Distinct Characteristics of the COVID-19 among Children and Young Adolescents Treated at Gulu Regional Referral Hospital; Northern Uganda: A Cross-Sectional Study
Received: 03-Feb-2022 / Manuscript No. JIDT--22-53271 / Editor assigned: 07-Feb-2022 / PreQC No. JIDT-22-53271(PQ) / Reviewed: 21-Feb-2022 / QC No. JIDT-22-53271 / Revised: 24-Feb-2022 / Manuscript No. JIDT--22-53271(R) / Published Date: 28-Feb-2022 DOI: 10.4173/2332-0877.22.S1.003.
Abstract
Background: Ever since the appearance of acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease (COVID-19) in Wuhan in mid-December 2019, its spread has been dramatic worldwide. It became apparent that the number of pediatric COVID-19 patients was much lower than in adults. Variable clinical presentations and progression have characterized morbidity and mortality in children and young adults.
Objective: The objective of this study was to assess the characteristics of the COVID-19 among children and adolescents 20 years and below in Northern Uganda and determine factors associated with treatment outcomes in the study population.
Methods: A cross-sectional study conducted a retrospective data abstraction of the COVID-19 patients registered in the Gulu Hospital Health Management Information System (HMIS) database and other tools. The study covered the period between March 2020 and October 2021. Data that met the inclusion criteria were consecutively mined from the Gulu Hospital HMIS database. A local IRB approved the study. SPSS version 25.0 was used for data analysis, and a p-value less than 0.05 was considered significant.
Results: There were 41 COVID-19 patients 20 years and below among the 664 total COVID-19 patient population, constituting 41/664(6.2%) of the COVID-19 patients treated at Gulu Regional Referral Hospital from March 2020 to October 2021. The median age was 19 years (range 13 to 20 years), the mean age was 18.2 years SD+1.95 at 95% CI: 17.51-18.74. Females constituted 58.5% of the study population. The mean duration of hospital stay was 14.44 days SD+10.45 at 95% CI: 11.14-17.74, and the mean duration of symptoms at admission were 7.96 days SD+7.38 at 95% CI: 4.84-11.07. The comorbidities were cardiovascular diseases 3/41(7.3%) and hypertension 3/41(7.3%) and were not in the same patients. Pneumonia 1/41(3.3%) and acute liver injury 1/41(3.3%) were the observed complications. The morbidity and mortality rates were 2/41(4.9%) and 0/41(0.0%), respectively. Participants’ symptoms, signs, complications, and comorbidities by gender were not statistically significant.
Conclusion: Data showed excellent treatment outcomes of the COVID-19 among children and adolescents 20 years and below in Northern Uganda with a recovery rate of 100.0%. The burden of symptoms of the illness, comorbidities, and complications was fewer. There is a need to conduct more extensive studies on the role played by age in the successful recovery of COVID-19 patients, even in a low-resource milieu.
Keywords: Adolescents; COVID-19; Recovery; Morbidity; Mortality
Introduction
Ever since the appearance of acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease (COVID-19) in Wuhan in mid-December 2019, its spread has been dramatic worldwide [1]. It became apparent that the number of pediatric COVID-19 patients was much lower than in adults [2]. Variable clinical presentations and progression have characterized morbidity and mortality in children and young adults [2]. However, coronavirus disease 2019 (COVID-19) remains one of the biggest global health challenges [3]. It is reported that more than 38 million people have so far been infected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes COVID-19, and more than one million people have died because of the infection [3]. Children comprise roughly 10% of all the infected persons with the COVID-19 in most studies [4].
In Qatar, for example, since the beginning of the pandemic in February 2020 up to April 2021, over 180,000 people have been infected with COVID-19, of whom a minority of 36.6% (95% CI: 35.7-37.5) were children (aged 0-18 years old) [5]. As in all countries affected by the COVID-19, there is a need to define symptomatology of the disease in children, develop and implement school health policies and determine what constitutes a clinical case definition [6]. This is expected to ease contact tracing and management of all cases of COVID-19 among children and young adults in communities with limited resources.
Although research suggests that children have a lower susceptibility to COVID-19 infection [7-9] than adults, children can still get infected and transmit the virus to others [10]. Research also suggests that children are less likely to develop symptomatic infection and less likely to have the severe disease than adults [8,11].
In many other ways, children have been indirectly affected by COVID-19, such as school closures in many countries [12-14]. The controversy about return-to-school policies remains unresolved though there is increasing evidence that transmission dynamics in children differed from that in adults [15,16]. In children, symptoms of the illness are like those of other acute respiratory viral infections, the upper airways being more affected than the lower airways [17]. Thus far, over 90% of children who tested positive for the virus in the United Kingdom presented with mild or moderate symptoms and signs [17]. In the United Kingdom, most children were asymptomatic, and only a few cases were severe, unlike the adult population [17]. In addition, incidences of deaths have been rare and occurred mainly in children with underlying co-morbidity [17].
The situation in Uganda and mainly northern Uganda has followed the same pattern. A review of the Hospital data from Gulu Regional Referral Hospital from March 2020 to October 2021 has shown exciting statistics, which is worth noting [18,19]. The number of children and adolescents 20 years and below infected with the COVID-19 virus was 41/664(6.2%), with no mortality in one year and seven months [18,19]. The rate of complications of the coronavirus-19 disease among the same age group was low at 2/41(4.9%) (Table 3).
The objective of this study was to assess the characteristics of the COVID-19 among children and adolescents 20 years and below in Northern Uganda and determine factors associated with treatment outcomes in the study population.
Materials And Methods
Study site
This study was conducted in Gulu Regional Referral Hospital in Northern Uganda, covering admissions of COVID-19 patients from March 2020 to October 2021. Gulu Hospital is a regional referral hospital for patients from Northern Uganda. However, it receives patients from neighboring countries, for example, South Sudan and the Democratic Republic of Congo (DR Congo). It is also a teaching hospital for Gulu University Medical school and many other health training institutions in the region. It is a 394-bed capacity hospital with outpatient services estimated at over 120,000 patients every year. The Hospital has specialized units such as internal medicine, surgery, pediatrics, reproductive health, tuberculosis, HIV, cardiac, chest, dental, dermatology, sickle cell disease, diabetes, hypertension, ear, nose and throat, nutrition, accident and emergency, laboratory, ophthalmology, mental health, and orthopedic and rehabilitative clinics that consultants from Gulu Regional Referral Hospital and Gulu University manage.
