Does the Third Sputum Exam has an Added Value in the Diagnosis of Pulmonary Tuberculosis?
Received: 11-Dec-2017 / Accepted Date: 28-Dec-2017 / Published Date: 04-Jan-2018
Abstract
Introduction: Current practice of examining three sputum for the diagnosis of pulmonary tuberculosis (PTB) has tended to overburden the already scarce human resources in all-purpose laboratories, and to increase the turn-around- time for patients seeking treatment. Therefore, assessing the added value of the third sputum in the diagnosis of PTB in resource-limited country with less functional External Quality Assurance (EQA) system is critical.
Materials and methods: Data on patients diagnosed with smear-positive PTB during 2012-2016 was collected retrospectively from laboratory register of nine hospitals in Eritrea. The data was extracted and analyzed for incremental yield of three sputum samples.
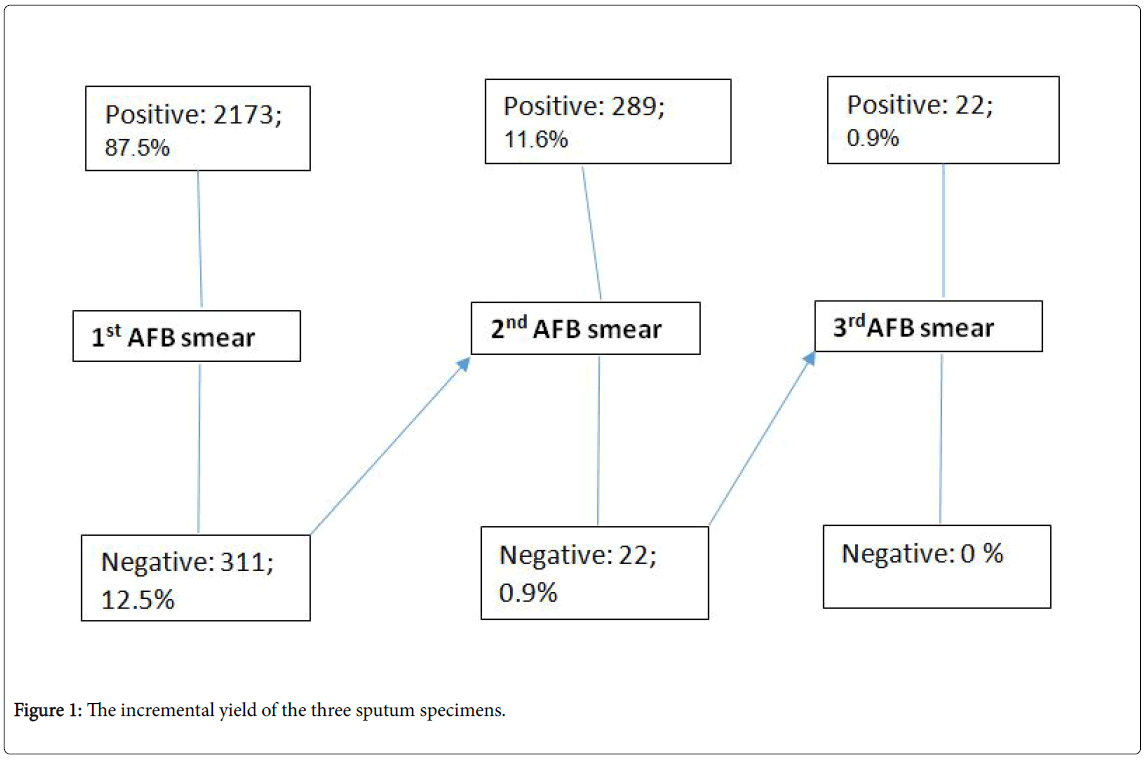
Results: Data from 2,484 microscopically confirmed acid-fast bacilli (AFB) smear positive PTB patients were reviewed. AFB was detected in the first sputum in 87.5% of patients, and 99.1% for the combined first and second sputum specimens. The incremental yield of the third sputum specimen as a diagnostic value was only 0.9%. No significant variation was detected by region, residence, gender or HIV.
