Research Article Open Access
Double Column Foot Osteotomy to Correct Flexible Valgus Foot Deformity in Children with Spastic Cerebral Palsy
Sherif Bishay*, George Magdy Morshed, Yehia Tarraf and Naguib Pasha
National Institute of Neuromotor System of Imbaba, General Organization of Teaching Hospitals and Institutes, Egypt
- *Corresponding Author:
- Sherif Bishay
Assistant Professor of Orthopaedic Surgery
National Institute of Neuromotor System of Imbaba
General Organization of Teaching Hospitals and Institutes, Egypt
Tel: 00202-37604539/0020122-3118518
E-mail: sherifbishay@outlook.com
Received date: Jul 20, 2016; Accepted date: Aug 09, 2016; Published date: Aug 20, 2016
Citation: Bishay S, Morshed GM, Tarraf Y, Pasha N (2016) Double Column Foot Osteotomy to Correct Flexible Valgus Foot Deformity in Children with Spastic Cerebral Palsy. Clin Res Foot Ankle 4:198. doi: 10.4172/2329-910X.1000198
Copyright: © 2016 Sherif Bishay, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
Backgound: Mobile (flexible or correctable) hindfoot valgus deformity is common in children with spastic cerebral palsy (CP). It is accompanied by short lateral and long medial foot column.
Patients and Methods: Eleven ambulatory children (20 feet) suffering spastic cerebral palsy (CP), two hemiplegic and nine diplegic, presenting with mobile (flexible) hindfoot valgus deformity, were evaluated neurologically, orthopaedically, and radiographically, and operated upon in the National Institute of Neuromotor System between September 2012 and September 2013. Double column foot osteotomy with medial cuneiform closing-wedge and cuboid opening-wedge without attacking the calcaneus was performed in all of them.
Results: The results were followed-up clinically and radiographically over a period ranging from a year and half (18 months) to two years (24 months) with an average of a year and 9 months (21 months), and were graded into four categories as excellent, good, fair, and poor according to the total calculated score. According to the suggested grading system, there were 8 excellent results, 8 good results, 4 fair results, and no poor results.
Conclusion: Double column foot osteotomy shortening the medial foot column and lengthening the lateral foot column to correct moderate to severe hindfoot valgus in ambulatory children with spastic cerebral palsy (CP), compared favourably with similar series, and offered option for achieving foot alignment, improving pain and skin problems and avoiding the problems associated with arthrodesis. Level of Evidence: The study is type IV therapeutic level of evidence.
Introduction
Mobile (flexible or correctable) hindfoot valgus deformity is common in children with spastic cerebral palsy (CP). In ambulatory children, the foot progresses into more valgus by standing. The talar head becomes more prominent and the medial longitudinal arch collapses making the orthosis difficult and even painful with possible skin problems.
Attempts to correct these deformities by lateral foot column lengthening through calcaneal osteotomy and iliac bone graft [1-3] may not be sufficient alone; as shortening osteotomy of the medial column may be necessary for complete correction. In addition, the calcaneal osteotomy may injure the subtalar joint in some cases owing to anatomic variation; and the iliac bone graft may be cumbersome. Fusion of one or multiple joints [4] may be followed by resorption or failure of the graft, non-union (pseudoarthrosis), loss of subtalar joint (STJ) motion [5,6] and vulnerability to skin ulceration of the rigid foot.
The aim of the work was to establish a protocol for diagnosis and treatment of paralytic mobile (flexible or correctable) subtalar hindfoot valgus deformity in ambulatory children with spastic cerebral palsy (CP), and to evaluate the results of the double column osteotomy of the spastic foot in correction of the foot deformity, foot pain relief, subtalar joint (STJ) mobility, tolerability to orthoses, and overall patient / parent satisfaction.
Patients and Methods
Eleven consecutive ambulatory children (20 feet) suffering spastic cerebral palsy (CP), 2 hemiplegic and 9 diplegic, and presenting with mobile (flexible) hindfoot valgus deformity, were operated upon in the National Institute of Neuromotor System between September 2012 and September 2013 in this study.
Inclusion criteria
Moderate (15°–20°) to severe (20° or more) mobile (flexible) hindfoot valgus deformity, in ambulatory children with spastic CP (Gross Motor Function Classification System GMFCS 1–2), with no neurological deficits as incoordination or involuntary movements, between 6–7 years of age, were chosen.
Exclusion criteria
Fixed (rigid) hindfoot valgus deformity as that of vertical talus, arthrogryposis, and tarsal coalition, other neurological disorders than spastic CP, non-ambulatory children with spastic CP (Gross Motor Function Classification System GMFCS > 2) or with neurological deficits as incoordination or involuntary movements, idiopathic pes valgus, and children below 6 years or above 7 years of age, were rejected.
The average age at the time of surgery was 6 years and 8 months (ranging from 6 to 7 years of age).
Five patients (9 feet) were at the age group of 6 to <6½, and 6 patients (11 feet) at the age group of 6½ to < 7. There were 6 male patients (or boys), 5 of them had both feet affection i.e., diplegic and one had only right foot affection i.e., right-sided hemiplegic; and 5 female patients (or girls), 4 of them had both feet affection i.e., dipledic and one had only left foot affection i.e., left-sided hemiplegic.
All of them underwent double column foot osteotomy. Among them, were 4 boys and 2 girls who underwent Achilles’ tendon lengthening (ATL), each in both feet; 2 boys (one of them in both feet, and one in the left foot) and 2 girls (one of them in both feet, and one in the right foot) who underwent peroneal tendon lengthening. The right foot was operated upon in 6 patients (all males, 5 of them bilateral, i.e., in 10 feet) and the left foot was operated upon in 5 patients (all females, 4 of them bilateral, i.e., in 10 feet) (Table 1).
| Operation | Males (Boys) | Females (Girls) | Total Cases (Feet) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Double column foot osteotomy | 6 | 5 | 20 feet | ||||||||||||
| Right | Left | Bilateral | Right | Left | Bilateral | ||||||||||
| 1 | 0 | 5 | 0 | 1 | 4 | ||||||||||
| Achilles’ tendon lengthening | 4 | 2 | 12 feet | ||||||||||||
| Right | Left | Bilateral | Right | Left | Bilateral | ||||||||||
| 0 | 0 | 4 | 0 | 0 | 2 | ||||||||||
| Peroneal tendon lengthening | 2 | 2 | 6 feet | ||||||||||||
| Right | Left | Bilateral | Right | Left | Bilateral | ||||||||||
| 0 | 1 | 1 | 1 | 0 | 1 | ||||||||||
Table 1: Classification of patients in relation to their gender, foot side, and surgery performed.
History, Original Disease, Examination and Treatment
All of the eleven patients had history of difficult delivery and were incubated at birth. Nine were spastic diplegic, and two were spastic hemiplegic (one right- and one left-sided), but no patient was of the total body involvement (TBI) type.
All were able to walk without support; and were considered to be community level ambulators with Growth Motor Function Classification System GMFCS of level II.
Each of them received some forms of non-operative treatment as physical therapy programs (range of motion exercises and gait training), orthoses (ankle-foot orthoses AFO), and skeletal muscle relaxant but no previous surgery.