Gulu Regional Referral Hospital was designated by the Ugandan Ministry of Health as a COVID-19 treatment center in March 2020 when COVID-19 was declared a pandemic. As a result, a particular treatment unit for the management of COVID-19 (Gulu CTU) was established with a fully-fledged high dependency unit (HDU), with oxygen supply and staff to manage the department. The team leader for the Gulu CTU is a consultant physician who cares for all the COVID-19 patients admitted to the unit.
In addition, the Ugandan Ministry of Health and World Health Organization (WHO) health experts give additional support for managing the COVID-19 patients at the center using standard protocols developed and practiced in Uganda.
Study design
This was a cross-sectional study design. A retrospective record review and abstraction of all COVID-19 hospital admissions registered in the Gulu Health Management Information System (HMIS) database and other tools was conducted. The period for the study was March 2020 to October 2021. Established by the Ugandan Ministry of Health, HMIS has been the primary source of information on COVID-19 hospital admissions, referrals, and deaths. In addition, COVID-19 notification is compulsory in Uganda, and the emergency operation center at the Uganda National Public Health Institute receives all reports on patients admitted to both public and private hospitals with COVID-19.
Sources of data
For the period of this study, COVID-19 patients admitted to Gulu Regional Referral Hospital with COVID-19 were nine hundred and forty-four (944). We included all patients registered in the Gulu Regional Referral Hospital HMIS database. Information on individual's socio-demographic characteristics, self-reported symptoms, signs, comorbidities, COVID-19 Treatment Unit (CTU) admissions, ICU admissions, and ventilatory support, dates of symptoms’ onset, dates of hospital admissions, dates of discharges/releases, duration of the hospital stay, the reported circumstances of contracting the coronavirus, the vaccination status and hospital outcomes (deaths, referrals, and releases/discharges) were documented. Gulu Hospital HMIS data were accessed, already de-identified and publicly available documents on patients treated during the study period. Following ethically agreed principles on open data access, this review did not require stringent ethical approval in Uganda as we mainly worked on records with no identifiers included. However, we obtained ethical and administrative approvals from the Gulu Regional Referral Hospital Institution and Ethics Review Committee to access the archived Gulu Hospital data on COVID-19 patients.
Selection criteria
Inclusion criteria: The following were the inclusion criteria for the participants (i) Confirmed cases of SARS-CoV-2 with positive RT-PCR results (ii) medical records of patients 12 years and above (iii) completed information on the chart and other medical tools (iv) admission records in the hospital
Exclusion criteria: We excluded (i) incomplete medical records, (ii) records with no RT-PCR results (iii) participants’ files that were not registered on the HMIS database.
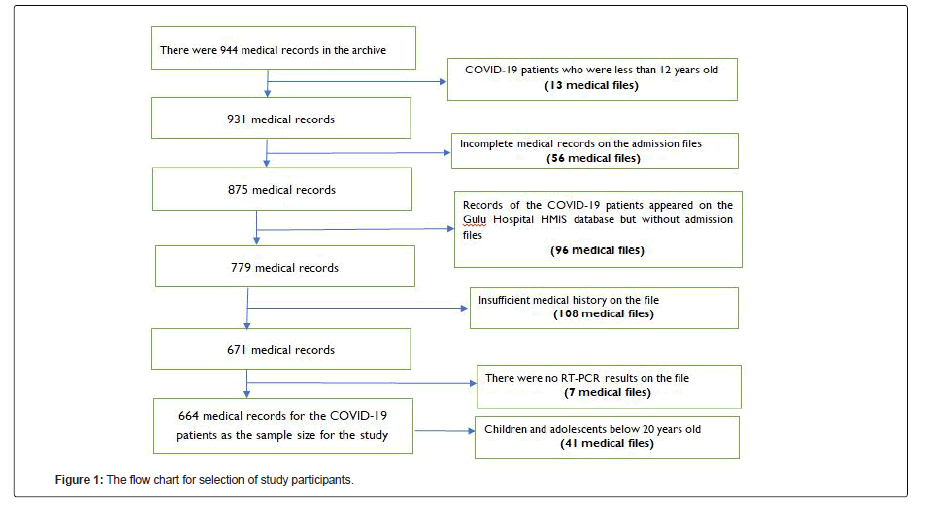
Selection of the medical files: The medical records for the COVID-19 patients in Gulu Regional Referral Hospital archives were accessed by the research team. The selection of the COVID-19 patients' files was conducted consecutively and reviewed by the research team. The selection criteria were applied to each admission file (a total of nine hundred and forty-four files); thirteen (13) patients were less than twelve years; fifty-six (56) patients had incomplete information on the files; ninety-six (96) patients appeared in the HMIS database without admission files; one hundred and eight (108) patients had insufficient medical history on the file, and seven (7) were excluded due to lack of positive RT-PCR results on the files. Finally, a total of six hundred and sixty-four (664) files were included in the participating medical records for this research. Out of these, 41 files were for patients 20 years and below and included in the final analysis.
Sample size: We determined the sample size for the study population using the selection criteria on the research protocol. Six hundred and sixty-four (664) records were included as the sample size, and forty-one were children and adolescents 20 years and below.
Training of research assistants: To obtain excellent and clean information from these COVID-19 patients' medical files, the research team trained the research assistants who were four in number (two medical officers, one clinical officer, and one nurse) on how to use the selection criteria, accurately record data from the admission forms and exclude forms that were considered incomplete. In addition, the research assistants were trained on infection, prevention, and control (IPC) of COVID-19. They were required to use facemasks, eye shields, and hand sanitizers during and after reviewing the documents. The corresponding author supervised the data collection exercise from the beginning to the end, ensuring that he checked every file to confirm the completeness of the data collected.
Procedures for data collection: Consecutively registered COVID-19 patients treated at Gulu Regional Referral Hospital with a positive quantitative RT-PCR test result for SARS-CoV-2 were recruited. SARS-CoV-2 diagnostic tests follow National and International standards. The tests were conducted in certified laboratories of Gulu Regional Referral Hospital and Uganda Virus Research Institute (UVRI) as the Ugandan Ministry of Health protocols required.