Conclusion: The added value of the third sputum is so minimal that its omission will reduce patient visits, workload and cost for patients and health services. Therefore, even countries like Eritrea, with limited EQA, should consider limiting the number of sputum examinations to improve quality.
Keywords: Acid-fast bacilli; Incremental yield; Sputum smear microscopy; Tuberculosis
Introduction
Tuberculosis (TB) continues to contribute significantly to the global disease burden, especially in developing countries [1]. According to the 2016 Global TB report, at the end of 2015 there were 10.4 million new TB cases globally with 6 countries accounting for the 60% of cases and 1.4 million TB deaths [1]. As in other developing countries, TB is one of the public health problems in Eritrea, a country located in the horn of Africa with an estimated population of 3.75 million. The annual incidence and mortality rate of tuberculosis in Eritrea at the end of 2015 was 65/100,000 and 13/100,000 population, respectively with Multi-Drug Resistant (MDR-TB) rate of 2.7% among all TB patients [1]. The disease was also one of the top 10 causes of admission and death in hospitals and health centers in both HIV negative and positive patients Health Management Information System (HMIS- 2016) report. The core element of TB control is an effective detection and treatment of patients, i.e., to identify and treat early the smear positive cases in order to reduce the prevalence and spread of this airborne infectious disease in the community [2]. World Health Organization and the International Union Against Tuberculosis and Lung Disease (The Union) guidelines states that a definite diagnosis is only established if Mycobacterium tuberculosis is isolated from coughed out respiratory specimens [2]. Despite the recent introduction of new molecular diagnostic tools such as (XpertMTB/Rif), the diagnosis of tuberculosis and monitoring of treatment in Eritrea will continue relying heavily on bacteriological examination of clinical specimens using conventional microscopes.
In accordance with international guidelines, the National Guideline for TB and Leprosy Control recommends the microscopic examination of three serial sputum specimens for all presumptive PTB cases in order to detect the presence of acid-fast bacilli (AFB) [3,4]. The first and third sputum specimens are collected in the health facility (spot specimens) and the second is an early morning specimen, usually collected at home [5,6]. Though, TB diagnosis is integrated in the general health care laboratories, most of the laboratories are singleroomed and understaffed with one or two medical laboratory technologists that carry out additional laboratory duties on a daily basis, making it difficult for them to handle high volume workloads. Some of the laboratories also lack consistent source of electricity and clean water, hence affecting the delivery of results. The inadequate numbers of staff, the workload from the various tests are factors that can affect the quality of the test as sensitivity of direct smear assay is highly dependent on sufficient time spent on preparing, staining, and reading of each smear [7]. The recommended three sputum samples that are done on two consecutive days may also affect turn-around time for diagnosis (from 24 hours to 2-3 days), and early initiation of treatment to reduce the airborne infectious disease and spread of infection in the community [7]. It may also result in increased cost for patients and dropping out of the diagnostic path way leading to untreated smear-positive patients and thus uninterrupted transmission. Therefore, to reduce the overload and cost of these laboratories and turn-around time of patients, WHO has recommended the reduction of sputum examination to two sputum examination and same-day sputum examinations in countries with well-established laboratory networks and EQA systems [8,9].
The National Guideline for TB and Leprosy Control recommends three sputum examinations for the diagnosis of presumptive PTB. However, no study had so far been conducted to assess the yield of the three sputum exams, the convenience and cost to patients and the workload to the laboratory technologists and its effect on quality. The aim of this study is therefore to examine the added value of the third sputum in the diagnosis of presumptive PTB cases in a developing country with a less well established External Quality Assurance (EQA) system.
