Disruption in Healthcare Services: Drawing Scenarios from Individual Healthcare during COVID-19
Received: 10-Mar-2023 / Manuscript No. JCMHE-23-91353 / Editor assigned: 13-Mar-2023 / PreQC No. JCMHE-23-91353 (PQ) / Reviewed: 27-Mar-2023 / QC No. JCMHE-23-91353 / Revised: 07-Jun-2023 / Manuscript No. JCMHE-23-91353 (R) / Published Date: 14-Jun-2023
Abstract
This study uncovers the disruptions in healthcare services of three distinct time stamps on individual healthcare services during COVID-19. Descriptive analysis was followed to understand various patterns in healthcare service disruptions. Logistic regression and Chi-square statistics were also followed to examine associations among three explanatory variables; age, sex and area of residency. Findings show, preventive routine healthcare, heart disease and lack of money were the most prominent issues in individual healthcare. Female (OR: 0.91, 95% CI: 0.87-0.94) and age group 26 to 35 (OR: 0.89, 95% CI: 0.80-0.98) significantly sought for healthcare urgency in all time periods. Suburban people required more medical attention for all the timelines (OR: 0.83, 95% CI: 0.80-0.87) and (OR: 0.88, 95% CI: 0.81-0.95) correspondingly. Geographically all the healthcare related descriptive variables were highly quantified in South African regions. The identification of required healthcare requirements and possible reasons for interruption can help to devise more effective mechanisms to address these two global health crisis issues during the period of chaos or any future pandemic.
Keywords: Healthcare; Individual healthcare service; Disruptions; COVID-19; Prominent issues
Introduction
COVID-19, as of February, 2021, has caused close to 6 million deaths worldwide with new variants and as a result of soaring number of infected cases, simultaneously, has shrunk the capacity of hospitals and healthcare systems globally [1]. Due to the strained conditions, in means of lockdowns and stay at home, hospital facilities and major healthcare services are out of reach for individuals. As a result, individuals are deprived of much needed healthcare attentions including child vaccination and other crucial medical attentions like life expanding cancer alleviative interventions [2-4]. In some cases, necessary health services like surgery, cancer treatment and dialysis have been delayed. Other medical and health service fields like major organ transplantation have also been observed in paucity of delivering desired care in terms of reduction in the number of beds in intensive care unit [5]. Urgent medical attention for example, urology patients with malignant disease were also in apprehension due to COVID-19. In this regard, lower income countries are facing greatest disruption to healthcare services and reduction of services is also conspicuous where the pandemic is most vivacious [6-8]. On top of that, in the case of child vaccination and health services estimation predicts that absence and reduction to crucial maternal and child healthcare services may trigger additional more than a million child deaths. It is worthy to mention that, health systems in the past during epidemics have also struggled and encountered similar disruption in service utilization and maintain routine services [9]. In general, health service crisis emerges as people, efforts and medical supplies are steered in emergency responses and a vacuum creates in basic regular health services unrelated to epidemic. Studies highlight that some plausible reasons for reduction in healthcare services during the Ebola epidemic were fear of contracting the Ebola virus, rumors and distrust. Prior experience from Taiwan, during the 2003 respiratory syndrome epidemic, unveiled that inpatient care and ambulatory care were reduced by more than 35% and 23% respectively [10]. COVID-19 pandemic is already disrupting healthcare services and utilization in the form of distorting Reproductive, Maternal, Newborn and Child Health (RMNCH) services. The global supply chain of pharmaceuticals and medical equipment is also disrupted due to COVID-19.
Expected disruptions to individual healthcare services, child and maternal healthcare services remain high for low middle income countries and in this regard WHO provided guidelines in maintaining essential healthcare services [11-13].
Thus, this study aims to capture a comprehensive overview of healthcare situation in terms of healthcare needs and disruptions for individual healthcare around the world during the COVID-19 pandemic. How healthcare systems were disrupted and geographical distribution of disruptions were the main objectives of this research [14]. In order to achieve the objectives healthcare data has been used from 76 countries during COVID-19. The paper tries to explain different healthcare needs for individual at different times and reasons for not availing the desired healthcare services. Additionally, the paper looks for the significant differences based on geographic locations of seeking the important health facilities, during the COVID-19 pandemic.
