Distraction Osteogenesis in Implantology for Ridge Augmentation - A Systematic Review
Received: 14-Feb-2017 / Accepted Date: 06-Mar-2017 / Published Date: 31-Mar-2017 DOI: 10.4172/2572-4835.1000119
Abstract
The purpose of this systematic review was to evaluate distraction osteogenesis for ridge augmentation in implant dentistry and also to present the associated advantages and limitations. A Medline and manual search was conducted to identify clinical studies concerning distraction osteogenesis in implant dentistry published between 1998 to 2012. 52 articles were assessed. The articles included evaluated the type of distractor used, augmentation achieved and the success and survival rate of implant placed in the augmented site. It was seen that when comparing methods of regeneration, a decreased treatment time is seen in cases of distraction osteogenesis. The reason for this lies in the fact that within 12 weeks the distraction segments are formed and there is a increase noted in the height of the alveolar bone, from 5 to 15 mm as well as an implant survival rate of 95.7%. It can be concluded that distraction osteogenesis is a relatively simple, effective and reliable technique for alveolar ridge reconstruction in contemporary implant dentistry. It can be considered versatile owing to its simplicity, possibility of avoiding bone grafts, infections and blood transfusions. The fact that graft and membrane exposure or inadequate tissue coverage do not pose complications, makes this an effective method of bone augmentation in implantology
Keywords: Augmentation; Distraction osteogenesis; Implants; Success rate; Survival rate
23939Introduction
The field of implant dentistry is dynamic. A major contraindication to the placement of dental implants is inadequate volume and integrity of bone at the chosen site. In patients who have decreased bone dimensions or bone of inferior quality in the mandible, augmentation bone grafts are essential before the placement of implants. As a result of periodontitis, extractions and trauma of the craniofacial region, sometimes there is atrophy of the alveolar ridge [1]. Placement of implants may be prevented by inadequate bone dimensions unless the deficient areas have bone grafts placed or the inferior alveolar nerve repositioned [2]. In order to correct bone, it is important to carry out autogenous onlay bone grafts, guided bone regeneration, alloplastic augmentation and alveolar split grafting [3-8]. Each of these have their respective pros and cons. Sometimes they do not guarantee the desired bone regeneration, specially in cases of large bone defects and therefore, there is a need for a secondary donor site. There are however some problems associated with this. These include graft rejection as well as donor site morbidity. Nerve repositioning may result in paresthesia from nerve manipulation. Although vast research has been done and documented on the concept of guided bone regeneration, the provision of adequate space for this regeneration seems difficult in cases of such large bone volume [5,6,9]. Unfortunately, none of the above methods provide reliable or predictable results. They all require a greater waiting time between surgeries to increase the ridge and the placement of the implant. Distraction osteogenesis (DO), described by Codivilla, is a biological process that stimulates the formation of new bone following the gradual separation of two bone segments previously joined together [10]. Illizarov carried forward this concept, and is credited with having defined and established the biological bases for the clinical use of osteogenesis distraction in the management of different bone deformities [11-13]. It was Block et al. who employed these principles experimentally following which they were the first to publish studies on the using alveolar distraction osteogenesis (ADO) in animals in 1996 [14]. In cases of ridge deficiencies in the maxillary arches, Chin et al. reported the use of ADO as a treatment option [15].
The ADO is a technique allowing augmentation of alveolar ridge height along with the formation of new bone. It also includes obtaining a significant increase in the surrounding soft tissues, thereby offering a predictable result, with low morbidity and infection rates and a significantly shorter waiting period for rehabilitation with implants (10 weeks) in comparison with the traditionally used methods [16-19]. The widespread use of distraction osteogenesis owes its success to the fact that it is versatile, simple, and there is simultaneous augmentation of the soft tissue with bone, and the possibility of avoiding bone grafts, infections, blood transfusions, and inter-maxillary fixation. It does not carry the unnecessary weight of complications of graft and membrane exposure or inadequate tissue coverage, therefore making the distraction procedure an ideal technique for bone augmentation in implantology.
Materials and Methods
Studies to be included in this structured review had to fulfil the following inclusion criteria:
1. Relevant data on the type of distractor employed.
2. Amount of augmentation achieved.
3. Total Number of implants placed.
4. Radiographic, clinical or histological observations.
5. Associated advantages and limitations.
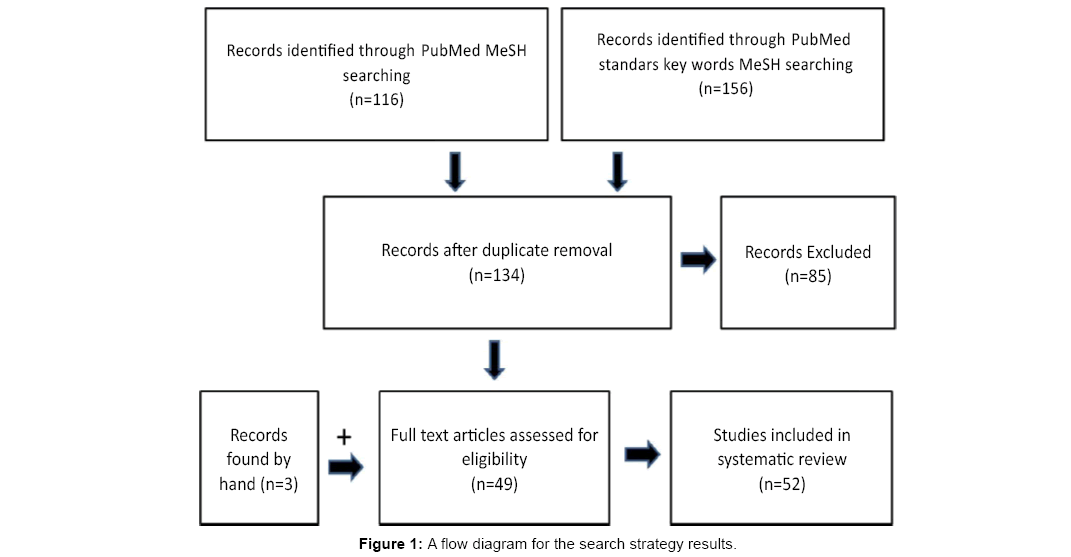
No restrictions were placed concerning the study design. Randomized and non-randomized clinical trials, cohort studies, case control studies and case reports were included in the review (Figure 1). A Medline search was performed to identify clinical articles published between the dates 1998 to 2012. The following search terms were used: distraction osteogenesis and implants, alveolar distractions osteogenesis and implants, alveolar distraction and implants. In addition the manual search of the journals from 1992 to 2012 was performed. The review looks on certain key aspects of distraction osteogenesis in implant dentistry that will be helpful in deciding whether to employ distraction osteogenesis for augmentation of bone before implant placement. Thus, the data obtained from each article (52 articles were reviewed) was divided into 2 (Tables 1 and 2).