Presentation Complaints
Foot pain
Frank foot pain (in 8 cases), or discomfort (in 12 cases) was experienced. Pain was particularly over the bony prominence (talar head).
Foot deformity
All the patients (or parents) were annoyed of the outwardly deviated shape of their (or their children's) feet which were not tolerating any form of shoes or orthoses.
Skin problems
Pressure sores or ulceration by shoes or orthoses were noticed in progressive deformities.
Preoperative Assessment
Clinical assessment
Neurological assessment: Neurological examination showed that all patients had spastic cerebral palsy (CP), of which 2 patients were hemiplegic and 9 patients were diplegic. Assessment implied detecting spasticity (hypertonia), eliciting of exaggerated deep reflexes, positive Babinski sign, and exclusion of incoordination and involuntary movements.
Orthopedic assessment: Orthopedic examination implied the gait, spastic muscle grading, the presence of deformities other than that of the foot, and the weightbearing alignment of the hindfoot.
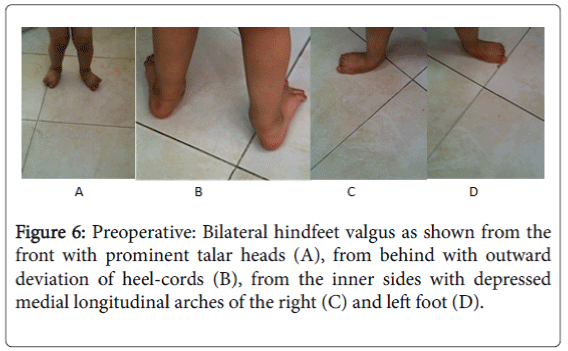
Foot Deformity
Outward deviation of the foot with prominent head of talus (i.e., hindfoot valgus) ranging from moderate (15°–<20°) to severe (20° or more), and collapsed medial longitudinal arch (examined by Jack's test) [7], were present in all cases.
Two patients (4 feet) had severe (20° or more) hindfoot valgus deformity; while the remaining 9 patients (16 feet) had moderate (15° to <20°) deformity.
All feet were sufficiently mobile (flexible or correctable) to normal alignment. Associated tight Achilles' tendon, but without ankle equinus deformity, (in 12 cases; examined by limited ankle dorsiflexion with the knee straight and/or flexed i.e., Silverskoiid test) [7], and prominent spastic peroneal tendons (in 6 cases) were evident.
From the history, progression of the deformity occurred in all patients with repeated change of shoes or orthoses.
Functional disabilities
All were able to walk without support and were considered to be community level ambulatory with Gross Motor Function Classification System GMFCS of level 1 – 2 before foot surgery.
They had variable active power around the ankles and feet (Table 2). Fourteen cases had no imbalance between the peronei and the tibialis anterior and posterior muscles.
| Case no. | EHL | EDL | TA | TP | PL andB | FHL | FDL | TS |
|---|---|---|---|---|---|---|---|---|
| 1 | 4 | 4 | 2 | 2 | 4 | 4 | 4 | 4 |
| 2 | 4 | 4 | 2 | 2 | 2 | 2 | 0 | 4 |
| 3 | 4 | 4 | 2 | 2 | 2 | 2 | 2 | 4 |
| 4 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| 5 | 4 | 4 | 3 | 3 | 3 | 4 | 4 | 4 |
| 6 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| 7 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| 8 | 4 | 4 | 4 | 4 | 4 | 3 | 3 | 5 |
| 9 | 3 | 3 | 4 | 4 | 4 | 3 | 3 | 3 |
| 10 | 3 | 3 | 2 | 2 | 2 | 3 | 3 | 3 |
| 11 | 4 | 4 | 2 | 2 | 2 | 2 | 4 | 4 |
| 12 | 3 | 3 | 2 | 2 | 4 | 3 | 3 | 3 |
| 13 | 3 | 3 | 0 | 0 | 4 | 3 | 3 | 3 |
| 14 | 5 | 5 | 2 | 2 | 4 | 5 | 5 | 5 |
| 15 | 4 | 4 | 2 | 2 | 5 | 5 | 5 | 5 |
| 16 | 4 | 5 | 2 | 2 | 2 | 5 | 5 | 5 |
| 17 | 4 | 4 | 5 | 5 | 5 | 4 | 4 | 4 |
| 18 | 5 | 5 | 4 | 4 | 4 | 5 | 5 | 5 |
| 19 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| 20 | 4 | 4 | 2 | 2 | 5 | 4 | 4 | 4 |
Table 2: Grading of the spastic muscles around the foot of all cases. EHL: extensor hallucis longus; EDL: extensor digitorum longus; TA: tibialis anterior; TP: tibialis posterior; PLandB: peroneus longus and brevis; FHL: flexor hallucis longus; FDL: flexor digitorum longus; TS: triceps surae.
Six cases had powerful peronei versus tibialis anterior and posterior muscles.
Radiographic Assessment
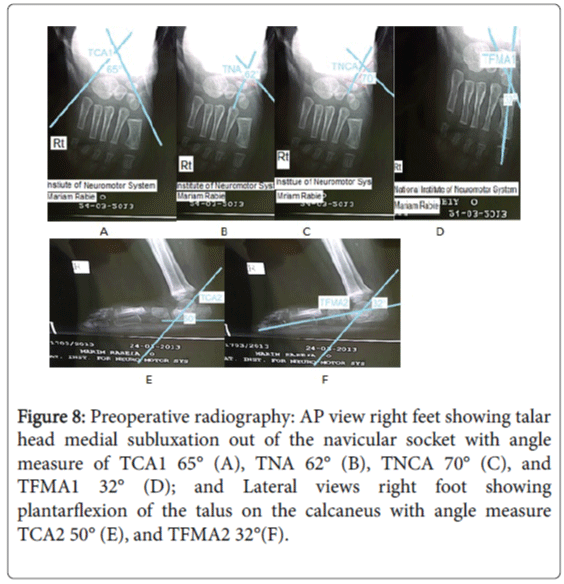
Weightbearing anteroposterior and lateral X-ray views of ankles and feet were taken for all patients. Ankle anteroposterior radiography excluded the possibility of valgus at the talotibial joint evidenced by talar tilt in the ankle mortise [8]. In the anteroposterior view of the foot the anterior talocalcaneal angle (TCA1) or Kite's angle, talonavicular angle (TNA), talonavicular coverage angle (TNCA), and anterior talo-first metatarsal angle (TFMA1) were measured. In the lateral view of the foot the lateral talocalcaneal angle (TCA2) and the lateral talo-first metatarsal angle (TFMA2) or Meary's angle were measured.
All patients had shown failure of conservative measures and ankle foot orthoses (AFO) treatment for at least six months before surgery. Four patients (7 cases) had difficulty in maintaining stability while walking. Six patients (11 cases) developed progressive deformity with collapsed medial longitudinal arch. Four patients (6 cases) developed footwear or orthotic intolerance and skin problems.
Operative Procedure
Double column foot osteotomy with medial cuneiform closingwedge and cuboid opening-wedge without attacking the calcaneus was performed in all of the eleven patients (20 feet).
Under general anesthesia, the patient was supine. A tourniquet was applied in the upper thigh. Skin was prepared and limb draped, with the knee on view to provide orientation to rotational alignment.