Materials and Methods
We performed secondary data analysis of the dataset retrieved from Global Health Data Exchange (GHDX) based on the individual routine healthcare disruption during COVID-19.
Study design, data sources and participants overview
We used data from Global Health Data exchange (GHDx) which is cross sectional in nature and collected with the contribution of Institute for Health Metrics and Evaluation (IHME), Bill and Melinda Gates Foundation (BMGF) and premise data corporation. We retrieved two distinguished datasets (on three time frames for each data, a total of four datasets) on individual healthcare service disruption in 2020 and 2021. For the first dataset, general population COVID-19 health services disruption, round one data was collected throughout July 2020 and the second round data throughout May-June 2021 on the premise platform [15-17]. Premise implemented the survey, which was prepared by IHME in partnership with the BMGF. As an inclusion criterion of the respondent for the survey other than the respondents’ country of residence, no other inclusion criteria were specified. The sample technique for this survey, to some extent, veers off from the representative sampling characteristics. To overcome and mitigate the effects of a non-representative sample, the survey weights were calculated using the estimated probability of selection of a representative sample [18]. As a criterion the representative dataset of global burden of disease 2020 population was followed, which estimates and proportions for age, gender and education by country. Following this standard procedure age and education categories were mapped to premise survey categories. Afterwards, weights were calculated as the inverse of the predicted probability of selection in the sample dataset. Survey weights were calculated using a combined dataset of responses to the ORB and IPSOS COVID-19 health services disruption survey 2020 and the premise general population COVID-19 health services disruption survey 2020 [19].
Individual healthcare disruption survey questionnaires had 36 features, including age, sex, area of residency, ethnicity, education, employment, religion, geographic location and related questions in each survey. All the included variables included in the survey is provided in data collector website [20]. Among these variables we are only interested in observing the magnitude of disruptions based on age, sex, area of residency and geographic locations in some required health service provisions. In observing individual healthcare service disruption we keenly distinguished the necessity of individual health services in Dec, 2019 to Feb, 2020 period to post March 2020 period and Feb, 2021 to May, 2021 time span on the following services:
• Individuals’ medication urgency for the selected diseases.
• Health conditions for which healthcare visits were necessary and
lastly.
• Reasons for which individuals were not being able to see/visit a
healthcare provider.
Datasets, timeline and variables
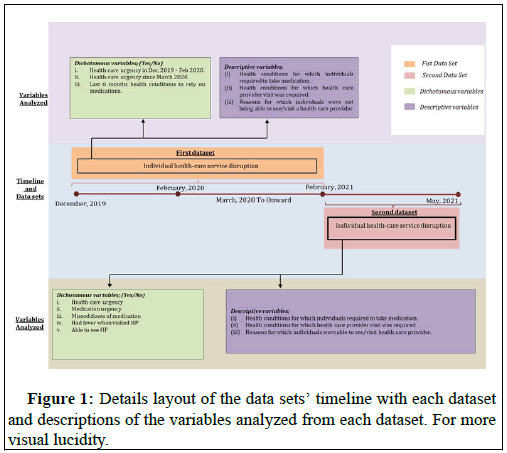
It shows Figure 1.
Procedures
Understanding disruption to individual routine healthcare: One of the objectives of this study was to understand the disruptions conditions to individual routine healthcare services due COVID-19. In understanding the significance of COVID-19 situation in disrupting individual routine healthcare services four distinct covariates age, sex, area of residency, and geographic locations were used against eight dichotomous variables. First three dichotomous variables:
• Healthcare urgency in Dec 2019-Feb 2020.
• Healthcare urgency since March 2020.
• Last 6 months (February-July, 2020) health conditions to rely on
medications were analyzed based on yes, no answers.
For the second timeline (started from Feb, 2021 to May, 2021 periods) we explore the following variables:
• Healthcare urgency in Feb 2021 to May 2021.
• Medication urgency in Feb 2021 to May 2021.
• Missed any doses of medication in Feb 2021 to May 2021.
• Had fever when visited healthcare provider.
• Able to see/visit healthcare provider.
All these variables were also in dichotomous (yes, no) in nature. Other variables including health conditions for which individuals required to take medication, health conditions for which healthcare provider visit was required, and lastly reasons for which individuals were not being able to see/visit a healthcare provider were explored using descriptive analysis.