Variables for the study: The outcome variables for this study were treatment outcomes (alive or dead) or gender (females or males). The independent variables were the socio-demographic characteristics of the COVID-19 patients (age, sex, occupation, religion, tribe, districts, and level of education), comorbidities, complications and treatments used, oxygen saturation at admission, date of discharge from the hospital, duration of hospital stay, disease severity, and others), clinical presentations (signs and symptoms), vaccination status, residences, and circumstances under which COVID-19 patients contracted the coronavirus.
Data analysis: The analysis period was from the epidemiological week (starting month and date of March 2020) to the epidemiological week (until month and date of October 2021). The analysis was pre- specified and defined before reading the medical data in the Gulu Regional Referral Hospital records. The sample size was all patients (aged ≥ 12 years and <20 years) with confirmed SARS-CoV-2 diagnoses admitted to the Gulu Regional Referral Hospital and registered in the HMIS database between the epidemiological weeks of March 2020 and October 2021.
Means, medians, standard deviations, histograms, frequencies, and percentages were used to summarize continuous variables, while frequencies and proportions were calculated for categorical variables. Age-adjusted and sex-adjusted rates for each district by the direct method using the estimated Ugandan population for 2020 as a reference were calculated.
We used the Chi-Square tests at bivariate analysis to observe associations between independent and dependent variables at 95% Confidence Intervals. Variables with p-values less or equal to 0.2 were entered into a multivariable logistic regression analysis to determine factors associated with COVID-19 patients treated at GRRH. However, the Gulu Hospital HMIS data contained much-missing information for some variables, such as reported symptoms, weight, height, drugs used, and co-morbidities. Therefore, we used additional GRRH records to fill in the missing data. Also, in the post hoc analysis, we evaluated the missing data pattern and conducted a sensitivity analysis via multiple imputations by chained equations, generating 30 imputed datasets. SPSS version 25.0 was used for data analysis, and various imputations were performed utilizing the STROBE guideline recommendations. In addition, Adjusted Odds Ratios (AOR) for independent variables were calculated for the COVID-19 patients 20 years and below who were treated at the Gulu Regional Referral Hospital from March 2020 to October 2021.
Ethical considerations
This retrospective data review of COVID-19 patients' medical files at the Gulu Regional Referral Hospital was approved by the Gulu Regional Hospital Institutional, Ethics, and Review Committee. All institutional guidelines were followed during the study and after.
Results
Findings from this study show that the overall mortality rate among the COVID-19 patients treated at the Gulu Regional Referral Hospital from March 2020 to October 2021 was 32/664(4.8%) and a recovery rate at 632/664(95.2%). Most patients treated were unvaccinated 661/664(99.5%). Interestingly, out of the many COVID-19 patients successfully treated at the Gulu Regional Referral Hospital CTU, forty-one (41) were children and adolescents 20 years and below. The mortality rate among this age group was 0/41(0.0%) and morbidity of 2/41(4.9%). The prevalence of co-morbidities among the children and adolescents 20 years and below was 12/41(27.3%). Nearly one-third of the COVID-19 patients 20 years and below were asymptomatic (Table 1). Females were the majority constituting 24/41(58.5%).
In Table 1, most participants were symptomatic 30(73.2%), females 24(58.5%), Acholi 28(68.3%), Born-Again by religion 33(80.5%), attained a primary and secondary level of education 11(26.8%) respectively, students 23(56.1%) and from Gulu District 18(43.9%).
| Variables | Frequency (n=41) | Percent (%) |
|---|---|---|
| Symptomatic | 30 | 73.2 |
| Asymptomatic | 11 | 26.8 |
| Sex | ||
| Female | 24 | 58.5 |
| Male | 17 | 41.5 |
| Tribe | ||
| Acholi | 28 | 68.3 |
| Baganda | 1 | 2.4 |
| Basoga | 2 | 4.9 |
| Madi | 1 | 2.4 |
| Others | 9 | 22 |
| Religion | ||
| Catholics | 6 | 14.6 |
| Protestants | 2 | 4.9 |
| Others | 33 | 80.5 |
| The highest level of education | ||
| No education | 2 | 4.9 |
| Primary | 11 | 26.8 |
| Secondary | 11 | 26.8 |
| Certificate | 6 | 14.8 |
| Diploma | 2 | 4.9 |
| Others | 9 | 22 |
| Occupation | ||
| Business | 5 | 12.2 |
| Civil servants | 3 | 7.3 |
| Health worker | 4 | 9.8 |
| Peasant farmer | 6 | 14.8 |
| Others | 23 | 56.1 |
| Districts | ||
| Amuru | 4 | 9.8 |
| Gulu | 18 | 43.9 |
| Kitgum | 5 | 12.2 |
| Lamwo | 2 | 4.9 |
| Nwoya | 2 | 4.9 |
| Omoro | 3 | 7.3 |
| Pader | 2 | 4.9 |
| Others | 5 | 4.9 |
Note: In Table 1, most participants were symptomatic 30(73.2%), females 24 (58.5%), Acholi by tribe 28 (68.3%), Born-Again 33(80.5%), a primary and secondary level of education 11(26.8%), respectively, students 23(56.1%) and from Gulu district 18(43.9%).
Table 1: Characteristics of the COVID-19 among children and adolescents below 20 years in Gulu Regional Referral Hospital.
In Table 2, the mean duration of hospital stay was 14.44 days SD+10.45 at 95% CI: 11.14-17.74; the mean age of the participants was 18.2 years SD+1.95 at 95% CI: 17.51-18.74; the mean duration of symptoms at admission was 7.96 days SD+7.38 at 95% CI:4.84-11.07.
| Measurements | Duration of hospital stay (days) | Ages (years) | Duration of symptoms (days) |
|---|---|---|---|
| Mean | 14.44 | 18.2 | 7.96 |
| 95% Confidence Interval (CI) | 11.14-17.74 | 17.51-18.74 | 4.84-11.07 |
| Standard Error (SE) | 1.63 | 0.31 | 1.51 |
| 5% trimmed mean | 13.15 | 18.27 | 7.12 |
| Median | 13 | 19 | 7 |
| variance | 109.25 | 3.81 | 54.39 |
| Standard Deviation (SD) | 10.45 | 1.95 | 7.38 |
| Minimum | 2 | 13 | 1 |
| Maximum | 72 | 20 | 31 |
| Range | 70 | 7 | 30 |
| Interquartile range | 6 | 3 | 9 |
| Skewness | 4.36 | -0.99 | 1.82 |
| Standard Error | 0.37 | 0.37 | 0.47 |
| Kurtosis | 23.73 | 0.05 | 3.49 |
| Standard Error | 0.72 | 0.72 | 0.92 |
Note: In Table 2, the mean duration of hospital stay was 14.44 days SD + 10.45 at 95% CI: 11.14-17.74; the mean age of the participants was 18.2 days SD + 1.95 at 95% CI: 17.51-18.74; duration of symptoms 7.96 days SD + 7.38 at 95% CI:4.84-11.07.
