Disseminated Cryptococcal Disease of the Bone Marrow, Cerebrospinal Fluid and Blood in an ART-Naive Patient with Advanced HIV: A Case Report
Received: 20-Mar-2017 / Accepted Date: 20-Apr-2018 / Published Date: 25-Apr-2018 DOI: 10.4172/2476-2024.1000139
Abstract
Background: Cryptococcosis affects 10-30% of patients with acquired immunodeficiency syndrome (AIDS) resulting in significant morbidity and mortality. The primary sites of cryptococcal disease are the lung and central nervous system with bone marrow involvement being rare.
Case presentation: This case report describes a human immunodeficiency virus (HIV) positive, anti-retroviral therapy (ART) naïve female with pancytopenia who demonstrated no significant symptoms nor clinical signs as well as a negative serum cryptococcal antigen (CrAg) test. A bone marrow biopsy was then performed which resulted in a diagnosis of disseminated cryptococcal disease of the bone marrow. Blood and cerebrospinal fluid (CSF) fungal cultures confirmed the presence of Cryptococcus neoformans. The patient was then successfully treated with antifungal agents-amphotericin B and fluconazole.
Conclusion: Bone marrow examination may therefore be a useful method in early diagnosis of disseminated cryptococcosis as a cause of cytopenias in immunocompromised patients, thus enabling early appropriate treatment and improved outcomes.
Keywords: Cryptococcus; Bone marrow; Human immunodeficiency virus; Acquired immunodeficiency syndrome
Abbreviations
HIV: Human Immunodeficiency Virus; AIDS: Acquired Immunodeficiency Syndrome; CrAg: Cryptococcal Antigen; ART: Anti-Retroviral Therapy; CSF: Cerebrospinal Fluid; MGG: May-Grünwald Giemsa; H&E: Haematoxylin and Eosin; PAS: Periodic Acid–Schiff; GMS: Grocott’s Methenamine Silver
Background
Fungal infections are among the most common opportunistic infections in human immunodeficiency virus (HIV) positive patients [1]. Cryptococcal disease affects 10-30% of patients with acquired immunodeficiency syndrome (AIDS) and causes significant morbidity and mortality [2]. The primary sites of cryptococcal disease are the lung and central nervous system with bone marrow involvement being rare. [3,4] This is a case report of disseminated cryptococcal disease of the bone marrow in a HIV positive female who presented with pancytopenia.
Case Presentation
A 25 year old female patient was referred from a local clinic and admitted to Groote Schuur Hospital, medical department, on 08/11/2016 for evaluation of a one-month history of pancytopenia.
The patient demonstrated no significant symptoms on presentation with normal respiratory and neurological examinations and no clinical source of infection. She was known to be HIV positive with a CD4 count of 44 cells/µL and a viral load of 73,596 RNA copies/mL. A negative serum cryptococcal antigen (CrAg) test was detected on reflex screening. She was anti-retroviral therapy (ART) naïve. The patient’s blood test parameters are listed below in Table 1.
| Blood Test | Result | Reference Range | |
|---|---|---|---|
| Full blood count | Total white cell count (× 109/L) | 3.02 ↓ | 3.90-12.60 |
| Haemoglobin (g/dL) | 7.7 ↓ | 12.0-15.0 | |
| Mean corpuscular volume (fL) | 88.2 | 78.9-98.5 | |
| Mean corpuscular haemoglobin (pg) | 31.3 | 26.1-33.5 | |
| Platelets (× 109/L) | 52 ↓ | 186-454 | |
| Differential count | Neutrophils (× 109/L) | 2.44 | 1.60-8.30 |
| Lymphocytes (× 109/L) | 0.38 ↓ | 1.40-4.50 | |
| Monocytes (× 109/L) | 0.13 ↓ | 0.20-0.80 | |
| Reticulocyte count | Absolute reticulocyte count (× 1012/L) | 0.017 ↓ | 0.050-0.100 |
| Corrected reticulocyte count (%) | 0.33 ↓ | 0.50-2.00 | |
| Reticulocyte production index | 0.2 ↓ | 1-2 | |
| Iron studies | Serum iron (µmol/L) | 2.6 ↓ | 9.0-30.4 |
| Transferrin (g/L) | 0.99 ↓ | 2.00-3.60 | |
| Transferrin saturation (%) | 10 ↓ | 15-50 | |
| Ferritin (µg/L) | 491 ↑ | 13-150 |
Table 1: Blood test parameters of patient.
