Research Article Open Access
Directly Observed Treatment Strategy Still a Challenge in Tuberculosis Control: The South African Plight
Winifred Nohaji, Nobesuthu Sokhela and Nomathemba Nonkelela*
Walter Sisulu University, Mthatha, Province of Eastern Cape, South Africa
- *Corresponding Author:
- Nomathemba Nonkelela, RN, PhD
Walter Sisulu University, Mthatha
Province of Eastern Cape, South Africa
Tel: +27 47 502 2746
Fax: +27 86 497 7327
E-mail: nnonkelela@wsu.ac.za
Received date: June 24, 2016; Accepted date: August 24, 2016; Published date: August 31, 2016
Citation: Nohaji W, Sokhela N, Nonkelela N (2016) Directly Observed Treatment Strategy Still a Challenge in Tuberculosis Control: The South African Plight. J Comm Pub Health Nurs 2:136. doi:10.4172/2471-9846.1000136
Copyright: ©2016 Nohaji W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
The challenges in the management of tuberculosis (TB) are clearly manifested by the escalating numbers of not only the ordinary tuberculosis but also the drug resistant forms of TB, namely MDR-(Multi-Drug Resistance) and XDR-TB (Extreme Drug Resistance-Tuberculosis). The management of tuberculosis in SA and the whole world has been ranked as a priority due to its impact on health and economy. The effectiveness of Directly Observed Treatment Strategy (DOTS) as a strategy for the control of TB and its treatment is affected by a variety of socioeconomic issues around the world and particularly in the developing countries. This study was conducted to highlight the challenges faced by the country in the control tuberculosis even in the implementation of the directly observed treatment strategy.
Keywords
DOTS; MDR; XDR
Introduction
The emergence of XDR TB has been potentially disastrous for the local and international TB control. Tuberculosis control programmes were adopted by the WHO in 1996 and have been continuously improving. The strategy adopted by the WHO is the Directly Observed Treatment Strategy in which the administration of anti-tuberculosis drugs is supervised. Various methods of supervision are designed to meet the geographical needs of the area. This forms part of the six elements that are used to drive this strategy. South Africa has been identified as one of the highly-burdened countries for drug resistance [1] but still experiences challenges in TB control.
Background and Significance of the Study
The World Health Organisation (WHO) declared Tuberculosis (TB) a global emergency in 1993. It stated that TB is humanity’s greatest killer because it kills more adults each year than any other infectious disease, including malaria and all tropical diseases. Tuberculosis (TB) is a health threat in most countries of the world and demands intervention strategies strongly supported by various government departments as well as non-governmental organisations. It is a communicable and contagious disease that kills around two million people each year and has currently infected one-third of the world’s population, with one person newly infected every few seconds each day [2].
TB has reached epidemic proportions in many parts of the world so much that as many as two million people die every year from a disease that is curable (WHO 2008: 18).
The literature used in this study relates to the incidence world-wide and challenges in the management of TB. In 1993 an urgent announcement of declaring TB a global emergency was pronounced for the first time by the WHO, having noticed that adults are killed by TB each year than any other communicable disease, including malaria and all tropical diseases (RSA Department of Health 2007: 23). This is the reason why South Africa decided to join other countries to adopt a strategy known as the Directly Observed Treatment Short Course (DOTS) which is believed to be the most effective means of controlling TB. With this strategy in place, cure rates are reported to be as high as 95% even in poor countries with few resources. In turn, without DOTS, the cure rates are as low as 40% and below. Poorly managed TB control programme may lead to a more serious state, the development of multi-drug resistant (MDR) TB with 50%-60% chance of cure (Department of Health, RSA 2008: 75).
The world-wide burden
Globally, out of 9.2 million TB cases reported in 2007, 1.7 million died. The incidence is aggravated by the emergence of TB/HIV coinfection. The WHO estimates that there are about 9 million new cases that occur annually and about 2.5 million deaths per year, making TB second only to HIV/AIDS as the leading cause of death from infectious disease [3].
Lawn (2008:325-333) states that the alarming increase of TB/HIV co-infection contributed 456 000 TB/HIV deaths in 2007, which is 23% of the global HIV/AIDS mortality. 79% of the disease burden was for Sub-Saharan Africa alone whilst South Africa alone was having more than a quarter of all the cases. Global TB Alliance reflected this statement in its 2005 Tuberculosis control report card, “Tuberculosis was last year’s most overlooked tragedy. Tuberculosis killed more people than all wars, earthquakes, floods, tsunamis, airline accidents, terrorist acts and murders worldwide the past year and with much less fanfare.
