Diagnosis and Multidisciplinary Care for a 72-Year-Old Alzheimerâs Patient: A Case Report
Received: 28-Jun-2023 / Manuscript No. JADP-23-110940 / Editor assigned: 30-Jun-2023 / PreQC No. JADP-23-110940 (PQ) / Reviewed: 14-Jul-2023 / QC No. JADP-23-110940 / Revised: 21-Jul-2023 / Manuscript No. JADP-23-110940 (R) / Published Date: 31-Jul-2023 DOI: 10.4172/2161-0460.1000575
Abstract
Alzheimer's Disease (AD) is a relentless and progressive neurodegenerative disorder that inflicts profound cognitive decline, memory impairment, and functional limitations upon those it affects. This case report serves as a comprehensive exploration of the clinical journey of a 72-year-old female patient, vividly illustrating the intricate process of her evaluation, diagnostic investigation, and the management strategies deployed upon her diagnosis of Alzheimer's Disease. Timely identification of cognitive changes and memory deficits is a linchpin for affording patients and their families the opportunity to access appropriate support and interventions. This case study, therefore, highlights the critical role played by vigilant healthcare providers in recognizing the subtle signs of AD. Crucially, the multidisciplinary approach to Alzheimer's management is a recurrent theme throughout this case. The collaborative efforts of neurologists, geriatric psychiatrists, social workers, and caregivers are indispensable in navigating the complex terrain of Alzheimer's care. This case report thus serves as a compelling reminder that Alzheimer's Disease necessitates a united front from healthcare professionals, family members, and support systems to enhance patient outcomes and provide much-needed solace amid the challenges posed by this debilitating condition.
Keywords: Alzheimer’s disease; Confusion; Hypertension; Dementia
Introduction
Alzheimer's Disease (AD) is an insidious and progressive neurodegenerative disorder that casts a shadow over the lives of millions, striking at the heart of cognitive function, memory, and daily functioning. This case study delves into the compelling narrative of a 72-year-old female patient who embarked on a journey through the labyrinthine landscape of Alzheimer's Disease [1]. It underscores the critical importance of early detection, precise diagnosis, and the collaborative, multidisciplinary approach essential for navigating the complexities of this challenging condition. The most common cause of dementia in the elderly, poses a profound burden on individuals and their families. As the global population ages, the prevalence of AD continues to rise, making it an urgent public health concern. This case report serves as an exemplar of the clinical evaluation, diagnostic workup, and management strategies employed in the face of Alzheimer's Disease, shedding light on the challenges and opportunities encountered in the pursuit of patient care and quality of life preservation. Recognizing and diagnosing Alzheimer's Disease, employing an array of cognitive assessments, neuroimaging, cerebrospinal fluid analysis, and genetic testing to achieve diagnostic clarity. Moreover, this report accentuates the pivotal role of a multidisciplinary healthcare team, including neurologists, geriatric psychiatrists, social workers, and dedicated caregivers, in orchestrating the symphony of care essential for patients grappling with AD [2,3].
Case Presentation
The patient, a 72-year-old female, was referred to our neurology clinic due to a progressive two-year history of memory decline, confusion, and personality changes. The concerns were initially raised by her family members, who noticed a subtle but consistent decline in her cognitive abilities. She frequently repeated questions, struggled to recognize close family members, and exhibited increased anxiety and agitation in unfamiliar situations. Additionally, her family noted significant difficulties in managing finances and maintaining personal hygiene, indicative of functional impairment. The patient had a history of well-controlled hypertension and hyperlipidemia, managed with antihypertensive and statin medications, respectively. There were no known allergies. Notably, the family history was significant for Alzheimer's Disease, with her mother and maternal aunt both having been diagnosed with the condition.