| Sr | Author and year | Subjects | Distractor used | Rate of distraction | Regenerative technique | Amount of augmentation achieved | Complications/Failures. |
|---|---|---|---|---|---|---|---|
| 1 | Block et al. [14] | 4 heartworm-free mongrel dogs- their left mandibular premolars and first molars extracted | 4, 8-mm-long, 3.25-mm-diameter hydroxyapatite- coated cylindrical implants (Sulzer Calicitek, Carlsbad, CA) horizontally placed through the buccal cortex, engaging the lingual cortex. | After 7 days, the mandible was distracted superiorly 0.5 mm twice a day for 10 consecutive days. | Significant difference for the labial cortex bone thickness between distracted (mean=1637.3 μm) and nondistracted bone (mean=911.8 μm). | ||
| 2 | Oda et al. [37] | 6 adult mongrel dogs. | Distraction device consisted of a distraction screw and a supporting plate | Latency period of 7 days-distraction achieved at a rate of 1.0 mm/day | Vertical augmentation averaged 6.83 ± 0.21 mm and 6.10 ± 0.53 mm after a 12-week consolidation period | ||
| 3 | Nosaka et al. [34] | 4 adult male mongrel dogs | A lengthening apparatus (Orthofix, M-100, Verona, Italy) connected to the pins | After a 7 day latency distraction at the rate of 1 mm/day for 14 consecutive days. | |||
| 4 | Gaggl et al. [49] | 35 patients with alveolar ridge deficiency | Distraction implants (SIS Trade Systems, Klagenfurt, Austria) | The distraction was carried out at a rate of 0.25 (atrophy) to 0.5 mm (defects) per day. It was continued for 8 to 24 days | Guided bone regeneration was used for bone augmentation in the 1 patient. | An increase of 4 to 6 mm in alveolar ridge height. | 2 distraction implants were lost. In 2 patients ankylosis of the distraction segment. In 1 patient the alveolar ridge was overcorrected, and another patient experienced a persisting hypoesthesia of the lip. 1 patient experienced loosening of 1 distraction implant. 1 patient required removal of the distraction implant. |
| 5 | Watzek et al. [18] | 6 patients | Multi-dimensional distraction system- distraction abutment | The greatest movements of the implant bone block measured was approximately 11 mm in the vertical direction, 4 mm in the palatal direction, and 3 mm in the buccal direction. | |||
| 6 | Chiapasco et al. [20] | 8 patients who presented with vertically deficient edentulous ridges | Intraoral alveolar distractor (Gebruder Martin GmbH, Tuttlingen, Germany). | After a waiting period of 7 days A distraction of 1 mm per day (subdivided into 2 activations of 0.5 mm every 12 hours) | Mean vertical bone gain of 8.5 mm | ||
| 7 | Mcallister [24] | 10 patients with the need for vertical augmentation of 3 mm or greater | An Endosseous distractor (ACE) | At the rate of 1 mm/day by clockwise turning of the axial distraction screw 2.5 revolutions with the 0.88 mm hex driver. | Small consolidation defects were observed and grafted with anorganic bovine bone | The average vertical distraction obtained was 7 mm with a range of 5 to 9 mm | 1 case of base plug settling and 2 cases with small areas of incomplete bone consolidation. |
| 8 | Nosaka et al. [50] | 6 beagle dogs Group 1-control, group 2 – DO sacrificed after 12 weeks of placement of implants and group 3- after 24 weeks. | An originally deviced lenghthening instrument. | After a latency period of 7 days distraction commenced at the rate of 1 mm/day for 5 consecutive days | |||
| 9 | Gaggl et al. [51] | 7 patients with severe periodontitis. | 11 distraction implants were placed. 4 patients having two and 3 patients one implant. | At the rate of 0.125 mm four times a day (a total of 0.5 mm daily). | |||
| 10 | Garcia, et al. [27] | 5 patients | Lead System distractor | Distraction was commenced 7 days later at a rate of 0.5 mm every 12 hours for 5 days | Defects Complications in 4 case-. Treatment was bone regeneration using Bio-Oss and Bio-Gide reabsorbable membranes. | Fracture of the Transport Segment occurred in 1 case, Incorrect Direction of Distraction, due to lingual deviation of the threaded rod.. Perforation of the Mucosa by the Transport Segment occurred twice, Suture Dehiscence occurred in 1 case. Bone Formation Defects arose in 4 cases | |
| 11 | Jensen et al. [23] | 25-anterior maxillary defects-at least 4 mm of vertical bone loss | Bidirectional orthodontic approach. When an orthodontic approach was not taken, a distraction implant 3.5 mm in diameter and 5 or 7 mm in length | Vertically 1 mm, 3 times per week for about 2 weeks using a cinch wire technique | Secondary bone grafting was required in 18 patients. Gingival augmentation procedures were done in 12 cases. | Mean distraction of 6.5 mm | 11 patients had anteriorization of the distracted segment. Relapse of the segment occurred in 14 segments. |
| 12 | Raghoebare et al. [31] | 10 patients suffering from reduced stability and insufficient retention of their mandibular denture | The Groningen Distraction Device (GDD, Martin Medizin Technik, Tuttlingen, Germany) | 5 days after, distraction is started (1 mm/day). The screws are rotated two revolutions per day. | |||
| 13 | Zaffe et al. [32] | 5 dentulous and 5 edentulous with varying degrees of mandibular alveolar ridge defect | Distraction device (Martin, Tuttlingen, Germany) | At the rate of (0.5 mm, twice a day. 4 weeks’ rest from distraction (3rd latency period) | alveolar ridge improvement of 10–15 mm with a mean of 12 mm. | Vestibuloplasty was necessary in all three patients to restore the depth of the buccal vestibule. In one patient lingual reversion of the osteotomized segment. | |
| 14 | Feichtinger et al. [52] | 35 patients | 62 distraction implants (The DISSIS distraction implant (SIS Trade Systems) | The distraction was carried out at a rate of 0.25 mm (alveolar ridge atrophy) to 0.5 mm (alveolar ridge defect) per day | Distraction was continued for 8 to 24 days to achieve an increase in the alveolar ridge height of 4 to 6 mm. | 2 patients with severe defects of the alveolar ridge had premature reunion of the fragments. In one patient, an overcorrection occurred. 2 distraction implants did not osseointegrate and had to be removed | |
| 15 | Garcia Garcia et al. [21] | 7 patients with unilateral or bilateral partial edentulism in the posterior mandible. | Lead System distractors | Distraction at a rate of 0.5 mm every 12 hours for 5 days, | The mean ratio of crown height to length of implant after distraction was 0.7 | ||
| 16 | Chiapasco et al. [29] | 21 patients with vertical alveolar ridge defects | Group 2 patients (10 patients) were treated by means of alveolar DO with an intraoral extraosseous distraction device (Gebrtider Martin GmbH & Co., KG, Nittlingen, Germany) | A distraction of 1 mm per day [subdivided into two activations of 0.5 mm every 12 h| was performed | Group 1 patients (11 patients) were treated by means of vertical GBR with e-PTFE titanium reinforced barrier and particulated autogenous bone taken from intraoral sites (chin and/or ramus of the mandible). | Distraction was performed until the desired amount of distraction was obtained (range: 4-9 mm). | |
| 17 | Chiapasco et al. [22] | 37 patients | Intraoral extraosseous distraction device (Track 1 or Track 1.5; Gebrüder Martin,) | A distraction of 1 mm per day (subdivided in 2 activations of 0.5 mm every 12 hours) was performed until the desired amount of distraction (4 to 15 mm) was obtained. | The mean bone gain was 9.9 mm (range 4 to 15 mm). | In 3 patients, a progressive lingual inclination of the distracted segment. In 2 patients a progressive palatal inclination of the distracted segment occurred. A patient presented with a mandibular fracture 4 weeks after the completion of distraction, and one with incomplete distraction (3 mm instead of the planned 6 mm). | |
| 18 | García García et al. [45] | 12 patients, mean age 42.6 years; underwent a total of 17 alveolar ridge distractions | Lead System distractor (Leibinger, Kalamazoo) | 1 week after implant placement, distraction commenced at 1 mm/day for mandible and 0.5 mm/day for maxilla. | Subcategory D consisted of lingual deviation of the distraction axis, | ||
| 19 | Rachmeil et al. [53] | Ten 1 year old sheep divided into two groups of five each. group 1 alveolar distraction alone was performed and in group 2 rhBMP-2 was injected locally during alveolar distraction | 1.5 mm alveolar distraction device was adapted to the lateral surface of the bone and fixed by 1.5 mm titanium screws. | After latency period of 5 days gradual distraction of 0.5 mm per day was performed on all animals by turning the device in the submandibular area | On the 5th day of distraction a single dose of 10 ug of rhBMP-2 in phosphate buffered saline containing 0.1% bovine serum albumin in 1 ml was injected slowly through the catheter directly to the distraction site in group 2. | 12 mm of alveolar augmentation was achieved in all 10 sheep. | |
| 20 | Enislidis et al. [54] | 9 edentulous women with severely atrophic mandibles | Distraction was started at a rate of 3 mm × 0.3 mm a day (a daily distraction of 0.9 mm). | Severe tilting of the transport segment. Fracture of the basal bone, fracture of the transport segment, breakage of the distractor, ptotic chin, defective formation of bone, immature bone at time of removal of the distractor, infection, reverse activation of the distraction device and dehiscence of the soft tissue. | |||
| 21 | Enislidis et al. [25] | 37 partially edentulous patients. 45 edentulous segments. Six segments were localized in the anterior mandible (incisor/canine region) and 39 segments in the posterior mandible (premolar/molar region). | 14 intraosseous devices (LEAD System; Stryker Leibinger, Kalamazoo, Mich) were used for short-span segments (for 1-2 implants), and 31 subperiosteal devices (Track Distractor 1.0 mm or Track Distractor 1.5 mm; Gebrueder Martin, Tuttlingen, Germany) | After a latency period of approximately 1 week following surgery, bone distraction was started at a daily rate of 0.9 mm (3 activations of 0.3 mm) | Secondary grafting procedures were performed in 11 of 45 distraction sites: | Average gain of 8.2 mm (range 5-15 mm) in alveolar bone height | Major complications were recorded in 21.6% of patients more frequently in the intraosseous distraction group and in the posterior site. Breakage of distractor required removal. Severe mechanical problems lead to preterm distractor removal and abortion of treatment in 2 cases and rescue operation for reinsertion of a disengaged distractor part in 1 case. 5 patients suffered from temporary postoperative hypoesthesia in 6 locations; 1 with fracture of basal bone. |