Table 2: Distinct characteristics of the COVID-19 among children and adolescent patients treated at Gulu Regional Referral Hospital.
In Table 3, most participants did not present with the common symptoms of COVID-19, had a duration of symptoms between 1-7 days 17(41.5%), normal systolic blood pressure 18(43.9%), normal diastolic blood pressure 28(68.3%), normal body temperatures 27(65.9%), and normal oxygen saturation level on admission (SpO2) 29(70.7%).
| Variables | Yes (%) | No (%) | Odds Ratio | 95% CI |
|---|---|---|---|---|
| Fever | 10(24.4) | 31(75.6) | 1.084 | 0.254-4.630 |
| Cough | 17(41.5) | 24(58.5) | 1.551 | 0.432-5.570 |
| Tiredness | 4(9.8) | 37(90.2) | 2.286 | 0.217-24.082 |
| Body aches and pain | 8(19.5) | 33(80.5) | 1.228 | 0.251-6.017 |
| Sore throat | 6(14.6) | 35(85.4) | 0.667 | 0.117-3.788 |
| Vomiting | 1(2.4) | 40(95.1) | 0.958 | 0.882-1.042 |
| Diarrhea | 2(4.9) | 39(95.1) | 0.696 | 0.040-11.958 |
| Headache | 13(31.7) | 28(68.3) | 2.039 | 0.450-9.237 |
| Loss of taste | 2(6.7) | 39(95.1) | 0.933 | 0.848-1.027 |
| Loss of smell | 1(3.3) | 40(97.6) | 0.967 | 0.905-1.033 |
| Difficulty in breathing/shortness of breath/chest pain | 6(20.0) | 35(85.4) | 2.5 | 0.266-23.527 |
| Rashes on skin or discoloration of toes and fingers | 1(3.3) | 40(97.6) | 0.967 | 0.905-1.033 |
| Other Cardiovascular diseases (CVDs) | 3(7.3) | 38(92.7) | 1.455 | 0.121-17.462 |
| Hypertension | 3(7.3) | 38(92.7) | 1.455 | 0.121-17.462 |
| Asthma | 2(6.7) | 39(95.1) | 0.696 | 0.040-11.958 |
| HIV and AIDS | 1(3.3) | 40(97.6) | 0.958 | 0.882-1.042 |
| Other comorbidities | 3(7.3) | 38(92.7) | 1.455 | 0.121-17.462 |
| Duration of hospital stay (days) | ||||
| 1-7 days | 17(41.5) | |||
| 8-14 days | 1(2.4) | |||
| 15-21 days | 0(0.0) | |||
| >28 days | 1(3.3) | |||
| Others | 22(53.7) | |||
| Systolic Blood Pressure (mmHg) | ||||
| <120 | 14(34.1) | |||
| 121-140 | 18(43.9) | |||
| >140 | 5(12.2) | |||
| Missing data | 4(9.8) | |||
| Diastolic Blood Pressure(mmHg) | ||||
| <80 | 28(68.3) | |||
| 81-120 | 5(12.2) | |||
| >120 | 4(9.8) | |||
| Missing data | 4(9.8) | |||
| Body temperature (°C) | ||||
| < 37.2 | 27(65.9) | |||
| 37.3-38.9 | 2(4.9) | |||
| Missing data | 12(29.3) | |||
| Oxygen Saturation (SpO2) | ||||
| 80-96 | 3(7.3) | |||
| >96 | 29(70.7) | |||
| Others | 9(22.0) |
Note: In Table 3, most participants did not present with the common symptoms of COVID-19; had the duration of symptoms of 1-7 days 17(41.5%), normal systolic blood pressure 18(43.9%), normal diastolic blood pressure 28(68.3%), normal body temperature 27(65.9%), and normal oxygen saturation level of >96 at admission (SpO2) 29(70.7%).
Table 3: Clinical presentations in children and adolescent COVID-19 patients at Gulu Hospital.
In Table 4, most participants did not have co-morbidities. The commonest co-morbidities were other cardiovascular diseases 3/41(7.3%) and hypertension 3/41(7.3%) in different patients.
| Variables | Yes (%) | No (%) | Odds ratios | 95% CI |
|---|---|---|---|---|
| Asthma | 2(4.9) | 39(95.1) | 0.933 | 0.799-1.014 |
| Cancer | 0(0.0) | 41(100.0) | 0.967 | 0.905-1.033 |
| Diabetes mellitus | 0(0.0) | 41(100.0) | 0.967 | 0.905-1.034 |
| Chronic obstructive pulmonary diseases (COPDs) | 0(0.0) | 41(100.0) | 0.967 | 0.905-1.035 |
| Cardiovascular diseases | 3(7.3) | 38(92.7) | 0.933 | 0.799-1.014 |
| Hypertension | 3(7.3) | 38(92.7) | 0.933 | 0.799-1.014 |
| Obesity | 0(0.0) | 41(100.0) | 0.967 | 0.905-1.033 |
| HIV and AIDS | 1(2.4) | 40(97.6) | 0.9 | 0.799-1.014 |
| Epilepsy | 1(2.4) | 40(97.6) | 0.9 | 0.799-1.014 |
| Hepatitis B | 1(2.4) | 40(97.6) | 0.9 | 0.799-1.014 |
| Sickle cell disease | 1(2.4) | 40(97.6) | 0.9 | 0.799-1.014 |
Note: In Table 4, most participants did not have comorbidities. The commonest comorbidities were other cardiovascular diseases 3/41(7.3%) and hypertension 3/41(7.3%).
