Case Report Open Access
Diarrhea and Symptomatic Coagulopathy: An Uncommon Presentation of Celiac Disease
Marta Eusébio1*, Paulo Caldeira1, Carlos Cabrita2, André Ramos1, Jesús Cadillá3 and Horácio Guerreiro1
1Gastroenterology Departament, Centro Hospitalar do Algarve, EPE, Rua Leão Penedo, 8000-386 Faro, Portugal
2Internal Medicine Department, Centro Hospitalar do Algarve, EPE, Rua Leão Penedo, 8000-386 Faro, Portugal
3Pathology Department, Centro Hospitalar do Algarve, EPE, Rua Leão Penedo, 8000-386 Faro, Portugal
- *Corresponding Author:
- Marta Soares dos Santos Eusébio
Gastroenterology Department
Centro Hospitalar do Algarve EPE, Rua Leão Penedo
8000-386 Faro, Portugal
Tel: +351 919186736
E-mail: martaeusebio@gmail.com
Received date: November 19, 2015, Accepted date: December 1, 2015, Published date: December 08, 2015
Citation: Eusébio M, Caldeira P, Cabrita C, Ramos A, Cadillá J, et al. (2015) Diarrhea and Symptomatic Coagulopathy: An Uncommon Presentation of Celiac Disease. J Gastrointest Dig Syst 5:358. doi:10.4172/2161-069X.1000358
Copyright:© 2015 Eusebio M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
A 39 year-old female was admitted to the emergency department due to watery diarrhea and weight loss for 3 weeks. Over the last days she also presented menorrhagia and vomiting. Physical examination revealed skin paleness and slight dehydration. Laboratory investigation showed microcytic anemia (hemoglobin 10,6 g/dL), multiple nutricional deficiencies and hypertransaminasemia (aspartate aminotransferase 120 UI/L and alanine aminotransferase 201 UI/L). International normalized ratio was greatly increased (11,87: more than 10 times the upper limit of normal) as well as activated partial thromboplastin time (100 seconds). Additional studies were positive for increased antitissue transglutaminase (above 300 UA/mL) and attenuation of duodenal villous pattern on upper endoscopy. Duodenal biopsies confirmed celiac disease. Coagulopathy was treated with vitamin K intravenously with normalization of coagulation assays. Following a gluten-free diet the patient became asymptomatic with no bleeding recurrence and achieved laboratory and histological recovery. Despite being a well-characterized disorder, celiac disease remains under diagnosed. This case highlights the several manifestations of celiac disease that may trigger the diagnosis. Furthermore, bleeding due to vitamin K malabsorption is a rare complication of the disease and is herein presented.
Keywords
Celiac disease;Coagulopathy;Malabsorption; Hypovitaminosis K
Introduction
Celiac disease is one of the most common lifelong disorders in Europe and United States of America [1,2]. Patients often present with gastrointestinal symptoms including altered bowel habits, abdominal pain and weight loss [3,4]. Extra-intestinal manifestations such as anemia, osteoporosis, short stature or peripheral neuropathy have been increasingly recognized and may dominate clinical presentation in adults [3,5,6]. Hemorragic presentations due to coagulopathy are, however, quite rare [5-8]. A patient with bleeding due to severe coagulopathy is presented. Celiac disease was suspected as there was evidence of malabsorption.
Case Report
A 39 year-old female presented to the emergency department with a history of diarrhea, weight loss (7 Kg), progressive fatigue and anorexia for 3 weeks. She reported between 5 to 6 daily episodes of bulky, watery and nonbloody diarrhea. 3 days before the admission she started vomiting and noticed menorrhagia.
She denied abdominal pain, fever, other blood losses namely melena or hematuria, spontaneous bruising or other symptoms. There was no history of recent travels or sick contacts.
Her past medical history was unremarkable. She had a regular diet and denied any medications or alcohol abuse.
Physical examination revealed skin paleness and slight dehydration. There were no bruises, cutaneous stigmata of liver disease, peripheral edema or other relevant findings on examination.
Laboratory investigation showed: hemoglobin 10.6 g/dL (normal: 12-16), mean corpuscular volume 65 fL (normal: 83-101), mean corpuscular hemoglobin 20 pg (normal: 27-32); leucocytes 3700/uL (normal: 4000-10000), platelets 412000/uL (normal: 150000-400000), serum potassium 2,5 mmol/L (N: 3.6-5.1), magnesium 1.3mg/dL (N: 3.6-5.1), phosphorus 2.7 mg/dL (N: 2.3-4.7), corrected calcium 9 mg/dL (N: 8.8–10); albumin 2.0 g/dL (N: 3.4-4.8), total protein 4,3 g/dL (N: 6.2-8.5), aspartate aminotransferase 120 UI/L (N: 5-34), alanine aminotransferase 201 UI/L (N <55) and protein C-reaction 7 mg/L (N: <5 mg/L). The prothrombine time (PT) was increased (143,4 seconds; N: 9.4-13; international normalized ratio of 11.87) as well as activated partial thromboplastin time (aPTT) (100 seconds; N: 20-40).