| 22 | Kunkel et al. [55] | 10 patients, box shaped or segmental resection of the mandible. Uneventful oncologic follow up of 26 months. | Mainz distractor. | After latency period of 4- 5 days transport rate was 0.5-1 mm/day. | Vertical gain of 7.3 mm | Loosening of one distractor. | |
| 23 | Laster et al. [56] | 9 patients with moderately deficient alveolar bone in the horizontal dimension | The Laster Crest Widener distraction device. | Distraction begins 1 week later by turning the activating screw 2 and 1/2 turns per day (0.4 mm) | |||
| 24 | Gaggl et al. [57] | In 6 patients with severe atrophy of the edentulous maxilla a sinus lift operation and placement of dental implants were carried out in the posterior maxilla. | Callus spreader (SIS-Trade Inc, Klagenfurt, Austria), In the anterior part of the maxilla a segmental split osteotomy and placement of two miniplate distractors were performed | 1 week after sinus lift distraction was started at the rate of 0.25 mm/day for 18-22 days | |||
| 25 | Perry et al. [38] | 5 adult American foxhounds | Distraction device designed to promote vertical distraction of 10 mm. | After latency period of 7 days, activation of the devices at the rate of 0.5 mm/twice a day for 10 days by turning the bone screw 1.5 times in a clockwise direction. | Autogenous onlay graft measuring 45 mm long, 10 mm high and 8 mm wide harvested from right iliac crest. | In 1 of the dog, the distraction segment appeared fenestrated | |
| 26 | Saulacic et al. [41] | 11 Patients presented with 15 mandibular and 2 maxillary vertical alveolar ridge defects. | Intraosseous distractor (LEAD; Leibinger, Kalamazoo, MI) | The mean of bone augmentation was 6.08 ± 1.82 mm at mesial points and 6.18 ± 1.90 mm at distal points of measurement. Following a period of consolidation. The mean of alveolar bone augmentaton was 4.34 ± 2.38 mm at mesial points and 4.40 ± 2.23 mm at distal points of measurement. | The mean of relapse during the consolidation period on mesial and distal aspect of implants was 1.57 ± 1.82 mm and 1.79 ± 1.68 mm, respectively. Cases with minor amount of distraction (<6 mm) showed major variety in relapse. | ||
| 27 | Chiapasco et al. [35] | 2-year period 7 patients with vertical alveolar ridge mandibular defects, | Intra-oral extra-osseous distraction device (Track 1.5 s, Gebru¨ der Martin GmbH & Co. KG, Tuttlingen, Germany). | 2 patients showed a progressive lingual inclination of the distracted segment. | |||
| 28 | Watzak et al. [58] | Upper and lower alveolar crests of seven patients with resorption class IV according to Cawood and Howell. | Titanium screws (1.2 mm+; Leibingers, Freiburg, Germany were the distraction devices | After a 1-week latency period, the screws were reset daily for horizontal expansion by 0.5 mm during the distraction period. | The overall gain of bone width was 2.77 mm after DO. Gain of bone area amounted to 34.01 mm | ||
| 29 | Chiapasco et al. [59] | Group 2 patients (nine patients) | Alveolar DO with an intraoral extraosseous distraction device (Gebru¨ der Martin GmbH & Co. KG, Tuttlingen, Germany). | A distraction of 1 mm per day (subdivided into two activations of 0.5 mm every 12 h) | Group 1 patients (8 patients) were treated by means of vertical onlay bone grafts harvested from the mandibular ramus | The mean bone gain after the grafting procedure was 4.6 mm and after distraction The mean vertical gain obtained was 5.3 mm | In two patients a progressive lingual inclination of the distracted segment occurred during distraction. In one patient, distraction was interrupted before completion, due to the impossibility of the distracted segment to be moved further |
| 30 | Marchetti et al. [60] | 10 patients with anterior maxillary (two patients) or mandibular (eight patients) vertical defects. | Gebru¨der Martin, Tuttlingen, Germany distraction device was used. | the distraction device was activated (0.5 mm, twice a day) until the required height was reached | In 1 patient with distraction of the mandible, it was necessary to perform an autologous onlay block Ramus graft. | Average gain of 10.9 –1.10 mm | The morphology of the mandibular buccal vestibule was inadequate in one edentulous patient, |
| 31 | Polo et al. [39] | 10 partially edentulous female patients | Not specified | Not specified | 1.5 mm to 5.8 mm | ||
| 32 | Saulacic et al. [61] | Patients who underwent distraction osteogenesis between 2000 and 2003-17 DO 15 mandibular, 2 maxillary in 12 patients. | Lead System | Latency period of 7 days and distraction rate of 0.5 mm/12 h. | In the case of bone defect formation, the treatment of choice was augmentation with bovine bone (Bio-Oss) and a collagen membrane (Bio-Gide). | The amount of augmentation performed for all 22 implants placed without bone defect formation was between 4.5 and 6.5 mm. 23.30% ± 4.18% for the no defect group and 36.61% ± 8.59% for the defect group. | |
| 33 | Schleier et al. [62] | 21 patients, unilateral, bilateral, or total edentulism in the mandible or maxilla in combination | 10 unidirectional, 11 bidirectional. | Rate of distraction was 0.25 mm/1/day to 0.25 mm/4/day. | 6 autogenous grafts following removal of the unilateral distractor, 2 cases after the use of the bidirectional distractor. bone harvested from chin or ramus region of the mandible or anterior nasal spine in the maxilla. | Mean bone gain resulting from the use a unidirectional distractor system was 5.3 ± 1.8 mm; the mean bone gain with use of a bidirectional distractor system was where 6.1 ± 2.3 mm | |
| 34 | Gonzalez-Garcia et al. [63] | The Piezosurgery System the piezoelectric handpiece with functional vibration frequency ranging from 25 to 30 kHz | Distraction is started 7 days later at a rate of 0.5 mm every 12 hours until the required height has been reached | ||||
| 35 | Perdijk et al. [48] | 45 patients suffering from atrophied edentulous mandibles, with a vertical height varying between 7.3 and 15.8 mm | Mondeal submucosal vertical distraction device (Mondeal Medical Systems GmBh, Tuttlingen, Germany) | After a latency period of 1 week patients activated at the rate of 0.5 mm/day | Early fractures (2%), late fractures (17%), bleeding or haematoma (4%), infections (6%), skin perforation (2%), mucosal dehiscence (8%), sensory disturbances (28%), sagging chin (13%). All patients showed a lingually oriented rotation of the upper bone segment. | ||
| 36 | Wolvius et al. [42] | 20 patients underwent vertical DO. anterior mandible (4), posterior mandible (4), anterior maxilla (10) and posterior maxilla (2) | Extraosseous subperiosteal evice (Track distractor 1 mm or 1.5 mm, Gebruder Martin, Germany) | Latency period of 1 week-distraction at the rate of 0.9 mm (3 activations of 0.3 mm daily | Mean alveolar distraction was 6.5 mm at the mesial point and 6.1 mm at the distal point. Mean augmentation mesial-5.3 mm (relapse-1.2 mm) and distally – 4.6 mm (relapse – 1.5 mm) | The mean relapse at the mesial point was 20% and at the distal point 17%. The intraoperative and postoperative problems encountered were fracture (1) and lingual (4) and palatal (6) displacement of the transport segment. Overall complication rate was 55%. | |
| 37 | Kanno et al. [47] | 35 patients underwent 38 procedures. 3 patients both maxilla and mandible, group A - healthy sites no surgery within 6 months, Group B - surgery in the past 6 months, | Track type distractor (KLS Martin) | After a latency period of 10 days, distraction started at the average rate of 0.4 mm (0.3 mm for track 1 and 0.5 mm for track 1.5) every 12 hrs. | The mean distraction was 9.7 mm. group A-9.9 mm, group B-9.5 mm | Although the 20 sites with a healthy alveolus had bone reductions of 1.5 and 2.5 mm (15 and 25%) the 18 sites group B at which alveolar DO had much greater bone loss of 2.7 and 4.8 mm (28 and 50%) respectively. | |
| 38 | Froum et al. [26] | 30 patients | 17 intraosseous devices (IDs) (Lead Stryker, Leibinger) and 13 extraosseous devices (EDs) (Track Plus System, KLS Martin) | At a rate of 0.4 to 1.2 mm per day. A 0.4-mm or 0.6-mm distraction rate was used for the first 3 days, followed by a rate of 1.2 mm per day | Additional hard tissue augmentation using GBR or block grafts was required in 18 of the 30 patients | Vertical augmentation in the 30 patients ranged from 3.5 to 13.0 mm (average, 7.8 mm) | Failure to achieve the desired buccal augmentation occurred in 22 of 30 cases. In 8 of 30 cases, a less-than-ideal esthetic result was reported. |
| 39 | González-García [64] | 17 Patients alveolar distraction osteogenesis for rehabilitation of edentulous mandibular regions. | A semirigid intraosseous distractor (LEAD System; Leibinger, Kalamazoo, MI).11 conventional osteotomy group, 6 Piezosurgery | Distraction commenced 7 days after surgery and proceeded at 0.5 mm every 12 hours, until the required height had been achieved. | Dysesthesia of the mental nerve in 35.3% of cases. Exposure of the transport segment due to perforation of the mucosa was observed in 58.8% of cases. Deviation of the direction of distraction was observed in 17.6% of cases. | ||
| 40 | Kanno et al. [65] | 9 patients. | Bidirectional distraction device. extraosseous | 1 turn-0.25 mm/24 hrs. after 1 week 1 turn/12 hrs. Active distraction duration-3-4 weeks. 3 months. (0.5 mm/day) after 10 mm achieved-labiobuccal 10 degrees/day. | Vertically – 5.8 mm and horizontal labial buccal augmentation-11.2 degrees. | In 4 cases slight bone deficits on the anterior buccolabial surface. | |
| 41 | Ragheobar et al. [33] | 46 patients with severe resorption of the anterior mandible symphyseal area mean height 6 mm | Groningen distraction device, intraoral device. | 1 mm/day, distraction beginning 5 days after placement of distractor. | Both the height after distraction in the midline and 3 mm distal of the implants were 13.3 ± 0.7 mm (range, 12 to 14 mm | In the midline there was a diminishment in height of 10.2% ± 0.8% and to the distal of the implants there was a diminishment in height of 9.8% ± 0.6%. 1 case of wound dehiscence. One mandibular fracture. 4 patients slight sensory disturbance in distracted region. | |