Statistical analysis: Our analysis used descriptive statistics, for individual healthcare service disruption data, to quantify characteristics such as health issues that required individuals to take medication, health conditions that required a visit to healthcare professionals and reasons for why individuals were unable to see/visit a healthcare professional were investigated. We have further used logistic regression to investigate the impacts of the pandemic situations on three timelines across the datasets with the covariates of age, sex and area of residency. In his regard, eight dichotomous variables were tested against respondents’ age, sex and area of residency. Variables analyzed in this research are illustrated in the Figure 1.
For geographical presentations of all the dichotomous variables across three different timelines we deployed Chi square statistics and a proportion of the responses of each variable are presented in per hundred populations. In this regard, countries were considered as the highest administrative unit in the whole map, as GADM (database of global administrative areas) described. This administrative unit represents, for example, United States, Saudi Arabia and India. Moreover, for the logistic regression analyses, we have reported associations as Odds Ratios (ORs) adjusted for age, sex, area of residence, with 95% CIs. We considered p values of less than 0·05 to be significant both for regression and Chi square statistics. All the statistical analysis and calculations were done using R, version 4.1.0 and Microsoft Excel. The graphical presentation of maps was done using ArcGIS, version 10.3.
Patient and public involvement statement: This study used secondary survey data collected by Global Health Data exchange (GHDx) in contribution of IHME and BMGF. No patient or public involved in this study.
Results
Results from the primary analysis shows that the both surveys include 52,492 and 18,642 participants, of whom 68% and 66% were male and 32% and 34% were female respectively. Considering the age group 16-25 aged group were highly observed in the population marking 50.5% and 41.5% and lastly city center or metropolitan area people were highly witnessed in both data set by 41.4% and 45% (Table 1).
| Timeline | December 2019 to February 2020 to March, 2020 to onward (6 months) (n=52492) | February 2021 to May 2021 (n=18642) |
|---|---|---|
| Gender | ||
| Male | 35696 (68%) | 12296 (66%) |
| Female | 16796 (32%) | 6346 (34%) |
| Age at baseline (years) | ||
| <16 | 1728 (3.3%) | - |
| 16 to 25 | 26520 (50.5%) | 7748 (41.5%) |
| 26 to 35 | 16336 (31.1%) | 6892 (37) |
| 36 to 45 | 5841 (11.1%) | 2771 (14.9%) |
| >45 | 2067 (3.9%) | 1231 (6.6%) |
| Area of residency | ||
| Rural | 14064 (26.8%) | 4668 (25%) |
| Suburban/Peri-urban | 16706 (31.8%) | 5590 (30%) |
| City center or metropolitan area | 21722 (41.4%) | 8384 (45%) |
Table 1: Baseline characteristics of the participants of the primary dataset from the two distinguished surveys.
Figure 1 shows the data about health conditions for which people sought visitation to healthcare professional during three particular time periods start from December 2019 to February 2020, since March of 2020 to six months forward and February 2021 to May 2021. For all the three timelines preventive or routine healthcare was highly demanded (34.76%, 37.66% and 3.12%) respectively. Secondly, health conditions like heart disease, malaria, stroke, injury and depression were the mostly noticed conditions for healthcare visit over these three periods by (12%, 7%, 4%, 4%, 3%) approximately in the December 2019 period, (13%, 5%, 5%, 3%, 3%) in since March 2020 to onward six months and (12%, 5%, 5%, 4%, 3%) in February 2021 to March 2021 timestamp. Finally, healthcare for COVID-19 care which was 11th rank in a row (2.9%) in Dec-Feb period but jumped into 5th rank (3.72%) in March, 2020 to onward period.
