Direction of Fascia Movement in Finkelstein Test in Non-Symptomatic Thumbs of Healthy Individuals
Received: 03-Jul-2023 / Manuscript No. jnp-23-104142 / Editor assigned: 05-Jul-2023 / PreQC No. jnp-23-104142 (PQ) / Reviewed: 19-Jul-2023 / Revised: 24-Jul-2023 / Manuscript No. jnp-23-104142 (R) / Published Date: 31-Jul-2023 DOI: 10.4172/2165-7025.1000606
Introduction
The fascia is a biologic and collagenous fabric layer of collagen that holds the muscles and underlying tissues together. The collagen consists of proteoglycominoglycans, that are glycosaminoglycans linked to core proteins (Bahm, 1995). According to Stahl (2015), the fascia is fibrous and gluey consisting of wet proteins that permit mobility between body parts. The fascia allows muscles to glide against adjacent muscles and ligaments (Rosen, 2008). The fascia slides over the muscle during joint movement. This is termed as sliding mechanism by Gimberteau et al. (2005) and is a polyhedral three-dimensional criss-crossing in space of multiple microvacuoles. This multi-microvacuolar system permits all fine movements to occur within the body. This system is capable of molecular fusion-scission-dilacerations that makes the system mobile and plastic (Guimberteau et al 2005). The Hyaluronic Acid (HA) is in the fluid found between fascia and muscle promoting glide between these fascia and muscle. High molecular weight HA hydrates muscle and fascia keeping them viscous and mobile, reflecting healthy tissues.
Deformed HA is thick and sticky limiting the sliding mechanism between fascia and muscle. The limited sliding mechanism is suggested to be associated to pain and dysfunctions observed in musculoskeletal conditions such as De Quervain’s Tenosynovitis (DQT).
De Quervain’s Tenosynovitis of the first wrist extensor compartment is a common pathology involving the Abductor Pollicis Longus (APL) and Extensor Pollicis Brevis (EPB) (Ilyas, 2007). The tendons are thickened, thus limiting their movement in the tendon sheath, which is formed by the fibers of first dorsal carpal ligament. De Quevain’s Tenosynovitis is associated with increased friction in the first wrist extensor compartment (Ilyas, 2007) associated with functional restrictions needing thumb movement (Bahm, 1995). Repeated thumb movement in DQT entails repeated muscular contractions of EPB and APL against tendon sheaths, which in the long term may lead to tendon inflammation [1-5].
According to Ilyas (2007), attritional forces due to friction can cause first dorsal compartment stenosing tenosynovitis. It produces swelling and thickening of tendon sheaths of APL and EBP, with the extensor retinaculum that covers the first dorsal compartment. In a microanatomic examination reported thickening of the tendon sheaths. The tendon sheath thickening was five times more in diameter than tendon sheath size of participants with non-symptomatic thumbs (Ilyas, 2007). The tendon sheath thickening was described as a deposition of dense fibrous tissue, increased vascularity of tendon sheaths, and accumulation of mucopolysaccharides, which are signs of myxoid degeneration. Thickened tendon sheath could affect the sliding mechanism that exists between fascia and muscle (Ilyas, 2007). Limited sliding mechanism in DQT could lead to thumb pain and dysfunction due to increased tendon friction.
The Finkelstein’s test is the definitive diagnostic test for DQT that replicates characteristic pain of patients. The clinician grasps a client’s thumb and quickly ulnarly deviates the wrist and hand. Finkelstein’s test stretches the tendons of APL and EPB (Kutsumi, 2005). During Finkelstein’s Test with wrist at 30 degrees of ulnar deviation, the EPB tendon was distal and prominent in the wrist (Stecco, 2009), with higher gliding resistance of EPB tendon in the wrist first extensor compartment. The gliding resistance met by tendon could affect the direction of movement of the fascia (Table 2).
The direction of the movement of the fascia can be evaluated using the palpation and musculoskeletal ultrasound. Palpation is a valid and reliable evaluation tool in determining movement of human structures such as fascia, muscle, tendon, and bones (Walsh et. al, 2009). Palpation is an evaluation procedure that aims to feel the human structures and its characteristics. Expertise in Palpation is an extremely helpful diagnostic method in musculoskeletal condition. Palpation of myofascial structures aids the clinician in identifying musculoskeletal abnormalities such as tightness, limitation of motion, trigger and tender points, joint dislocation, and fractures (Razo, 2004). Through palpation, the clinician will have a better understanding of the different layers soft tissue involvement. In the study conducted by J. manual palpation of sciatic, tibial, and common peroneal nerves in the examination of low back related leg pain demonstrated excellent reliability. The nerves were palpated manually, to determine pressure pain threshold. The same study showed highest scores of diagnostic accuracy (sensitivity = 0.83; specificity = 0.73).