| 42 | Robiony et al. [30] | 12 patients, partially or a completely edentulous mandible. | Intraoral extraosseous distractor. A traditional or a bidirectional device. | After latency phase of 15 days activated at the rate of 0.5 mm/day. | Platelet rich plasma. | Average distraction achieved-7.4 mm. In 11 patients achieved. | 1 patient - fibrotic scarring. |
| Superior iliac crest bone graft. | 1 bone fracture at the inferior mandibular rim. 2 cases-lingual inclination. 1 case-fracture of the distracted segment. Exposure of the transport plate of the distractor. | ||||||
| 43 | Perez-Sayans et al. [66] | 9 patients had undergone alveolar DO, 14 – 12 mandibular, 2 maxillary. | Semirigid intraosseous distractor (LEAD system, Stryker Leibinger, Freiburg, Germany) | After a latency period of 7 days distraction commenced at the rate of 1 mm/day in the maxilla and 0.5 mm/12 hrs in the mandible | |||
| 44 | Zhao et al. [67] | 6 adult mongrel dogs. All mandibular premolars were extracted, and an alveoloplasty was performed to simulate an atrophic ridge. | A new DI system with the dual functions of distractor and prosthetic implant and was tested in this experiment,(Fourth Military Medical University, Shaanxi, China) | Distraction was carried out at a rate of 1 mm per day for 8 consecutive days. | Augmentation averaged 6.92 ± 1.00 mm. Radiographically 7.25 ± 0.40 mm. | ||
| 45 | Bilbao et al. [36] | 20 healthy, non-smoker female patients with The mean age 48.6 ± 9.9 years. | Extraosseous device (Track-Plus; KLS/Martin, Jacksonville, FL, USA) | The rate of distraction – was 0.9 mm/day of 3 movements of 0.3 mm/day | |||
| 46 | Elo et al. [28] | Retrospectively 82 patients requiring alveolar augmentation prior to implant placement were evaluated. | 17 patients underwent distraction osteogenesis prior to implant placement. | No specific distractor and the rates of distraction. | 65 patients (anterior iliac crest: 44; retromolar: 17; tibia: 2; chin: 2), | ||
| 47 | Ettl et al. [46] | 30 partially edentulous patients | 36 extra-osseous distractors (Track® Distractor 1.0 or 1.5 mm, Martin, Tuttlingen, Germany). Eleven devices were inserted in the maxilla and 25 in the mandible. | After a mean latency period of 8.1 days (range 6–13 days), the distractors were activated with a transport of 0.9 mm/day (three activations of 0.3 mm for track distractor 1.0 mm) or 1 mm/day (two activations of 0.5 mm for track distractor 1.5 mm). | Mean length of the distracted segment was 19 mm. The average vertical augmentation immediately after distraction was 8.1 mm. In the maxilla, bone gain measured a mean of 7.9 mm, in the mandible 8.2 mm. | A total of 33 complications. In 15 cases displacement of the transport segment occurred. In 13 cases, extension of the fixed gingiva was missing resulting in inadequate morphology of the buccal vestibule. In 2 patients, device failure—plate and rod fracture. 2 soft tissue dehiscences occurred without infection. In 1 case, fracture of the mandible appeared | |
| 48 | Funaki et al. [68] | 5 beagle dogs | Horizontal DO device (Alveo-Wider, okada Medical supply, Tokyo, japaan) | After a latency period of 7 days distraction commenced at a rate of 0.4 mm/day for 10 days. | Bone splitting (BS) method with a bone graft combined with simultaneous implant placement. | The average amount of bone gain on the DO side (2.7 mm) was significantly greater than that on the BS side (1.7 mm). The keratinized soft tissue gain on the DO side (2.8 mm) was significantly greater than that on the BS side (0.6 mm). | On the DO side decubitus ulcers of the buccal mucosa developed during the distraction period |
| 49 | Xie et al. [69] | 12 adult mongrel canines | Ti-Ni-SMA distractors | 7.5 to 11.5 mm of augmentation was reached after 3 to 5 days of device activation | |||
| 50 | Kanno et al. [44] | 25 maxillary sinus sites in 17 systemically healthy patients | An alveolar distractor (KLS Martin, Tuttlingen, Germany; Medartis AG, Basel, Switzerland) | Following a latent period of 3 weeks, patient self distraction was started at a slow rate of one turn (0.5 mm) per day. Next, the activation rate was accelerated to two turns (1.0 mm) per day, considering the soft tissue condition. | The average alveolar bone height augmented for implant placement was 13.7 mm for bilateral cases. 12.9 mm for unilateral cases. | ||
| 51 | Yamauchi et al. [43] | 13 sites in 12 patients who presented with severe horizontal atrophy (Atwood class IV) of a partially edentulous maxilla or mandible | The horizontal distraction device consisted of a 0.3-mm-wide commercially pure (CP) titanium mesh plate and a pure titanium distraction screw 2 mm in diameter and 12 mm in length (Alveo-Wider®, Okada Medical Instrument Supply, Tokyo, Japan). | 0.4 mm with one turn; the driver distraction rate is typically 0.4–0.8 mm/day | In 3 cases a minor bone graft with or without resorbable membrane (BioGide®, Geistlich, Wolhusen, Switzerland) was applied at implant insertion | The median of actual gain in bone width at the end of the consolidation period was 3.6 mm | In 3 cases, there was minor bone loss in the crestal region, In 1 case, inadequate fracture of the transport segment occurred. In 2 cases, dehiscence at the edge of the crestal region. In 3 cases, partial exposure of the titanium mesh. |
| 52 | Chenping et al. [70] | 10 patients | Fibular flap and custom made distractor (DID) (Yinghao Timing, Shanghai, China) | After a 7 day latency period distraction begun at the rate of 0.7 mm/day | The mean vertical bone height attained with the DID device was 11.4 mm. | 2 DID devices loosened. 9/10 patients-satisfied with their facial asymmetry, the one who was not had 2 DIDs during the follow up period. |
Table 1: Demographic data and type of distraction device used and related clinical parameters observed.
| Sr | Author | Type and number of implants/implant system. | Immediate or delayed loading | Duration | Radiographic/histologic finding/clinical finding | Failures | Survival/success rate |
|---|---|---|---|---|---|---|---|
| 1 | Block et al. [14] | Two 16-mm dental implants (Mark II, Nobel Biocare USA, Westmont, IL) | 4 months | The vertical distance between the implants, as measured from the centre of the abutments averaged 9.05 ± 1.01 mm after the initial 10 days of distraction, and 8.85 ± 1.05 mm after 10 weeks of healing. From 6 to 10 weeks, and until sacrifice at 12 months after loading, the radiographic density of the bone between the distracted segment and the remaining corpus of the mandible increased. Histologically the cortices were intact and continuous across the distraction gap. | |||
| 2 | Oda et al. [37] | 12 implants | Greater integration between the implant and the distracted segment-12 weeks after distraction than at 8 weeks. Bone-implant contact within the distracted bone averaged 15.7 ± 17.8% and 30.2 ± 19.1%, and bone area within the distracted bone averaged 39.3 ± 24.8% and 56.9 ± 30.5% at 8 weeks and 12 weeks, respectively. | 6 cover screws became exposed in the oral cavity. | |||
| 3 | Nosaka et al. [34] | Screw-type implants (Astra Tech AB, Mölndal, Sweden; 8 mm in length and 3.5 mm in Diameter. | 3 weeks after the completion of distraction | 12 weeks after implants placement, the distracted site had converted completely into new bone. On axial radiographs taken at 24 weeks the left side of the mandible was clearly elongated. In high-magnification photomicrographs, active osteoblasts could be seen on the surface of the woven bone. Microscopic examination of Villanueva-stained sections revealed newly formed mature lamellar bone around the implant. Direct bone contact with the implant surface could be seen | |||
| 4 | Gaggl et al. [49] | The distraction implants were loaded by prosthetic superstructures 4 to 6 months after distraction | For 5% of the implants, pathologic probing depth of more than 3 mm and sulcus bleeding were registered prior to prosthetic treatment. These observations decreased during the next 9 months. Periotest values were normal before the start of prosthetic treatment. There was a decrease in the Periotest values, thus an increase in implant stability, during the following 9 months | ||||
| 5 | Watzek et al [18] | 11 Nobel Biocare, Göteborg, Sweden, regular platform, length 10 to 15 mm). | 8 weeks | 7 months | Computed tomograms obtained pre- and postoperatively showed consistent ossification of the osteotomized and distracted areas | ||
| 6 | Chiapasco et al. [20] | 4 patients received 15 Brånemark System implants (Nobel Biocare, Göteborg, Sweden), and 4 patients received 11 screw-type ITI implants (Straumann, Waldenburg, Switzerland). | 4 to 6 months later, abutments were connected to the implants, and prosthetic treatment was started. | 14 months | Radiographic examinations 12 months after functional loading of implants showed a significant increase in the density of the newly generated bone in the distracted areas. The mean bone resorption was 1.3 ± 0.3 mm | Cumulative success rate 100%. | |
| 7 | Mcallister [24] | 16 implants | Implant placement was performed immediately at the time of distractor and base plug removal in 3 cases. In the remaining 4 cases, a delayed approach for implant placement was employed. | 13 to 30 months | All cases showed radiographic evidence of new bone formation in the coronal direction from the apical host bone and in an apical direction from the transport segment in the regeneration zone | ||
| 8 | Nosaka et al. [50] | Astra Tech AB, Molndal, Sweden, 8 mm length, 3.5 mm diameter | 12 days after bony consolidation. | 12 weeks after the placement of implants, thin lamellar bone rose horizontally from the transport segment towards the surface of the implant. Twenty-four weeks after their placement, the implants were fully embedded in mature lamellar bone, and direct bone contact with the implant surface could be seen. | |||
| 9 | Gaggl et al. [51] | After a radiographic estimate of the success of distraction the distraction insert was exchanged for the permanent implant head. In 2 patients a further conventional implant was inserted after a delay of 4-6 weeks. The distraction implants and conventional implants were allowed to heal for 4 months before prosthetic treatment started | The mean peri-implant probing depth was 1.8 mm before start of the prosthetic treatment and decreased to 1.2 mm 12 months after implant loading. | ||||
