Digital Health Technology in Cardiovascular Disease Prevention and Rehabilitation
Received: 27-Jun-2022 / Manuscript No. jcpr-22-67694 / Editor assigned: 29-Jun-2022 / PreQC No. jcpr-22-67694 (PQ); / Reviewed: 13-Jul-2022 / QC No. jcpr-22-67694 / Revised: 18-Jul-2022 / Manuscript No. jcpr-22-67694 (R) / Published Date: 25-Jul-2022 DOI: 10.4172/jcpr.1000168
Abstract
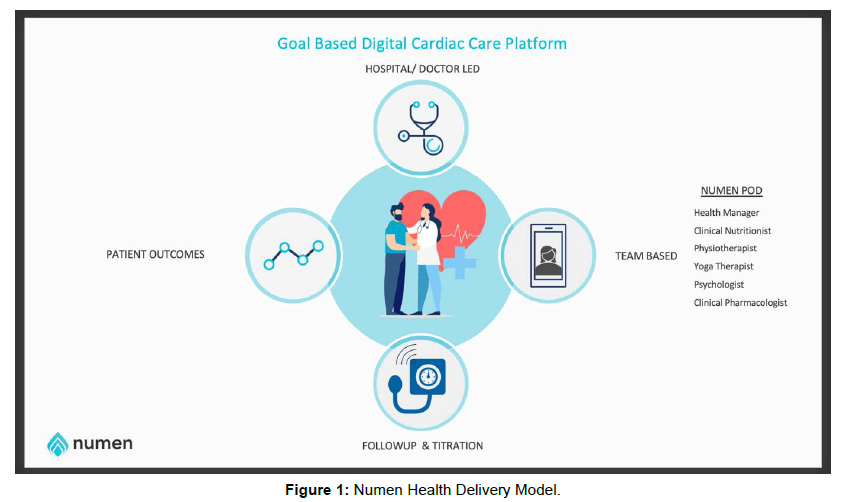
Cardiovascular diseases remain the number one cause of mortality across the world. Nearly 80% of the global cardiovascular-related deaths happen in developing countries. Modifiable risk factors for a cardiovascular event are common knowledge. Implementing a continuous care model that modifies these risk factors is nearly impossible with current healthcare delivery models. Non-therapeutic interventions are more easily adapted with constant nudging, regular feedback, and simple strategies to overcome perceived barriers to living a healthy lifestyle.Numen Health is a digital health platform that provides a practicing cardiovascular disease physician or surgeon with an extended multidisciplinary team to deliver multifaceted interventions. All the interventions target reducing risk factors that cause cardiovascular event and the whole program focuses on lowering mortality, re-hospitalization, and improved quality of life for survivors.
Keywords
Digital health technology; Cardiovascular Disease; Rehabilitation; Cardiology
Introduction
In 2019, as per the Global Burden of Disease, the cardiovascular disease (CVD) prevalence was 523 million (95% uncertainty interval (UI):497 to 550). It has nearly doubled in three decades, from 1990 to 2019. It remains the number one cause of mortality and disabilityadjusted life years. 18.6 million deaths (95% UI: 17.1 to 19.7 million) in 2019, with global trends for Disability Adjusted Life Years (DALYs) and Years of life lost (YLLs) increasing significantly, and Years of living with disability (YLDs) doubling; 17.7 million (95% UI: 12.9 to 22.5 million) to 34.4 million (95% UI: 24.9 to 43.6 million) in the same period.
India has the highest burden of CVD deaths, 272 per 100,000 population (an increase of 138% compared to 1990), much higher than 235 per 100,000 globally [1, 2]. Among all the CVDs, hypertensive heart disease, a preventable and reversible CVD, was responsible for 261,694 deaths in 2013 [3]. India recorded the highest cumulative excess deaths during the pandemic; 4.07 million (3·71-4·36) [4]. The pandemic has exposed the vulnerability of people with comorbidities, especially uncontrolled hypertension, diabetes, sub-clinical coronary artery disease, and obesity [5].
India requires an urgent infusion of technology into healthcare delivery to meet the growing burden of CVD death and disability. Adopting digital health during the pandemic is proof of its efficiency and effectiveness in delivering continuous care to patients in need of chronic disease management [6-9]. Transactional healthcare delivery cannot meet the growing burden of CVD risk factor management and having a reactive healthcare system will not impact mortality and disability rates in India [10].
