Case Report Open Access
Does Timing of Aerobic Walking Impact Blood Glucose Control and Personal Preference in Adults with Type 2 Diabetes?
Cory D Cox MS1 and Daniel J Cox2*
1Winthrop University Department of Kinesiology, Rock Hill, South Carolina, USA
2University of Virginia Health Sciences Center, Charlottesville, Virginia, USA
- *Corresponding Author:
- Daniel J Cox
Department of Psychiatry and Neurobehavioral Sciences
Box 800-223, University of Virginia Health System
Charlottesville, Virginia 22908, USA
Tel: 434-982-8021
Fax: 434-924-0185
E-mail: djc4f@hscmail.mcc.virginia.edu
Received date: May 26, 2016; Accepted date: September 07, 2016; Published date: September  15, 2016
Citation: Cox CDMS, Cox DJ (2016) Does Timing of Aerobic Walking Impact Blood Glucose Control and Personal Preference in Adults with Type 2 Diabetes?. J Aerobics Fitness 1:105.
Copyright: © 2016 Cox CDMS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Aerobics & Fitness
Introduction
Aerobic exercise has two primary benefits for people with type 2 diabetes (T2D): 1) It temporarily reduces insulin resistance up to 48 hours, and 2) It lowers blood glucose (BG) even in the absence of effective insulin action [1]. Therefore, a dose of exercise should indirectly lower BG by reducing insulin resistance. Exercising after meals while BG is rising should directly lower postprandial glucose (PPG), a primary contributor to glycosylated hemoglobin [2] and a risk factor for cardiovascular disease [3]. The only exercise guidelines given in the ADA’s 2012 Position Statement [4] on the management of T2D were, “As much physical activity as possible should be promoted, ideally aiming for at least 150 min/week of moderate activity including aerobic, resistance, and flexibility training”.
DiPietro [5] demonstrated that 45 minutes of aerobic walking, whether done in three 15-minute bouts after meals or in a single dose, similarly and significantly lowered 24-hour BG among adults at risk for developing T2D. Aerobic walking performed after meals, however, led to significantly lower postprandial BG. Not only is the type and timing of exercise important, but compliance among individuals with T2D is also critical. It may be that doing several 15-minute bouts of postprandial exercise is preferable to a single 45-minute block.
Methods
This pilot study replicated DiPietro’s hospital-based investigation and extended it to include: 1) Adults with T2D, 2) During their daily routine, 3) While documenting personal preference for and performance of the two types of physical activity. Both studies incorporated a cross-over design. Three adults participated whose ages were 64, 60, 65 years, genders were M, F, M, and BMI was 25.4, 41.2, 31.2 respectively. They were all diagnosed with T2D within the last 5 years and were not taking diabetes medication. Data collection occurred only after subjects signed a consent form approved by the University of Virginia ethics committee. In the study, they performed self-monitoring of blood glucose (SMBG) before meals, two hours after meals and at bedtime. This was done for four consecutive days (days 1-2 were controls and 3-4 were experimental days), for each of three conditions presented in a randomized order (12 days total). The 2 control days were important since aerobic activity can impact insulin resistance for up to 48 hours [6]. On the control days, a maximum of 6,000 steps and 100 aerobic steps (quantified by HJ-323U Multi- Function Downloadable Pedometer) was required so as to not influence the experimental days (days 3-4). The three experimental conditions implemented during days 3-4 were: 1) the Sedentary condition, wheresubjects restricted aerobic walking to a maximum of 6,000 steps and 100 aerobic steps, 2) the 15-PPG condition, where subjects performed 15 minutes of aerobic walking (>108 steps/min) starting 30 minutes after each of three daily meals, and 3) the 45-Block condition, where subjects performed 45 minutes of continuous aerobic walking two hours or more after starting their evening meal. To ensure stability in the three test conditions, BG was averaged over days 3-4, SMBG (as measured with a Verio IQ meter, LifeScan Inc.) was measured twice and averaged at each of the seven daily measurement points, and subjects were asked to eat the same meals during all experimental days. The latter was confirmed with 24 hours ASA dietary recall [7].
One month following the intervention, subjects were telephoned and asked which exercise format they preferred, and how much and when they walked aerobically in the previous seven days.