| 10 | Garcia Garcia, et al. [27] | (8 ITI _ 4.1 mm, 12.0 mm PLUS; Straumann, Waldenburg, Switzerland and 4 Frialoc D4/L13; Friadent, Mannheim, Germany). | After 12 weeks, the distractor was removed, and the implants were placed. At 14 weeks after implant placement, the prosthetic restoration was commenced and subjected to load. | All 7 distractions were followed by the placement of 2 implants. The restoration was ideal in 4 of the 7 cases and functional but not ideal in the remaining 3. | |||
| 11 | Jensen et al. [23] | 84 Conventional, 4-mm-wide 1-stage implant (3 i Osteotite, Implant Innovations, West Palm Beach, FL) | After 2 months implants placed and After 6 months restoration. | 18 months | The implants maintained stable bone levels and remained well integrated with stable gingival esthetics (1 mm or less gingival recession | 8 implants failed to integrate (9.6%), all of which were lost prior to restoration. | |
| 12 | Raghoebare et al. [31] | ITI Bonefit implantsA (Straumann AG, Waldenburg, Switzerland) (nΩ6 patients, 12 implants), Brånemark implantsA (Nobel Biocare AB, Gothenburg, Sweden) (nΩ4 patients, 8 implants). The length of the implants used was 12 mm (nΩ8), 13 mm (nΩ8), and 14 mm (nΩ4). | 2 months after the last day of distraction implants were placed and 12 weeks after implantation, the prosthetic treatment was started | Light microscopic evaluation of all specimens confirmed the radiographic assumption that new bone had formed in the distraction gap | 1 ITI implant was lost - wound dehiscence had occurred | ||
| 13 | Zaffe et al. [32] | Submerged implant (3i OsseotiteA, Implant System, Implant Innovations, Palm Beach Gdns, FL, USA) | Implant uncovering and prosthetic rehabilitation was done after 4 months | Histological results show a regression in bone deposition processes 8 days after the end of distraction culminating in a virtual steady-state after a certain time. The results suggest that early implant insertion may be desirable to avoid bone loss due to mechanical unloading. | |||
| 14 | Feichtinger et al. [52] | 62 implants | After the planned distraction height was achieved, the distraction insert was replaced by the definitive implant insert. The distraction implants were loaded with prosthetic superstructures 4 to 6 months after distraction. | 9 months | Radiologic evaluation showed a mean periimplant bone resorption of 0.3 mm at 3 months after distraction, 0.4 mm at 6 months after distraction, and 0.4 mm at 9 months after distraction. | ||
| 15 | Garcia Garcia et al. [21] | 16 International Team for Implantology Straumann, Switzerland, and 4 Frialoc, Friadent, Germany | 3 months to ensure bony consolidation, then removed to allow insertion of implants. The prothesis was constructed 3 months after implantation | 6 months - 2 years | Before distraction, the mean (SD) predicted crown height was 12.8 (2.1) mm; mean bone height available for implantation was 7.8 (1.5) mm. After distraction and insertion of implants, mean crown height was 8.1 mm, and mean implant length was 11.3 mm. Before distraction, the mean required crown height:available bone height ratio was 1.7; after distraction and insertion of implants, the mean crown:implant ratio was 0.7. | ||
| 16 | Chiapasco et al. [29] | Titanium screw-shaped endosseous implants were placed in the distracted segments (eight patients received 28 Branemark system implants and two patients received six screw-type ITI implants). | After 2-3 months of consolidation implants were placed. After to 3-6 months, abutments were connected to tbe implants | 31 months | The mean peri-implant bone resorption between implant placement and abutment connection, between abutment connection and 1-3 years after the start of prosthetic loading were 0.50 mm, 1.13 mm, 1.24 mm, and 1.41 mm respectively. | ||
| 17 | Chiapasco et al. [22] | 138 10 mm length titanium screw-type endosseous implants | 2-3 months after consolidation implants were placed and 3-6 months later abutments were placed. | 4 years | Mean peri-implant bone resorption was 0.8 mm 1 year after prosthetic loading, 1.1 mm after 2 years, 1.2 mm after 3 years, and 1.4 after 4 years. | 8 implants presented peri-implant bone resorption values higher than those proposed by Albrektsson and associates’ criteria. | 100% and 94.2% |
| 18 | García García et al. [45] | 37ITI, Straumann, Waldenburg, Switzerland, 6 Frialoc implants, Friadent, Mannhein, Germany, 1 Frialit-2 implant, Friadent. | After 3 months for consolidation implants placed and later after 3 months prosthesis. | 1 year | Category I consisted of wide alveolar rim and no bone defects; 7 (41.2%) of the 17 ridges were assigned to this category, and a total of 22 implants were placed with no complications. Category II consisted of wide alveolar rim, lateral bone surface concavity; 4 (24%) of the 17 ridges were assigned to this category, and a total of 8 implants were placed, with fenestration defects being the most frequent complication (2 of 8 implants [25%]). Category III consisted of narrow alveolar rim, lateral bone surface concavity; 5 (29.4%) of the 17 ridges were assigned to this category, and a total of 13 implants were placed, with dehiscence defects being the most frequent complication (4 of 13 implants [31%]). Category IV consisted of distraction transport segment forming a bridge, without bone formed beneath, necessitating guided bone regeneration; 1 (6%) of the 17 ridges was assigned to this category, and following bone regeneration 1 implant was placed, without complications. | 100% functional after 1 year. | |
| 19 | Rachmeil et al. [53] | 3-4 titanium threaded implants were placed in each animal. | 12 weeks of consolidation | The x rays demonstrated radiopacity of the new bone formation. | No implant failure was noted | ||
| 20 | Enislidis et al. [54] | 31 IMZ®, Xive®, Frialit II® Friadent Mannheim, Germany. | The distractors were removed after 1.5-5.0 months (mean 2.9 months) and, whenever possible, implants were placed at that time. | In 1 patient, implants had to be removed the day after insertion, Removal of 3 implants; Secondary insertion of 4 implants and simultaneous secondary augmentation | |||
| 21 | Enislidis et al. [25] | 94 implants | 2.6 months consolidation. After 5.9 months of initial osseointegration, prosthetic rehabilitation was performed. 70 implants in 22 patients could be placed at the time of distractor removal. In some instances, dental implants were inserted at a second stage (19 implants in 8 patients) after a mean of 4.8 months (range 1-12 months) after distractor removal. Two patients had dental implants inserted both primarily during distractor removal and at a second stage (4 implants in 2 patients | 3 implants were lost before and 1 after prosthetic loading. In replacement of a lost implant, 1 supplementary implant had to be inserted for adequate distribution of prosthetic load. | cumulative implant survival rate was 95.7% | ||
| 22 | Kunkel et al. [55] | 28 14-18 mm length implants | Within a week and abutment 4-6 months later. | 38 months | 1 case and 6 months after abutment placement peri implantitis reappeared and in the next 10 months 6 mm bone loss and implant removed. | 1 case showed early bone loss of 3 mm and implant was stable for 10 months. | 4 yr estimated survival rate 90% and success rate - 59% |
| 23 | Laster et al. [56] | 7- to 10-day retention period for early bone “consolidation, ” the distraction device was removed and 1 week later implants were inserted percutaneously. The exposure of dental implants performed 3 to 4 months after insertion, and prosthetic rehabilitation completed thereafter | 6-24 months. | 1 case of marginal bone resorption was observed | 1 implant failed to integrate - inadequate primary stability | ||
| 24 | Gaggl et al. [57] | 58 implants | 12 weeks allowed to heal then implants placed. After a second healing period of 4 months the implants were used for loading by a fixed prosthetic superstructure | 1 year | 7 failed. Removed and reimplanted 3 months after | No implants were then lost. | |
| 25 | Perry et al. [38] | Sand blasted large grit acid etched solid screw type 4.1 x 12 mm. | 12 weeks after consolidation | The mean BIC (±SD) for implants placed in the distracted sites was 54.7% ± 14.6%; for the onlay grafted sites 53.8% ± 11.8%; and for the control sites 51.2% ± 14.4%. | . | ||
| 26 | Saulacic et al. [41] | 33 ITI (Straumann, Waldenburg, Switzerland) and 10 Frialoc (Frialit, Friaburg, Germany) | The mean of bone relapse following consolidation period was 1.57 ± 1.82 mm at the mesial and 1.79 ± 1.68 mm at the distal aspects of implants | ||||
| 27 | Chiapasco et al. [35] | 20 ITI solid screw SLA implants, 3.3 or 4.1 mm in diameter and 10-12 mm in length, | 3-4 months later abutments were connected to the implants and the prosthetic treatment was initiated | 18 months. | Cumulative survival and success rates of implants 100% and 95%. | ||
| 28 | Watzak et al. [58] | 10 screwshaped Branemarks MK III, two screwshaped Replace select straights, Ti-Unite, Nobel Biocaret; Gothenburg, Sweden). Implant lengths varied between 11.5 and 13 mm | 12 weeks consolidation. All implants were uncovered after a healing time of 2-4 months. Single or splinted crowns were attached after wearing temporaries | 30 months | The mean peri-implant bone resorption between implant placement and abutment connection was 0.1 mm. After 1 year of prosthetic loading, the mean periimplant bone loss amounted to 0.7 mm | ||
| 29 | Chiapasco et al. [59] | Straumann implants (Institut Straumann AG, Basel, Switzerland)19 in were inserted into the reconstructed areas, 21 placed in the distracted segments. | 4 years | The mean peri-implant bone resorption between implant placement and abutment connection after 4 years was 1.1 mm and in group 2 was 1.3 mm | In group 1 Cumulative survival and success rates of implants 100% and 89.5%, group 2 Survival and success rates of implants were 100% and 94.7%, | ||
| 30 | Marchetti et al. [60] | 36 implants | After 70 days The endosseous implants were inserted in the distracted area on the day of distractor removal in six patients and 180 days after the end of distraction in four patients. | 2 years | 1 of 36 implants (2.78%) and was removed at the moment of healing abutment connection | ||