The peripheral blood smear showed normocytic normochromic red cells with rouleaux formation, vacuolated neutrophils and reactive lymphocytes. Electrolytes, renal function and liver function tests were all within normal limits. Blood cultures (bacterial, mycobacterial/fungal) were done. A lumbar puncture was also performed with cerebrospinal fluid (CSF) submitted for cultures. However no CSF CrAg test was requested.
The next day, on 09/11/2016, the patient was referred to haematopathology for a bone marrow biopsy to investigate the cause of the pancytopenia. Bilateral bone marrow aspirates and trephines were obtained using an 11 gauge bone marrow needle. Aspirate slides were stained with May-Grünwald Giemsa (MGG) and the trephine with haematoxylin and eosin (H&E).
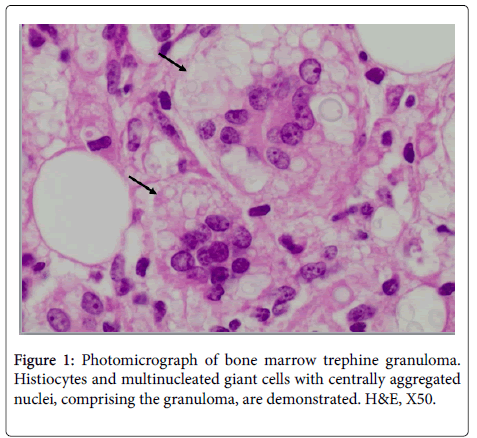
The aspirate demonstrated hypocellular particles surrounded by proteinaceous haloes with gelatinous transformation. Haemopoiesis revealed trilineage hypocellularity with mild dysplasia of all three cell lines. The myeloid:erythroid (M:E) ratio was 9:1. The trephine was hypocellular, estimated at 55%, with trilineage hypocellularity. The architecture was disrupted by multiple granulomas of various sizes, with the largest measuring approximately three quarters of a 50 × high power field. These granulomas comprised of histocytes and multinucleated giant cells, with centrally aggregated nuclei (Figure 1).
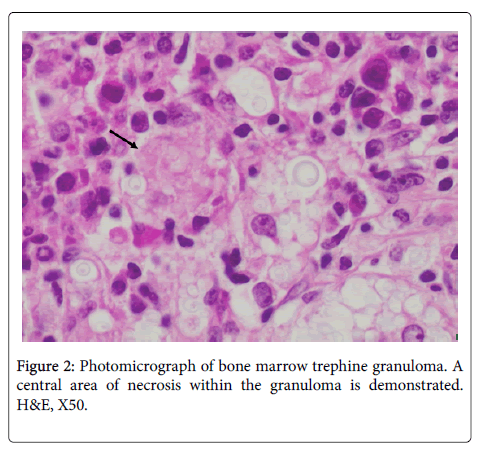
The granulomas also demonstrated central areas of necrosis (Figure 2). Numerous phagocytosed, spherical, encapsulated microorganisms surrounded by haloes were observed in clusters within the granulomas as well as scattered interstitially, which were morphologically consistent with Cryptococcus (Figure 3).
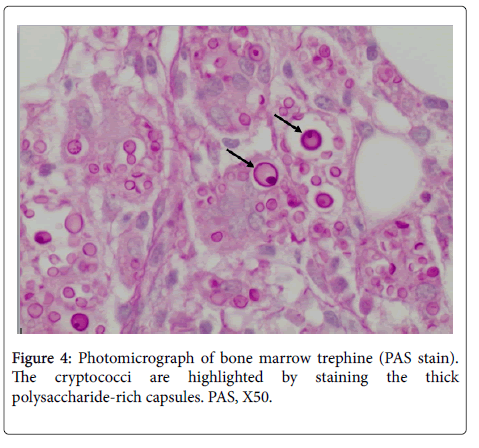
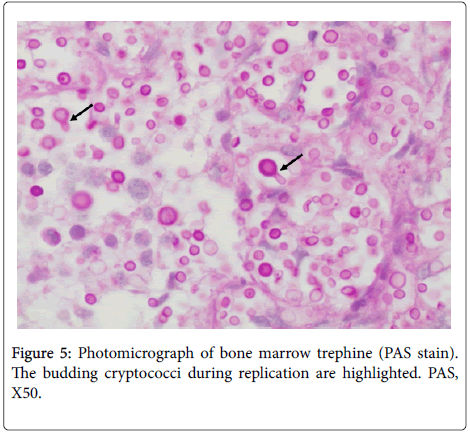
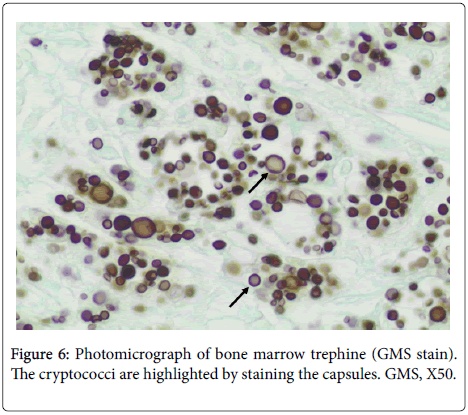
Periodic acid-Schiff (PAS) and Grocott’s methenamine silver (GMS) stains were performed which highlighted the cryptococci within histiocytes that occurred in aggregates forming the granulomas as well as in single histiocytes interstitially (Figures 4-6).