Subsequent analysis revealed: serum iron 20 ug/dL (normal: 40-145), ferritin 11 ng/mL (normal: 15-160), B12 vitamin 166 pg/mL (normal: 200-900), folic acid 1.2 ng/mL (normal: 3-17).
Celiac serology showed antitissue transglutaminase above 300 UA/mL (normal: <15). Other laboratory work-up was unremarkable including bilirubin, alkaline phosphatase, gamma-glutamyl transpeptidase, cholesterol, triglycerides, thyroid function tests, serology for human immunodeficiency virus, hepatitis serology and liver autoimmune panel. Bleeding time and fibrinogen were also normal. Abdominal ultrasound was unrevealing.
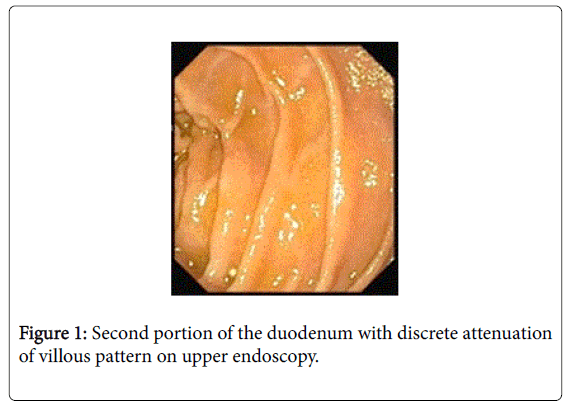
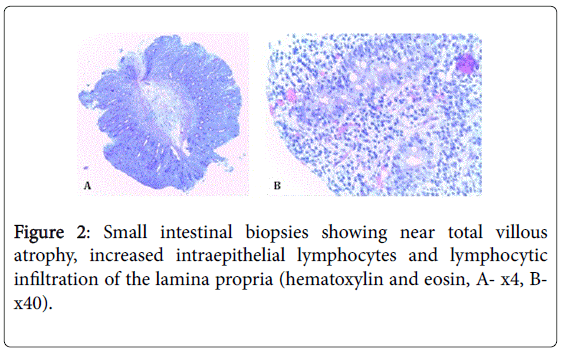
Upper endoscopy evidenced a discrete attenuation of duodenal villous pattern without other findings (Figure 1). Histopathological examination of duodenal biopsies showed near total villous atrophy, increased intraepithelial lymphocytes and lymphocytic infiltration in the lamina propria (Figure 2). These findings were consistent with celiac disease.
She was started on a gluten free diet. Coagulopathy was treated with vitamin K intravenously with immediate normalization of the PT and aPTT. Replacement of electrolytes was done as well as oral B12 vitamin and folic acid. During the hospital stay, menorrhagia was documented initially associated with a decrease in the hemoglobin level (8,4 g/dL) with good response to intravenous iron.
One week after hospital admission, the patient was discharged asymptomatic on a gluten free diet.
At 3 and 12 months follow-up, she remained asymptomatic with regular menstruations, no recurrent bleeding or diarrhea. There was also full normalization of laboratory tests (hemoglobin, iron studies, electrolytes, albumin, TP, aPTT, aminotransferases, vitamins) and negativity of celiac serology. Upper endoscopy was repeated at 12 months and showed marked improvement with only slight villous atrophy.
Discussion
Celiac disease or gluten-sensitive enteropathy is an autoimmune disorder triggered by dietary gluten that primarily affects the small intestine in subjects with a genetic predisposition [6,9]. It may appear at any age and can present with a wide variety of clinical symptoms or signs [3,9]. This enteropathy is one of the most common causes of malabsorption characterized by diarrhea, steatorrhea, weight loss, failure to thrive or multiple deficiencies of macronutrients and micronutrients. This results from injury to the small intestine with loss of absorptive surface area, reduction of digestive enzymes and consequential impaired absorption [9].
Anemia secondary to malabsorption of iron, folic acid, and/or vitamin B12 is the most common hematologic manifestation of celiac disease, which may also be associated with thrombocytosis and leukopenia, as in our case. Malabsorption of vitamin K can occur causing a decrease in K vitamin-dependent coagulation factors. This results in prolongation of coagulation assays namely the PT, INR and aPTT [10]. In fact, prolonged TP has been found in up to 20% of untreated adult cases [11]. However, overt bleeding has been rarely described [5-8].