Materials and Methods
The study was a retrospective secondary data analysis of data collected from the laboratory register of smear-positive sputa in the period 2012-2016. The study was conducted in nine hospitals (three national and six regional referral hospitals and other three general hospitals) located in the six regions of the country. These hospitals were purposely selected for their high volume of sputum examinations for acid-fast bacilli (AFBs) and are responsible for the diagnosis of almost 70% of the TB patients in the country.
A standardized data extraction sheet was used to record all available patient demographic data and sputum results from the TB-laboratory registers. All new-smear positive sputa in at least one of the three specimens registered in TB-Lab register in the selected health facilities from 2012 to 2016 were included in the study. All the other types of specimens, all negative sputum results, and sputum tests done for follow up patients and incomplete sputum tests were excluded in the analysis. All the data extracted from the TB-registers were manually cleaned and entered into computer using an entry program developed for the purpose using CS Pro version 6.3.2 (census and survey processing system) software package. Then the cleaned data was analyzed using the Statistical Package for Social Science Version 22 (SPSS 22). The data was used to calculate the incremental yield of the three specimens by dividing each smear positive spot to total smear positive patients who had three specimens examined, at least one of which was positive. The analysis provided the statistical significance analysis of the diagnostic value of the three sputum specimens, especially the second and third specimens.
Ethical clearance
The study was approved by the Research Ethics and Protocol Review Committee of the Ministry of Health. As the study was retrospective, data collection was based entirely on data extraction from existing laboratory register with removal of all patient identifiers.
Results
A total of 2,484 patients with microscopically confirmed AFB-smear positive results were recorded in the TB laboratory register of the nine hospitals. Among these 1,251(50.4%) were male patients and 1,233 (49.6%) were female patients with sex ratio of almost 1:1.The majority of the patients 2,449 (98.6%) were in the age group 15 and above with mean age of 40 years. The highest proportions of patients were from Gash Barka Region followed by Maekel and the least proportion was from Southern Red Sea Region. The proportion of patients from urban area accounted for the 52% of collected data (Table 1).
| Background information | Number of cases | Percent | |
|---|---|---|---|
| Region | Maekel | 649 | 26.10% |
| Anseba | 293 | 11.80% | |
| Gash-Barka | 815 | 32.80% | |
| Debub | 297 | 12.00% | |
| Northern Red Sea | 337 | 13.60% | |
| Southern Red Sea | 93 | 3.70% | |
| Sex | Male | 1,251 | 50.40% |
| Female | 1,233 | 49.60% | |
| Residence | Urban | 1,296 | 52.20% |
| Rural | 1,188 | 47.80% | |
| Age group | <15 | 35 | 1.40% |
| 15+ | 2,449 | 98.60% | |
| Total | 2,484 | 100 | |
Table 1: Socio-demographic characteristics of patients.
A total of 7,452 sputum tests were recorded in the laboratory register with 3 sputum examination for each of the 2,484 patients. The first sputum test was done on the spot, the 2nd early was morning sample taken from home, and the 3rd was taken on the second day on spot. In 87.5% (2,173 samples) of the sputa, AFB was detected in the first sputum specimen. The incremental yield of the second sputum specimens when the first AFB-smeared slides were negative was 11.6% (289 cases). The value of the third sputum specimen as a diagnostic value when the first two specimens (1st spot and early morning samples) were negative was 0.9% (22 cases) (Figure 1).
The highest yield of the first spot was found in Gash Barka and Debub (90%), while the value of the third sputum specimen when the first two specimens were negative was below 2%in all six regions. Furthermore, there was no marked variation by sex, age group and residence on the yield of the first and incremental yield of the 2nd and 3rd sputum (Table 2).