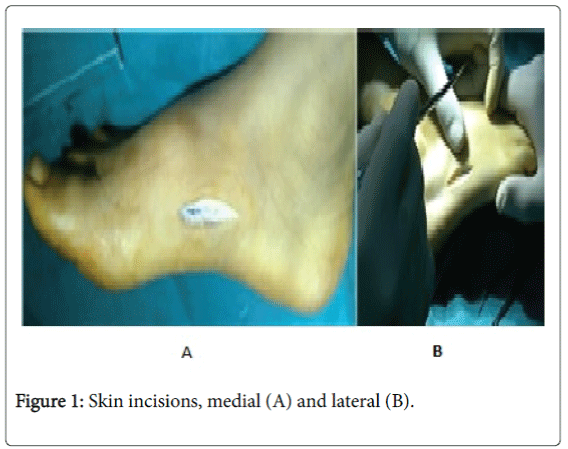
Skin Incisions
The skin was incised through two skin incisions, longitudinal medial one over the medial cuneiform exposing it, and longitudinal lateral one along the cuboid exposing it, anterior and parallel to the peroneal tendons (Figure 1).
Care was taken in the medial incision to avoid injury of the tibialis anterior tendon and the long saphenous vein. The lateral incision was extended following Langer’s skin lines, below and behind the lateral malleolus (Ollier’s) in cases of peroneal tendon lengthening.
Care was taken to avoid injury of the sural nerve and the short saphenous vein which were carefully retracted.
An additional posteromedial skin incision parallel to Achilles’ tendon was made in cases of Achilles’ tendon lengthening (ATL).
Soft-Tissue (Tendons) Procedures
Peroneal tendon lengthening and Achilles' tendon lengthening were performed, according to the circumstances of the case, in the same session, but before the bony procedures.
Peroneal tendon lengthening
Through extension of the lateral skin incision a sagittal plane longitudinal split in the peroneal tendons was performed in cases of severely spastic peronei functioning as a deforming element (6 cases).
Achilles’ tendon lengthening (ATL):
A Z-plasty of the tendenious part was performed in cases associated with tight Achilles' tendon (12 cases). The tendon was split longitudinally in the sagittal plane, and divided at its distal end laterally and its proximal end medially into two longitudinal halves. The lateral distal cut was to eliminate the tendon pull laterally on the hindfoot. It also corrects any possible equinus component. The deformity was corrected till the foot was plantigrade (tibio-calcaneal angle 90°) with the knee fully extended to prevent postoperative deformity in the opposite calcanean position.
Bony Procedures
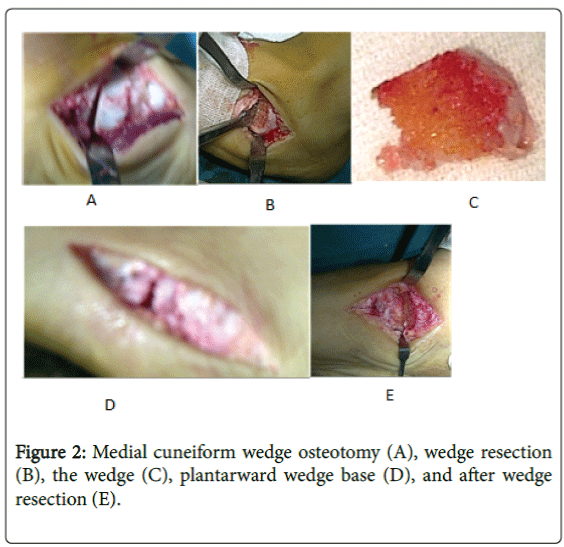
Medial cuneiform closing wedge resection
The middle third (i.e., central portion) of the medial cuneiform was removed by a fine sharp osteotome (or even a scalpel in some cases with softer bones), with its base plantarward to allow its later closing wedge in adduction and plantar direction recreating a medial longitudinal arch [9] (Figure 2).
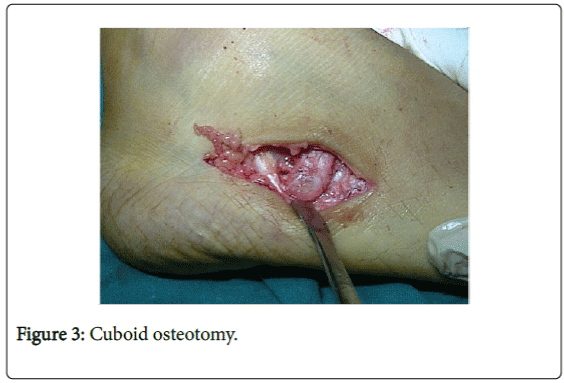
Cuboid opening wedge osteotomy
An osteotomy was made in the cuboid, opening a wedge in it according to the predetermined amount and distracting it in position by a suitable osteotome or a laminar spreader (Figure 3). An intraoperative ruler measured the base length of the wedge, comparing it with the predetermined one, overcorrecting the foot deformity [6].
Wedge determination
Tracing papers were used on the X-ray films. At first, the anteroposterior X-ray was drawn to determine the amount of the talar displacement in relation to the navicular bone and the site and amount of the cuboid wedge. Then, a cut was made by a scissors carefully around the talar head dividing the paper into two segments, a proximal segment enclosing the talus and the calcaneus, and a distal segment enclosing the other tarsal and metatarsal bones. The distal segment was rotated till adequate talar head coverage with the navicular socket was achieved. A second tracing paper was put and a cut was made in the drawing of the cuboid till the second paper was superimposed on the first one. The amount of the cut of the cuboid drawing was corresponding to the base length of its required medial cuneiform wedge. A similar method was done on the lateral X-ray film till the talar axis fit that of the first metatarsal.
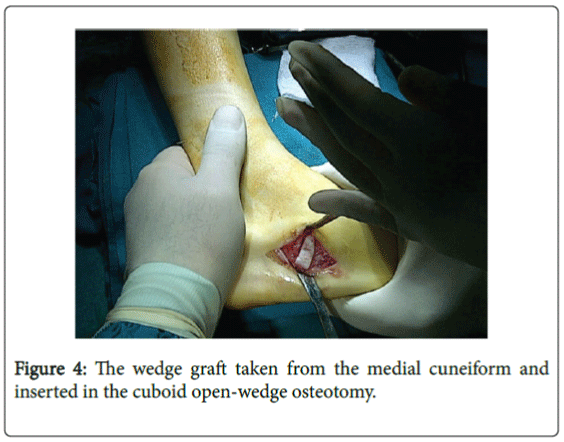
Graft insertion
The wedge graft taken from the medial cuneiform was inserted in the cuboid open-wedge osteotomy, increasing the length of the foot lateral column and correcting the pes valgus deformity [6] (Figure 4).
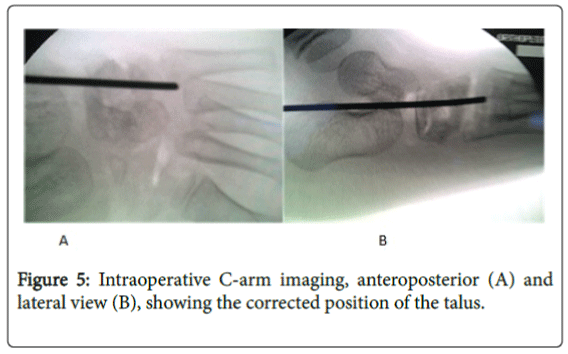
An intraoperative C-arm image would be helpful to assess the corrected foot position in two planes: anteroposterior and lateral (Figure 5).