| 31 | Polo et al. [39] | 34 acid-etched surfaced implants. | Implants placed after the planned distraction had been obtained, the mobile segment was held in place for 8 to 12 weeks allowing bone consolidation and Prosthetic treatment was performed 4 months after implant insertion, | 12.1-3.8 months | A total of 34 implants were followed for 12.1 ± 3.8 months post-restoration and 16.1 ± 3.8 months post-insertion. Mean loss of marginal bone height was 2.6 ± 1.0 mm. During the follow-up period, radiolucent lines along the implant surface were absent. | 2 (5.9%) implants failed to integrate prior to restoration and were replaced. | implant survival rate of 100% |
| 32 | Saulacic et al. [61] | 33 Straumann, 10 Frialoc | After 3 months of consolidation, 38 in the mandible and 5 in the maxilla | 8 implants demonstrated bone fenestrations and 13 demonstrated bone dehiscences. | |||
| 33 | Schleier et al. [62] | 59 Straumann dental implants (4.1 mm or 3.3 mm in diameter; lengths of 10 to 14 mm | 30 months | 1 implant was removed between the 3rd and 4th week postoperatively. | 94% survived for up to 30 months, with no significant difference between the 2 methods of distraction. | ||
| 34 | Gonzalez-Garcia et al. [63] | Implants specifications not given. | |||||
| 35 | Perdijk et al. [48] | 99 Friadent, Germany-12 IMZ, 22Frialit-II, 65 Xive) | After consolidation period of 12 weeks implants were placed and after 3 months abutments. | Failure of dental implants (13%) in 8 patients, 11 installed endoosseous implants appeared not to be successful of which 9 failed. | |||
| 36 | Wolvius et al. [42] | 63 implants | Consolidation period-2.8 to 4 months, 18 cases implants placed and 2 pateints 2 weeks after. | Of all implants placed one was lost - Insufficient primary stability | Implant success rate was 98%. | ||
| 37 | Kanno et al. [47] | 141 implants | 1 month after removing the distractor | Mean amount of bony relapse during consolidation phase at the central aspect of implant was 2.1 mm (1.5 mm group A, 2.7 mm group B)at the time of implant placement mean bony relapse was 3.6 mm (group A maintained 75% while B maintained 50% of height.) | |||
| 38 | Froum et al. [26] | 7 machined surfaces and 48 rough-surfaced implants. 4 different companies (Endopore Innova, ITI Straumann, Nobel Biocare, and Implant Innovations | consolidation time 9 to 12 weeks | 34 to 60 months | 5/55 failed. 4 occurred in sites where the transport bone underwent moderate to severe resorption. The other implant failure occurred as a result of infection at the surgical site. | ||
| 39 | González-García [64] | 12 weeks later the distractor was removed and the implants were placed. The implants were loaded 6 weeks after placement | Dehiscence or fenestration defects in 70.6% of cases (63.6% of cases in the Conventional group, 83.3% of cases in the Peizo group specifically fenestration defects in 27.3% of cases in the Conventional group and 66.7% of cases in the Piezo group and dehiscence defects in 45.5% of cases in Conventional and 83.3% of cases in Peizo. | . | success rate for distraction (implant placement and loading after distraction) was 88.2%, with only overall success rate was 100% in the Conventional group versus only 66.7% in the Peizo group. | ||
| 40 | Kanno et al. [65] | 34 11.5-15 mm length | 1 month after distraction and later After 3 months prosthesis placed | 1.8 y. | 1 implant removed | ||
| 41 | Ragheobar et al. [33] | 92 10-14 mm length implants | consolidation phase - 4 weeks. and 2 months after distraction implants were placed | 72 months. | No apparent bone loss at 164 sites, sight bone loss at 18 sites and severe at 2 sites. | 3 endoosseous implants were lost | Pt satisfaction score-8.1.surviavl rate-97%. |
| 42 | Robiony et al. [30] | 47 13-15 mm length implants | After 60 days implants placed and after 6 months of implant placement abutment and prosthesis placed. | 5 y | Total bone volume decreases at the time of implant placement-2.3% and at the time of abutment connection-0.61 mm, 1.51 mm after 5 y. mean vertical bone loss-18.7% after 5 years | In 3 cases, there was an imperfect morphology of adherent mucosa with implant coils’ exposure that required a palatal fibromucous graft. | 97.9%and 91.5% |
| 43 | Perez-Sayans et al. [66] | 28 Straumann and 9 Friaolac. Length varied from 8 mm to 13 mm. | After a consolidation period of 12 weeks implants were placed and after 12 weeks of osseointegration implants were loaded. | 1 year | None of the implants was lost | ||
| 44 | Zhao et al. [67] | After 1 week of consolidation, the distraction screws were replaced by consolidation screws to combine the coronal portion of the DI with the apical portion, so that the distractors were transformed in prosthetic implants | The tissue along the lingual cortex was very hard and appeared to be dense cortical bone just 5 weeks after consolidation, whereas the labial surface did not show continuous cortical bone until 12 weeks after consolidation. BIC was higher around the threads of the DI (60.48% ± 6.12%) than around the threads of the distraction screw (51.65% ± 3.83%). | ||||
| 45 | Bilbao et al. [36] | 71 Straumanns (Institut Straumann AG, Basel, Switzerland) titanium dental implants All implants were 10 mm long and with a 4.1 mm RN diameter with an SLAs surface | The consolidation period was 8 weeks. A total of 39 implants were placed in native bone and 32 in newly ODG bone | The resonance frequency analysis at implant placement in distracted bone showed a mean ISQ of 73 ± 4.1, whereas the implants placed in pristine bone yielded a value of 76.8 ± 4.4 ISQ. | Implant stability was higher for implants located in pristine bone. | ||
| 46 | Elo et al. [28] | 184 implants were placed in the autogenous bone-grafted sites and 56 implants were placed in the distracted bone sites. | 36 months | In the autogenous grafted group, 3 implants failed in the posterior mandible, 1 in the anterior maxilla, 1 in the anterior mandible, and 1 in the posterior maxilla. In the distraction group, 1 implant failed in the posterior mandible. | Implants placed in sites restored with autogenous bone grafts had an implant success rate of 97% (178/184), implants placed in distracted bone sites had a success rate of 98% 55/56. | ||
| 47 | Ettl et al. [46] | 2 Camlog®-Implants, Camlog Biotechnologies, Basel, Switzerland; seven Astra®-Implants, Astra Tech, Mölndal, Sweden; 73 ITI®-Implants Straumann, Basel, Switzerland) | Due to deficient ossification of the callus, soft tissue dehiscence, or inadequate fixed gingiva, insertion of dental implants was prolonged to an average of 2 months, resulting in an overall mean consolidation period of 4.5 months (135.9 days). | 45.8 months | The mean vertical bone height after implantation was 6.4 mm with 6.3 mm (range 5-8 mm) in the maxilla and 6.4 mm (range 4-12 mm) in the mandible. | Four implants of three patients failed.1 immediate loss and three explantations due to periimplantitis were recorded. | Survival rate was 95.10% |
| 48 | Funaki et al. [68] | 9 mm length 3.5 mm diameter, astra tech, moindal, Sweden | Implant placement 2 months after augmentation | Resonance frequency analysis revealed that implants placed in the distracted area achieved good stability. The implants were fully embedded in mature lamellar bone, and direct bone contact with the implant surface was seen 3 months after implant placement in the distracted area.ISQ on DO side-60.4. | |||
| 49 | Xie et al. [69] | 3 months after the completion of distraction, 2 titanium implants were placed. | The implant-bone interface showed bony integration, and there was no significant difference in the implant-bone contact rate between the distraction and control sides. X-rays showed that the implants were well integrated 3 months after implant placement. | ||||
| 50 | Kanno et al. [44] | 80 Straumann ITI, Institute Straumann AG, Basel, Switzerland; Astra Tech, Astra Tech AB, G¨oteborg, Sweden; Novel Biocare AB, G¨oteborg, Switzerland), more than 11 mm in length and 4 mm in platform width, | 3 months consolidation time. After the alveolar distractor was removed, soft tissue was allowed to heal for 3-4 weeks before implant surgery | 47.5 months | 3 failed in three patients (one bilateral and two unilateral distraction cases) | survival rate was 96.3% 77/80 | |
| 51 | Yamauchi et al. [43] | 32 Astra Tech AB, Mo lndal, Sweden; 3 Nobel Biocare AB, Gothenburg, | Consolidation period 13 weeks | 5 years | 2 implants were not achieved to the successful results during the follow-up period: 1 caused symptomatic pain and the other was located in an inappropriate position without implant mobility or peri-implant radiolucency | The implant survival and success rates were 100% and 94.2%, respectively. | |
| 52 | Chenping et al. [70] | After a consolidation period of 3 to 4 months the implant was left in the bone, The mean period from the first operation to the start of dental implant loading was 6.3 months. | 3-year | Cumulative survival rate of the dental implants was 93.75%. |
BIC, Bone Implant contact; DI, Distraction implant; SD, Standard deviation.
Table 2: Implants placed in the distracted segment and associated clinical parameters observed.
Results
Distraction osteogenesis for the correction of deficits of edentulous ridges seems to be a reliable method for overcoming the problems connected with bone grafting and GBR. The following advantages can be anticipated with intraoral distraction osteogenesis:
i) Provides the opportunity to obtain a natural formation of bone between the distracted segment and basal bone in a relatively short time span.
ii) Eliminates the need to harvest bone, with consequent shortening of operating times and reduction in morbidity.
iii) Soft tissues can follow elongation of the underlying bone.
iv) Can be frequently performed under local anaesthesia on an outpatient basis and postoperative recovery is favourable.
v) The regenerated bone seems to resist resorption.
vi) The newly generated bone seems to be able to withstand the functional demands of implant supported prostheses [14]. Distraction osteogenesis can produce a gain in alveolar bone height from 5 to15 mm in edentulous segments of the mandible and mean values from 5 mm to 9.9 mm [20-22]. Two recent prospective studies documented average vertical gains following DO of 6.5 mm (range, 3 to 15 mm) and 7 mm (range, 5 to 9 mm) [23,24].