Numen Health by Anantam technologies India (https:// numenhealth.com/) connects thousands of CVD patients with registered health experts who monitor and provide preventive and rehabilitative services. The multidisciplinary team supports the treating physician in continuing the patient’s care at their homes. Numen’s digital technology is available via a mobile application that inputs data from the patient on their health vitals and outputs valuable insights into what action they need to do. All of the communications occurring on the application are available in real-time to the physician. In this paper, we will elaborate on the role of digital health in CVD care and how Numen Health fits into this evolving domain.
Digital Health in Chronic Disease Care
Traditional healthcare delivery is transactional, with the doctor at the center and the other stakeholders supporting [11]. The patient does not get an opportunity to participate and thus feels less responsible for their health [12]. Behavior modification requires constant nudging with encouragement, which is impossible with the overburdened doctor-based clinic currently managing chronic conditions. Therefore, risk factor exposure continues to rise with each decade of life, and we see increasing disability living due to chronic diseases at a very young age [13].
Managing chronic diseases between doctor’s appointments through seamless and continuous care can help lower hospital admissions and emergency interventions [14]. At the same time, the advent of smartphones, cloud computing, and global connectivity has created a universe of consumers accustomed to everything from checking bank balances, making purchases, and watching movies on mobile devices. Increasingly, those consumers wonder why health systems cannot provide similar service innovations [15].
In that respect, digital-health companies would appear to be best positioned: innovation is in their DNA, they have attracted billions of dollars in venture capital, and they have the flexibility to design applications that cater directly to patient groups. Yet digital-health companies have been impeded by a lack of access to health data and uncertainty about distributing the economic benefits generated by smartphone applications [16].
Digital health systems can be defined as tools that manage chronic conditions in various ways. It is a booming health care system, and this rapid growth is mainly driven by the urgent need to manage chronic diseases, particularly after the COVID-19 pandemic [16]. Digital healthcare systems can potentially address the failures of traditional treatments and therapies by efficiently sharing information with patients, providers and decision-makers, overcoming the barrier of geographic location to expand access to health care, delivering personalized care more precisely; reducing travel and treatment costs, improving compliance and patient adherence; and enabling remote monitoring of patients [17, 18].
However, focusing on the direct clinical effect of digital technology on patients is often overlooked [19]. Digital health systems are divided into several categories according to the objectives and criteria. These include telehealth and telemedicine, medical education, digital diagnosis or decision-making tools, devices to regulate or improve physiological functions, health informatics etc., [20]. From the patient’s perspective, digital health technologies offer valuable resources for developing self-management skills using diverse online platforms and mobile and wearable devices. Digital health technologies have already created many new opportunities to change the future of primary health care and ensure successful public health management [21].
Despite the potential of healthcare delivery, the implementation and sustainability of digital healthcare interventions is not an easy task. Creating a universal "digital prescription" for managing chronic diseases is challenging due to people’s variable socio-cultural and economic status and other countries' different laws and policies regarding adopting digital health care interventions [22]. Besides, digital health interventions are very complex, and their practical implementation is very challenging due to various factors such as reliability/technical stability of electronic sensors and data transmissions; transparency of algorithms for autonomous decisions; access and usability; reorganization of workflow/infrastructure; poor implementation planning and security threats in data transmission and storage [23-25].
However, descriptions of specific implementation strategies in the literature are limited and poorly reported. Sketchy details of the implementation process can restrict replication and scale-up and make it difficult for implementation researchers and other stakeholders [26]. Due to these barriers, only a limited number of successful, evidencebased digital health interventions are beyond the pilot or feasibility stage. Many studies have investigated the efficacy of digital health applications for chronic diseases such as cardiovascular diseases, cancers, chronic respiratory diseases, diabetes mellitus, chronic kidney diseases, and skin diseases [27]. The efficacy of these digital health applications was assessed using different disease control outcome measures, such as rate of unplanned hospital admissions or clinic visits, symptom assessments, adverse events, exercise capacity, diseaserelated mortality, self-efficacy, quality of life assessment, and economic outcomes. The results of most of these studies were mixed, or the existing studies had no clinical effects [28]. The most significant aspect that influences the efficacy of these treatments is the monitoring and evaluation methodology used to measure progress, identify problems, and support adjustments to improve service delivery and achieve intended goals [29]. Many efforts have also been made to leverage data to improve health information exchange and care coordination. Still, unfortunately, these efforts are significantly fragmented and providercentric rather than patient-centric [30]. Though the use of digital technologies in chronic disease management is still in its early stages, extensive ongoing research and continuous efforts in this field may lead to the introduction of evidence-based digital health applications for chronic disease management, which could be significant disruptors to healthcare markets in the coming years.