Results
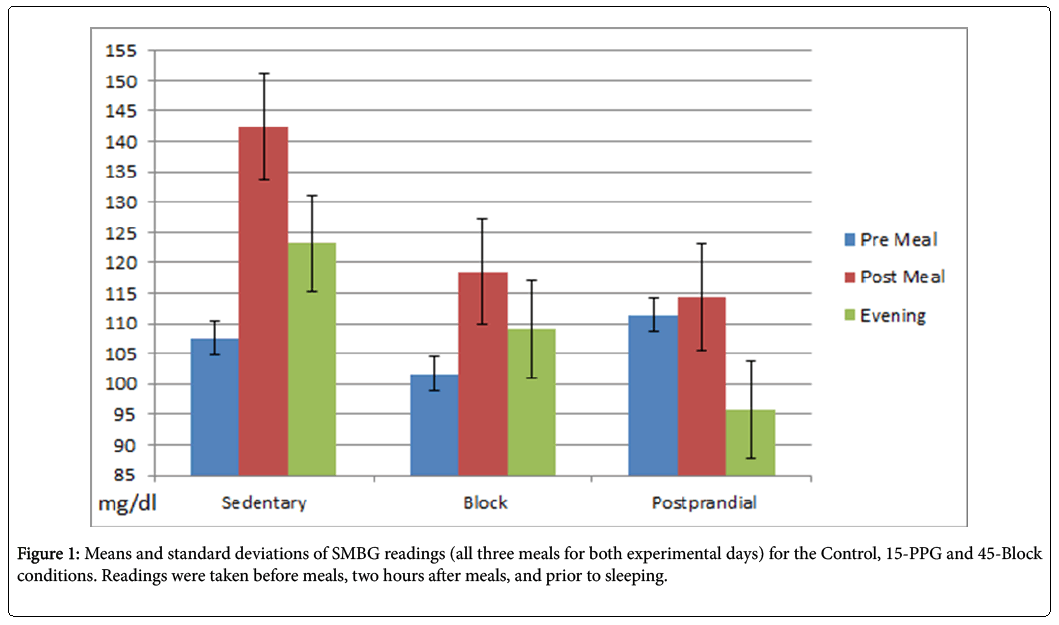
For the Sedentary, 15-PPG and 45-Block conditions, subjects averaged 0, 45.6, and 46.5 min/day of aerobic walking respectively, affirming the experimental manipulation. With 28 SMBG readings/ subject (2 days X 7 readings X 2 SMBG/reading), mean BG for the Sedentary, 15-PPG and 45-Block conditions was 123.8, 109.9 and 109.0 mg/dl respectively, reflecting extremely good metabolic control for T2D patients not taking diabetes medication. Mean PPG averaged across the two experimental days and three meals was 142.3, 114.7 and 119.90 mg/dl for the sedentary, 15-PPG and 45-Block conditions respectively. The respective mean pre to post BG change was 35.3, 3.1, and 18.5 mg/dl (Figure 1). At one month follow-up, all subjects reported preferring 15-PPG over 45-Block exercise, and performing an estimated 495 minutes of block and 555 minutes of postprandial aerobic walking during the previous week.
Conclusion
These data confirm that adults with T2D benefit metabolically from 45 minutes/day of aerobic walking. More specifically, it indicates for the first time that individuals with T2D can lower PPG when this is broken down into three 15-minute segments after meals. Further, these individuals prefered 15-minute segments and perform more minutes of exercise when it is done in 15 minute segments rather than a block of 45 minutes. These data affirm laboratory findings [5] of pre-diabetic individuals that generally indicate post-meal aerobic walking is associated with lower post-meal SMBG readings. In conclusion, it may be more metabolically effective and behaviorally efficient to encourage those with T2D to engage daily in several brief post-meal exercise periods rather than a single, lengthy block of exercise.
References
- Turcotte LP, Fisher JS(2008) Skeletal muscle insulin resistance: Roles of fatty acid metabolism and exercise. Phys Ther 88: 1279-1296
- Monnier L, Lapinski H, Colette C (2003)Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients.Diabetes Care 26:881-885.
- Barrett-Connor E, Ferrara A(1998) Isolated postchallenge hyperglycemia and the risk of fatal cardiovascular disease in older women and men: The Rancho Bernardo Study. Diabetes Care 21: 1236–1239.
- Inzucchi SE, Bergenstal RM, Buse JB,Diamant M, Ferrannini E, et al.(2013)Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care35: 1364-1379.
- DiPietro L, Gribok A,Stevens MS, Hamm L, Rumpler W (2013) Three 15-min bouts of moderate postmeal walking signigicantly improves 24-h glycemic control in older people at risk for impaired glucose tolerance. Diabetes Care 36: 3262-3268.
- Zacker R (2005) Strength training in diabetes management. Diabetes Spectrum 18:71-75.
- Subar AF, Kirkpatrick SI, Mittl B, Zimmerman TP, Thompson FE, et al. (2012) The automated self-administered 24-hour dietary recall (ASA24): a resource for researchers, clinicians, and educators from the National Cancer Institute. J Acad Nutr Diet 112: 1134-1137.
Relevant Topics
- Active Life Style
- Aerobic Capacity
- Aerobic Dance
- Aerobic Exercise
- Aerobic Metabolism
- Aerobic Respiration
- Aerobics in Pregnancy
- Aqua Aerobic
- Brain Aerobic
- Cardio Exercise
- Cardiovascular Efficiency
- Diet and Fitness
- Fitness Tips
- Health Fitness
- Kids Aerobics
- Metabolic Rate
- Muscular Endurance
- Muscular Strength
- Physical Training
- Respiratory Endurance
- Role of Proteins in Fitness
- Sport Aerobics
- Step Aerobics
- Steroids and Fitness
- Weight Loss Plans
Recommended Journals
Article Tools
Article Usage
- Total views: 10849
- [From(publication date):
July-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 10029
- PDF downloads : 820