A study by Wood et al. [4] revealed poor tuberculosis control measures in South Africa and it is still not clear why this is the case. This is based on a study conducted in 2005 where approximately 7457 had tuberculin test and 37.4% tested positive. Although South Africa has made progress in reducing Tuberculosis prevalence and related deaths by implementing the basics for TB diagnosis and treatment, the burden of Tuberculosis in the country remains enormous. It is apparent that the prevalence of tuberculosis is exacerbated by its coexistence with HIV which has escalated from 200/100,000 population in 1990 to 800/100,000 population as recorded in a study conducted in 2013 [5]. With the increase in tuberculosis notifications DOTS implementation seems to be negatively affected.
The role of the community in TB response
Kheshavjee et al. [6] argue that there are a lot of challenges for community role in TB response. In 86% of countries reporting to the WHO, the health workers continue to be the main providers of directly observed treatment (DOT), which reflects that the client-centred approach is neglected although it is mentioned in principle. Patients, and therefore the community, should be the main care providers and fully engaged in the shaping of their own care. They should form the cornerstone in the prevention of all the various forms of illness [7].
Another threat is the emergence of drug resistant tuberculosis which demanded an urgent response by the WHO in 2007. The WHO realized that millions of rand are needed annually to meet the demands of diagnosing and treating over 1.5 million patients with drug-resistant TB by 2015. This is in line with TB universal access aims for 2010 and the 2015 Stop TB Partnership targets [8].
Directly Observed Treatment Strategy (DOTS)
The World Health Organisation adopted a strategy to deal with tuberculosis in the whole world, the Directly Observed Treatment Short-Course (DOTS) strategy. In South Africa it was adopted and implemented in 1996. This strategy requires that, among other principles, each patient is supervised when taking treatment. The treatment is given according to the national TB control programme guidelines. Drug combinations as well as single drugs are used in the first-line treatment of TB. Second-line drugs are used in the treatment of drug resistance and patients referred to specialised MDR-TB units like Jose Pearson and Fort Grey for the Eastern Cape.
The treatment is to be supervised directly by nurses in the clinics or in the homes for patients. Use is made of Directly Observed Treatment (DOT) supporters in the form of community health workers and patients’ family members. Nurses are trained to adhere to the treatment guidelines. The treatment success rate was 68% in 2002 [9].
In 2007 the South African government committed itself to working with all stakeholders both locally and internationally to contain the spread of XDR-TB and ensure that all reported cases are effectively managed. The following measures to strengthen infection control in health facilities to help reduce TB transmission were also outlined:
Improvement of MDR-TB units country wide to deal with infection control where it was not possible to extend the facility/wards were identified in hospitals for accommodating additional patients and the necessary structural adjustments were made.
It was also announced that, in addition to resources available in provinces, the government has allocated extra money from Global Fund grant to support the infection control renovation projects.
Evaluation of directly observed treatment strategy in one of the provinces in South Africa revealed that only 56.8% of tuberculosis patients on re-treatment regimen are on directly observed treatment rather than those on first-line treatment [10]. The current study was done in a different province in the country.
Methods
This study was conducted with the purpose of determining the challenges in the management of tuberculosis (TB) that could contribute to drug resistant TB. It was conducted in 4 community health centres in the O.R. Tambo District in the Eastern Cape. The community health centres were purposively selected due to the high caseload of tuberculosis.
Mixed methods (qualitative and quantitative research methods) were used in the study. Qualitative data collection was used to obtain information from the TB trained professional nurses responsible for TB management from each of the health centres under study to determine how they implemented the DOTS strategy and how they managed patients who experienced problems. Quantitative data was collected to determine the problems encountered by patients in adhering to the correct practices within the TB management such as the right times for treatment and food intake, support from families, nutrition and accessibility of health services.
From each health facility one registered nurse trained on and responsible for TB programme management was purposively selected. Ten TB patients on retreatment were randomly selected and two drugresistant TB patients were purposively selected. The total sample was 40 re-treatment patients, 8 drug resistant patients and 4 registered nurses.