4- K-wire fixation
The cuboid opening wedge and the graft were pinned percutaneously by 1.6 mm K-wires.
Closure
All wounds were closed in layers. The skin was closed by interrupted or subcuticular 0/3 vicryl sutures.
The K-wires were bent 90° and left out through the skin.
Immobilization POP cast and postoperative care
A well-moulded non-weightbearing below-knee POP cast was applied in almost all cases, except for 12 cases in which an above-knee POP cast was applied for Achilles’ tendon lengthening.
The K-wires and the interrupted skin sutures were removed at the time of cast change after 6 weeks. The period of immobilization was 8 weeks for all cases.
Postoperative Assessment and Follow-Up Regime
After cast removal, at least 6-week interval of gait training physiotherapy was instructed to all cases.
A follow-up period ranging from a year and half (18 months) to two years (24 months) with an average of a year and 9 months (21 months) was planned.
All cases were assessed clinically and radiographically, fulfilling the following criteria:
Clinical Assessment
1) Presence or absence of foot pain or discomfort.
2) Correction of the foot deformity:
(a) Position of the heel in respect to the calf as seen from behind.
(b) Prominence of the talar head.
(c) Absence of the skin problems (callus, ulcer, …etc).
3) Subtalar joint (STJ) mobility.
4) Patient (or parents) satisfaction.
Radiographic Assessment
Weightbearing anteroposterior and lateral radiograph of the ankle and foot were taken, immediately postoperative (the day after operation), after change of the cast and removal of K-wires (6 weeks), after cast removal (8 weeks), and at 2 months interval.
The anterior talocalcaneal angle (TCA1) talonavicular angle (TNA), talonavicular coverage angle (TNCA), the anterior talo-first metatarsal angle (TFMA1), the lateral talocalcaneal angle (TCA2), and the lateral talo-first metatarsal angle (TFMA2) were measured.
The degree of correction of the angle measure was calculated by comparing the postoperative measures with those of the preoperative.
Intra-observer and inter-observer variability
Intra-observer and inter-observer variability were studied. Ten feet were examined and scored independently by four observers.
On a separate occasion, two of the observers repeated the assessments of the same feet in the absence of information from the initial observations.
The chance corrected and weighted kappa statistics for observer agreement, both for inter-observer and intra-observer variability demonstrated satisfactory repeatability of the foot grading system.
The overall intra-observer mean weighted kappa was χw = +0.61 (range SE χ = 0.011–0.053) and the overall inter-observer mean weighted kappa was χw= +0.54 (range SE χ = 0.009–0.041).
Results
In the previous series or literatures, evaluation of hindfoot valgus was classified as stated by Stevens and Toomey [10] depending only on the radiographic measures and the relationship between the talus, tibia, and calcaneus.
The evaluation in that scheme was lacking the clinical objective and subjective results.
Therefore, a grading system was suggested in this study depending on both clinical and radiographic measures and correlating them with point scores (Table 3).
| Clinical results | Score |
|---|---|
| Foot Pain: | |
| Absent | 2 |
| Mild, Not over the talar head | 1 |
| Present, Over the talar head | 0 |
| Foot Deformity: | |
| Full correction (< 10° valgus) | 2 |
| Partial correction (valgus <15°) | 1 |
| Valgus >15° | 0 |
| Subtalar joint (STJ) mobility: | |
| Preserved | 2 |
| Limited | 1 |
| Stiff (Immobile) | 0 |
| Patient (or parent) satisfaction: | |
| Satisfied | 2 |
| Accepting | 1 |
| Unsatisfied | 0 |
| Radiographic Results | Score |
| Anterior talocalcaneal angle (TCA1): | |
| < 30° | 2 |
| 30° to 40° | 1 |
| > 40° | 0 |
| Talonavicular angle (TNA): | |
| < 30° | 2 |
| 30° to 40° | 1 |
| > 40° | 0 |
| Talonavicular coverage angle (TNCA): | |
| <5° (i.e.,> 90% coverage) | 2 |
| 5° to10° (i.e., 75% to 90% coverage) | 1 |
| >10° (i.e.,< 75% coverage) | 0 |
| 4- Anterior talo-first metatarsal angle (TFMA1): | |
| <4° | 2 |
| 4° to 10° | 1 |
| > 10° | 0 |
| 5- Lateral talocalcaneal angle (TCA2): | |
| < 45° | 2 |
| 45° to 50° | 1 |
| >50° | 0 |
| 6- Lateral talo-first metatarsal angle (TFMA2): | |
| <4° | 2 |
| 4° to 10° | 1 |
| > 10° | 0 |
Table 3: Grading system: Score of the clinical and radiographic results.
The clinical evaluation (8 points) was based on the following criteria:
1. Presence or absence of foot pain (2 points).
2. Correction of the foot deformity (2 points).
3. Subtalar joint (STJ) mobility (2 points).
4. Patient (or parents) satisfaction (2 points).
The radiographic evaluation (12 points) relied on the following anteroposterior and lateral weightbearing angle measure:
1. Anterior talocalcaneal angle (TCA1) measure (2 points).
2. Talonavicular angle (TNA) measure (2 points).
3. Talonavicular coverage angle (TNCA) measure i.e., talar head coverage (2 points).
4. Anterior talo-first metatarsal angle (TFMA1) measure (2 points).
5. Lateral talocalcaneal angle (TCA2) measure (2 points).
6. Lateral talo-first metatarsal angle (TFMA2) measure (2 points).
Clinical Evaluation
Foot pain
There was no foot pain postoperatively anywhere in the foot particularly over the talar head in seven patients (14 cases or feet) and in the right foot of one patient. There was only mild foot discomfort postoperatively but not over the talar head and no frank pain in two patient (4 cases or feet) and in the left foot of one patient.
This is in contrast to frank foot pain particularly over the bony prominence (talar head) preoperatively (in 8 cases) or discomfort (in 12 cases). Pain disappeared in the postoperative gait training and physiotherapy period. Other non-mechanical pain as that at the site of sutures or K-wires was of no significance as it was short-termed and disappeared spontaneously.
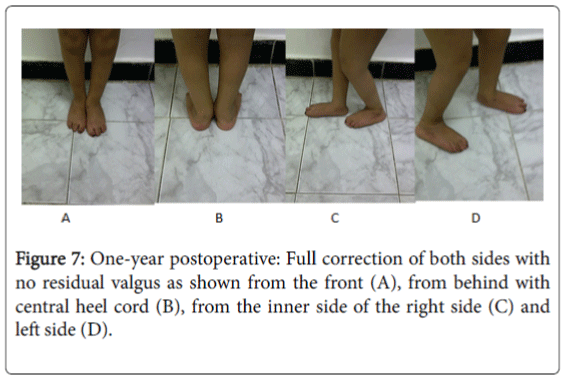
Foot deformity
The degree of hindfoot valgus improved postoperatively in all of the eleven patients (20 cases or feet). However, only one patient (2 cases or feet) had residual hindfoot valgus less than 15° at the last follow-up which was attributed to under-correction of the hindfoot valgus due to severe preoperative tight Achilles' tendon, which was difficult to achieve full-correction without calcanean subluxation in such two cases.