Table 4: Comorbidities in children and adolescent COVID-19 patients at Gulu Regional Hospital.
In Table 5, most participants did not develop complications of the SARS-CoV-2 infection; a tiny percentage developed pneumonia and acute liver injury at 1/44(3.3%) each, respectively.
| Variables (%) |
Yes(%) | No (%) |
|---|---|---|
| Depression | 0(0.0) | 41(100.0) |
| Nightmares | 0(0.0) | 41(100.0) |
| Multiple Organ Failure (MOF) | 0(0.0) | 41(100.0) |
| Acute Respiratory Failure (ARF) | 0(0.0) | 41(100.0) |
| Acute Cardiac failure (ACF) | 0(0.0) | 41(100.0) |
| Systemic Infections | 0(0.0) | 41(100.0) |
| Septic Shock | 0(0.0) | 41(100.0) |
| Disseminated intravascular Coagulation (DIC) | 0(0.0) | 41(100.0) |
| Blood clots | 0(0.0) | 41(100.0) |
| Acute Respiratory Distress syndromes (ARDS) | 0(0.0) | 41(100.0) |
| Acute kidney failure | 0(0.0) | 41(100.0) |
| Chronic fatigue | 0(0.0) | 41(100.0) |
| Pneumonia | 1(3.3) | 40(96.7) |
| Acute liver injury | 1(3.3) | 40(96.7) |
Note: In Table 5, most participants did not develop complications of the SARS-CoV-2 infection; a tiny percentage developed pneumonia and acute liver injury at 1/41(3.3%), respectively.
Table 5: Complications among the COVID-19 children and adolescent patients treated at Gulu Regional Referral Hospital.
In Table 6, there were no statistically significant associations between participants’ symptoms and co-morbidities as disaggregated by gender.
| Symptoms | Gender | Frequency (%) | Odds ratios at 95%CI |
|---|---|---|---|
| Headache | Males | 7(29.2) | 0.366(0.100-1.339) |
| Loss of taste | Males | 2(8.3) | 0.917(0.813-1.034) |
| Loss of smell | Males | 1(4.2) | 0.958(0.882-1.042) |
| Rashes on the skin or discoloration of the toes and nails | Males | 1(4.2) | 0.958(0.882-1.042) |
| Shortness of breath/difficulty in breathing and chest pain | Males | 4(16.7) | 0.933(0.180-4.838) |
| Other cardiovascular diseases (CVDs) | Males | 2(8.3) | 1.455(0.121-17.462) |
| Hypertension | Males | 2(8.3) | 1.455(0.121-17.462) |
| Asthma | Males | 1(4.2) | 0.696(0.040-11.958) |
| HIV and AIDS | Males | 2(8.3) | 0.958(0.882-1.042) |
| Other comorbidities | Males | 2(8.3) | 1.455(0.121-17.462) |
Note: In Table 6, there were no statistically significant associations between participants’ symptoms and comorbidities by gender.
Table 6: Characteristics of children and adolescent COVID-19 patients treated at Gulu Regional Referral Hospital by gender.
Table 7 describes the correlations between variables observed on children and adolescent COVID-19 patients treated at Gulu Regional Referral Hospital from March 2020 to October 2021.
| Variables | Cough | Tiredness | BAP | Diarrhea | Fever | Loss of smell | Other CVDs | Hypertension | HIV | Vitamin D | Systolic BP |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | 0.444(0.004) | 0.387(0.012) | 0.437(0.004) | 0.377(0.010) | |||||||
| Cough | 0.391(0.012) | 0.335(0.032) | 0.444(0.004) | ||||||||
| Tiredness | 0.391(0.012) | 0.668(0.000) | 0.387(0.012) | ||||||||
| Body aches and pains | 0.335(0.032) | 0.668(0.000) | 0.437(0.004) | ||||||||
| Sore throat | 0.382(0.014) | 0.414(0.007) | 0.414(0.007) | 0.382(0.014) | 0.381(0.014) | ||||||
| Vomiting | 0.698(0.000) | 0.278(0.078) | 0.563(0.000) | 0.563(0.000) | 0.307(0.064) | ||||||
| Diarrhea | 0.399(0.010) | 0.371(0.017) | 0.371(0.017) | ||||||||
| Loss of Taste | 0.698(0.000) | 0.371(0.017) | 0.371(0.017) | ||||||||
| Loss of smell | |||||||||||
| Rashes on the body | |||||||||||
| Difficulty in breathing | 0.499(0.001) | 0.348(0.026) | |||||||||
| DoS | 0.371(0.017) | 0.563(0.000) | -0.521(0.0009) | -0.401(0.014) | |||||||
| Other CVDS | 0.371(0.017 | 0.563(0.000) | 1.0(0.000) | ||||||||
| HIV and AIDs | |||||||||||
| Other comorbidities | 0.563(0.000) | ||||||||||
| Treatment with steroids | |||||||||||
| Treatment with Vitamin D | |||||||||||
| Treatment with Vitamin C | -0.307(0.051) | 0.563(0.000) | |||||||||
| Pneumonia | 0.321(0.041) | 0.563(0.000) | |||||||||
| Acute Liver Injury | 1.0(0.000) | 0.563(0.000) | 0.5639(0.000) | ||||||||
| Low Sp02 |
Note: DoS=Duration of hospital stay (days); CVDs=Other cardiovascular diseases; DIB=Difficulty in breathing; Sp02 Oxygen saturation at admission; BAP=General Body aches and pains.