Discussion
The data related to the long-term survival rate of implants in the lower jaws post distraction osteogenesis in partially edentulous patients is limited. In a study by Enisdilis et al. survival rate of 95.7% after a mean follow-up of 39.4 months (range 4.8-58.3 months) post-implantation was observed which is comparable to the survival rate of 100% reported by Chiapasco et al. [22,25]. The results of the investigation by Froum et al. documented a similar implant success rate (90.9%) [26]. In case of the maxilla, a survival rate of 90.4% was reported by Jensen et al. with at least 3 years follow-up postrestoration after a vertical distraction of 3-15 mm (mean 6.5 mm) [23]. Even though there was an adequate bone production, ensuring a high longterm implant survival rate in this series, 75.7% of patients suffered complications. In the literature, the total percentage of complications ranges from 0% to 100% [27]. No statistical difference was observed in success rates between implants placed in autogenous bone grafted sites v/s distracted bone sites. However when comparing bone grafting neovascularity with distraction regenerate has neovascularity it is seen that the latter is more resistant to infection than is the case with bone grafting.
Elo et al. displayed as much success in autogenous bone grafting as distraction osteogenesis in preprosthetic alveolar bone augmentation procedure [28]. Chiapasco et al. reported a better long term prognosis, when comparing GBR to DO as far as bone gain maintenance and peri-implant bone resorption after prosthetic loading are concerned. Though survival rates of implants are the same between DO and GBR groups, the success rates of implants differ significantly. Since it is possible to achieve more vertical gain with DO, it is more commonly indicated than GBR. Results from this multicenter prospective study seem to demonstrate that DO can be an effective and reliable surgical alternative to correct vertical deficits of edentulous ridges resulting from atrophy, trauma, congenital malformation, and the resection of benign or malignant tumors [29]. These results have been confirmed by other studies [23,30]. Regenerated bone seems to withstand the biomechanical demands of implant loading well. By taking periapical radiographs from time to time it is possible to assess the subsequent increase in bone density, 3 to 4 years after prosthetic loading. These encouraging results have been confirmed by other studies from the histologic and histomorphometric perspectives [31-33].
The histological analysis revealed that the new bone formed interconnected bone trabeculae that were oriented at an angle to the cut bone surface that was created through osteotomy. Furthermore, the new bone in the distraction region consisted of woven bone reinforced by parallel-fibered bone. With regards to the rate of distraction Ragheobar et al. waited for 5 days before initiation of distraction and used a rate of distraction of 1mm/day, which worked well [31]. A rate of distraction that allows for lengthening with bone formation and a proper soft tissue response is one that is said to be optimum. If too rapid, non-union will occur, whereas if it is too slow, there may be premature union. A continuous rhythm of distraction is thought to be ideal, wherein lengthening of approximately 1mm a day is noted [14]. A 3-week consolidation period before implant placement offers an immature bone that starts to form columns from the borders of the distracted area.
Histological studies carried out in humans, have proved the presence of bone trabecula parallel to the distraction vector and support the criterion that an 8-week consolidation period is enough for implant placement [32]. At the end of a 3-month consolidation period, the cumulative success rate of dental implants was 100% in human models [34,35]. In his series, Bilbao et al. with the same consolidation period, high primary stability was obtained only slightly lower than that achieved in native bone [36]. A human histologic study performed by Zaffe et al. showed that bone formation finished 60 days after the end of the distraction and decreased with longer times; early implant insertion was suggested to avoid bone loss due to mechanical unloading [32]. Placing an implant after 3 weeks of completion of distraction does not hamper bone regeneration. The implants osseointegrated in the augmented ridge, and the integration between implants and regenerated bone was better at 12 weeks after distraction than at 8 weeks after distraction [37].
In contrast Perry et al. concluded that integration of implants placed into augmented sites was equal to that of the control sites, and there was no difference in integration between the grafted and distracted sites [38]. With regards to peri-implant bone resorption alveolar bone distraction exhibited a mean peri-implant bone loss of 1.9 mm/year, together with high survival rates following prosthetic loading hence in alveolar DO, an overcorrection with 1 to 3 mm is suggested [39-41]. Wolvius et al. reported resorption rate of around 20% using a rigid extraosseous device [42]. Bone resorption does not depend only upon the use of a rigid or a semirigid distractor device. This was substantiated by Saulacic et al. described who described bone relapse of 26-29% with the use of an intraosseous semirigid distractor [41]. However a long-term implant survival rate for oral rehabilitation was noticed [43].The use of sinus lifting along with alveolar distraction for pre-implant reconstruction has also been seen. This brought about a change in the contour of a severely atrophic resorbed maxillary alveolus, thereby regenerating adequate bone on both the alveolar side and inside the maxillary sinus. This along with simultaneous sinus lifting proves to be a useful technique for patients with a severely atrophic maxilla requiring dental implant rehabilitation [44].
Complications
Chiapasco et al. concluded that despite very promising results, some limits were related to DO. First, inclination of the distracted bone segment, probably the result of traction of the palatal mucosa or of the muscles of the floor of the mouth which was successfully corrected by means of orthodontic appliances. Second, it is possible that there may be an insufficient dimension of the neocallus in the distracted region during the time of placing the implant. This may lead to a partial exposure of the implant threads in the region of distracted neogenerated tissue because of insufficient bone volume which has to be corrected by grafting the area with autogenous bone to cover the exposed implant threads. Third, the distraction device limits the application of the technique to composite vertical and horizontal defects. Adequate vertical osteotomies must be made in order to prevent interferences in the movement of the osteotomized segment. This may compromise the final result. Finally, minimal residual bone height of the atrophic area is needed to avoid the risk of alveolar damage, violation of the floor of the nose or the maxillary sinus, or mandibular fracture.
The authors arbitrarily chose a minimum bone height of approximately 5 mm to obtain a bone segment with enough volume to be stabilized by the distraction plate and microscrews with no risk of violation of the floor of the nose, the maxillary sinus mucosa, or the alveolar nerve. Moreover, vertically atrophied mandibles with less than 5 mm of bone height present a relevant risk of fracture during or after the performance of the osteotomy. 22 Fractures of basal bone and transport segment, breakage of distractor, and severe mechanical problems leading to abortion of treatment have also been described [27].Bone formation defects post distraction osteogenesis were usually chanced upon at the time of distractor explantation. These require supplementary corrective augmentation procedures in 11 of 45 distraction sites in a study [45].
Three-quarters of patients suffered complications requiring supplementary treatment measures were reported by Enisdilis et al. Distraction implantation to distractor removal was the case of fourfifths of complications that occurred. These figures undermine the theory that distraction osteogenesis is not an uncomplicated procedure [25]. However, dental implants were safely inserted into distracted areas in most instances and long-term survival of loaded implants was satisfactory. Often-mentioned soft tissue complications are dehiscences and failed lengthening of the fixed gingiva, resulting in a reduced vestibular sulcus Soft tissue dehiscences more frequently occur by the use of extraosseous devices which demand a larger covering mucoperiosteal flap and enforce the tension caused by surrounding cheek and tongue muscles [25,41]. According to Ettl et al. missing soft tissue extension may be more common with distraction of mandibular bone [46]. Kanno et al. said if a vertical alveolar DO is planned within 6 months of surgery such as for tooth extraction or alveolar trauma there should be sufficient over correction to compensate for a bone relapse of upto50% [47]. As concluded by Predjik et al. patients suffering from severe mandibular atrophy that were treated either with conventional augmentation techniques or VDO prove to be more susceptible to various complications wherein a majority of these complications occurred in the first year [48]. As with any surgical procedure there are a few limitations associated with DO, but the advantages outweigh the limitations. Hence DO can be considered as a dependable option to augment complex alveolar ridge defects.
Conclusion
Distraction osteogenesis is an effective surgical procedure to treat vertical horizontal alveolar ridge deficiencies. By the various studies reviewed it can be concluded that is a reliable technique without any major complication and has a better long term prognosis and stability, especially after implant placement than conventional guided bone regeneration and bone transplantation techniques. In complex bony defects prior to implant placement excellent predictable ridge augmentation can be achieved which is very difficult with other conventional modalities. It can produce a gain in alveolar bone height from 5 to15 mm with the survival rate of implants ranging from 95.7- 100% and success rate 94.2-98%. To conclude alveolar distraction osteogenesis is a relatively simple, effective and reliable technique for alveolar ridge reconstruction in contemporary implant dentistry.
References
- Polo WCK, Cury PR, Sendyk WR, Gromatzky A (2005) Posterior mandibular alveolar distraction osteogenesis utilizing an extraosseous distractor: A prospective study. J Periodontol 76: 1463-1468.
- Block MS, Chang A, Crawford C (1996) Mandibular alveolar ridge augmentation in the dog using distraction osteogenesis. J Oral Maxillofac Surg 54: 309-314.
- Nystrom E, Kahnberg K-E, Gunne J (1993) Bone grafts and Branemark implants in the treatment of severely resorbed maxilla: A two year longitudinal study. Int J Oral Maxillofac Implant 8: 45-53.
- Triplett RG, Schow SR (1996) Autologous bone grafts and endosseous implants: Complementary techniques. J Oral Maxillofac Surg 54: 486-494.
- Caplains L, Sigurdsson TJ, Rohrer MD, Wikesjo UM (1997) Effect of allogeneic, freeze-dried, demineralized bone matrix on guided bone regeneration in supra-alveolar peri-implant defects in dogs. Int J Oral Maxillofac Implant 12: 634-642.