This is in contrast to 2 patients (4 feet) who had severe (20° or more) hindfoot valgus deformity; and 9 patients (16 feet) had moderate (15° ≤ 20°) deformity preoperatively. All cases had no problem with the footwear. No cases recorded a discomfort or a skin problem since the prominent talar head was sufficiently corrected. All wore ordinary shoes.
Subtalar joint (STJ) mobility
Following the postoperative physiotherapy period, five patients (10 cases or feet) and the right foot of one patient had supple (mobile) subtalar joint with passive and active movements; while four patients (8 cases or feet) and the left foot of one patient had some limitation of full inversion rather than eversion, probably due to some osseous changes in the talocalcaneal complex.
Patient (or parents) satisfaction
Eight patients (15 cases or feet) were fully satisfied; while three patients (5 cases or feet) were not fully satisfied but also not dissatisfied and were accepting the result due to the disappearance of preoperative pain/discomfort, the correction of the foot deformity, the better footwear, and the overall improvement of the gait.
Radiographic Evaluation
In all of the eleven patients (20 cases or feet) there was improvement (decrease) in all angle measures postoperatively as compared with the preoperative ones, but with variable degrees (Table 4).
| Preoperative measure | Postoperative measure | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case no. | TCA1 | TNA | TNCA | TFMA1 | TCA2 | TFMA2 | TCA1 | TNA | TNCA | TFMA1 | TCA2 | TFMA2 | |
| 1 | 63° | 40° | 30° | 40° | 53° | 15° | 20° | 28° | 2° | 3° | 40° | 5° | |
| 2 | 54° | 77° | 62° | 22° | 49° | 39° | 36° | 31° | 5° | 5° | 30° | 9° | |
| 3 | 70° | 48° | 62° | 38° | 77° | 40° | 34° | 33° | 5° | 8° | 32° | 5° | |
| 4 | 65° | 62° | 70° | 32° | 50° | 32° | 26° | 22° | 3° | 3° | 33° | 3° | |
| 5 | 72° | 42° | 23° | 43° | 50° | 55° | 30° | 26° | 1° | 3° | 20° | 4° | |
| 6 | 65° | 35° | 28° | 19° | 53° | 22° | 35° | 23° | 5° | 7° | 43° | 4° | |
| 7 | 48° | 38° | 38° | 10° | 48° | 22° | 37° | 18° | 7° | 6° | 33° | 4° | |
| 8 | 53° | 75° | 63° | 20° | 47° | 38° | 35° | 30° | 5° | 8° | 30° | 9° | |
| 9 | 76° | 48° | 62° | 38° | 77° | 40° | 34° | 33° | 5° | 8° | 32° | 5° | |
| 10 | 50° | 35° | 20° | 25° | 52° | 20° | 22° | 15° | 0° | 2° | 26° | 2° | |
| 11 | 65° | 36° | 30° | 43° | 58° | 20° | 30° | 20° | 2° | 3° | 38° | 3° | |
| 12 | 50° | 54° | 53° | 25° | 68° | 38° | 35° | 38° | 6° | 10° | 43° | 6° | |
| 13 | 50° | 48° | 45° | 35° | 63° | 42° | 42° | 32° | 9° | 10° | 38° | 3° | |
| 14 | 68° | 45° | 41° | 40° | 50° | 38° | 33° | 10° | 0° | 2° | 34° | 4° | |
| 15 | 60° | 55° | 35° | 48° | 67° | 42° | 28° | 18° | 0° | 3° | 25° | 1° | |
| 16 | 48° | 38° | 29° | 28° | 48° | 22° | 23° | 18° | 0° | 2° | 25° | 4° | |
| 17 | 54° | 38° | 20° | 30° | 48° | 28° | 22° | 20° | 1° | 2° | 31° | 1° | |
| 18 | 55° | 45° | 37° | 40° | 50° | 28° | 33° | 31° | 6° | 9° | 49° | 17° | |
| 19 | 65° | 35° | 28° | 28° | 55° | 22° | 35° | 30° | 6° | 9° | 43° | 8° | |
| 20 | 77° | 50° | 24° | 26° | 48° | 23° | 36° | 20° | 3° | 6° | 25° | 8° | |
Table 4: Pre-and postoperative angle measure. TCA1: anterior talocalcaneal angle; TNA: talonavicular angle; TNCA: talonavicular coverage angle; TFMA1: anterior talo-first metatarsal angle; TCA2: lateral talocalcaneal angle; and TFMA2: lateral talo-first metatarsal angle.
Anterior talocalcaneal angle (TCA1)
Preoperative measure ranged from 48° to 77° with the average of 60.4°, while postoperative measure 20° to 42° with the average of 31.3°.
Talonavicular angle (TNA)
Preoperative measure ranged from 35° to 77° with the average of 47.2°, while postoperative measure 15° to 38° with the average of 24.8°.
Talonavicular coverage angle (TNCA)
Preoperative measure ranged from 20° to 70° with the average of 40°, while postoperative measure 0° to 9° with the average of 3.6°.
Anterior talo-first metatarsal angle (TFMA1)
Preoperative measure ranged from 10° to 48° with the average of 31.5°, while postoperative measure 2° to 10° with the average of 5.5°.
Lateral talocalcaneal angle (TCA2)
Preoperative measure ranged from 47° to 77° with the average of 55.5°, while postoperative measure 20° to 49° with the average of 33.5°.
Lateral talo-first metatarsal angle (TFMA2)
Preoperative measure ranged from 15° to 55° with the average of 31.3°, while postoperative measure 1° to 17° with the average of 5.25°.
Table 5 shows the average pre- and post-operative all angles measures with calculation of the standard deviation (STD) through its mathematical equation.
| Angle | Average measure ± STD | Average measure ± STD |
|---|---|---|
| Preoperative | Postoperative | |
| TCA1 | 60.4° ± 12.2° | 31.3°± 8.6° |
| TNA | 47.2° ± 8.4° | 24.8°±4.1° |
| TNCA | 40° ± 6.7° | 3.6° ± 1.2° |
| TFMA1 | 31.5° ± 5.9° | 5.5° ± 0.9° |
| TCA2 | 55.5° ± 9.6° | 33.5° ± 6.3° |
| TFMA2 | 31.3° ± 6.5° | 5.25° ± 1.1° |
Table 5: Pre- and post-operative average angle measure.
TCA1: anterior talocalcaneal angle; TNA: talonavicular angle; TNCA: talonavicular coverage angle; TFMA1: anterior talo-first metatarsal angle; TCA2: lateral talocalcaneal angle; and TFMA2: lateral talo-first metatarsal angle.
No major complication occurred. Only superficial wound infection occurred in one case (no. 9). It was treated by local wound debridement and antibiotic administration. The infection was eradicated within two weeks and followed up for 24 months without recurrence. No case of deep infection was recorded.
Clinical and radiographic assessments were achieved over the follow-up period (Figures 6-11).
Figure 8: Preoperative radiography: AP view right feet showing talar head medial subluxation out of the navicular socket with angle measure of TCA1 65° (A), TNA 62° (B), TNCA 70° (C), and TFMA1 32° (D); and Lateral views right foot showing plantarflexion of the talus on the calcaneus with angle measure TCA2 50° (E), and TFMA2 32°(F).