Table 7a: Correlations between variables in children and adolescent COVID-19 patients treated at Gulu Regional Hospital.
| Variables | DIB | Vitamin C | Vomiting | Body Rashes | Other comorbidities | sore throat | Diastolic BP | Loss of taste | Pneumonia | Acute liver injury | DOS | Steroid |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | ||||||||||||
| Cough | ||||||||||||
| Tiredness | ||||||||||||
| Body aches and pains | ||||||||||||
| Sore throat | ||||||||||||
| Vomiting | 0.348(0.026) | -0.481(0.001) | ||||||||||
| Diarrhea | 0.499(0.001) | -0.307(0.051) | 0.698(0.000) | |||||||||
| Loss of Taste | 0.698(0.000) | 0.371(0.017) | ||||||||||
| Loss of smell | 0.382(0.014) | -0.412(0.011) | 0.698(0.000) | |||||||||
| Rashes on the body | 0.698(0.000) | |||||||||||
| Difficulty in breathing | 0.348(0.026) | 0.348(0.026) | ||||||||||
| DoS | 0.370(0.017) | 0.563(0.000) | 0.414(0.007) | -0.289(0.0083) | 0.371(0.017) | |||||||
| Other CVDS | 0.370(0.017) | 0.563(0.000) | 0.414(0.007) | 0.371(0.017) | 0.563(0.000) | 0.563(0.000) | ||||||
| HIV and AIDs | 0.382(0.014) | -0.521(0.009) | ||||||||||
| Other comorbidities | 0.37(0.017) | |||||||||||
| Treatment with steroids | -0.481(0.001) | |||||||||||
| Treatment with Vitamin D | 0.348(0.026) | 0.382(0.014) | ||||||||||
| Treatment with Vitamin C | -0.481(0.001) | 0.481(0.001) | ||||||||||
| Pneumonia | 0.348(0.026) | 0.382(0.014) | ||||||||||
| Acute Liver Injury | 0.563(0.000) | 0.382(0.014) | -0.412(0.011) | 0.689(0.000) | ||||||||
| Low Sp02 | 0.558(0.001) | 0.558(0.001) |
Note: DoS=Duration of hospital stay (days); CVDs=Other cardiovascular diseases; DIB=Difficulty in breathing; Sp02=Oxygen saturation at admission.
Table 7b: Table 7 describes the correlations between variables observed on children and adolescent COVID-19 patients treated at Gulu Regional Referral Hospital from March 2020 to October 2021.
Figure 1 is a systematic diagram showing how medical files were selected for the study.
In Figure 2, most <20-year-old COVID-19 patients treated at Gulu Regional Referral Hospital had a short hospital stay of 10-15 days.
In Figure 3, most <20-year-old COVID-19 patients presented early (1-7 days) to the hospital with coronavirus symptoms.
Discussion
In this study which covered the period from March 2020 to October 2021, there were forty-one children and adolescent COVID-19 patients less than 20 years out of six hundred and sixty-four patients 41/664(6.2%) who were treated for the COVID-19 at Gulu Regional Referral Hospital (Tables 1 and 2) (Figure 1). The most significant findings were that no mortality was reported among COVID-19 patients 20 years and below 0/41(0.0%), but the mortality rate among the adult population in this study cohort was 32/623(5.1%). The commonest morbidity observed among patients 20 years and below was pneumonia 1(3.3%) and acute live injury 1(3.3%), and this was lower compared to the adult population at 256/623(41.1%) (Tables 3-5).
Nearly one-third of the patients were asymptomatic (identified using contact tracing approach and self-referrals to the hospital), and the symptomatic cases presented with mild symptoms with dry cough 17(41.5%) and headache 13(31.7%) (Table 3).
The severe COVID-19 disease is usually shown by extreme difficulty in breathing and low oxygen saturation at admission. The severe form was not observed among the children and adolescents 20 years and below in this cohort (Table 3). This may explain the low rate of complications observed among this study population (Table 5). This finding has implications on how the Ugandan Ministry of Health could use this information to plan the response to the COVID-19 pandemic while preserving lives and at the same time saving the Ugandan economy [20,21]. For a long time, scholars and academicians in Uganda have argued for a complete re-opening of the economy, which has been affected by the lockdown measures instituted in March 2020 [20,21]. The current economic situation in Uganda following the two-year lockdown is worrying, and authors argue it should be lifted in a phased manner but quickly [20,21]. The population should be allowed to get back to work to rebuild the economy, evidently struggling [20,21].
Also, this study demonstrated that children and adolescents 20 years and below with COVID-19 treated at Gulu Regional Referral Hospital had very mild disease, with few complications and no mortality (Tables 1-7). Authors suggest that although there are many uncertainties about the mid-term and long-term consequences of the infection with the coronavirus, it would be desirable that the government opens its economy so that it does not get into more economic downfall. This finding is also suitable for Uganda because most Ugandans are young, below 30 years, and are the least affected by the COVID-19 [22]. Children and adolescents 20 years and below who get infected with the coronavirus develop a mild form and recover from the illness quickly (Figures 1 and 2).
The Authors have raised concerns about the short and long-term effects of COVID-19 on school performance and learning and suggest a formal and comprehensive study to determine this [23]. Authors were concerned that most COVID-19 patients 20 years and below were school-going children. Fears raised by many scholars and academicians on the impact of the disease on children’s education are genuine. They should be addressed in a formal study so that proper guidance based on evidence is provided to the Government of Uganda.
In addition, the most productive age group of the Ugandan population is those below 30 years, and the virus largely spares this group, as seen by the low prevalence of the disease in this age group (Figure 1 and Table 1). In this, authors have re-considered the rationale for the prolonged lockdown measures imposed on the most productive age group of the Ugandan population as counterproductive, leading to more economic turmoil. Instead, authors have suggested the “enhanced shielding approach” where the most vulnerable people (the elderly and those with comorbidities are isolated) as the most optimum approach for handling the COVID-19 situation in Uganda [21,22].
Authors have also urged the Ugandan government to stick to its model of managing the COVID-19; for example, maintaining strong leadership and simultaneous application of multiple public health measures as the best approach for handling the COVID-19 pandemic in Uganda now and in the future [24]. In addition, a regional approach to the containment of the virus should be enhanced and promoted whereby working closely with the East African regional leaders ensures that the virus is not spread from one country to another [24].
Also, most clinical presentations of the illness among children and adolescents 20 years and below were mild and short, between 1-7 days 17(41.5%) and with low symptom burden (Tables 1 and 2) (Figures 2 and 3). Similarly, their hospital stay was shorter than adults in the overall study population [18].