Clinical examination
The patient appeared well-nourished and appropriately groomed for her age. She exhibited disorientation to time and place during the assessment. Her responses to basic questions were often delayed and inaccurate. The patient's score on the Mini-Mental State Examination (MMSE) was 20 out of 30, indicative of significant cognitive impairment. Physical examination revealed no focal neurological deficits or other abnormalities, aside from signs of aging. The diagnosis of Alzheimer's Disease and rule out other potential causes of cognitive impairment, a comprehensive diagnostic workup was initiated and it includes the following:
Cognitive assessment: The MMSE, a standard cognitive screening tool, revealed a score of 20/30, consistent with moderate cognitive impairment. The Montreal Cognitive Assessment (MoCA) was administered, resulting in a score of 16/30, further supporting cognitive decline. The Clinical Dementia Rating (CDR) assessment yielded a score of 2, confirming a diagnosis of moderate dementia.
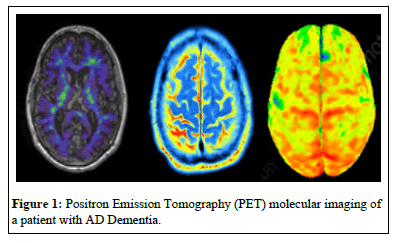
Neuroimaging: Magnetic Resonance Imaging (MRI) of the brain displayed significant global atrophy, particularly in the medial temporal lobe, which is characteristic of Alzheimer's Disease. PET scans utilize radiotracers that highlight abnormal accumulations of beta-amyloid plaques and tau protein tangles, both hallmark features of Alzheimer's pathology. By tracking these biomarkers, clinicians can visualize the extent and distribution of these abnormalities in the brain, aiding in the differential diagnosis of dementia. Furthermore, PET allows for early detection, enabling timely interventions and personalized treatment plans. This non-invasive imaging technique plays a pivotal role in monitoring disease progression, assessing treatment efficacy, and advancing our understanding of Alzheimer's, ultimately enhancing patient care and research efforts (Figure 1).
Routine blood tests: These include a Complete Blood Count (CBC), Comprehensive Metabolic Panel (CMP), thyroid function tests, and vitamin B12 levels, which were all within normal limits, effectively ruling out common reversible causes of cognitive impairment.
Cerebrospinal fluid analysis: Cerebrospinal Fluid (CSF) analysis was performed, revealing elevated levels of tau protein and decreased levels of amyloid-beta protein, consistent with the profile seen in Alzheimer's Disease. Genetic analysis for the Apolipoprotein E (APOE) gene revealed that the patient carried one e4 allele, which is associated with an increased risk of Alzheimer's Disease. Based on the comprehensive clinical evaluation, cognitive assessments, neuroimaging findings, CSF analysis results, and genetic testing, the patient was diagnosed with Alzheimer's Disease. This diagnosis met the criteria outlined in both the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), and the National Institute on Aging-Alzheimer's Association (NIA-AA) criteria for probable Alzheimer's Disease.
Results and Discussion
The comprehensive diagnostic workup of the 72-year-old female patient revealed a consistent and compelling profile indicative of Alzheimer's Disease. The patient's cognitive assessment, as evaluated by the MMSE and MoCA, demonstrated moderate cognitive impairment.
Her struggles with memory, orientation, and attention were evident through her scores. The Clinical Dementia Rating (CDR) assessment corroborated these findings, further confirming the presence of moderate dementia. These cognitive assessments collectively provided strong evidence for an AD diagnosis. Magnetic Resonance Imaging (MRI) of the brain unveiled marked global atrophy, with a particular emphasis on atrophy within the medial temporal lobe. This pattern is highly characteristic of Alzheimer's Disease and aligns with the expected neuroanatomical changes seen in AD patients. Routine laboratory tests, including CBC, CMP, thyroid function tests, and vitamin B12 levels, returned within normal limits. This ruled out common medical conditions that might present with cognitive impairment, such as hypothyroidism or vitamin B12 deficiency [4]. The CSF analysis yielded crucial biomarker information. Elevated tau protein levels and reduced amyloid-beta protein levels in the CSF were consistent with the biomarker profile associated with Alzheimer's Disease. Elevated tau reflects neurodegeneration, while reduced amyloid-beta indicates the accumulation of amyloid plaques in the brain, both hallmarks of AD. Genetic testing revealed the presence of one e4 allele of the Apolipoprotein E (APOE ) gene. This genetic profile is associated with an increased risk of developing Alzheimer's Disease. While not diagnostic on its own, it adds weight to the overall clinical diagnosis [5].