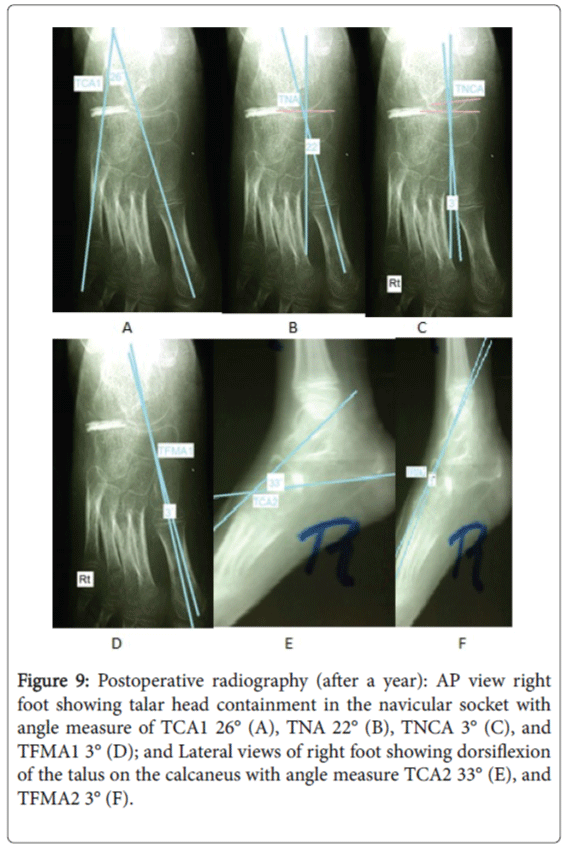
Figure 9: Postoperative radiography (after a year): AP view right foot showing talar head containment in the navicular socket with angle measure of TCA1 26° (A), TNA 22° (B), TNCA 3° (C), and TFMA1 3° (D); and Lateral views of right foot showing dorsiflexion of the talus on the calcaneus with angle measure TCA2 33° (E), and TFMA2 3° (F).
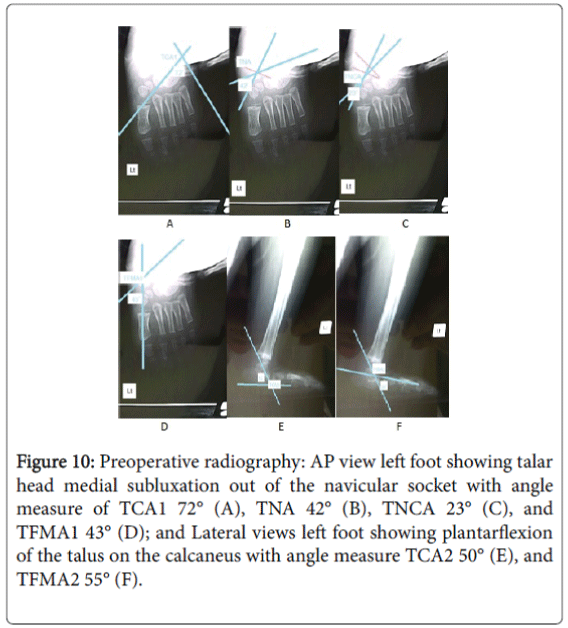
Figure 10: Preoperative radiography: AP view left foot showing talar head medial subluxation out of the navicular socket with angle measure of TCA1 72° (A), TNA 42° (B), TNCA 23° (C), and TFMA1 43° (D); and Lateral views left foot showing plantarflexion of the talus on the calcaneus with angle measure TCA2 50° (E), and TFMA2 55° (F).
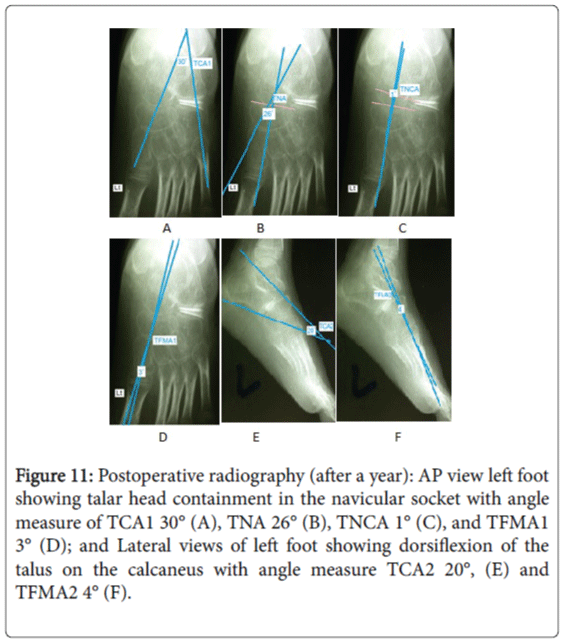
Figure 11: Postoperative radiography (after a year): AP view left foot showing talar head containment in the navicular socket with angle measure of TCA1 30° (A), TNA 26° (B), TNCA 1° (C), and TFMA1 3° (D); and Lateral views of left foot showing dorsiflexion of the talus on the calcaneus with angle measure TCA2 20°, (E) and TFMA2 4° (F).
The results were graded into four categories as excellent, good, fair, and poor according to the total calculated score. If the total score was 18–20, the result would be considered excellent, 15–17 would be good, 12–14 would be fair, and <12 would be poor. According to this grading system, there were 8 excellent results, 8 good results, 4 fair results, and no poor results (Table 6).
| Category | Total Score | Number of cases |
|---|---|---|
| Excellent | 18 – 20 | 8 |
| Good | 15 –17 | 8 |
| Fair | 12 – 14 | 4 |
| Poor | < 12 | 0 |
Table 6: Categories and number of cases.
Discussion
Cerebral palsy (CP) is a permanent non-progressive brain damage which mainly affects the cognitive and motor functions due to perinatal brain insult. The spastic type of cerebral palsy (CP) accounts for 85% of the affected patients; and results in muscle imbalance, joint deformity, torsional malalignmen, bony changes in growing children, and disturbed gait pattern in ambulatory patients [11].
Hindfoot valgus deformity is common in spastic cerebral palsy (CP), especially in diplegia [12]. Because of the spasticity and muscular contractures, alterations develop in the anatomic relation between the tarsal bones. These changes include external rotation of the calcaneus, and internal rotation and inferior subluxation of the talus. Additional structural alterations develop because of the abnormal forces applied through the mid- and forefoot and loss of stability, which result in midfoot break [13]. Foot pain accompanies the foot deformity and results from midfoot break with prominant talar head in the weightbearing part of the foot [11,13]. Radiographically, there is increase in the anterior talocalcaneal Kite's angle, talonavicular angle, talonavicular coverage angle, anterior talo-first metatarsal angle, lateral talocalcaneal angle and lateral talo-first metatarsal Meary's angle [14-18]. A short stride length and low velocity are also observed owing to spasticity, which also causes a reduced step length. With progression of the deformity, other pathologic features develop, including forefoot supination and hallux valgus [19].