Moreover, prolonged illness was observed but was very infrequent 1/41(3.3%) and lower than for adults 86/601 (14.3%) (Table 2). The Authors found age not to correlate with illness duration overall among children and adolescents in this cohort (Tables 6 and 7). In this study population, children and adolescents with an illness duration of 28 days or more were few and contrasted with previous findings in adults in the United Kingdom [25]. This has implications on the duration patients spent in the hospital (hospital stay), which was usually short and allowed bed space for others to receive services at the COVID-19 treatment center. This information is essential as many hospitals in Uganda rarely experienced the exponential rise in the number of cases beyond the ability of the health systems to handle. The Ugandan health system's COVID-19 curve remained manageable, which was commendable for the Ugandan health managers.
In addition, a small percentage of the patients 20 years and below had comorbidities (Tables 4-7). The low prevalence of diabetes mellitus, cardiovascular diseases, and chronic obstructive pulmonary diseases had perhaps influenced treatment outcomes among this age group. This is important for the country because this age group could engage in economic activities with limited restrictions to allow the country’s economy to remain afloat.
Additionally, more public health approaches, vaccination, wearing facemasks in public settings, and reduction in congregate settings could be applied to ensure that the spread of the virus is limited in the Ugandan populations. Authors have argued that extreme care should shield elders and those with co-morbidities from the general population. This is also in line with the findings that about one-fourth of the children and adolescents with COVD-19 were asymptomatic (Table 1). This implies their interaction with those at high risks, such as the elderly and those with co-morbidities, should be limited in the Ugandan settings.
Authors suggest that the Ugandan Ministry of Health should design a strategy to have the young people continue their economic activity and, at the same time, reduce the chances of spreading the COVID-19 to the high-risk groups. A formal and comprehensive analysis of the home set up in Uganda and how young people 20 years and below could be prevented from spreading the virus to the elderly may be an ideal approach from now on.
Authors have also found that most COVID-19 patients 20 years and below in our cohort were females (Table 1). However, there was no statistically significant gender difference in the occurrence of the coronavirus in this study population (Table 3). The finding is different in the adult population in our previous study, where a statistically significant gender difference and more mortality were observed among females [18]. In that study, females had more co-morbidities, such as HIV and AIDS, cardiovascular diseases, and chronic obstructive pulmonary diseases, compared to males. These were thought to be the driving factors in the higher mortality rates among females than males in the study population [18].
The absence of gender difference among the 20-year and below perhaps underpins the importance of the age factor in guaranteeing gender uniformity among the COVID-19 patients in this study population (Table 3). In addition, the low prevalence of co-morbidities among this age group may partly explain the observation among the cohort since there was no substantial gender difference (clinical presentations and socio-demographic characteristics) among this age group (Table 6).
Furthermore, the authors found that in contrast to other respiratory viruses, children have less severe symptoms when infected with the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [26-28]. In the literature reviews, the authors were persuaded by arguments on the proposed hypotheses for the age-related differences in the severity of coronavirus disease 2019 (COVID-19). Factors proposed to explain the difference in the severity of COVID-19 in children and adults include those that put adults at higher risk and those that protect children. These include: (i) age-related increase in endothelial damage and changes in clotting function; (ii) higher density, increased affinity, and different distribution of angiotensin-converting enzyme two receptors and transmembrane serine protease 2; (iii) pre-existing coronavirus antibodies (including antibody-dependent enhancement) and T cells; (iv) immunosenescence and inflammation, including the effects of chronic cytomegalovirus infection; (v) a higher prevalence of co-morbidities associated with severe COVID-19 and (vi) lower levels of vitamin D in adults compared to children and adolescents [26-28].
In the hypotheses, it is further proposed that factors that might protect children include the following: (i) differences in innate and adaptive immunity; (ii) more frequent recurrent and concurrent infections; (iii) pre-existing immunity to coronaviruses; (iv) differences in microbiota; (v) higher levels of melatonin; (vi) protective off-target effects of live vaccines and (vii) lower intensity of exposure to SARS- CoV-2 [26-28].
In summary, the authors argue that the low prevalence, co- morbidities, symptoms burden, complications, and mortality of COVID-19 among children and adolescents 20 years and below in Northern Uganda is a blessing for the country. The Ugandan Bureau of Statistics reports show that 52.6% of the Ugandan population is below 20 years [22]. This is the most productive age group that could help drive the Ugandan economy forward after the lockdown if limited restrictions on their economic activities were accorded. Strengths and limitations of this study: This study was a retrospective review of HMIS datasets from the COVID-19 medical records of Gulu Regional Referral Hospital. The period of the evaluation was from March 2020 to October 2021. The study has limitations on how Gulu Regional Referral Hospital handled records and record keeping. In addition, vital information, for example, weight, height, and BMI of COVID-19 patients, was not recorded due to the emergency handling of the cases at the beginning of the pandemic in March 2020. The missing variables in the Gulu Hospital HMIS records excluded some files from participating in this study. In this, authors have suggested a need for a prospective or longitudinal assessment of the COVID-19 cases in the future, ensuring that all data were measured and recorded accordingly.
This data is vital as it is one of the well-documented completed data for over 664 cases of COVID-19 treated in a Regional Referral Hospital in Uganda. In this cohort, forty-one were children and adolescents twenty years and below, with no reported mortality and very few morbidities. Findings from this study show tremendous and good clinical practices at Gulu Regional Referral Hospital despite the challenges faced during the pandemic.
Generalization of the data from this study: These findings should be cautiously interpreted and generalized only to Regional Referral Hospitals in Uganda. However, this data could be similarly observed in many hospitals in African countries with low-resource settings.
Conclusion
Data showed excellent treatment outcomes of the COVID-19 among children and adolescents 20 years and below in Northern Uganda with a recovery rate of 100.0%. The burden of symptoms of the illness, co-morbidities, and complications was fewer. There is a need to conduct more extensive studies on the role played by age in the successful recovery of COVID-19 patients, even in a low-resource environment.
Declarations
Ethics approval and consent to participate
The Gulu Regional Referral Hospital Institutional and Ethics Committee approved this study. In addition, the study was conducted following all relevant institutional guidelines and regulations.
Availability of data and materials: All datasets supporting the conclusion in this article are within this article, and more information is accessible by a reasonable request to the corresponding author.
Competing interests: All authors declare no conflict of interest.
Funding
Most funding for this study was the contribution of individual research members of the Uganda Medical Association (UMA) Acholi branch.
