Does Smoking Cannabis Increase the Risk of Barrett's Esophagus?
Abstract
A case of 41-year-old African American male is described who was presented to the emergency room of a large academic urban hospital with abdominal pain and exacerbation of nausea and vomiting which he had experienced episodically over the last two years.
Keywords: Cannabis; Barrett’s esophagus; Esophageal metaplasia
Introduction
Cannabis use has been documented for millennia and it is sometimes suggested as a safer alternative to cigarette smoking. Its use is climbing exponentially with the recent legalization of cannabis in many states. Chronic cannabis use may lead to nausea, vomiting, and abdominal pain such as in cyclic vomiting syndrome. Despite the wellknown gastrointestinal side effects of chronic cannabis use, there have been no reported cases of Barrett’s esophagus with chronic cannabis use.
Case Description
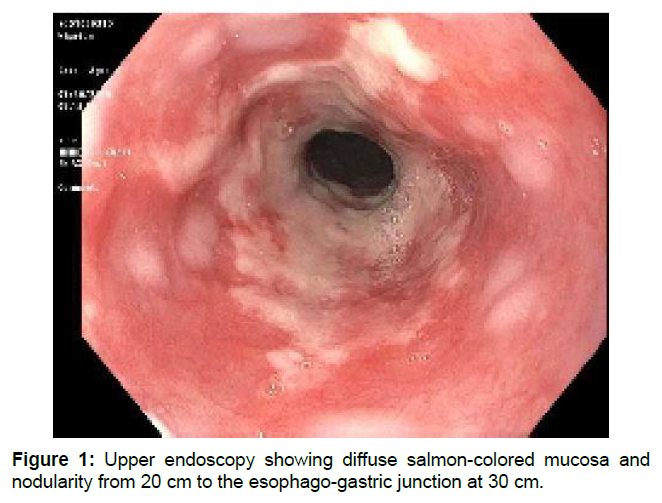
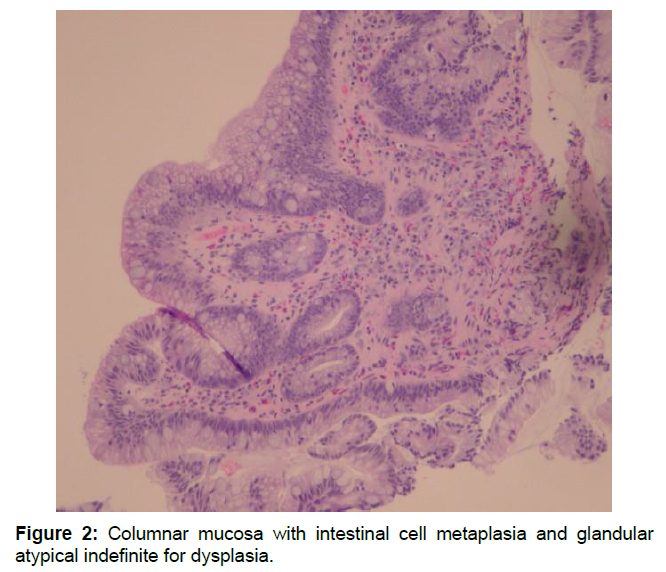
A 41-year-old African American male presented to the emergency room of a large academic urban hospital with abdominal pain and exacerbation of nausea and vomiting which he had experienced episodically over the last two years. Up until this time he was successful in using hot showers to relieve the symptoms. He denied abdominal distention, fever, or constipation. He smoked cannabis two to three times daily over the past twenty years. Vital signs were stable, and his physical exam was unremarkable with a normal body mass index. Contrast-enhanced computed tomography (CT scan) showed a large hiatal hernia with marked thickening of the distal esophagus and gastro esophageal junction. No other abnormalities were noted. Upper endoscopy showed diffuse salmon-colored mucosa and nodularity from 20 cm to the esophago-gastric junction at 30 cm (Figure 1). Histology showed columnar mucosa with intestinal cell metaplasia and glandular atypia indefinite for dysplasia (Figure 2). The patient’s condition improved and he was discharged on a PPI and encouraged to cease cannabis use. He was recommended to have a follow up endoscopy in 3-6 months [1,2].
Cannabis comes from the Cannabis sativa or Cannabis indica plant. Tetrahydrocannabinol (THC) is the primary chemical through which Cannabis exerts its effect. Documentation of Cannabis use dates to Asia circa 500 BC. Ancient cultures used cannabis primarily as an anesthetic and analgesic. Cannabis became a popular recreational drug in the United States in the early 1900s when it was brought over via Mexican immigrants escaping the Mexican revolution. According to the Centers for Disease Control and Prevention (CDC), as of 2015, 22.2 million individuals smoke cannabis every month [3]. Since cannabis use has increased dramatically more research has been devoted to the drug and its adverse reactions. Nausea, vomiting, and cyclic vomiting syndrome are well described complications of chronic cannabis use [4]. There are no case reports in the literature of the habitual use of cannabis and the subsequent diagnosis of Barrett’s esophagus.