| Yield of the three serial sputum specimens | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1st sputum | 2nd sputum | 3rd sputum | Total | ||||||
| cases | % | cases | % | cases | % | cases | % | ||
| Region | Maekel | 543 | 83.7 | 101 | 15.6 | 5 | 1 | 649 | 100 |
| Anseba | 244 | 83.3 | 45 | 15.4 | 4 | 1 | 293 | 100 | |
| Gash Barka | 746 | 91.5 | 65 | 8 | 4 | 1 | 815 | 100 | |
| Debub | 269 | 90.6 | 22 | 7.4 | 6 | 2 | 297 | 100 | |
| NRS | 291 | 86.4 | 43 | 12.8 | 3 | 1 | 337 | 100 | |
| SRS | 80 | 86 | 13 | 14 | 0 | 0 | 93 | 100 | |
| Sex | Male | 1084 | 86.7 | 156 | 12.5 | 9 | 1 | 1245 | 100 |
| Female | 1089 | 88.3 | 130 | 10.6 | 13 | 1 | 1227 | 100 | |
| Residence | Urban | 1121 | 86.5 | 163 | 12.6 | 12 | 1 | 1296 | 100 |
| Rural | 1052 | 88.6 | 126 | 10.6 | 10 | 1 | 1188 | 100 | |
| Age | <15 | 32 | 91.4 | 3 | 8.6 | 0 | 0 | 35 | 100 |
| 15+ | 2141 | 87.4 | 286 | 11.7 | 22 | 1 | 2449 | 100 | |
| Total | 2173 | 87.5 | 289 | 11.6 | 22 | 0.9 | 2484 | 100 | |
Table 2: Yield of the three sputum specimens in the six regions.
HIV status was recorded in the laboratory register in 1,266 (51%) of the patients. Out of these 139 were HIV positive with HIV prevalence of 11%. In those HIV infected patients, AFB was detected in the first on spot test in 119 cases (85.6%), in the second early morning sputum in 19 (13.7%) and the incremental yield of the third sputum was only 0.7%. indicating the similarity of yield in both HIV positive and HIV negative patients (Table 3).
| HIV Status | 1st sputum | 2nd sputum | 3rd sputum | Total |
|---|---|---|---|---|
| HIV Positive | 119 (85.6%) | 19 (13.7%) | 1 (0.7%) | 139 |
| HIV Negative | 991 (87.9%) | 133 (11.8%) | 3 (0.3%) | 1127 |
| Total | 1110 (87.7%) | 152 (12%) | 4 (0.3%) | 1266 |
Table 3: Yield of the three serial sputum specimens in patients with known HIV status TB patients.
Significance test results of the third sputum exam
In order to support the recommendation to whether exclude the third sputum test for the diagnosis of presumptive TB, the national percentage of the positive cases identified by the third test 0.9% [95% C.I: 0.6%, 1.3%], was taken as the decision criteria. Student t-one sample testing procedure of the SPSS was used to test whether there is statistically significant difference between the regions and HIV status and the national average results.
As presented in Table 3 the findings of the analysis revealed the exception of Debub region, the third sputum significance test procedure has identified positive cases below the national average. For Debub region, 2.7% of all positive cases were identified by third sputum sample, which was above the national average. However, the difference between the results of region Debub and National average was statistically not significant (P=0.172, >0.05). Moreover, the results by HIV status was below the national average and statistically not significantly different from the national average (0.9%) (Table 4).
| Region and HIV status | P-Value | Mean Difference | 95% Confidence Interval of the Difference | N | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Region | |||||
| Maekel | 0.706 | -0.12958 | -0.804 | 0.5449 | 649 |
| Anseba | 0.494 | 0.46519 | -0.8713 | 1.8017 | 293 |
| Gash-Barka | 0.095 | -0.4092 | -0.89 | 0.0716 | 815 |
| Debub | 0.172 | 1.1202 | -0.4891 | 2.7295 | 297 |
| NRS | 0.985 | -0.00979 | -1.0178 | 0.9982 | 337 |
| SRS | 0 | 0 | NA | NA | 93 |
| HIV status | |||||
| Positive | 0.802 | -0.18058 | -1.6031 | 1.2419 | 139 |
| Negative | 0 | -0.63381 | -0.9351 | -0.3325 | 1127 |
Table 4: Student t-one sample significance test result of the third Sputum testing procedure by region and HIV status of the patients.