This diagnosis has significant clinical implications. AD is a progressive and incurable neurodegenerative disorder that leads to a decline in cognitive function, impaired daily living activities, and a substantial burden on the patient and their caregivers. The patient and her family must now grapple with the challenges posed by this chronic condition. The importance of early detection and diagnosis of Alzheimer's Disease cannot be overstated. This case highlights the significance of vigilant family members and healthcare providers in recognizing subtle cognitive changes. Early diagnosis enables the initiation of interventions aimed at improving the quality of life for the patient and provides an opportunity to plan for future care needs. Alzheimer's Disease management necessitates a multidisciplinary approach. This case report underscores the crucial role of various healthcare professionals, including neurologists, geriatric psychiatrists, and social workers, in providing comprehensive care and support. Additionally, dedicated caregivers play a pivotal role in the patient's journey, ensuring their safety and well-being [6]. The presence of an APOE e4 allele in this patient raises awareness of the role of genetics in Alzheimer's Disease. While genetics can influence susceptibility, it is not the sole determinant. Environmental factors and lifestyle choices also play a significant role in the disease's onset and progression.
Conclusion
Alzheimer's Disease remains a challenging field in healthcare, with no cure currently available. Ongoing research into disease mechanisms, biomarkers, and potential treatments is essential. Clinical trials and advancements in pharmacological and non-pharmacological interventions offer hope for improved outcomes in the future. This case underscores the critical need for early recognition, precise diagnosis, and a collaborative approach to managing Alzheimer's Disease. It serves as a reminder of the complexities and challenges faced by both patients and their caregivers and emphasizes the importance of ongoing research and support systems in the fight against this devastating neurodegenerative disorder.
References
- Andrade AG, Bubu OM, Varga AW, Osorio RS (2018). The relationship between obstructive sleep apnea and Alzheimer’s disease. J Alzheimers Dis 64(s1):S255-S270.
[Crossref] [Google Scholar] [PubMed]
- Affoo RH, Foley N, Garrick R, Siqueira WL, Martin RE (2015). Meta‐analysis of salivary flow rates in young and older adults. J Am Geriatr Soc 63(10):2142-2151.
[Crossref] [Google Scholar] [PubMed]
- Wilcock GK, Esiri MM (1982). Plaques, tangles and dementia: A quantitative study. Am J Psychiatry 56(2-3):343-356.
[Crossref] [Google Scholar] [PubMed]
- Pohjasvaara T, Erkinjuntti T, Ylikoski R, Hietanen M, Vataja R, et al. (1998). Clinical determinants of poststroke dementia. Stroke 29(1):75-81.
[Crossref] [Google Scholar] [PubMed]
- Bianchetti A, Rozzini R, Guerini F, Boffelli S, Ranieri P, et al. (2020). Clinical presentation of COVID-19 in dementia patients. The J Nutr Health Aging 24:560-562.
[Crossref] [Google Scholar] [PubMed]
- Zoe A, Raj CS, Davide AB (2019). Diagnosis and management of dementia: Review. JAMA 322(16):1589-1599.
[Crossref] [Google Scholar] [PubMed]
Citation: Thompson E (2023) Diagnosis and Multidisciplinary Care for a 72-Year-Old Alzheimer’s Patient: A Case Report. J Alzheimers Dis Parkinsonism 13: 575. DOI: 10.4172/2161-0460.1000575
Copyright: © 2023 Thompson E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1396
- [From(publication date): 0-2023 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 1168
- PDF downloads: 228