Numen Health - A Virtual Home-Based Cardiac Rehabilitation Platform
Figure 1 illustrates the model adopted by Numen Health. The patient is the central focus, and the doctor is connected with the multidisciplinary team who delivers nutritional advice, medication counseling, mental wellness, and physiotherapy, including yoga. This reduces the cognitive load of the doctor, who is expected to remember and manage the complex variations of presentations among patients. Stereotypical approaches to managing chronic diseases can only achieve treatment goals and not improve holistic health outcomes. Numen Health provides personalized goal-oriented interventions that integrate seamlessly with the treatment objectives (Figure 1).
Patients get enrolled in the program by being referred by their treating doctor. A self-enrollment is also possible through the web portal. Downloading the mobile application on the app store initiates the patient’s journey on the platform. Doctors who refer get to see their patients on a dedicated doctor’s application. The referral process is straightforward and can be completed quickly. A dedicated team of health experts receives the referral details, and the patient needs to provide formal consent to initiate their journey on the program. During this consent process, the details of the program and its expected duties are clearly explained. The patient provides consent by signing an online acceptance form and making the payment for the subscribed program. The programs are broadly divided into Preventive and Recovery; preventive is optimizing risk factors and reversing the early stages of diabetes or hypertension. Recovery follows any acute cardiovascular event or hospitalization and requires rehabilitation. Every subscriber has a preliminary assessment for base lining their health status. All available clinical information, history, and medical records are assimilated into a profile summary. The objectives and interventions offered in the home-based cardiac rehabilitation follows the American Heart Association scientific statement [31]. This summary is further tagged for future reference and goal setting.
Common threads used for tagging include; age group (young, middle-aged, elderly), body habitus (normal, overweight, obese), significant medical history (menopausal, dyslipidemia, hypertension, Type 2 diabetes), cardiovascular disease type (Ischemic heart disease, Heart failure type, Valvular heart disease etc.,) coronary interventions performed (post coronary artery bypass graft, post percutaneous transluminal coronary angioplasty). The participation goals are developed in consultation with the treating / referring physician and the patient with inputs from their immediate caregivers. These goals are categorized as primary and secondary. The primary goals will focus on the available diagnosis of the patient, while the secondary goals will focus on other symptoms and outcomes experienced/perceived by the patient (Table 1).
| Medical Condition | Accepted Health Goals | Age category | Proposed Program duration |
|---|---|---|---|
| Hypertension | Hypertension Remission: Blood pressure ≤130/80 | Adults ≥18 years | 3-12 months |
| Diabetes | Diabetes control: HbA1c ≤6.5% | Adults ≥18 years | 6-12 months |
| Ischemic Heart Disease – post acute coronary syndrome | Avoid re-hospitalization Angina free life | Adults ≥18 years | 6-12 months |
| Heart Failure | Increase longevity Improve the quality of life Control Breathlessness Avoid re-hospitalization |
Adults ≥18 years | 12 months |
| Post Coronary Artery Bypass Graft surgery | Wound care-avoid infection Prevent re-hospitalization | Adults ≥18 years | 6-12 months |
| Post percutaneous Transcatheter coronary angioplasty | Prevent bleeding Angina free life Risk factor control |
Adults ≥18 years | 6-12 months |
| Post intracardiac implants procedure (having a pacemaker, cardiac resynchronization (CRT), or implantable cardiac defibrillator (ICD) | Wound care-avoid infection Anxiety management Improved exercise capacity, quality of life |
Adults ≥18 years | 6 months |
| Post cardiac transplant surgery | Anxiety management Increase exercise capacity Improve overall quality of life |
Adults ≥18 years | 12 months |
Table1: Disease Category for virtual cardio-metabolic disease rehabilitation.