Discussion
One of the key components of TB prevention and control program is an early detection of smear positive infectious PTB cases and early initiation of treatment to reduce person-to-person TB transmission within the community. Although, the best and preferable choice in identifying the mycobacterium tuberculosis is by growing the organism in culture media, which confirms the diagnosis and also provides the drug sensitivity, or by new diagnostic tools such as Polymerase Chain Reaction (PCR), their complexity and the need for well-established infrastructure and human resources, limits their use in Eritrea and many other resources-constrained countries. Therefore, AFB smear microscopy using three sputum specimens will remain the cornerstone for diagnosing most infectious cases of tuberculosis in most of the resource limited countries [10].
Of late, the practice of routinely examining three sputum specimens has become a great concern on delivering quality services in the diagnosis of PTB due to the need for frequent patient visits, the longer turn-around time, and additional strain on hospital human resources and expenses [11].
In this study the yield of the three sputum examinations was assessed and showed that majority (87.5%) of the patients were diagnosed by the first on spot sputum and the remaining few (11.6%) by the second morning sputum. The incremental yield of the third sputum indicated that its contribution to the diagnosis was negligible as almost all (99.1%) of the cases were detected with first two sputum examinations. The yield was similar in all the regions irrespective of residence, gender or HIV status.
This study agrees with similar studies conducted elsewhere that indicated the added diagnostic value of the third sputum specimen is small [12-14]. A study conducted in Bangladesh has shown that the examination of two consecutive sputum specimens was sufficient enough for the effective diagnosis of TB with only 2% diagnosed by the 3rd sputum [15]. Another study has also shown that examination of 2 consecutive specimens (on spot and overnight sputum) was large enough to detect most of the infectious cases i.e., 96% [16]. Different studies also indicated that the first two sputum smears can detect as much as 95% of the presumptive cases [17]. A systematic review of 37 eligible studies demonstrated that the average incremental yield of the third specimen, when the first two specimens were negative, was very small 3.1% [18].
The emergence of the HIV epidemic has led to a dramatic increase in the incidence of TB globally, resulting in marked increases in morbidity and mortality mainly in Africa [19,20]. Early laboratory diagnosis of TB in HIV patients in most resource limited settings remains microscopic examination of sputum smears [21,22]. Since HIV infection reduces the sensitivity of sputum microscopy by lowering the number of AFB in the airway and poor granuloma formation in the lungs [23]. There is still a concern about whether two or three sputum specimens should be examined for diagnosis of TB among HIV patients [24-26]. Eritrea with <1% of the adult population infected with HIV is a low prevalence country. However, the higher HIV prevalence of 11% in TB patients deserves due attention in the early detection of presumptive TB in HIV infected individuals. Our study evaluated the real and actual value of the three sputum specimens in the diagnosis of PTB in HIV patients. In this study the incremental yield of the second and third sputum examination was the same irrespective of the HIV status of patients. TB was diagnosed in 85.6% of HIV positive patients in the first sputum exam and 13.7% in the 2nd sputum (early morning), while the yield in the third sputum was below 1%. A study in Iran that determined the value of third sputum smear for detection of PTB in HIV infected patients also found an incremental yield of only 6.3% in the third sputum [27]. Similar study conducted in Malawi also showed that 97% of HIV infected patients were detected with the first two smears; the diagnostic value of the third sputum was small [24].
Enough time for preparation and reading processed sputum specimen is key in increasing the efficiency and the sensitivity of detecting AFB. In one study the high volume laboratory workload which reduced the quality of results, patients repeated visits to the health center, and the very low average incremental yield of the third specimen, all negated the added value of the third sputum [28]. Furthermore, the frequent visits may discourage patients from completing the diagnosis steps resulting in defaulting or failure to start early treatment. A study conducted in urban Zambia, added to the above demerits that 15% of smear-positive cases dropped out of the diagnostic pathway between submitting specimens and being offered treatment [29].