The word esophagus is derived from the Greek word oisophagos which means gullet. The root oisein means “to carry” while the word phagein means “to eat.” The esophagus is a fibro muscular tube that enables food to pass from the oral cavity to the stomach. It is normally lined by stratified squamous epithelial cells. Stratified squamous epithelium is found on organs that are exposed to the outside environment, such as the anus and vagina. The stratified squamous epithelium of the esophagus provides protection and stability. An intact layer of stratified squamous epithelium is vital to enable food to travel safely from the oral cavity to the stomach.
Barrett’s esophagus is a disease in which the normal squamous epithelium is replaced by mucus secreting metaplastic columnar epithelium that lines the stomach. A cause of Barrett’s esophagus is gastro esophageal reflux disease (GERD). The constant reflux of acidic juices from the stomach into the esophagus places stress on the normal squamous epithelium of the esophagus. In order to better address the stress caused by the acidic juices, the squamous epithelium undergoes metaplasia to mucus secreting columnar epithelium. Barrett’s esophagus is often asymptomatic and goes unrecognized. Occasionally individuals with Barrett’s esophagus can develop esophageal ulcers and other complications. Approximately, 0.1-3% of individuals with Barrett’s esophagus develops adenocarcinoma.
Screening and early detection of Barrett’s esophagus are vital in preventing the feared complication of esophageal adenocarcinoma. Current screening recommendations focus on individuals with multiple risk factors for adenocarcinoma such as patients who are obese, smoke, or have a family history of Barrett’s esophagus or esophageal adenocarcinoma. If dysplastic Barrett’s esophagus is detected treatment options such a radiofrequency ablation and photodynamic therapy can be used to prevent the progression to adenocarcinoma.
Barrett’s esophagus is most common in Caucasian men over the age of 55. The lowest prevalence of Barrett’s esophagus is in African Americans. The two most common types of Barrett’s esophagus are short and long segment Barrett’s. Short segment involves less than 3 cm of Barrett’s mucosa while long segment involves 4-10 cm of Barrett’s mucosa. Short segment Barrett’s is much more prevalent than long segment Barrett’s. Due to the fact that Barrett’s esophagus most commonly presents in Caucasian men over the age of 55, screening is primarily aimed at this population [5].
Many risk factors have been implicated in the development of Barrett’s esophagus. GERD, obesity, and smoking are some of the well-known risk factors. Cannabis is viewed by our culture as a safer alternative to other drugs. The perceived risk of using Cannabis is at an all-time low, and the prevalence of Cannabis use is at an all-time high [6].
Conclusion
We suggest that chronic cannabis use may be a significant risk factor to the development of Barrett’s esophagus at a younger age and in populations that Barrett’s is not usually prevalent in. Our patient, a young African American male, smoked cannabis regularly for twenty years and presented with extensive long segment Barrett’s esophagus. If cannabis is a contributing factor to the development of Barrett’s esophagus it is important that patients and physicians are aware of this so that it can be screened for and addressed accordingly.
Although, other factors such as GERD could have contributed to the patient’s extensive Barrett’s esophagus, he had no typical reflux symptoms. It is hard to ignore the extensive use of cannabis as a possible contributing aetiology of the disease process. African Americans have a higher prevalence of Cannabis abuse than Caucasians and can thus be more at risk for the development of Barrett’s esophagus from smoking Cannabis. Although Barrett’s esophagus is unusual in African Americans, perhaps endoscopic surveillance needs to be modified in the future for African American patients who chronically use cannabis.
References
- Melamede R (2005) Cannabis and tobacco smoke are not equally carcinogenic. Harm Reduct J 2: 21.
- Pattathan MB, Hejazi RA, Mccallum RW (2012) Association of Marijuana use and cyclic vomiting syndrome. Pharmaceuticals 5: 719-726.
- http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.htm
- Runge TM, Abrams JA, Shaheen NJ (2015) Epidemiology of Barrett's esophagus and esophageal adenocarcinoma. Gastroenterol Clin North Am 44: 203-231
- Qumseya B, Sultan S, Bain P, Jamil L, Jacobson B, et al. (2019) ASGE guideline on screening and surveillance of Barrett’s esophagus. Gastrointestinal Endoscopy 90: 335-359e2.
- Schulenberg J, Johnston L, Omalley P, Bachman J, Miech R, et al. (2019) Monitoring the future national survey results on drug use, 1975-2018: Volume II, College students and adults ages 19-60.
Citation: Levy J, Buhl K, Fernandez C, Kumaraswamy J (2020) Does Smoking Cannabis Increase the Risk of Barrett’s Esophagus?. J Gastrointest Dig Syst 10: 608.
Copyright: © 2020 Levy J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4391
- [From(publication date): 0-2020 - Apr 28, 2025]
- Breakdown by view type
- HTML page views: 3559
- PDF downloads: 832