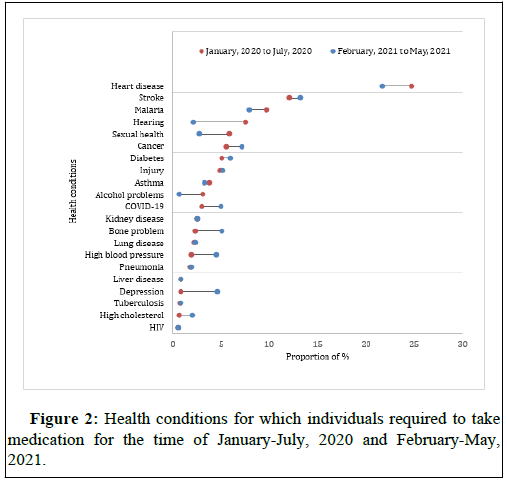
Below Figure 2 explains health conditions for which individuals required to take medication for the time of January-July, 2020 and February-May, 2021. Analysis shows that heart disease (24.68%), stroke (12.07%), malaria (9.72%), hearing or vision problems (7.52%) and sexual and reproductive health (5.87%) were highly observed individual health conditions for which medication was essential in January, 2020 to July, 2020. The same health conditions were also the dominant reasons for which medication was essential in February, 2021 to May, 2021 by sharing (21.62%) (13.10%) (7.97%) correspondingly. Additional information is in Supplementary Figure 2.
Supplementary Figure 3 shows reasons for which individuals were not being able to see/visit a healthcare provider in all the timestamps. Results represent that in December 2019 to February 2020, lack of money (22.20%) and turned away from health facilities (20.9%) were the two most significant reasons. Closed health facility (17%), treatments or tests unavailability (16%) and lack of transportation were also some other major reasons. Since March 2020 to onward period, closed health facilities due to COVID-19 jumped to the top position as a reason of inability access healthcare sharing by 23% response. Lack of money which was in first place a few months ago jumped 2 steps down though the percentage remained almost same like before. Turned away from health facility (26.31%) was top most reason for not accessing healthcare facility or healthcare professionals in Feb 2021 to May 2021. Closed health facilities (21.77%), unavailability of tests and treatment (14.53%) were also mostly mentioned reasons for failing to access healthcare.
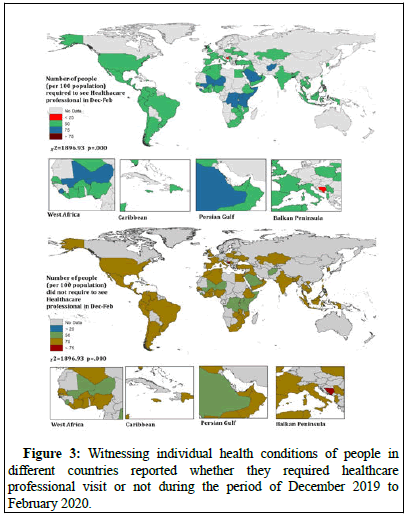
From Figure 3 in observing country wise comparison for the urgency of individual healthcare professional visit in December 2019 to February 2020 was highly noted in Somalia (63%), Afghanistan (61%), Sierra Leone (61%), Tanzania (60%) and Uganda. People of Democratic Republic of Congo, Mali, Niger, Saudi Arabia and Kenya were also identified with more than 50% accorded to sought healthcare professional visit. While individuals in Hong Kong (80%), Bosnia and Herzegovina (75%) and Bahrain (75%) had less urgency to visiting to healthcare professionals and all these are statistically significant. Healthcare necessity in March, 2020 to forward time period also had the similar pattern with December, 2019 to February, 2020 time period. But in less urge for healthcare was observed in Bahrain, Bosnia and Herzegovina and Italy with more than 80% conformity from each country. Highest number of people reported in Sierra Leone, Democratic Republic of the Congo, Senegal, Afghanistan and Bangladesh with more than 60% consensus in each country that they had to rely on medication for medical urgency in the past six months from March, 2020.
And this trend of relying on medication for medical urgency was significantly low in South Korea, Hong Kong, Taiwan and Albania with confirming more than 70% from each country (Supplementary Figures 1-2). For the timeline of February, 2021 to May, 2021 healthcare urgency for individual health was significantly observed in Somalia (100%), Sierra Leone, Jordan and Tanzania with 60% compliances. Missed medication from the health facilities was highly reported in Lebanon Bahrain and Oman with 100% compliances and in Cambodia, Lithuania, Bosnia and Herzegovina, Algeria, France, Jamaica, Albania, Niger, India individual reported with more than 80% compliances that they have missed medication dosed from facilities in February, 2021 to May 2021 timeline. The cases of healthcare visit with fever were also highly reported in Bahrain and Oman (100% for each country). People in Liberia, Italy, Ivory coast and Lebanon also reported with more than 90% conformity that they had fever during healthcare visit. People from Bahrain (100%), Italy (89.4%) and Albania (80%) failed to see healthcare professional in times of emergency (Supplementary Figures 3-7).
