Distal Posterior Cerebral Artery Aneurysm Treatment
Received: 31-Oct-2022 / Manuscript No. roa-22-82179 / Editor assigned: 02-Nov-2022 / PreQC No. roa-22-82179 (PQ) / Reviewed: 16-Nov-2022 / QC No. roa-22-82179 / Revised: 18-Nov-2022 / Manuscript No. roa-22-82179 (R) / Published Date: 25-Nov-2022 DOI: 10.4172/2167-7964.1000411
Image Article
Aneurysm of the distal back cerebral vein is a rare and challenging condition to treat due to its characteristics, extensive physical area, and comprehensive neuroanatomical designs. Distal PCA aneurysms can be treated with careful cutout, parent vessel obstruction (PVO), or endovascular treatment. Endovascular the board with stream diverter stents is one of these, and its use has increased recently with positive outcomes. In this review, we discuss our specific thoughts regarding the Pipeline embolization device (PED) treatment of a P3 aneurysm.
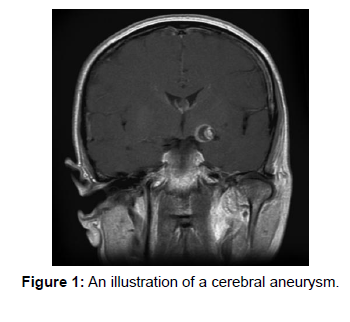
Although distal back cerebral supply route (PCA) aneurysms are fascinating substances, their extensive anatomic area, intricate neuro anatomic designs, and higher prevalence of fusiform and large saccular aneurysms make them difficult to treat. Despite their connection to other vasculopathies like vasculitis, AVMs, and Moyamoya, saccular aneurysms are more likely to rupture in the beginning, which is unstable due to a faster rate of dilatation and drainage. Endovascular treatment is now the most common form of treatment out of all the options for administration. The development of stream diverters in recent years has led to an increase in their use in the treatment of various aneurysms, including PCA. The Pipeline embolization device’s off the shelf use in the treatment of distal PCA aneurysms is the subject of our in-depth review (Figure 1).
PCA aneurysms address a fascinating and provocative condition to treat. When compared to cerebral aneurysms elsewhere, they will typically have distinct characteristics, such as a preference to include proximal fragments (P1 and P2), a higher frequency of fusiform and enormous saccular aneurysms, a greater likelihood of saccular aneurysms breaking apart in the beginning, which are unstable with a higher rate of dilatation and discharge, and a relationship with other vasculopathies like vasculitis, AVM and Moyamoya [1-4].
References
- Goehre F, Jahromi BR, Hernesniemi J, Elsharkawy A, Kivisaari R, et al. (2014) Characteristics of posterior cerebral artery aneurysms: an angiographic analysis of 93 aneurysms in 81 patients. Neurosurgery 75: 134-144.
- Kobkitsuksakul C, Somboonnitiphol K, Apirakkan M, Lueangapapong P, Chanthanaphak E (2020) Dolichoectasia of the internal carotid artery terminus, posterior communicating artery, and posterior cerebral artery: The embryonic caudal ramus internal carotid segmental vulnerability legacy. Interv Neuroradiol 26: 124-130.
- Hou K, Lv X, Yu J (2022) Endovascular Treatment of Posterior Cerebral Artery Trunk Aneurysm: The Status Quo and Dilemma. Front Neurol 12: 746525.
- Ciceri EF, Klucznik RP, Grossman RG, Rose JE, Mawad ME (2001) Aneurysms of the posterior cerebral artery: classification and endovascular treatment. AJNR Am J Neuroradiol 22: 27-34.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Sharma P (2022) Distal Posterior Cerebral Artery Aneurysm Treatment. OMICS J Radiol 11: 411. DOI: 10.4172/2167-7964.1000411
Copyright: © 2022 Sharma P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1675
- [From(publication date): 0-2022 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 1353
- PDF downloads: 322