Motion Palpation is integral to practitioners of manual therapy, despite the fact that most researches show it to be unreliable, with interexaminer reliability usually found near chance levels of agreement (Cooperstein, 2016). The common reasons for the low reliability of motion palpation include variation in procedure, poor inter-examiner expertise, inaccurate determination of landmarks, and variations in patient anatomy (Cooperstein 2016). The authors of this study used a standardized step by step procedure in the assessment of first wrist extensor compartment (Methodology section).
Musculoskeletal Ultrasound (MSUS) uses sound waves to produce pictures of muscles, fascia, tendons, ligaments, and joints throughout the body. Musculoskeletal ultrasound is safe and painless since it does not use ionizing radiation. It is better than the other scanning devices because images are captured in real-time. Musculoskeletal ultrasound can visualize the structure and movement. Inflammation of tendon sheath may be associated with decreased fascia mobility in the first wrist extensor compartment. No current literature reports on the direction of fascia movement in the first wrist extensor compartment in non-symptomatic thumbs during Finkelstein test. This study aims to determine the direction of fascia movement overlying the first wrist extensor compartment in non-symptomatic thumbs (Stecco, 2015) after the above-mentioned test [6-8].
Methodology
This research project was conducted using a step-by-step and interlinked approach where multiple studies, each with discrete research aims and methods, were utilized to contribute to a broader research objective. Three phases involved in this study were the following:
Phase I: Cadaver dissection
Orientation of the wrist fascia overlying the first wrist extensor compartment.
Fascia-sparing approach was used in cadaver dissection. The skin and superficial fascia of the distal third of the forearm and wrist were dissected and cut off to expose underlying deep fascia. The deep fascia overlying the first dorsal compartment of the wrist was captured using Samsung S7 Edge Phone Camera and Wolf Vision Eye14. The wrist dissection began with an incision on the lateral distal third of the forearm and continued in the base of the nail bed of the thumb. Incision going to the middle posterior distal third of the forearm and to the middle anterior distal third of the forearm was also performed. Skin flaps were raised to expose and traced the orientation or direction of the superficial fascia of the wrist and anatomical snuff box. The superficial fascias were dissected to expose and traced the orientation or direction of the deep fascia of the wrist and anatomical snuff box. The separation of the skin, superficial fascia, and the deep fascia was also noted in the study. The presence of radial artery was also noted. The description of the fascia direction of the study was the the basis of the hand placement and musculoskeletal ultrasound hockey stick placement on wrist of the living healthy participants in the succeeding phases of the study[9,10].
Phase II: Reliability of Sonographers and Physiotherapists in the use of Musculoskeletal Ultrasound and Palpation
Qualitative Descriptive study with an independent, blinded comparison of fascia movement test with MSUS as reference standard among consecutive healthy participants. Ten healthy participants were recruited from General Mariano Alvarez and City of Dasmariñas, province of Cavite from August 1, 2017 to August 31, 2017. The author screened potential participants using the inclusion/exclusion criteria. Inclusion criteria: Women Age 30 – 40, healthy Individual, no wrist pain, no psychological disorder, and should not possess any of exclusion criteria. The exclusion criteria are the following: participants with bilateral wrist radial pain, pregnant women, malignancy, fracture of the involved extremity and neck, osteoarthritis of the wrist and thumb, recent blunt force trauma, recent injury on the hand, previous surgery, any systemic disease known to cause general body malaise, motor vehicular accident. Consenting participants were evaluated using Palpation and Konika Minolta Sonimage HS14 US Imaging System at Research Office of UST-CRS (Table 1).
| MSK (N=60) | Palpation (N=180) | |||||||
|---|---|---|---|---|---|---|---|---|
| n (%) | Proximal | Distal | % Overall Agreement | Proximal | Distal | % Overall Agreement | ||
| Anatomic Snuff box | ||||||||
| Right | 3.33 | 96.67 | 0.93 | 15.00 | 85.00 | 0.78 | ||
| Left | 0 | 100 | 1.00 | 16.67 | 83.33 | 0.76 | ||
| Dorsolateral aspect of the middle 1st MCP | ||||||||
| Right | 5.00 | 95.00 | 0.91 | 21.67 | 78.33 | 0.65 | ||
| Left | 0 | 100 | 1.00 | 33.33 | 66.67 | 0.59 | ||
Number of raters=2; Number of participants=10
N=total number of trials
n=frequency; %= proportion
| Palpation (N=75) | |||
|---|---|---|---|
| n (%) | Proximal | Distal | % Overall Agreement |
| Anatomic Snuff box | |||
| Right | 0 | 75 (100) | 1.00 |
| Left | 0 | 75 (100) | 1.00 |
| Dorsolateral aspect of the middle 1st MCP | |||
| Right | 0 | 75 (100) | 1.00 |
| Left | 0 | 75 (100) | 1.00 |
Number of raters =1; Number of participants=25
N=total number of trials
n=frequency; %= proportion
Procedure
1. Hockey stick probe of MSUS was used for better imaging.
2. The MSUS operators identified first the Lister’s tubercle which was a bony prominence on the dorsal aspect of the radius.