Challenges with Acceptance of Digital Health
During the last two decades, mobile phone penetration has exponentially grown in South Asian countries, with India having the highest penetration, 55% in 2018 [8]. Healthcare delivery models using mobile phone applications have been studied in various chronic illnesses, including CVD prevention and rehabilitation [9, 32]. However, the acceptance of digital health in mainstream healthcare services remain very nascent. The challenges range from affordability, ethics, integration, and validation. Healthcare is expensive and has the lowest priority in spending on preventive and rehabilitation services. Nearly 18% of Indians experience catastrophic healthcare expenditure leading them into extreme poverty after a significant illness or hospitalization [33]. Literacy on data privacy is low, and systems for protecting privileged health information are evolving [34, 35]. This creates a lacuna in understanding the ethical boundaries of sharing health information for effective digital health interventions. Healthcare data digitization resources and wireframes for integration are in their infancy stage. This is an opportunity for new technologies, but the process is prolonged and impedes hospitals’ adoption of digital technology in their health care delivery [36]. Evidence of digital health interventions and mobile-based online health interventions to provide cardiac rehabilitation is emerging at frequent intervals [7, 32, 37, 38].
Barriers to Adopting Rehabilitation and Preventive Programs
The reasons for refusal to rehabilitation and preventive programs after being referred by their treating doctors are broadly categorized as; lack of time, feeling they can do it alone, and affordability (finance and logistic feasibility) [39].
Acceptance rates for joining a digital online rehabilitative healthcare platform are based on convenience and affordability. Doctors do not insist on the need for rehabilitation, fearing their weaning of interest to follow-up and intake of medications. Some also leave the choice to the patient, who often compares the virtual sessions as equivalent or inferior to seeing the doctor in their clinic. Similar perceptions were reported in a recent survey among doctors [7] and patients [40]. Technology is an essential facilitator for connecting patients to rehabilitative services with their doctor oversight but could also become a barrier by overburdening the user with frequent interactions [41, 42].
Conclusion
Digital health platforms have emerged as solutions to enhance the quality and access of healthcare, especially in chronic disease care. CVD causes premature mortality and disability in disproportionate ways across socio-demographic spheres. Imbalances in the social determinants of health have been attributed to the inequities in health observed between and within countries [43]. Affordable and evidence-based programs delivered through a mobile phone have engaged various CVD patients worldwide [6, 44]. Mobile phone-based interventions modify behaviour among patients with CVD risk factors and disease outcomes. They can improve medication adherence, reduce anxiety and optimize risk factor levels in various populations spread across diverse socio-demographic locations [6, 38, 45, 46]. Digital health platforms like Numen Health can offer access to patients for conveniently adopting evidence based secondary prevention and cardiac rehabilitation following a coronary artery event or an intervention. Even patients with emerging risk factors for developing acute coronary events could experience a positive change in their attitude, awareness, behaviour, and approach. More research is needed to measure its effectiveness in delivering evidence-based healthcare in India. The COVID-19 pandemic is creating the necessary change for adopting digital healthcare globally and in India. We believe that technology combined with human interphase for rehabilitative services can reduce CVD prevalence's growth rate.
Competing Interests
Dr. Alben Sigamani is the founding partner and chief scientific officer at Numen Health Bangalore. He declares no non-financial conflict of interest but a financial conflict of interest as he receives a consultation fee and is invested in private equity at Anantam Technologies.
Dr. Rajeev Gupta declares no Competing Financial or Non- Financial Interests.
Pallav Singh is the Founder and CEO for Anantam Technologies and declares a financial conflict of interest in the company.
Data Availability
The data supporting this paper's findings are available from the corresponding author, [Dr. Alben Sigamani, dralbens@numenhealth. com], upon reasonable request.
Author Contributions
Dr. Alben Sigamani, the corresponding author, conceived the ideas for the paper, wrote the first draft of the article, and finalized the entire manuscript for submission to the journal.
Dr. Rajeev Gupta, the Co-Author, contributed by providing valuable insights into the epidemiology of cardiovascular disease in India and helped edit and finalize the manuscript.
Pallav Singh has contributed to editing the drafts of the paper and is involved in the operations of the program.
References
- Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E et al. (2020) Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J Am Coll Cardiol 76: 2982-3021.
- Prabhakaran D, Jeemon P, Roy A (2016) Cardiovascular Diseases in India: Current Epidemiology and Future Directions. Circulation 133: 1605-1620.