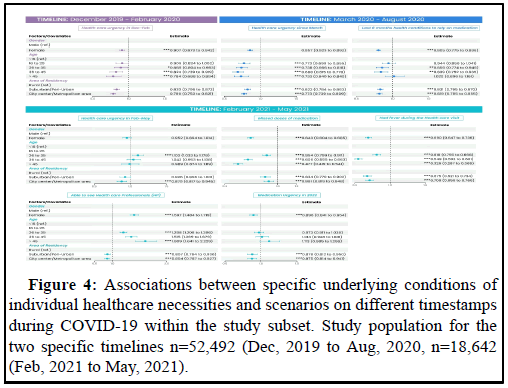
Figure 3 reports Odds Ratios (ORs) for the eight different response variables in individual health issues controlled against respondents’ gender, age and area of residency for the three broad specific timelines. For the first timeline of December, 2019 to February, 2020 in witnessing the urgency of medical healthcare professionals visit was observed highly (OR: 0.90, 95% CI: 0.87-0.94, p=.000) in female group. Age range group of 26 to 35 were mostly observed seeking OR: 0.8, 95% CI: 0.80-0.98, p=.022) healthcare urgency in the same timeline. Since March of 2020 to onward healthcare urgency were significant for all controlled variables, among them suburban/peri-urban residents healthcare necessity compared to rural residents were statistically significant (OR: 0.82, 95% CI: 0.78-0.86, p=.000) and age group >45 also had significant healthcare urgency OR: 0.73, 95% CI: 0.64-0.84] p=.000). Medication dependency in the last six months, in the timeline of March 2020, were highly significant in age group of 26 to 35 (OR: 0.86, 95% CI: 0.77-0.95, p=.000) and 36 to 45 (OR: 0.84, 95% CI: 0.75-0.94, p=.000). For the third timeline, February of 2021 to May of 2021, healthcare urgency was significantly observed in 26 to 35 age group (OR: 1.10, 95% CI: 1.03-1.18, p=001) and city and metropolitan people had the same urgency (OR: 0.88, 95% CI: 0.82-0.95, p=000). Missing doses of medication was significantly observed among the age group of 26 to 35, 36 to 45 and >45. City people have highly reported the cases of missing doses of medication (OR: 0.89, 95% CI: 0.82-0.95, p=.000). Fever during the healthcare visit was highly significantly quantified in 26 to 35 aged people (OR: 0.81, 95% CI: 0.76-0.87, p=.000). And medication urgency was significantly observed for the city residents (OR: 0.88, 95% CI: 0.81-0.94, p=.000) (Supplementary Figures 8-10).
Discussion
Throughout this study we were inclined to understand the impacts of the COVID-19 in disrupting individual healthcare service provisions in some chosen healthcare services as the global transmission of COVID-19 has caused experts to think about the health systems of Low or Middle Income Countries (LMICs).
In this study individual healthcare provisions, we explored the following patterns in three specific timelines:
• Serious health conditions for which medication was required.
• Medical conditions for which individual sought healthcare.
• Reasons for not being able to access to health facility during
COVID-19 outbreak.
Though our study provided combined country perspectives in the circumstances of individual inability to access healthcare facilities and among these circumstances’ money shortages, closed health facility, turned away from services, unavailability of treatments in health facility and transportation problem were the most prevalent and highly pronounced. This scenario was likely the same in Africa where urban health facilities were overcrowded and understaffed and rural health facilities were inaccessible due to roads and transportation problem. Likewise, similar condition from India also affirms that since late Mach of 2020 both healthcare workers and poor healthcare seeking individuals had problems to reach health facility due to restriction on public transportations. Moreover, health facilities reduced services by 21%, clinical admission for acute cardiac events by 50% and care for admitted pulmonary patients by 32%. Representing the findings of this study, during this chaotic phase of health system disorder, noncommunicable diseases like Cardiovascular Disease (CVD), cancer and diabetes were also on the rise as a primary cause of death worldwide due to the inadequate health services (Figure 4).