Authors’s Contributions
DLK, JNO, JA, SB, CO, LO, ENI, and FWDO participated in designing the study, SB and DLK were responsible for data abstraction supervision, BS, JA, LO, and DLK were responsible for data analysis, interpretation, writing, and CO, NAO, JA, DA, JNO, LO, FWDO, for revising the manuscript.
Acknowledgment
We acknowledge with many thanks to the support from the administration of Gulu Regional Referral Hospital for the information obtained. Dr. Laban Oketcho, Dr. Anek Janet Schola, Dr. Baguma Steven, and Mr. Dominic Ogwal Savio for the well-collected data from the archives of Gulu Regional Referral Hospital. We also thank Mr. Lawence Obalim for the data analysis well conducted. In addition, financial support from UMA Acholi branch members, which enabled the team to conduct this study successfully, is most appreciated. In honor of our two fallen colleagues (Co- authors), Dr. Paska Layet and Dr. Oola Janet, may their souls rest in peace!
References
- (2020) World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19.
- Ludvigsson JF (2020) A systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr.
[Crossref] [Google Scholar] [Pub Med]
- Worldometer(2020) COVID-19 Coronavirus Pandemic.
- Mayoclinic (2020) COVID-19 (coronavirus) in babies and children.
[Crossref] [Google Scholar] [Pub Med]
- Health MoP. Coronavirus Disease (COVID-19 2021).
- Badran S (2021) An evidence base for school health policy during the COVID-19 pandemic. Health Behav 8:40-47.
- Dong Y, Mo X, Hu Y, Qi X, Jiang F, et al. (2020) Epidemiology of COVID-19 among children in China. Pediatrics 145(6).
[Crossref] [Google Scholar] [Pub Med]
- Lee PI (2020) Are children less susceptible to COVID-19? J Microbiol Immunol Infect 53:371.
[Crossref] [Google Scholar] [Pub Med]
- Petter B (2020) Why is COVID‐19 so mild in children. Acta Paediatrica 109.
[Crossref] [Google Scholar] [Pub Med]
- Centers for Disease Control and Prevention (2020) COVID-19 in Children and Teens.
- Ludvigsson JF (2020) A systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica 109:1088-1095.
[Crossref] [Google Scholar] [Pub Med]
- World Health Organization
- Esposito S, Principi N (2020) School closure during the coronavirus disease 2019 (COVID-19) pandemic: an effective intervention at the global level?. JAMA pediatr. 174:921-922.
[Crossref] [Google Scholar] [Pub Med]
- Chang SL, Harding N, Zachreson C, Cliff OM, Prokopenko M (2020) Modelling transmission and control of the COVID-19 pandemic in Australia. Nat Commun. 11:1-3.
[Crossref] [Google Scholar] [Pub Med]
- Viner RM, Mytton OT, Bonell C, Melendez-Torres GJ, Ward J, Hudson L, et al. (2021) Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: A systematic review and meta-analysis. JAMA pediatr 175:143-156.
[Crossref] [Google Scholar] [Pub Med]
- Yonker LM, Neilan AM, Bartsch Y, Patel AB, Regan J, et al. (2020) Pediatric severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Clinical presentation, infectivity, and immune responses. J Pediatr. 227:45-52.
[Crossref] [Google Scholar] [Pub Med]
- Molteni E, Sudre CH, Canas LS, Bhopal SS, Hughes RC, et al. (2021) Illness duration and symptom profile in symptomatic UK school-aged children tested for SARS-CoV-2. Lancet Child Adolesc Health. 5:708-718.
[Crossref] [Google Scholar] [Pub Med]
- Okot C, Baguma S, Onira NA, Agings WO, Arwinyo B, et al. Characteristics of the COVID-19 patients treated at Gulu Regional Referral Hospital, Northern Uganda: A cross-sectional study. Research Square.
- Baguma S, Okot C, Onira NA, Apiyo P, Layet P, et al. (2021) Factors associated with mortality among the COVID-19 patients treated at Gulu Regional Referral Hospital: A retrospective study. Research Square.
- Kitara DL, Ikoona EN (2020) Proposed strategies for easing COVID-19 lockdown measures in Africa. Pan Afr Med J 36:10.
[Crossref] [Google Scholar] [Pub Med]
- Ikoona EN, Kitara DL (2021) A proposed framework to limit post-lockdown community transmission of COVID-19 in Africa. Pan Afr Med J. 38.
[Crossref] [Google Scholar] [Pub Med]
- UBOS (Uganda Bureau of Statistics) (2020) Uganda Bureau of Statistics 2020 statistical analysis.
- Ludvigsson JF (2021) Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta Paediatr 110: 914-921.
[Crossref] [Google Scholar] [Pub Med]
- Kitara DL, Ikoona EN (2020) COVID-19 pandemic, Uganda’s story. Pan Afr Med J 35.
[Crossref] [Google Scholar] [Pub Med]
- Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, et al. (2021) Attributes and predictors of long COVID. Nat Med. 27:626-631.
[Crossref] [Google Scholar] [Pub Med]
- Grifoni A, Sidney J, Zhang Y, Scheuermann RH, Peters B, Sette A (2020) Sequence homology and bioinformatic approach can predict candidate targets for immune responses towards CoV-2. Cell Host Microbe 27:671-680.
[Crossref] [Google Scholar] [Pub Med]
- Shao X, Guo X, Esper F, Weibel C, Kahn JS (2007) Seroepidemiology of group I human coronaviruses in children. J Clin Virol 40:207-213.
[Crossref] [Google Scholar] [Pub Med]
- Petra Zimmermann, Nigel Curtis (2021) Why is COVID-19 less severe in children? A review of the proposed mechanisms underlying the age-related difference in the severity of SARS-CoV-2 infections. Arch Dis Childm106:429-439.
[Crossref] [Google Scholar] [Pub Med]
Citation: Aloyo J, Acullu D, Alema NO, Baguma S, Okot C, et al. (2022) Distinct Characteristics of the COVID-19 among Children and Young Adolescents Treated at Gulu Regional Referral Hospital; Northern Uganda: A Cross-Sectional Study. J Infect Dis Ther S1:003. DOI: 10.4173/2332-0877.22.S1.003.
Copyright: © 2022 Aloyo J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2687
- [From(publication date): 0-2022 - Nov 21, 2025]
- Breakdown by view type
- HTML page views: 2069
- PDF downloads: 618