- Gupta R, Xavier D (2018) Hypertension: The most important non communicable disease risk factor in India. Indian Heart J 70: 565-572.
- Wang H, Paulson KR, Pease SA, Watson S, Comfort H et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet 399: 1513-1536.
- Phelps M, Christensen DM, Gerds T, Fosbøl E, Torp-Pedersen C et al. (2021) Cardiovascular comorbidities as predictors for severe COVID-19 infection or death. Eur Heart J Qual Care Clin Outcomes 7: 172-180.
- Cruz-Ramos NA, Alor-Hernández G, Colombo-Mendoza LO, Sánchez-Cervantes JL, Rodríguez-Mazahua L et al. (2022) mHealth Apps for Self-Management of Cardiovascular Diseases: A Scoping Review. Healthcare (Basel) 10: 322.
- Dalal HM, Doherty P, McDonagh ST, Paul K, Taylor RS (2021) Virtual and in-person cardiac rehabilitation. BMJ 373: n1270.
- Elliott R (2020) Mobile Penetration in South Asia and Southeast Asia.
- Feinberg L, Menon J, Smith R, Rajeev JG, Kumar RK et al. (2017) Potential for mobile health (mHealth) prevention of cardiovascular diseases in Kerala: A population-based survey. Indian Heart J 69: 182-199.
- Kumar AS, Sinha N (2020) Cardiovascular disease in India: A 360 degree overview. Med J Armed Forces India 76: 1-3.
- King MW (2017) Health Care Efficiencies: Consolidation and Alternative Models vs. Health Care and Antitrust Regulation - Irreconcilable Differences? Am J Law Med 43: 426-467.
- Sobhi E, Moghaddam H R, Soola AH (2022) Challenges and Facilitators of Health Literacy in Patients with Acute Coronary Syndrome: a Qualitative Study. Ann Ig 34: 326-343.
- Deckersbach T, Das SK, Urban LE, Salinardi T, Batra P et al. (2014) Pilot randomized trial demonstrating reversal of obesity-related abnormalities in reward system responsivity to food cues with a behavioral intervention. Nutr Diabetes 4: e129.
- Seixas AA, Olaye IM, Wall SP, Dunn P (2021) Optimizing Healthcare Through Digital Health and Wellness Solutions to Meet the Needs of Patients With Chronic Disease During the COVID-19 Era. Front Public Health 9: 667654.
- Morcos R (2020) How Telehealth And Mobile Devices Work Hand In Hand To Increase Health Outcomes.
- Cummins N, Schuller BW (2020) Five Crucial Challenges in Digital Health. Front Digit Health 2: 536203.
- Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC (2021) Digital Transformation in Healthcare: Analyzing the Current State-of-Research. J Bus Res 123: 557-567.
- Lear SA, Norena M, Banner D (2021) Assessment of an Interactive Digital Health–Based Self-management Program to Reduce Hospitalizations Among Patients With Multiple Chronic Diseases: A Randomized Clinical Trial. JAMA Network Open 4: e2140591.
- Kuwabara A, Su S, Krauss J (2019) Utilizing Digital Health Technologies for Patient Education in Lifestyle Medicine. Am J Lifestyle Med 14: 137-142.
- Vansimaeys C, Benamar L, Balagué C (2021) Digital health and management of chronic disease: A multimodal technologies typology. Int J Health Plann Manage 36: 1107-1125.
- WHO (2021) Global strategy on digital health 2020-2025.
- Szinay D, Jones A, Chadborn T, Brown J, Naughton F (2020) Influences on the Uptake of and Engagement With Health and Well-Being Smartphone Apps: Systematic Review. J Med Internet Res 22: e17572.
- Majumder S, Mondal T, Deen MJ (2017) Wearable Sensors for Remote Health Monitoring. Sensors (Basel) 17: 130.
- Gurupur VP, Wan TTH (2017) Challenges in implementing mHealth interventions: a technical perspective. Mhealth 3: 32.
- von Huben A, Howell M, Howard K, Carrello J, Norris S (2021) Health technology assessment for digital technologies that manage chronic disease: a systematic review. Int J Technol Assess Health Care 37: e66.
- Ross J, Stevenson S, Dack C, Pal K, May C et al. (2018) Developing an implementation strategy for a digital health intervention: an example in routine healthcare. BMC Health Serv Res 18: 794.