Data Analysis
Quantitative data analysis
Non-parametric statistical analysis of quantitative data, collected from all MDR-TB and all retreatment patients in the study, was followed. The pre-analytic phase involved administrative and clerical tasks like reviewing the raw data for completeness, logging in the filled questionnaires from the research subjects and selecting statistical software for doing the data analysis. The raw data was coded thus giving numbers as befits statistical analysis and entered onto computer files creating a data set as in the following table that represents a portion of the collected data (Table 1).
| Subjects | Resistance | b/type | b/time | t/pills | helper | diva | Meal/times | Types | K/p |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 1 | 10:00 | 2 | 1 | 1 | 2 | 5 | 1 |
| 2 | 1 | 2 | 12:00 | 2 | 2 | 2 | 3 | 4 | 1 |
| 3 | 1 | 1 | 7:00 | 2 | 2 | 1 | 4 | 6 | 1 |
| 4 | 1 | 2 | 6:00 | 1 | 1 | 2 | 4 | 8 | 2 |
| 5 | 1 | 2 | 8:00 | 1 | 1 | 2 | 4 | 8 | 1 |
Table 1: Portion of quantitative data.
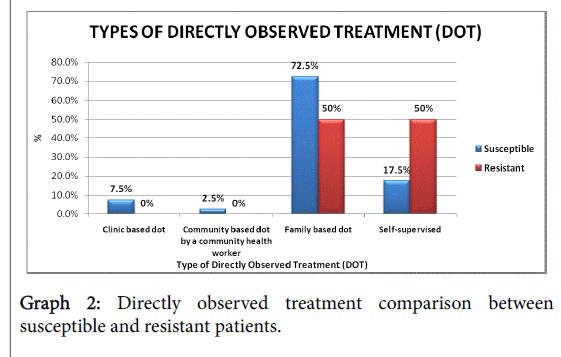
The study comprised fifty two subjects i.e. forty retreatment patients, eight MDR-TB patients, four TB trained nurses and eighteen variables and the results were as follows (Table 2 and Graphs 1-3).
| DOT for all | Observed by relatives | Observed by CHWs | Clinic-based DOT | Self-supervised |
|---|---|---|---|---|
| % | 68.7 | 2.1 | 6.3 | 22.9 |
Table 2: Directly Observed Treatment for all 48 participants.
Susceptibility
Out of forty eight subjects, forty were susceptible to TB treatment and eight were resistant which gave 83.3% and 16.6% respectively.
Results
Both nurses and patients provided similar views with regard to challenges experienced in TB control strategies.
Challenges in integrating TB and HIV/AIDS programme
Nurses complain of missed opportunities in diagnosing TB and HIV/AIDS due to poor integration of these services as most of the clients are co- infected with HIV. In most clinics HIV clients are attended in different units from TB infected clients. This situation makes it difficult to identify those clients who are co-infected by the two conditions.
Once patients are diagnosed they move to other areas out of shame that they have TB especially where it is coupled with HIV positive status. This ‘cross border’ situation from one health sub-district to another makes it difficult for nurses to trace treatment defaulters.
This is partly due to need for training amongst the health workers and partly due to lack of space to accommodate the two programmes under one roof. Nurses feel there is a dire necessity for a lot of budget to be channelled through to the TB control programme to train all nurses and continually update them on new developments and new practices and protocols on both TB and HIV/AIDS. In the presence of these two conditions facilities must be upgraded to suit the implementation of integrated services. There is high potential for cross infection due to limited space which also makes it difficult to integrate TB and HIV/AIDS. Strengthening of infection control is one of the key issues in TB management in order to prevent the spread of the TB disease. Health workers are already getting infected with TB. There are some facilities which experience difficulties in keeping constant stock of appropriate masks due to lack of funds to buy these.
Types of food and patterns for meals per day for the patients
Most of the participants reported inability to have access to nutritious well balanced food because of lack of funds and energy to tender their own gardens. The types of food that they could afford consisted mainly of maize products which contain a lot of starch. Some could manage beans and vegetables. For some these meals are enjoyed only once a day with maize based beverages for the rest of the day.