A Ziehl-Neelsen stain was also performed which excluded acid-fast bacilli.
A diagnosis of disseminated cryptococcal disease of the bone marrow was made, on 11/11/2016, based on morphological and histochemical evidence. The dysplastic changes noted on the aspirate were concluded to be associated with retroviral disease. Subsequently, on 13/11/2016, the patient’s blood and CSF fungal cultures were both found to be positive for Cryptococcus neoformans.
The patient commenced treatment with antifungal agents on the day of the bone marrow diagnosis according to the Southern African HIV Clinicians Society guideline 2013 update for cryptococcal meningitis, which included an induction phase of intravenous amphotericin B 50 mg/day+oral fluconazole 800 mg/day for 2 weeks. A repeat fungal blood culture was performed after this induction phase which yielded a negative result. Thereafter, she was discharged and referred to her local ART clinic for continuation of fluconazole as well as ART initiation.
On 09/12/2016, 4 weeks after starting antifungal therapy, the patient was initiated onto first line ART which consisted of tenofovir 300 mg+emtricitabine 200 mg+efavirenz 600 mg as a fixed-dose combination. The antifungal therapy continued with the consolidation phase of oral fluconazole 400 mg/day for 8 weeks and finally a maintenance phase of oral fluconazole 200 mg/day. One year after the start of cryptococcal treatment, on 14/11/2017, the final phase of fluconazole was discontinued after the patient had maintained two consecutive CD4 counts of 264 cells/µL and 307 cells/µL, taken 6 months apart, with a suppressed HIV viral load. Her full blood count had also completely normalized at this stage.
Discussion
Fungal infections are among the most common opportunistic infections in patients infected with HIV. Cryptococcal disease affects 10-30% of patients with AIDS and causes significant morbidity and mortality [1,2]. Principal sites of cryptococcal disease are the lung and central nervous system [3]. Involvement of the bone marrow is rare [4]. Disseminated cryptococcosis is defined as the demonstration of Cryptococcus in blood, sterile body fluids, or tissues other than pulmonary tissue [5].
Cryptococcal disease is caused by two pathogenic species-complexes namely Cryptococcus neoformans and Cryptococcus gattii both of which collectively comprise of seven clade species [6]. Cryptococcus neoformans is an encapsulated yeast that grows and replicates by budding. It is acquired from inhalation of fungal spores or acapsular yeast cells in the environment, particularly from fungi-laden pigeon droppings [3]. Once inside the host, the yeast can change the composition and size of the capsule to increase its chances of resisting or eluding the host’s defence mechanisms [7]. Its morphology is characterized by a spherical to oval shape of variable sizes ranging from 5-10 µm surrounded by a distinct halo and thick capsule; and demonstrates narrow-based budding. PAS and GMS stains allow for better visualisation of these organisms by staining the thick polysaccharide-rich capsules [3].
Cryptococcosis stimulates a granulomatous response in most cases despite immunosuppression. The number of organisms is inversely proportional to the adequacy of the granulomatous response [4]. The granulomatous response is, in turn, dependent on the CD4 count [8]. Cryptococci in the marrow may result in cytopenias by acting in synergy with the HIV; activating macrophages which suppress erythroid progenitor cell development; and by cryptococcal-associated haemophagocytosis [4,9,10].
The Southern African HIV Clinicians Society guideline 2013 update for cryptococcal meningitis recommends that HIV-infected adults with a CD4 count less than 100 cells/µl be screened for cryptococcal antigenaemia. This screening may be done by reflex laboratory or clinician-initiated testing. With regards to the latter, screening should be restricted to ART-naïve adults with a CD4 count less than 100 cells/µl and no prior cryptococcal meningitis. The screening test, performed on serum or plasma, should be a rapid CrAg test - either latex agglutination test or lateral flow assay. For patients suspected of first episode cryptococcal meningitis, a lumbar puncture should be performed and CSF submitted for a rapid test (preferably CrAg test) as well as a fungal culture [11].