Our case refers to a patient with celiac disease presenting with signs and symptoms of malabsorption as evidenced by multiple nutritional deficits including electrolyte imbalance, low serum iron, vitamin B12, folic acid and reduced serum albumin. Moreover the patient presented with symptomatic coagulopathy in the form of menorrhagia associated with a severe prolongation of PT, INR (more than 10 times the upper limit of normal) and aPTT, which is a rare manifestation of the disease. The abnormality of both the PT and aPTT, as seen in our case, could indicate either abnormalities of multiple coagulation factors or, less commonly, a deficiency or presence of inhibitors of the common pathway factors II, V, X or fibrinogen. Our patient was not taking vitamin K antagonists, denied a “super-warfarin” rodenticide ingestion and had no evidence of liver disease, biliary obstruction or disseminated intravascular coagulation. The association of symptoms and other signs of malabsorption suggested that the mechanism of this coagulopathy was malabsorption of vitamin K. In the majority of cases, hypoprothrombinemia presents with echymosis and hematomas, which were not present in our case [5]. Instead, menorrhagia was noticed causing a decrease in hemoglobin level.
Furthermore, our patient presented hypertransaminasemia, which is the most common liver abnormality in patients with celiac disease [12]. One proposed explanation for hepatic involvement in these patients is that the increased intestinal permeability may ease the entry of toxins, antigens, and inflammatory substances (cytokines and/or autoantibodies) to the portal circulation that, subsequently, play a role in liver injury [13].
The positive serology for celiac disease and the documentation of villous atrophy on histopathological analysis confirmed the clinical suspicion. Marked clinical improvement without recurrence of bleeding associated with normalization of the laboratory abnormalities and histological recovery after gluten withdrawal was consistent with the diagnosis.
The authors present this case as it represents a good clinical picture of celiac disease including symptomatic hypovitaminosis K, which is a rare complication of the disease. This diagnosis must be kept in mind of the clinicians specially if gastrointestinal symptoms coexist.
References
- Fasano A, Berti , Gerarduzzi T, Not T, Colletti RB, et al. (2003) Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med 163: 286-292.
- Catassi C, Fabiani E, Rätsch IM, Coppa GV, Giorgi PL et al. (1996) The coeliac iceberg in Italy. A multicentre antigliadin antibodies screening for coeliac disease in school-age subjects. Acta Paediatr Suppl 412: 29–35.
- Castillo NE, Theethira TG, Leffler DA (2015) The present and the future in the diagnosis and management of celiac disease. Gastroenterol Rep (Oxf) 3: 3-11.
- McNicholas BA, Bell M (2010) Coeliac disease causing symptomatic hypocalcaemia, osteomalacia and coagulapathy. BMJ Case Rep.
- Chen CS, Cumbler EU, Triebling AT (2007) Coagulopathy due to celiac disease presenting as intramuscular hemorrhage. J Gen Intern Med 22: 1608-1612.
- Kostovski A, Zdraveska N (2011) Coagulopathy as initial manifestation of concomitant celiac disease and cystic fibrosis: a case report. J Med Case Rep 5: 116.
- Graham DR, Bellingham AJ, Alstead E, Krasner N, Martindale J (1982) Coeliac disease presenting as acute bleeding disorders. Postgrad Med J 58:178–179.
- Vaynshtein G, Rosenbaum H, Groisman GM, Markel A (2004) Celiac sprue presenting as severe hemorrhagic diathesis due to vitamin K deficiency. Isr Med Assoc J 6: 781–783.
- Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA; American College of Gastroenterology (2013) ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol 108: 656-676.
- Halfdanarson TR, Litzow MR, Murray JA (2007) Hematologic manifestations of celiac disease. Blood 109: 412-421.
- Cavallaro R, Iovino P, Castiglione F, Palumbo A, Marino M, et al. (2004) Prevalence and clinical associations of prolonged prothrombin time in adult untreated coeliac disease. Eur J Gastroenterol Hepatol 16: 219-223.
- Rubio-Tapia A, Murray JA (2007) The liver in celiac disease. Hepatology 46: 1650-1658.
- Zanini B, Baschè R, Ferraresi A, Pigozzi MG, Ricci C, et al. (2014) Factors that contribute to hypertransaminasemia in patients with celiac disease or functional gastrointestinal syndromes. Clin Gastroenterol Hepatol 12: 804-810.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 12395
- [From(publication date):
December-2015 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 11510
- PDF downloads : 885