In Ireland in a study titled ‘the corona citizens' science study’ reported that 32% of respondents (10,830 people) postponed their medical checkups and treatments and more than half of them claimed that healthcare professional was not seeing any patients at that moment. Another study in Nigeria revealed that since March, 2020 34% respondents’ required healthcare services and 26% of them failed to access the needed services. Describing predicaments 55% of the respondents mentioned financial constraints and a quarter of them reported inaccessibility due to lockdowns and movement restrictions. Moreover, the fact that the categories of people based on socioeconomic conditions are more susceptible to the consequences of COVID-19 infection and disruption. For instance, low income communities tend to have higher incidence of chronic diseases due to fewer financial and medical resources, overcrowding and poor infrastructure which also increases the higher rate of morbidity.
In order to draw a world view on health service disruption WHO report depicts that among 112 countries in primary care services, routinely scheduled visits and health promotion services were disturbed in more than half of the countries (54% and 53% respectively). On the other hand, essential care services like special care and visits for undifferentiated symptoms were curbed down in half of the countries’. Altogether this public health concern issue has caused over 45% of the countries among 135 nations facing disruptions in primary, rehabilitative, palliative and long term healthcare services for the most vulnerable people. In the meantime, disruptions in primary healthcare during pandemic has barred individuals in seeking medical care which has additionally increased number of patients with heart disease, strokes and other acute diseases which completely captures the similar findings corroborating our study drawing the world perspective. Though the numbers of non-COVID-19 patients with other medical conditions have reduced in hospital visits but it is self-evident that during social upheavals due to the well-established effects of stress and the brain-heart connection the danger of Acute Myocardial Infarctions (AMIs) and strokes has increased significantly. One study revealed that in England the wide spread cut down in health services, due to COVID-19, instigated cancellation of treatment and operation for older people living in more deprived areas and where nearly 74% of the population age over 50 required immediate medical attention. In African countries essential healthcare services including maternal and child health services, HIV treatments and surgeries were reduced more than half. Findings from our study to explore individual healthcare disruptions from broad perspectives, even with country perspectives too, aligns with the findings of various reports of WHO and other geographically and separate significant works.
Conclusion
Combining all the scattered scenarios, this study has a strong appeal in understanding worldwide healthcare disruptions which is still missing in literature. Though it is anticipated that COVID-19 is in reined, but the emergence of new variants or the new viruses could create another chaotic scenario worldwide. Our study has compiled three time stamps of individual healthcare disruptions from 76 countries. Although the data sets for two different healthcare services were different, findings were largely consistent, supporting the generalizability of our observations. But one important limitation of this study, based on the data source used, was that for few countries the data was insufficient and overall generalizability from the aggregated results was considered in that respect.
As public healthcare system crumbles in countries facing societal realities where large populations, informal workers and migrant workers make a big dent in the way of progress. Despite the limitation the study unveils the true picture of healthcare disruptions across the world. In conclusion, individuals were deprived of healthcare services due to their inability to reach health facility with imposing restrictions on movements and service provider’s absence or closed health facility coupled with individual economical limitations. Rise in other non- COVID diseases specifically heart disease, stroke and malaria were also significant. Regional, national and global coordination and collaboration with both public and private collaboration is quite necessary to reduce further disruptions in healthcare services. Moreover, determining right interventions and indicators for maintaining essential healthcare services is essential situation like this. Mobilization of prioritized and required resources in minimizing the adverse effect of the pandemic and finally maintaining the progress, at least try to reduce the risk of reversing the progress and achievements made in public health is crucial worldwide.
Author’s Contributions
SA designed the study framework and methodology, SA and IAF analyzed and visualize the data, SA drafted the firm manuscript and SA and IAF revised the draft. Both authors were involved in critically revising the manuscript and approving the final version.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not for profit sectors.
Competing Interests
None declared.
Research Ethics Approval
For this study any kind of ethical approval was not required based on the nature of this study.
References
- Angelico R, Trapani S, Manzia TM, Lombardini L, Tisone G, et al. (2020) The COVID-19 outbreak in Italy: Initial implications for organ transplantation programs. Am J Transplant 20: 1780-1784.
[Crossref] [Google Scholar] [PubMed]
- Wang D, Korte ML, Hemler EC, Abdullahi YY, Lankoande B, et al. (2021) Reported barriers to healthcare access and service disruptions caused by COVID-19 in Burkina Faso, Ethiopia and Nigeria: A telephone survey. Am J Trop Med Hyg 105: 323.