Limited studies exist on the cost-effectiveness of two versus three sputum examinations; nevertheless, reducing the number of sputum examinations may result in reduced cost for patients and health services. A cost-effectiveness study conducted in Zambia from the health providers’ perspective have shown that the average cost per case detected ranged from 11USD for the third smear to 5USD for the first and 8 USD for the second smear a cost saving of 28% [30]. Another study in Malawi that compared examination of two versus three sputum specimens have shown that examining only two specimens have reduced the number of specimens collected by 29% while it also showed savings of $220 in the cost of laboratory commodities[31].
Therefore, reducing the number of sputum examinations has the potential of reducing the workload, reducing the number of patient visit, and maximizing on the laboratory resources with negligible effect on the yield of sputum and this in turn enhancing the quality assurance program.
Conclusion
In Eritrea, like in other developing countries, serial sputum microscopy has remained the cornerstone for the diagnosis of presumptive PTB. However, this study has indicated that the added value of the third sputum in the diagnosis of presumptive PTB is so minimal that its omission will contribute to reduced laboratory workload, number of patient visits and the cost to the patient and health services. Although, WHO guidelines in limiting the number of sputum examinations are based on the availability of strong External Quality Assurance (EQA) services. The sensitivity and specificity of AFB smear microscopy is on the other hand increased due to the time saved in examining two rather than three sputum specimens in all the presumptive PTB cases.
Acknowledgement
The authors would like to thank Mr. Hagos Ahmed of the National Statistics Office for assisting in statistical analysis; Regional Medical Office and Hospital Directors for facilitating the data collection process.
References
- World Health Organization (2005) WHO report 2005 Global tuberculosis control: surveillance, planning, financing.
- World Health Organization, International Union against Tuberculosis and Lung Disease, Royal Netherlands Tuberculosis Association (2001) Revised international definitions in tuberculosis control. Int J Tuberc Lung Dis 5: 213-215.
- World Health Organization (2003) Treatment of tuberculosis: guide-lines for national programmes. WHO, Geneva.
- Enarson D A, Rieder H L, Arnadottir T, Trébucq A (2000) Management of tuberculosis: a guide for low-income countries. International Union against Tuberculosis and Lung Disease, Paris, France.
- World Health Organization (1998) Laboratory services in tuberculosis control. Parts I–III: Organization and management. WHO, Geneva.
- Parsons LM, Somoskövi A, Gutierrez C, Lee E, Paramasivan CN, et al. (2001) Laboratory diagnosis of tuberculosis in resource- poor countries; challenges and opportunities. Clin Microbiol Rev 24: 314-350.
- World Health Organization (2011) Same-day diagnosis of tuberculosis by microscopy. Policy statement. WHO, Geneva.
- World Health Organization (2007) Proposed reduction of number of smears for the diagnosis of Pulmonary TB: Background document. WHO, Geneva.
- Diagnostic standards and classification of Tuberculosis in Adults and Children (2000) This statement was endorsed by the council of the infectious Diseases Society of America, September 1999. Am J Respir Crit Care Med 161: 1376-1395.
- Kisa O, Albay A (2003) Orhan Balan Leven Doganci; The value of submitting multiple sputum specimens for accurate diagnosis of Pulmonary Tuberculosis. J Microbiol 40: 301-304.
- Yassin MA, Cuevas LE (2003) How many sputum smears are necessary for case finding in pulmonary tuberculosis? Trop Med Int Health 8: 927-932.
- Van DA, Salim AH, Cooreman E, Hossain MA, Rema A, et al. (2002) Optimal tuberculosis case detection by direct sputum smear microscopy: how much better is more?. Int J Tuberc Lung Dis 6: 222-230.
- Gopi PG, Subramani R, Selvakumar N, Santha T, Eusuff SI, et al. (2004) Smear examination of two specimens for diagnosis of pulmonary tuberculosis in Tiruvallur District, South India. Int J Tuberc Lung Dis 8: 824-828.