Surgery is the definitive measure which is indicated in moderate to severe hindfoot valgus deformity causing mechanical instability affecting the child's gait; and in children not tolerating the ankle-foot orthoses (AFO) or not responding to prolonged non-operative course (at least 6 months) with persistent pain, deformity, callus or skin ulceration [20]. Surgical interventions improve the gait as examined by gait analysis [21]. Multilevel surgeries, soft tissue and bony procedures, if well selected have significant improvement in ankle and foot functions as well as the spastic muscle function [22]. Numerous operative procedures have been described in the last decades to correct hindfoot valgus deformities.
There are four levels of surgical correction of hindfoot valgus deformity: (1) soft-tissue procedures alone; (2) osteotomies, (3) pseudoarthrodesis or arthroereisis without arthrodesis; and (4) arthrodesis, either limited, or triple arthrodesis.
The simplest soft-tissue procedures include Achilles' tendon lengthening (ATL) and/or peroneal tendon lengthening [23]. In general, soft-tissue procedures alone cannot withstand the forces of weight bearing, and the deformity tends to recur [24]. They only convert painful deformity to a painless one, owing to the fact that pes valgus deformity and the depressed medial longitudinal arch had both muscular as well as bony contributions. Most surgeons combine softtissue procedures with concurrent bony procedures to change the shape of the foot [24,25].
The second level of surgical intervention for hind foot valgus includes osteotomies. Most of the reports of various osteotomies to correct hind foot valgus deformity were relatively small series with short follow-up. The Dwyer [26] lateral opening-wedge osteotomy of the posterior calcaneus to correct hindfoot valgus was located at the subtalar joint STJ injuring it, and was not located at the angle or centre of rotational angulation (CORA) of the deformity. Evans [27] recommended elongation of the lateral column as a treatment for planovalgus or calcaneovalgus foot, but stated at that time that the operation was inappropriate for children with spastic paresis because of high prevalence of overcorrection, or in other paralytic children because of osteopenia and muscle imbalance deteriorating the results. Phillips [28] reported 20-year follow-up on 23 of the feet originally operated for calcaneal lengthening osteotomy by Evans [27] as good or very good results in 17 feet but did not define the criteria for classifying results. There were also noted degenerative changes in the calcaneocuboid joint in all 15 of the patients with good results. More recently, Mosca [1], Andreacchio et al. [2] and Hanna et al. [3], modified the procedure described by Evans and reported the ability of the lateral foot column lengthening to correct the abnormal anatomy of the deformity while preserving the subtalar joint (STJ) motion. Mosca [1] reported at an average of 2 to 3 years of follow-up, satisfactory results in 29 of 31 feet, and failure in the two feet with the most severe deformity. Eight had the addition of either cuneiform wedge osteotomy or talocalcaneal arthrodesis. Andreacchio et al. [2] reported at an average of 4.1 years of follow-up, 17 feet had good, 2 fair, and 4 poor outcomes which resulted from recurrence of deformity. Hanna et al. [3], reported at an average of 2 years of follow-up, 5 feet had excellent, 17 good, 5 fair, and no poor results. Previous studies showed that calcaneal lengthening osteotomy was suitable for mild to moderate, flexible hindfoot valgus deformity [2,29]. In contrast, some studies recommended calcaneal lengthening, even for severe hindfoot valgus deformity [1]. Because of the anatomic variation of the anterior and middle articular facets of the calcaneus, the calcaneal lengthening osteotomy can be intra-articular causing articular damage to the subtalar joint (STJ) [30]. Torosian et al. [31] described a displacement osteotomy of the os calcis only to correct hindfoot valgus in myelomeningocoele with subtalar joint (STJ) preservation. The procedure succeeded to correct the valgus in 31 out of 38 feet over a follow-up period more than 5 years, but failed to correct forefoot abduction or medial longitudinal arch collapse [32]. Rathjen et al. [9], described a combination of a sliding calcaneal osteotomy, an openingwedge cuboid osteotomy, and a pronation, plantarflexion closing wedge osteotomy of the medial cuneiform in addition to appropriate soft-tissue releases; and compared favorably with similar series in achieving excellent foot alignment parallel to the axis of progression in 23 out of 24 feet over a follow-up period of an average of 1½ years. However, violation of the subtalar joint (STJ) articular surface owing to anatomic variation of the calcaneal facets [30].
In the current study, the calcaneus was preserved of osteotomy. Through a double column foot osteotomy, the medial foot column was shortened by a plantarward based medial cuneiform closing wedge, while the lateral foot column was lengthened by a laterally based cuboid opening wedge filled by wedge resected from the medial cuneiformm. The procedure was applied to moderate and severe mobile (flexible) hindfoot valgus and reported 20 feet over a follow-up period of an average of 1 years; 8 excellent, 8 good, 4 fair, and no poor results; according to a preset scoring system combining both clinical and radiographic results. It was not only a redirectional osteotomy of the acetabulum pedis that corrects subluxation or dislocation of the subtalar joint (STJ), but also strengths the windlass mechanism by tightening the plantar fascia restoring the medial longitudinal arch height [33]. It had the advantage of lateral column foot lengthening, the medial column foot shortening, and the preservation of the subtalar joint (STJ) mobility.
This study arrived at the fact that paralytic subtalar hindfoot valgus is presented with certain pattern of muscle paresis, depending on foot evertors/invertors power. There were two patterns of muscle paresis, namely, without or with evertors/invertors imbalance. Though the two groups differ in pathogenesis, there is no much difference in the outcome. The first group with no evertors/invertors imbalance is mostly due to developmental changes in the foot, as bowstringing of the calcaneus predisposing to talonavicular subluxation, and ligamentous laxity depressing the medial longitudinal arch. The second group with evertors/invertors imbalance is mostly due to adaptive changes caused by forces on the foot with powerful peronei relative to tibialis anterior and posterior muscles, also, powerful long toes extensors, driving the talonavicular joint to subluxate laterally. In the two patterns, the other components of the deformity are exactly the same. Cases with muscle imbalance require, in addition to double column foot osteotomy, peroneal tendon lengthening. Also cases with powerful triceps surae require Achilles’ tendon lengthening provided that there is no strong dorsiflexors.
The third level of surgical intervention is peudoarthrodesis or arthroereisis of the subtalar joint (STJ) to restrict eversion either by placing a bone block in the sinus tarsi or by a synthetic implant was followed by implant problems [34]. Pisani [35] used a cancellous screw and a silastic or polypropylene dome of high molecular weight. It is a non comparable modality to the current study.
The fourth or final level of surgical intervention is a salvage procedure of either limited fusion or multiple joint fusion of the subtalar joint (STJ) complex. Limited or extra-articular arthrodesis of the subtalar joint initially described by Grice [4] had the benefit of preserving the subtalar articular joint cartilage with minor interference with bone growth, but was followed by recurrence of the foot deformity due to graft resorption or failure. It was mainly provided to patients with poor ambulation. Triple arthrodesis represents the final and most definitive surgical option for valgus foot deformity. It is reliable in correcting deformity and maintaining normal foot position. Unfortunately, it also increases the stresses at adjacent joints and limits the growth of the foot in children [36].
In conclusion, the double column foot osteotomy shortening the medial foot column by medial cuneiform closing wedge and lengthening the lateral foot column by cuboid opening wedge osteotomy to correct moderate to severe hindfoot valgus in ambulatory children with spastic cerebral palsy (CP) compared favourably with similar series that used other techniques, and offered option for achieving foot alignment, improving pain and skin problems and avoiding the problems associated with arthrodesis. A long-term follow-up with a larger patient population series was recommended to detect any recurrent or residual hindfoot deformity.