3. The participant was sitting opposite the clinician. The palm of the hand of the participant placed flat on the examination table. The probe was placed in axial position over the Lister’s tubercle.
4. The probe was on radial side of wrist scanning the first wrist dorsal compartment containing Extensor Pollicis Brevis and Abductor Pollicis Longus.
5. Using skin marker, the evaluator marked the tendon of the Extensor Pollicis Longus which is the posteromedial border of the anatomical snuff box and served as landmark. The participant was asked to place her hand in karate chop position. Then the probe was placed in longitudinal position in the anatomic snuff box. The evaluator located the radial pulse and the radial styloid process. The area between the radial pulse and the radial styloid process was observed and appeared on the MSUS screen. Clear view of striations was established first in order to have a better observation of the movement. The image depth on MSUS screen is one.
6. The evaluator asked the participant to bend her thumb down across the palm of the hand, and cover the thumb with the fingers. The participant bent her wrist toward the little finger. While the patient was doing the motion the clinician scanned the wrist while it was moving for several times in order to have accurate images of the fascia movement and continued to observe the movement of the fascia on the location mentioned above.
Results
A: Cadaver dissection results
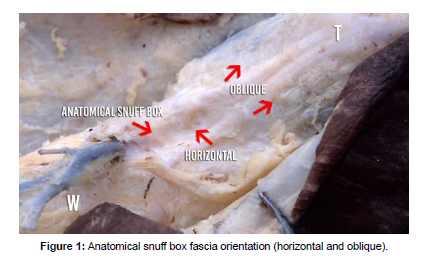
The fascia overlying the anatomical snuffbox was horizontal to the wrist. The fascia was obliquely oriented over the first metacarpal bone, following the muscle fibers of first wrist extensor compartment (Figure 1).
Out of the 60 trials for MSK assessment, at least 96% revealed that in both right and left anatomic snuff boxes the direction of movement of fascia are distal rather than proximal with almost perfect overall agreement (fleiss’ kappa: 0.93) and perfect (fleiss’ kappa: 1.00) agreement, respectively. Although with lower proportion and % over all agreement, the results of MSK were found to be consistent with the results of palpation which revealed substantial agreement for both right (fleiss’ kappa: 0.78) and left (fleiss’ kappa: 0.76) anatomic boxes. As for the dorsolateral aspect of the middle 1st MCP, at least 95% out of the 60 trials for MSK assessment revealed that in both right and left direction of movement of the fascia are distal rather than proximal with almost perfect overall agreement (fleiss’ kappa: 0.91) and perfect (fleiss’ kappa: 1.00) agreement, respectively. This was also found to be consistent with the results of palpation moderate (fleiss’ kappa: 0.59) to substantial (fleiss’ kappa: 0.65) agreement for the left and right landmarks, respectively. Like the results for assessment of anatomic snuff box, percentage overall agreement using palpation compared to MSK was found as well in the assessment of the dorsolateral aspect of the middle 1st MCP.
Three trials were conducted for MSK assessment as well as for Palpation assessment. A total of 60 trials were obtained from MSK and 60 trials were also obtained from palpation. Results gathered from every assessment (either proximal or distal) were added and divided into total number of trials (60) to identify the final direction of movement of the fascia.
Discussion
During the cadaver dissection, the evaluators’ expertise in human anatomy as well as familiarity on the fascia were very significant factors in the outcomes of this study. Mastery of the fascia-sparing approach also contributed to the proper identification of the anatomical orientation of the fascia. The accurate anatomical orientation of the fascia was very significant in the succeeding phases of this research. In this study, ten cadavers were utilized and it was discovered that the fibers of anatomical snuff box fascia are oriented horizontally in relation to the wrist. It was also discovered that after the anatomical snuffbox, the fibers of the fascia became oblique in orientation following the fibers of first extensor compartment muscles. These findings on the cadaver dissection coincide with the description stated in Function Atlas of the Human Fascial System by Stecco (2015). The placement of the palpating thumb of the evaluator as well as the placement of the hockey stick probe of MSUS must be perpendicular to the orientation of the fascia. Improper placement of the palpating thumb of the evaluator and of the hockey stick probe of MSK will have inaccurate results (Salonen, 1993).