[Crossref] [Google Scholar] [PubMed]
- Baum A, Schwartz MD (2020) Admissions to veteran’s affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA 324: 96-99.
[Crossref] [Google Scholar] [PubMed]
- Cash R, Patel V (2020) Has COVID-19 subverted global health?. Lancet 395: 1687-1688.
[Crossref] [Google Scholar] [PubMed]
- Causey K, Fullman N, Sorensen RJ, Galles NC, Zheng P, et al. (2021) Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: A modelling study. Lancet 398: 522-534.
[Crossref] [Google Scholar] [PubMed]
- Connor MJ, Winkler M, Miah S (2020) COVID-19 pandemic is virtual urology clinic the answer to keeping the cancer pathway moving? BJU Int 125: E3-E4.
[Crossref] [Google Scholar] [PubMed]
- Dong E, Du H, Gardner L (2020) An interactive web based dashboard to track COVID-19 in real time. Lancet Infect Dis 20: 533-534.
[Crossref] [Google Scholar] [PubMed]
- El-Sadr WM, Justman J (2020) Africa in the path of COVID-19. N Engl J Med 383: e11.
[Crossref] [Google Scholar] [PubMed]
- Elston JW, Moosa AJ, Moses F, Walker G, Dotta N, et al. (2016) Impact of the Ebola outbreak on health systems and population health in Sierra Leone. J Public Health 38: 673-678.
[Crossref] [Google Scholar] [PubMed]
- Hartnett KP, Kite-Powell A, de Vies J, Coletta MA, Boehmer TK, et al. (2020) Impact of the COVID-19 pandemic on emergency department visits United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep 69: 699.
[Crossref] [Google Scholar] [PubMed]
- Mann DM, Chen J, Chunara R, Testa PA, Nov O (2020) COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc 27: 1132-1135.
[Crossref] [Google Scholar] [PubMed]
- McDonald HI, Tessier E, White JM, Woodruff M, Knowles C, et al. (2020) Early impact of the Coronavirus Disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro Surveill 25: 2000848.
[Crossref] [Google Scholar] [PubMed]
- Medeiros K, Baicu CF, Fitzgibbons TP, Shaw P, Tighe DA, et al. (2014) Systolic and diastolic mechanics in stress cardiomyopathy. Circulation 129: 1659-1667.
[Crossref] [Google Scholar] [PubMed]
- Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, et al. (2020) Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low income and middle income countries: A modelling study. Lancet Glob Health 8: e901-e908.
[Crossref] [Google Scholar] [PubMed]
- Rust G, Melbourne M, Truman BI, Daniels E, Fry-Johnson Y, et al. (2009) Role of the primary care safety net in pandemic influenza. Am J Public Health 99: S316-S323.
[Crossref] [Google Scholar] [PubMed]
- Salerno R, Conti CB, de Silvestri A, Davies SEC, Mezzina N, et al. (2020) The impact of COVID-19 pandemic on urgent endoscopy in Italy: A nation-wide multicenter study. Scand J Gastroenterol 55: 870-876.
[Crossref] [Google Scholar] [PubMed]
- Samuels MA (2007) The brain-heart connection. Circulation 116: 77-84.
[Crossref] [Google Scholar] [PubMed]
- Schirmer CM, Ringer AJ, Arthur AS, Binning MJ, Fox WC, et al. (2020) Delayed presentation of acute ischemic strokes during the COVID-19 crisis. J Neurointerv Surg 12: 639-642.
[Crossref] [Google Scholar] [PubMed]
- Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, et al. (2015) Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med 373: 929-938.
[Crossref] [Google Scholar] [PubMed]
- Lancet T (2020) COVID-19: Too little, too late? Lancet 395: 755.
[Crossref] [Google Scholar] [PubMed]
Citation: Ahmed S, Faid IA (2023) Disruption in Healthcare Services: Drawing Scenarios from Individual Healthcare during COVID-19. J Community Med Health Educ 13: 826.
Copyright: © 2023 Ahmed S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 869
- [From(publication date): 0-2023 - Apr 26, 2025]
- Breakdown by view type
- HTML page views: 645
- PDF downloads: 224