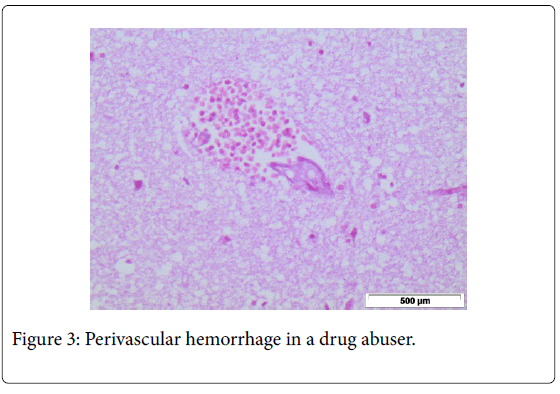
Leukocyte migration was observed through the brain endothelial monolayers towards the brain parenchyma, regardless of the type of drug abused. This perivascular infiltration by inflammatory cells (lymphocytes, pigmented macrophages, mast cells, neutrophils and eosinophils) is believed to be the result of repeated, intravenous injections of various impurities or part of an immune-mediated perivascular inflammatory reaction to the drug per se. There were also foci of interstitial edema (p< 0.05) and hemorrhage (p< 0.05) around small arteries and capillaries due to rupture of their basal membrane (possibly also as a result of an immune-mediated process) (Figures 1,2 and 3).
Discussion
A wide range of changes has been observed in the central nervous system of drug abusers [1]. Most of these findings are the sequelae of ischemia secondary to cerebrovascular diseases. Despite the fact that the human brain receives a significantly disproportionate amount of blood, with regards to its size, the function of its vessels in various neuropathological conditions has not been studied extensively.
Morphological, physiological and neurochemical abnormalities have been observed in chronic drug abusers with the use of neuroradiological techniques such as computerised tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET) and single photon emission computed tomography (SPECT). The full range of neuropathological changes observed in drug users' brains is wide, but major findings include ischemic and hemorrhagic stroke, subarachnoid hemorrhage, intracerebral hemorrhage and cerebral ischemia [2-7]. Particularly, patients with co-existing, underlying cerebral arteriovenous malformations or aneurysms are at significantly high risk for the development of such cerebrovascular events [8].
The use of Masson's trichrome stain has revealed extensive vacuolar degeneration of the cerebral hemispheres' white matter in patients with heroin-induced spongiform leukoengephalopathy (HSLE) and the vacuoles were arranged around gray matter capillaries and arterioles, while no vacuoles were found around cerebral vessels of the control group [9].
Conclusion
Drug abuse has been associated with various cerebrovascular events, such as cerebral infarcts and hemorrhage. However, a systematic study of the perivascular changes occuring in the brains of drug addicts was lacking from the literature. We have found a statistically significant perivascular infiltration of cerebral vessels by inflammatory cells, as well as perivascular edema and hemorrhage, in various areas examined (such as the frontal cortex, basal ganglia, hippocampus, cerebellum and brainstem). All these abnormal alterations may explain, at least in part the neurological deficits observed after chronic drug abuse and may point towards a new perspective regarding their treatment and rehabilitation.
Acknowledgement
This study was conducted with the support of IKY Fellowships of Excellence for Postgraduate studies in Greece - Siemens Program.
References
- Büttner A (2011) Review: The neuropathology of drug abuse. NeuropatholApplNeurobiol 37: 118-134.
- Brown E, Prager J, Lee HY, Rarnsey RG (1992) CNS Complications of Cocaine Abuse: Prevalence, Pathophysiology, and Neuroradiology. AJR Am J Roentgenol 159: 137-147.
- Brust JC (1997) Vasculitis owing to substance abuse. NeurolClin 15: 945-957.
- Buxton N, McConachie NS (2000) Amphetamine abuse and intracranial haemorrhage. J R Soc Med 93: 472-477.
- Daras M, Tuchman AJ, Koppel BS, Samkoff LM, Weitzner I, et al. (1994) Neurovascular complications of cocaine. ActaNeurolScand 90: 124-129.
- De Silva DA, Wong MC, Lee MP, Chen CLH, Chang HM (2007) Amphetamine-associated ischemic stroke: clinical presentation and proposed pathogenesis. J Stroke Cerebrovasc Dis 16: 185-186.
- Finsterer J, Christian P,Wolfgang K (2004) Occipital stroke shortly after cannabis consumption. ClinNeurolNeurosurg 106: 305-308.
- Rumbaugh CL, Bergeron RT, Fang HCL, McCormack R (1971) Cerebral angiographic changes in the drug abuse patient. Radiology 101: 335-344.
- Yin J, Pan SY, Zhou L, Lu TM, Luo YF, et al. (2007) Pathological analysis of heroin spongiform leukoencephalopathy. J South Med Univ 27: 881-886.
Citation: Zogopoulos P, Theocharis S, Kotakidis N, Patsouris E, Agapitos E (2016) Drug Abuse and Perivascular Changes of the Brain. J Clin Exp Pathol 6:281. DOI: 10.4172/2161-0681.1000281
Copyright: © 2016 Zogopoulos P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 12842
- [From(publication date): 7-2016 - Jul 02, 2025]
- Breakdown by view type
- HTML page views: 11836
- PDF downloads: 1006