According to the literature reviewed in this research, motion palpation (sensitivity= 0.83; specificity = 0.73)(Razo, 2005) and the use of MSUS (sensitivity, 100%; 95% confidence interval [CI]: 74%, 100%)(Choi et al, 2011) were the best methodology in identifying the movement direction of the underlying fascia. There were several factors that could affect the results of palpation and MSUS. This includes knowledge on the anatomical landmarks; length and size of the examined structure; length of range of motion of the structure being examined; years of experience and practice of the evaluator; and familiarity of the evaluator on the structure being examined (Cooperstein, 2016). In this study, a total of 35 subjects were identified to be eligible thru assessment with 10 subjects assigned to Phase II of study and 25 subjects to Phase III. The study revealed that the level of agreement of the examiners both in MSK and palpation is higher in anatomical snuffbox location than the agreement in dorsolateral aspect of the middle 1st MCP. One of the reasons on why there was a higher level of agreement in the anatomical snuffbox is the length of range of motion in this area. Accuracy in identifying the direction of fascia movement through palpation in the dorsolateral aspect of the middle of 1st MCP was difficult due to different muscle bulkiness of the participants. The study also revealed that palpation and MSK have an acceptable level of agreement for all locations, proving precision of the identified direction of movement for each location analyzed, which is distal. Palpation revealed substantial level of agreement while the MSK is almost perfect agreement. For palpation, the result is due to the clinical experience or mastery in palpation of the clinician (McNally, 2008). And for the MSK, expertise in operating the machine as well as the knowledge of the human anatomy will affect the result of the study (Billingham, 2013). Based on the results, palpation and musculoskeletal ultrasound were acceptable evaluation tools. Follow-up study should be done comparing the direction of fascia movement in Finkelstein’s test in symptomatic thumb of DQT patients.
Conclusion
This study involved 70 non-symptomatic wrists of 35 healthy participants. This study revealed that both palpation and MSK have an acceptable level of agreement (0.70 and 0.96, respectively). Palpation and musculoskeletal ultrasound were acceptable evaluation tools in determining the movement of fascia in the first wrist extensor compartment. Therefore, during the Finkelstein’s test, the fascia of the healthy individual’s non-symptomatic thumb overlying the first extensor compartment of the wrist was moving distally or away from the proximal joint. The distal movement of the fascia during Finkelstein test reflected fascia’s normal movement in non-symptomatic thumbs.
References
- Aktan ZA, Oztürk L, Calli IH (1998) An anatomical study of the first extensor compartment of the wrist. Kaibogaku Zasshi 73:49-54.
- Bahm J , Szabo Z , Foucher G (1995) The anatomy of de Quervain’s disease: a study of operative findings . Int Orthop 19 : 209-211 .
- Stahl (2015) Work related etiology of de Quervain’s tenosynovitis: a case-control study with prospectively collected data: BMC Musculoskeletal Disord 16:126
- Stecco A, Gesi M, Stecco C, Stern R (2013).Fascial components of the myofascial pain syndrome. Curr Pain Headache Rep17:352-359.
- Kutsumi K, Amadio PC, Zhao C, Zobitz ME, Tanaka T ,et al.(2005) Finkelstein’stest: A biomechanical analysis. J Hand Surg 30:130-135.
- Razo, David (2004) Athletic injuries of the wrist and hand. Part II: overuse injuries of the wrist and traumatic injuries to the hand. Am J Sports Med 32:262–273.
- Walsh J (2009) Reliability, validity, and diagnostic accuracy of palpation of the sciatic, tibial, and common peroneal nerves in the examination of low back related leg pain. Man Ther 14: 623-629.
- Lipscomb PR (1951) Stensosing Tenosynovitis at the Radial Styloid Process: Ann Surg 134:110-115.
- Minamikawa Y , Peimer CA , Cox WL , Sherwin FS (1991) De Quervain’s syndrome: surgical and anatomical studies of the fi broosseous canal . Orthopedics 14: 545-549 .
- Iagnocco A (2012) The reliability of musculoskeletal ultrasound in the detection of cartilage abnormalities at the metacarpo-phalangeal joints . 20:1142-1146
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Patrick L (2023) Direction of Fascia Movement in Finkelstein Test in Non- Symptomatic Thumbs of Healthy Individuals. J Nov Physiother 13: 606. DOI: 10.4172/2165-7025.1000606
Copyright: © 2023 Patrick L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1002
- [From(publication date): 0-2023 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 774
- PDF downloads: 228