Time for pills in relation to food intake
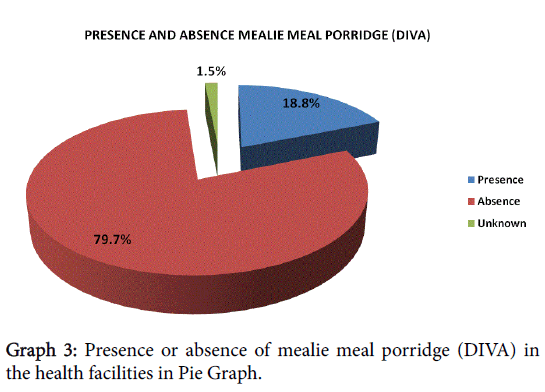
37.5% of the patients took their TB treatment before breakfast while 62.5% took it after breakfast. The presence of ‘diva’ in the clinics assists the patients to associate treatment intake with food intake. This comes in handy for patients who stay alone and have challenges preparing their own meals especially in the morning.
Availability of a helper
Many (62.5%) of TB patients reported not having anybody to help at home. So they depended on themselves for cooking and taking treatment. This makes things difficult especially if they are not feeling well on a particular day.
Knowledge of the TB treatment
Most of the participants did not have full knowledge of their treatment and why they had to take it for such long periods of time. This leads to stoppage of treatment once the person feels better even when the treatment tern is not over. 83% reported swallowing their daily dose of tablets at the same time and 17% split the dose.
Induced vomiting before or after TB treatment
Culturally people believe in induced vomiting to relieve stomach upset.
Seventy seven percent (77%) of patients did not induce vomiting at all while 8% induced vomiting before meals and 14.5% after taking treatment if they experience stomach upset caused by TB/HIV drugs.
Accessibility of the health facility
Accessing health facilities poses challenges as most of these are not within easy reach for the clients. This leads to poor treatment compliance for some clients. TB patients are often very sick and cannot travel long distances.
Staff shortage
Gross shortage of the nursing staff makes it difficult for them to visit the patient homes as they have to maintain fast queues for TB patients. Other important service for the patients, including health education, treatment adherence counselling and even proper recording on the available registers and patients cards, suffer in the light of staff shortage. Coupled with this is the lack of community health workers in places that are far from the health facilities.
“Cross border” treatment problems
There is great need for strengthening of the referral systems even though patients are free to seek healthcare wherever they want. This only encourages treatment interruption if proper referral is not implemented. Patients move from one sub-district to another seeking medication and end up defaulting TB treatment. When they get sick again they are tempted to change names and report as new clients who have never been on treatment before. Most of these patients are usually far from the sub-districts they belong to and decide to cross to any health facility that might be a bit nearer although transport will have to be used. When they feel better they just stop treatment on their own as there are no treatment supervisors in these areas. The nurses themselves are unable to reach them because of shortage of staff and lack of transport in the facilities. This becomes a very difficult situation for both the nurses and the clients. In situations like these the importance of the mobile services to rescue can never be overemphasised because patients are unemployed and they lack funds to travel up and down. Most of them are so poor that they do not even afford to access good diet hence the need for nutritional supplements.
Poor supervision of treatment
There is evidence of poor supervision of treatment due to shortage of staff, absence of community-based DOT supporters and long distances to be travelled by patients for clinic-based DOTS. Some TB sufferers fail to disclose the diagnosis to relatives. As a result some relatives are often unaware that the patient has TB until the person is very ill.
Very few patients have access to clinic-based DOT as it can be costly for those staying far from the health facilities. Although this is the most desirable type it is often difficult and costly for patients who are not even working to access services. It becomes better when the trained health workers are available to do community-based DOT but their shortage is also experienced which forces the service to fall in the hands of patients` relative some of whom are not even properly updated about it.
When supervision is done by the relatives the onus lies upon the nursing staff to fully equip them before they undertake to do it. Some patients do not even have relatives. They stay alone and cannot afford clinic-based DOT due to poverty, long distance from the clinic and being very sick and weak. This group of patients have no alternative if not admitted in hospital but to take treatment on their own. Not all of the community health workers receive a stipend which makes it difficult for all of them to visit the villages to support patients from time to time whilst illness progresses. These patients stand very little chances of cure but progress to extensively-resistant Tuberculosis.