References
- MoscaVS (1995) Calcaneal lengthening for valgus deformity of the hindfoot. J Bone Joint Surg Am 77: 500 –512.
- Andreacchio A, Orellana CA, Miller F, Bowen TR (2000) Lateral column lengthening as treatment for planovalgus foot deformity in ambulatory children with spastic cerebral palsy. J PediatrOrthop 20: 501 –505.
- Hanna AAZ, Al-Inani WG, Borai AN, Bishay SNG (2004) Surgical correction of valgus foot deformity by lateral column lengthening in ambulatory children with cerebral palsy. Kasr El Aini Medical Journal 10: 107 – 114.
- Grice DS (1952) An extra-articular arthrodesis of the subastragalar joint for correction of paralytic flat feet in children. J Bone Joint Surg Am 34: 927 – 940.
- Ross PM, Lyne ED (1980) The Grice procedure: indications and evaluation of long-term results. ClinOrthopRelat Res 153: 194 – 200.
- Hsu LCS, Jaffary D, Leong JCY (1986) The Batchelor-Grice extra-articular subtalar arthrodesis. J Bone Joint Surg (Br) 68: 125 – 127.
- Mosca VS (2009) Flexible flatfoot and skewfoot. In:Drennan's the child's foot and ankle (2nd edn.) Lippincott Williams and Wilkins,Philadelphia. pp: 136 – 159.
- Sensiba PR, Coffey MJ, Williams NE, Mariscalco M, Laughlin RT (2010) Inter- and intraobserver reliability in the radiographic evaluation of adult flatfoot deformity. Foot Ankle Int 31:141 – 145.
- Rathjen KE, Mubarak SJ (1998) Calcaneo-cuboid- cuneiform osteotomy for the correction of valgus foot deformities in children. J PediatrOrthop 18:775 – 782.
- Stevens PM, Toomey E (1988) Fibular-Achilles tenodesis for paralytic ankle valgus. J PediatrOrthop 8: 169 – 175.
- Miller F (2005) Neurologic control of the musculoskeletal system. In: Cerebral Palsy, Miller Springer New York.pp: 90 – 150.
- O'Connell PA, D'Souza L, Dudeney S, Stephens M (1998) Foot deformities in children with cerebral palsy. J PediatrOrthop 18: 743 – 747.
- Kadhim M, Holmes L, Miller F (2013) Long-term outcome of planovalgus foot surgical correction in children with cerebral palsy. J Foot Ankle Surg 52: 697 – 703.
- Metcalfe SA, Bowling FL, Baltzopoulos V, Maganaris C, Reeves ND (2012) The reliability of measurements taken from radiographs in the assessment of paediatric flatfoot deformity. The Foot 22: 156 – 162.
- Adelman VR, Szczepanski JA, Adelman RP (2008) Radiographic evaluation of endoscopic gastrocnemius recession, subtalar joint arthroereisis, and flexor tendon transfer for surgical correction of stage II posterior tibial tendon dysfunction: a pilot study. J Foot Ankle Surg 47: 400 - 408.
- Isikan VE (1993) The values of talonavicular angles in patients with pesplanus. J Foot Ankle Surg 32: 514 – 516.
- Davitt JS, Mac Williams BA, Armstrong PF (2001) Plantar pressure and radiographic changes after distal calcaneal lengthening in children and adolescents. J PediatrOrthop 21: 70 – 75.
- Loza ME, Bishay SNG, El-Barbbary HM, Hanna AAZ, Tarraf YN, et al. (2010) Double column osteotomy for correction of residual adduction deformity in idiopathic clubfoot. Ann R CollSurgEngl 92: 673 – 679.
- Kun BP, Hui WP, Ki SL, Sun YJ, Hyun WK (2008) Changes in dynamic foot pressure after surgical treatment of valgus deformity in the hindfoot in cerebral palsy. J Bone Joint Surg 90: 1712 – 1721.
- Herring JA (2008) Flexible flatfoot (pesplanovalgus). In:Tachdjian's Pediatric Orthopaedics (4th edn) Saunders, Philadelphia. pp: 1054 – 1068.
- Katharine JB, Sylvia O, De Luca PA, Romness MJ (2002) Natural progression of gait in children with cerebral palsy. J PediatrOrthop22:677 – 682.
- Saraph V, Zwick EB, Zwick G, Steinwender C,Steinwender G, et al. (2002) Multilevel surgery in spastic diplegia: evaluation by physical examination and gait analysis in 25 children. J PediatrOrthop 22: 150 – 157.
- Jones BS (1975) Flat foot: a preliminary report of an operation for severe cases. J Bone Joint SurgBr 57: 279 – 282.
- Bouchard M, Mosca V (2014) Flatfoot deformity in children and adolescents: surgical indications and managements. J Am AcadOrthopSurg 22: 623 – 632.
- Mosca VS (2010) Flexible flatfoot in children and adolescents. J Child Orthop 4: 107 – 121.
- Dwyer FC (1959) Osteotomy of the calcaneum for pescavus. J Bone Joint Surg (Br) 41: 80 – 86.
- Evan D (1975) Calcaneovalgus deformity. J Bone Joint Surg 57: 270 – 278.
- Philips GE (1983) A review of the elongation of oscalcis for flat feet. J Bone Joint Surg 65:15–18.
- Dogan A, Zorer G, Mumcuoglo EI, Akman EY (2009) A comparison of two different techniques in the surgical treatment of flexible pesplanovalgus: calcaneal lengthening and extra-articular subtalar arthrodesis. J PediatrOrthop B 18: 167–175.
- Ragab AA, Stewart SI, Cooperman DR (2003) Implications of subtalar joint anatomic variation in calcaneal lengthening osteotomy. J PediatrOrthop 23: 79 – 83.
- Torosian CM, Dias LS (2000) Surgical treatment of severe hindfoot valgus by medial displacement osteotomy of the oscalcis in children with myelomeningocoele. J PediatrOrthop 20: 226 – 229.
- Easley ME, Trnka HJ, Schon LC, Myerson MS (2000) Isolated subtalar arthrodesis. J Bone Joint SurgAm 82: 613 – 625.
- Kim JR, Shin SJ, Wang SI, Kang SM (2013) Comparison of lateral opening wedge calcaneal osteotomy and medial calcaneal sliding-opening wedge cuboid-closing wedge cuneiform osteotomy for correction of planovalgus foot deformity in children. J Foot Ankle Surg 52: 162 – 165.
- Zaret DI, Myerson MS (2003) Arthroereisis of the subtalar joint. Foot Ankle Clin 8: 605 – 617.
- Da Silva LAA, De Barros Fucs PMM (2010) Surgical treatment of planovalgus foot in cerebral palsy by Pisani'sarthroereisis. ActaOrthop Bras 18: 162 – 165.
- Kiewiet NJ, Benirschke SK, Brage ME (2014) Triple arthrodesis: tips and tricks to navigate trouble. Foot Ankle Clin. 19:483 – 497.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14195
- [From(publication date):
September-2016 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 13251
- PDF downloads : 944