- Fan K, Zhao Y (2022) Mobile health technology: a novel tool in chronic disease management. Intell Med 2: 41-47.
- Safavi K, Mathews SC, Bates DW, Dorsey ER, Cohen AB (2019) Top-Funded Digital Health Companies And Their Impact On High-Burden, High-Cost Conditions. Health Aff (Millwood) 38: 115-123.
- Mitchell M, Kan L (2019) Digital Technology and the Future of Health Systems. Health Syst Reform 5: 113-120.
- Baird A, Nowak S (2014) Why primary care practices should become digital health information hubs for their patients. BMC Fam Pract 15: 190.
- Thomas RJ, Beatty AL, Beckie TM, Brewer LC, Brown TM et al. (2019) Home-Based Cardiac Rehabilitation: A Scientific Statement From the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 140: e69-e89.
- Abaza H, Marschollek M (2017) mHealth Application Areas and Technology Combinations*. A Comparison of Literature from High and Low/Middle Income Countries. Methods Inf Med 56: e105-e122.
- Loganathan K, Deshmukh PR, Raut AV (2017) Socio-demographic determinants of out-of-pocket health expenditure in a rural area of Wardha district of Maharashtra, India. Indian J Med Res 146: 654-661.
- Sinha S (2018) Annual Consumer Survey On Data Privacy In India 2018.
- Mireku KK, Zhang F, Komlan G (2017) Patient knowledge and data privacy in healthcare records system. IEEE 154-159.
- Gudi N, Lakiang T, Pattanshetty S, Sarbadhikari S N, John O (2021) Challenges and prospects in india's digital health journey. Indian J Public Health 65: 209-212.
- Guo Y, Hong YA, Qiao J, Xu Z, Zhang H et al. (2018) Run4Love, a mHealth (WeChat-based) intervention to improve mental health of people living with HIV: a randomized controlled trial protocol. BMC Public Health 18: 793.
- Lear SA, Singer J, Banner-Lukaris D, Horvat D, Park JE et al. (2014) Randomized Trial of a Virtual Cardiac Rehabilitation Program Delivered at a Distance via the Internet. Circ Cardiovasc Qual Outcomes 7: 952-959.
- Thompson DR, Ski CF, Clark AM (2019) Cardiac rehabilitation and secondary prevention: Wrong terms, aims, models and outcomes? Eur J Prev Cardiol 26: 995-997.
- Dibbelt S, Schaidhammer M, Fleischer C, Greitemann B (2010) Patient-Doctor Interaction in Rehabilitation: is there a relationship between Perceived interaction quality and long term treatment results? Rehabilitation (Stuttg) 49: 315-325.
- Mendell J, Bates J, Banner-Lukaris D, Horvat D, kang B et al. (2018) What Do Patients Talk About? A Qualitative Analysis of Online Chat Sessions with Health Care Specialists During a "Virtual" Cardiac Rehabilitation Program. Telemed J E Health 25: 71-78.
- Tadas S, Coyle D (2020) Barriers to and Facilitators of Technology in Cardiac Rehabilitation and Self-Management: Systematic Qualitative Grounded Theory Review. J Med Internet Res 22: e18025.
- Kreatsoulas C, Anand SS (2010) The impact of social determinants on cardiovascular disease. Can J Cardiol 26 Suppl C: 8C-13C.
- Shan R, Ding J, Plante TB, Martin SS (2019) Mobile Health Access and Use Among Individuals With or At Risk for Cardiovascular Disease: 2018 Health Information National Trends Survey (HINTS). J Am Heart Assoc 8: e014390.
- Fujita S, Pitaktong I, Steller GV, Dadfar V, Huang Q et al. (2018) Pilot study of a smartphone application designed to socially motivate cardiovascular disease patients to improve medication adherence. Mhealth 4: 1.
- Dale LP, Dobson R, Whittaker R, Maddison R (2016) The effectiveness of mobile-health behaviour change interventions for cardiovascular disease self-management: A systematic review. Eur J Prev Cardiol 23: 801-817.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Sigamani A, Gupta R, Singh P (2022) Digital Health Technology in Cardiovascular Disease Prevention and Rehabilitation. J Card Pulm Rehabi 6: 168. DOI: 10.4172/jcpr.1000168
Copyright: © 2022 Sigamani A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2747
- [From(publication date): 0-2022 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 2348
- PDF downloads: 399