- Jenson OT, Green RO Jr, Johnson L, Kessebaum D (1995) Vertical guided bone-graft augmentation in a new canine mandibular model. Int J Oral Maxillofac Implant 10: 335-344.
- Oikarinen KS, Sandor GK, Kainulainen VT, Salonen KM (2003) Augmentation of narrow traumatized anterior alveolar ridge to facilitate dental implant placement. Dent Traumatol 19: 19-29.
- Rummelhart JM, Mellonig JT, Gray JL, Towle HJ (1989) A comparison of freeze-dried bone allograft and demineralized freeze-dried bone allograft in human periodontal osseous defects. J Periodontol 60: 655-663.
- Lovelace TB, Mellonig JT, Meffert RM, Jones AA, Nummikoski PV, et al. (1998) Clinical evaluation of bioactive glass in the treatment of periodontal osseous defects in humans. J Periodontol 69: 1027-1035.
- Codivilla A (1905) On the means of lengthening, in the lower limbs, the muscles and tissues which are shortened through deformity. J Bone Joint Surg Am 2: 353-369.
- Illizarov GA, Devyatov AA, Kamerin VK (1980) Plastic reconstruction of longitudinal bone defects by means of compression and subsequent distraction. Acta Chir Plast 22: 32-41.
- Illizarov GA (1989) The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability and fixation and soft tissue preservation. Clin Orthop Relat Res 238: 249-281.
- Illizarov GA (1989) The tension-stress effect on the genesis and growth of tissues. Part II The influence of rate and frequency of distraction. Clin Orthop Relat Res 239: 263-285.
- Block MS, Almerico B, Crawford C, Gardiner D, Chang A (1998) Bone response to functioning implants in dog mandibular alveolar ridges augmented with distraction osteogenesis. Int J Oral Maxillofac Implant 13: 342-351
- Chin M, Toth BA (1996) Distraction osteogenesis in maxillofacial surgery using internal devises: Review of five cases. J Oral Maxillofac Surg 54: 45-53.
- Rachemiel A, Srouji S, Peled M (2001) Alveolar ridge augmentation by distraction osteogenesis. Int J Oral Maxillofac Surg 30: 510-517.
- Uckan S, Haydar SG, Dolanmaz D (2002) Alveolar distraction: Analysis of 10 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94: 561-565.
- Watzek G, Zechner W, Crismani A, Zauza K (2000) A Distraction sbutment System for 3-Dimensional distraction osteogenesis of the alveolar process: Technical Note. Int J Oral Maxillofac Implants 15: 731-737.
- Oda T, Sawaki Y, Ueda M (1999) Alveolar ridge augmentation by distraction osteogenesis using titanium implants: An experimental study. Int J Oral Maxillofac Surg 28: 151-156.
- Chiapasco M, Romeo E, Vogel G (2001) Vertical distraction osteogenesis of edentulous ridges for improvement of oral implant positioning: A clinical report of preliminary results. Int J Oral Maxillofac Implants 16: 43-51
- Garcia-Garcia A, Somoza-Martin M, Gandara-Vila P, Saulacic N, Gandara-Rey JM (2003) Alveolar distraction before insertion of dental implants in the posterior Mandible. Br J Oral Maxillofac Surg 41: 376-379.
- Chiapasco M, Consolo U, Bianchi A, Ronchi P (2004) Alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: A multicenter prospective study on Humans. Int J Oral Maxillofac Implants 19: 399-407.
- Jensen OT, Cockrell R, Kuhike L, Reed C (2002) Anterior maxillary alveolar distraction osteogenesis: A prospective 5-Year clinical study. Int J Oral Maxillofac Implants 17: 52-68.
- McAllister BS (2001) Histologic and radiographic evidence of vertical ridge augmentation utilizing distraction osteogenesis: 10 consecutively placed distractors. J Periodontol 72: 1767-1779.
- Enislidis G, Fock N, Millesi-Schobel G, Klug C, Wittwer G, et al. (2005) Analysis of complications following alveolar distraction osteogenesis and implant placement in the partially edentulous mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 100: 25-30
- Froum SJ, Rosenberg ES, Elian N, Tarnow D, Cho SC (2008) Distraction osteogenesis for ridge augmentation: Prevention and treatment of complications. Thirty case reports. Int J Periodontics Restorative Dent 28: 337-345.
- Garcia AG, Martin MS, Vila PG, Maceiras JL (2002) Minor complications arising in alveolar distraction osteogenesis. J Oral Maxillofac Surg 60: 496-501
- Elo JA, Herford AS, Boyne PJ (2009) Implant success in distracted bone versus autogenous bone grafted sites. J Oral Implantol 35: 181-184
- Chiapasco M, Romeo E, Casentini P, Rimondini L (2004) Alveolar distraction osteogenesis vs. vertical guided bone regeneration for the correction of vertically deficient edentulous ridges: A 1-3-year prospective study on humans. Clin Oral Implants Res 15: 82-95.
- Robiony M, Zorzan E, Polini F, Sembronio S, Toro C, et al. (2008) Osteogenesis distraction and platelet rich plasma-combined use in restoration of severe atrophic mandible.long term results. Clin Oral Implants Res 19: 1202-1210.
- Raghoebar GM, Liem RS, Vissink A (2002) Vertical distraction of the severely resorbed edentulous mandible A clinical, histological and electron microscopic study. Clin Oral Implants Res 13: 558-565.
- Zaffe D, Bertoldi C, Palumbo C, Consolo U (2002) Morphofunctional and clinical study on mandibular alveolar distraction osteogenesis. Clin Oral Implants Res 13: 550-557.
- Raghoebar GM, Stellingsma K, Meijer HJ, Vissink A (2008) Vertical distraction of severely resorbed edentulous mandible: an assessment of treatment outcome. Int J Oral Maxillofac Implants 23: 299-307.
- Nosaka Y, Tsunokuma M, Hayashi H, Kakudo K (2000) Placement of implants in distraction osteogenesis: A pilot study in dogs. Int J Oral Maxillofac Implants 15: 185-192
- Chiapasco M, Lang NP, Bosshardt DD (2006) Quality and quantity of bone following alveolar distraction osteogenesis in the human mandible. Clin Oral Implants Res 17: 394-402.
- Bilbao A, Oliveira MH, Varela-Centelles PI, Seoane J (2009) Assessment of dental implant stability in osseodistraction-generated bone: a resonance frequency analysis. Clin Oral Implants Res 20: 772-777.
- Oda T, Sawaki Y, Ueda M (2000) Experimental alveolar ridge augmentation by distraction osteogenesis using a simple device that permits secondary implant placement. Int J Oral Maxillofac Implants 15: 95-102
- Perry M, Hodges N, Hallmon DW, Rees T, Opperman LA (2005) Distraction osteogenesis versus autogenous onlay grafting.part 1: outcome of implant integration. Int J Oral Maxillofac Implants 20: 695-702.
- Polo WC, de Araujo NS, Lima YB, Joly JC, Sendyk WR, et al. (2007) Peri-Implant bone loss around posterior mandible dental implants placed after distraction osteogenesis: Preliminary findings. J Periodontol 78: 204-208.
- McAllister BS (2003) Gaffaney TE Distraction osteogenesis for vertical bone augmentation prior to oral implant reconstruction. Periodontol 2000 33: 54-66.
- Saulacic N, Somoza-Martin M, Gándara-Vila P, Garcia-Garcia A (2005) Relapse in alveolar distraction osteogenesis: An indication for overcorrection. J Oral Maxillofac Surg 63: 978-981.
- Wolvius EB, Scholtemeijer M, Weijland M, Hop WC, van der Wal KG (2007) Complications and relapse in alveolar distraction osteogenesis in partially dentulous patients. Int J Oral Maxillofac Surg 36: 700-705
- Yamauchi K, Takahashi T, Nogami S, Kataoka Y, Miyamoto I, et al. (2013) Horizontal alveolar distraction osteogenesis for dental implant: long-term results. Clin Oral Implants Res 24: 563-568
- Kanno T, Mitsugi M, Paeng JY, Sukegawa S, Furuki Y, et al. (2012) Simultaneous sinus lifting and alveolar distraction of a severely atrophic posteriormaxilla for oral rehabilitation with dental implants. Int J Dent 2012: 471320.
- GarcÃa GarcÃa A, Somoza Martin M, Gandara Vila P, Gandara Rey JM (2004) A preliminary morphologic classification of the alveolar ridge after distraction osteogenesis. J Oral Maxillofac Surg 62: 563-566.
- Ettl T, Gerlach T, Schüsselbauer T, Gosau M, Reichert TE, et al. (2010) Bone resorption and complications in alveolar distraction osteogenesis. Clin Oral Investig 14: 481-489.
- Kanno T, Mitsugi M, Furuki Y, Hosoe M, Akamatsu H, et al. (2007) Overcorrection in vertical alveolar distraction osteogenesis for dental implants. Int J Oral Maxillofac Surg 36: 398-402.
- Perdjik FBT, Meijer GJ, Strijen PJ, Koole R (2007) Complications in alveolar distraction osteogenesis in the atrophic mandible. Int J Oral Maxillofac Surg 36: 916-921.
Citation: Sumra N, Kulshrestha R (2017) Distraction Osteogenesis in Implantology for Ridge Augmentation - A Systematic Review. Dent Implants Dentures 2: 119. DOI: 10.4172/2572-4835.1000119
Copyright: © 2017 Sumra N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5861
- [From(publication date): 0-2017 - Jul 01, 2025]
- Breakdown by view type
- HTML page views: 4804
- PDF downloads: 1057