Shortage of drugs
Constant availability of essential drugs in the TB programme is not always ensured as the nurses clarified that they did not receive treatment they ordered from the central medical stores. Availability of combination of rifampicin and isoniazid (RH) which is used in the continuation phase of treatment also poses many problems. Constant supply of drugs is one of the five important elements of the DOTS strategy.
Nutrition
Nutritional supplements have been found to be a problem nowadays, diva is not available, neither any food parcels are given to patients whilst poverty is ruling over them. Others are forced to go begging in order to eat. Some of them revealed that they thrive on only one meal per day and there is no alternative as they are unemployed. Other families are so poor that they depend entirely on fetching fire wood to cook, better still are the ones that use paraffin. Patients declared that they do not have people to help them at home and it is likely that these are starving as they rely on themselves for preparing their own food irrespective of their health status. Poor families use wood that can be fetched by a healthy person or paraffin that requires financial support. Lack of support grant plays a big role in the prevention of relapse for some patients.
Inaccessibility of health service
Long distances having to be travelled to the health facilities coupled with lack of community-based treatment supporters, and lack of money for public transport use, all came up clearly from the patients as problems that they encounter. Mobile services designed to provide treatment under supervision for rural communities should be provided for each health facility.
Discussion
The patients can easily adhere to their treatment through clinicbased DOT, should they be properly informed of such services by the nurses. Since TB is a major public health problem across the globe, every possible effort and strategy that is of help should be pursued as DOTS strategy is a globally recognized strategy for assisting TB clients to complete their treatment within the expected period, which is six months for all new clients and eight months for retreatment patients. DOTS is also used for the MDR TB and is here known as DOTS Plus strategy [11].
This is the only strategy that is capable of yielding 100% assurance that the client has swallowed his tablets because his treatment supporter has actually observed him swallowing the tablets and recorded in the appropriate treatment card of the patient [3].
Very few patients had their treatment supervised by the nurses or community health workers at the clinics (clinic-based DOT) during the time of research. There are still patients that are supervised by their relatives at home. Although sometimes there is no alternative, this is not at all reliable and is therefore not desirable because treatment may be interrupted when such relatives are away from home. Alternatively the patient may have to take treatment without supervision and this is greatly discouraged.
Experience has taught the health practitioners that there is a tendency among patients to interrupt their treatment when they feel better because TB treatment is taken for a lengthy period even when they no longer feel sick. This is a strong temptation for them to stop treatment thus calling for a need for home visits by both nurses and community health workers.
Health education alone is not sufficient to motivate them to complete their treatment, more so because loneliness and despair are two well known companions of patients with debilitating disease like TB and so the treatment supporter is a vital link to give emotional support and encouragement to enable the patient to overcome these feelings (Department of Health 2008: 46).
On the other hand, it is also clear that DOTS expansion is imperative if the TB problem is to be contained. This is a global need demanding TB advocacy, social mobilization and political commitment. The Dept of Health will never be able to fight the disease single- handed because it has gone out of control and is no longer just a medical but a social problem as well. Human, material as well as financial resources need to be put in place for success to be achieved [12].
There are even lost opportunities from those on streptomycin injection who could also swallow their treatment whilst coming for injections. According to the current guidelines of the SA National TB Control Programme, all re-treatment patients should be given an injection of streptomycin during the first two months of the three months initial phase. TB treatment is given seven days per week, including weekends. This poses a very good chance for these clients to be treated as clinic- based DOTS patients, swallowing their tablets whilst receiving their daily doses of streptomycin. This is possible for patients within a walking distance from the clinic and who are strong enough to do so. It is important for the nurses to make good use of this opportunity as some patients may be so sick that it becomes imperative for them to be admitted in hospital for these injections. This is one of the hospital admission criteria [13].
Social issues associated with attempts to control TB through DOTS
In most rural areas around South Africa people are completely or semi-literate. Children at high school level are often the “best educated” that often assist the family members in taking treatment of whatever nature. This is because as the younger ones they can still remember the instructions given at the clinic and can also read what is written on the treatment container. When it is not possible to have a community health worker for treatment supervision the high scholars take this responsibility. This therefore calls for the constant presence of this child at home in order to monitor treatment compliance. On the cultural level it sometimes becomes a problem for the young “carer” to insist on treatment compliance because if the TB sufferer refuses to take treatment, the younger one often has no way of convincing the sufferer, especially if the sufferer is older. Other challenges may involve inability to maintain a hygienic environment if the TB sufferer is still weak from the illness.