Conclusion
Bone marrow examination may be a useful method of diagnosing invasive opportunistic fungal infections such as cryptococcosis as a cause of cytopenias in immunocompromised patients with a negative serum CrAg test, however a CSF CrAg test may have also been useful in this case. This may lead to early diagnosis and treatment thereby decreasing the morbidity and mortality of AIDS patients.
Teaching Points
• Cryptococcal screening with the serum/plasma CrAg test in HIV-infected adults with a CD4 count<100 cells/µl and pre-emptive antifungal treatment, for early detection and treatment of cryptococcal disease, is recommended for routine implementation in South Africa.
• For suspected first episode cryptococcal meningitis, CSF should be obtained and submitted for both a CrAg test and fungal culture.
• Bone marrow examination may be a useful method in early diagnosis of disseminated cryptococcosis in immunocompromised patients with cytopenias and a negative serum CrAg test.
• Disseminated cryptococcal disease of the bone marrow stimulates a granulomatous response despite immunosuppression.
The cryptococci in the marrow cause cytopenias by:
• Acting in synergy with the HIV.
• Activating macrophages which suppress erythroid progenitor cell development.
• Cryptococcal-associated haemophagocytosis.
Declarations
Ethics approval and consent to participate
According to the University of Cape Town, Faculty of Health Sciences, Human Research Ethics Committee-Definition of Health Research and Human Participants Standard Operating Procedure: “Single case reports (≤ 3 patients). Since a single case report does not produce generalizable knowledge it does not meet the definition of research requiring Human Research Ethics Committee approval.”
Consent for publication
Written informed consent to publication of a written case report has been obtained from the patient and is available for review by the editors of this journal.
Availability of data and material
Not applicable.
Conflict of Interest
The authors declare that they have no competing interests.
Funding
There are no sources of financial support that facilitated conduct of the work described in this manuscript or the writing of the manuscript itself.
Authors’ Contributions
Sumaiya Cassim performed the bone marrow biopsy, collected the data, contributed to histological examination of the bone marrow, and was the major contributor in writing the manuscript.
Monalisa Ntobongwana was a major contributor to histological examination of the bone marrow and making the pathological diagnosis. All authors have read and approved the final manuscript.
References
- Spencer PM, Jackson GG (1989) Fungal and mycobacterial infections in patients infected with the human immunodeficiency virus. J Antimicrob Chemother 23: 107-125.
- Perfect JR, Dismukes WE, Dromer F (2010) Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of America. Clin Infect Dis 50: 291-322.
- Guarner J, Brandt ME (2011) Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev 24: 247-280.
- Pantanowitz L, Omar T, Sonnendecker H, Karstaedt AS (2000) Bone marrow cryptococcal infection in the acquired immunodeficiency syndrome. J Infect 41: 92-94.
- Taneja J, Bhargava A, Loomba P, Dogra V, Thakur A, et al. (2008) Cryptococcal granulomas in an immunocompromised HIV-negative patient. Indian J Pathol Microbiol 51: 553-555.
- Hagen F, Lumbsch HT, Arsenijevic VA (2017) Importance of resolving fungal nomenclature: the case of multiple pathogenic species in the Cryptococcus genus. mSphere 2: 1-13.
- Gupta G, Fries BC (2010) Variability of phenotypic traits in Cryptococcus varieties and species and the resulting implications for pathogenesis. Future Microbiol 5: 775-787.
- Hill Jo (1992) CD4+ T cells cause multinucleated giant cells to form around Cryptococcus neoformans and confine the yeast within the primary site of infection in the respiratory tract. J Exp Med 175: 1685–1695.
- Pendle S, Sacks LV (1998) Pancytopenia in a patient with Cryptococcus meningitis. S Afr Med J 88: 1011.
- Roodman GD (1987) Mechanisms of erythroid suppression in the anemia of chronic disease. Blood Cells 13: 171-184.
- Govender NP, Meintjes G, Bicanic T (2013) Guideline for the prevention, diagnosis and management of cryptococcal meningitis among HIV-infected persons: 2013 update by the Southern African HIV Clinicians Society. S Afr J HIV Med 14: 76-86.
Citation: Cassim S, Ntobongwana M (2018) Disseminated Cryptococcal Disease of the Bone Marrow, Cerebrospinal Fluid and Blood in an ART-Naïve Patient with Advanced HIV: A Case Report. Diagn Pathol Open 3: 139. DOI: 10.4172/2476-2024.1000139
Copyright: © 2018 Cassim S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 7678
- [From(publication date): 0-2018 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 6956
- PDF downloads: 722