- Islam MR, Khatun R, Mafij Uddin MD, Khan SR, Rahman T, et al. (2013) Yield of two consecutive sputum specimens for the effective diagnosis of pulmonary tuberculosis. PLoS ONE 8: e67678.
- Hamid S, Hussain SA, Imtiyaz A (2012) Screening tuberculosis suspects: How many sputum specimens are adequate? Ann Trop Med Pub Health 5: 317-320.
- Friden T (2004) Toman’s tuberculosis case detection, treatment and monitoring; questions and answers. World Health Organiziation, Geneva.
- Mase SR, Ramsay A, Ng N, Henry M, Hopewell PC, et al. (2007) Yield of serial sputum specimen examinations in the diagnosis of pulmonary tuberculosis: a systematic review. Int J Tuberc Lung Dis 11: 485-495.
- Chaisson RE, Martinson NA (2008) Tuberculosis in Africa--combating an HIV-driven crisis. N Engl J Med 358: 1089-1092.
- Gebre N, Karlsson U, Jonsson G, Macaden R, Wolde A, et al. (1995) Improved microscopical diagnosis of pulmonary tuberculosis in developing countries. Trans R Soc Trop Med Hyg 89: 191-193.
- Wilkinson D, Sturm AW (1997) Diagnosing tuberculosis in a resource poor setting: the value of sputum concentration. Trans R Soc Trop Med Hyg 91: 420-421.
- American Thoracic Society (2000) Diagnostic standards and classification of tuberculosis in adults and children. Am J Respir Crit Care Med 161: 1376-1395.
- Crampin AC, Floyd S, Mwaungulu F, Black G, Ndhlovu R, et al. (2001) Comparison of two versus three smears in identifying culture-positive tuberculosis patients in a rural African setting with high HIV prevalence. Int J Tuberc Lung Dis 5: 994-999.
- Rieder HL, Chiang CY, Rusen ID (2005) A method to determine the utility of the third diagnostic and the second follow-up sputum smear examinations to diagnose tuberculosis cases and failures. Int J Tuberc Lung Dis 9: 384-391.
- Katamba A, Laticevschi D, Rieder HL (2007) Efficiency of a third serial sputum smear examination in the diagnosis of tuberculosis in Moldova and Uganda. Int J Tuberc Lung Dis 11: 659-664.
- Marjani M, Tabarsi P, Baghaei P, Mansouri D, Masjedi MR, et al. (2012) value of third sputum smear for detection of pulmonary tuberculosis in HIV infected patients. Infect Dis Rep 4: e35.
- Dujardin B, Haelterman E, Van Damme W, Kegels G (1997) The adequacy of one sputum smear for diagnosing pulmonary tuberculosis. Am J Public Health 87: 1234-1235.
- Needham DM, Faussett GP, Foster SD (1998) Barriers to tuberculosis control in urban Zambia: the economic impact and burden on patients prior to diagnosis. Int J Tuberc Lung Dis 2: 811-817.
- Walker D, McNerney R, Mwembo MK, Foster S, Tihon V, et al. (2000) An incremental cost-effectiveness analysis of the first, second and third sputum examination in the diagnosis of pulmonary tuberculosis. Int J Tuberc Lung Dis 4: 246-251.
- Harries AD, Mphasa NB, Mundy C, Banerjee A, Kwanjana JH, et al. (2000) Screening tuberculosis suspects using two sputum smears. Int J Tuberc Lung Dis 4: 36-40.
Citation: Tuumzghi HA, Berhane A, Asrat M (2018) Does the Third Sputum Exam has an Added Value in the Diagnosis of Pulmonary Tuberculosis? J Tuberc Ther 3: 111.
Copyright: © 2018 Tuumzghi HA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 7734
- [From(publication date): 0-2018 - Nov 24, 2025]
- Breakdown by view type
- HTML page views: 6695
- PDF downloads: 1039