TB patients often display stubborn attitude or arrogance probably triggered by shame associated with suffering from TB or being cared for by someone else, particularly if the carer is a younger person. Culturally the older people assume that it is their responsibility to care for the younger ones. It becomes embarrassing for some of them to be a burden to their children as a result of ill health. Some may even pretend to be able to take care of themselves when in fact they cannot.
Limitations of this study
People with tuberculosis are still reluctant to disclose their illness because having tuberculosis is still carrying a stigma in many societies especially in the rural areas, hence the small sample for participation.
Recommendations
The results revealed that all the elements of the DOTS strategy were affected negatively by challenges such as the gross staff shortage, poor nutrition for patients, lack of community health workers for treatment supervision in some communities, periodical drug shortages and long distances travelled by patients, leading to treatment interruption.
It is recommended that the DOTS strategy be expanded and strengthened so that more patients receive clinic-based DOTS while community health workers are distributed to supervise all patients who cannot come to the clinic for daily treatment. Furthermore, patients on TB treatment must be given health education where balanced diet is emphasized. Outreach campaigns must be strengthened with strong emphasis on family involvement and education on prevention of diseases and adherence to treatment. Contacts must be traced and referred properly and defaulters traced early.
Chronic illnesses like TB need to be considered for financial support because good nutrition is a demand when patients are on treatment.
On-going research would be beneficial in identifying factors that lead to relapse and development of MDR -TB and management of such factors.
An interdisciplinary team comprising doctors, nurses, social workers, health promoters, various government departments as well as psychologists and other sectors is necessary to deal with a lot of challenges inherent in the TB management programme.
Conclusion
With escalating numbers of newly identified Tuberculosis people living below the poverty datum line and TB continuing to bear a stigma within local communities the control of TB is still going to pose serious challenges. More still needs to be done to educate people, especially the rural communities, that TB can be cured. Having said that, cultivation of land for vegetables needs to be encouraged so that people do not depend on buying all food stuff as the cost of living is also going up on a daily basis.
References
- MlamboCK, Warren RM, Poswa X, Victor TC, Duse AG & Marais (2008) Genotypic diversity of extensively drug-resistant tuberculosis. International Journal of tuberculosis lung disease 12: 99-104.
- Department of Health. RSA: Tuberculosis and HIV/AIDS: The DOTS strategy.
- World Health Organization (2008) Incidence of tuberculosis (per 100 000 population per year). WHO, Geneva.
- Wood R, Lawn SD, Johnstone-Robertson S,Bekker L-G (2011) Tuberculosis in South African prison: a transmission modelling analysis. South African Medical Journal101: 2.
- Churchyard GJ, Mametja LD, Mvusi L, Ndjeka N, Hesseling AC, et al. (2014) Tuberculosis control in South Africa – successes and challenges South African Medical Journal 104: 244-248
- Keshavjee S, Gelmanova IY, Farmer PE, Mishustin SP, Strelis AK, et al. (2008) Treatment of extensively drug-resistant tuberculosis in Tomsk, Russia: a retrospective cohort study.Lancet 372: 1403-1409.
- Kurtz DL, Lau E, Ong K, Zhao K, Kelly M. et al. (2010) Future young patient demand for primary and revision joint replacement. PubMed. US National Library of Medicine National Institutes of Health.
- World Health Organization (2007) Stop TB partnership – the global MDR-TB and XDR-TB response plan. WHO, Geneva.
- World Health Organization (2005) Global Tuberculosis control, surveillance, planning and financing. WHO, Geneva.
- Tumbo JM, Ogumbanjo GA (2011) Evaluation of DOTS in North West Province, South Africa. African Journal of Primary Health Care and Family Medicine 3: 1-4.
- International Council of Nurses (ICN) (2005) TB Guidelines for Nurses in the Care and Control of Tuberculosis and Multi-drug Resistant Tuberculosis.
- WHO Report (2005) Global Tuberculosis Control, Surveillance, Planning, Financing. WHO, Geneva.
- Department of Health (2009) The SA tuberculosis Practical Guidelines. Pretoria Department of Health.
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 12766
- [From(publication date):
August-2016 - Jul 15, 2025] - Breakdown by view type
- HTML page views : 11747
- PDF downloads : 1019