Diagnosis and Management of Thyroid Nodules with Atypia: A Three-year Study at an Institution in Taiwan
Received: 14-Dec-2015 / Accepted Date: 28-Jan-2016 / Published Date: 01-Feb-2016 DOI: 10.4172/2476-2024.1000105
Abstract
Objective: According to Bethesda System for Reporting Thyroid Cytopathology, the category, atypia of undetermined significance (AUS), is estimated to have a low malignancy risk of around 5%-15%. Variable surgical malignancy rates of AUS have been reported in diverse populations. The present study evaluated the malignancy rate at our institution and associated demographic data to identify high-risk nodules.
Methods: In this retrospective study, thyroid nodules with initial fine-needle aspirations (FNAs) reported as AUS from April 2010 to May 2013 were analyzed. Demographic data, clinical managements, and histopathologic results were evaluated.
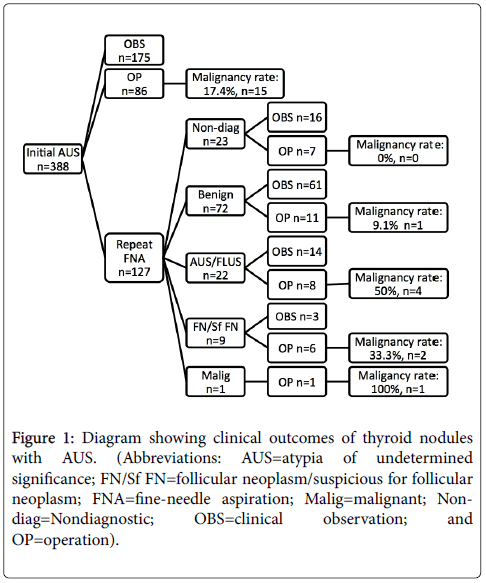
Results: A total of 7382 aspirations performed during the study period were analyzed; 5.7% were reported as atypia, 70.3% as benign, 1.5% as follicular neoplasm, 2.7% as suspicious for malignancy or malignant, and 19.8% as nondiagnostic. A total of 388 patients with one nodule reported as AUS were enrolled for analysis; 86 (22.2%) underwent surgical biopsy directly, 127 (32.7%) received follow-up FNAs, and 175 (45.1%) received clinical observation. The malignancy rate in the 86 patients who underwent surgical biopsy directly after first AUS was 17.4%. Out of the 127 patients who received follow-up FNAs, 105 were reclassified into the different-rank risk categories (benign, neoplasm or malignancy, and nondiagnostic) and 22 remained in AUS. Among the 33 patients out of 127 who received thyroid surgery after follow-up FNAs, the malignancy rates in the 8 patients with repeated AUS results and 11 patients with benign results in the second FNA were 50% and 9.1%, respectively. No significant difference in sex, age, nodular size, numbers, and preoperative thyroid-stimulating hormone level between the benign and malignant groups in the thyroid AUS cases was observed.
Conclusion: Repeated AUS may be associated with a higher malignancy rate in final histopathology, and other supplementary techniques are required to enhance preoperative diagnostic accuracy.
Keywords: Follicular neoplasm; Fine needle aspirations (FNA); Cytopathology
6136Introduction
Fine-needle aspiration (FNA) is the procedure of choice for evaluating thyroid nodules and has been widely applied in clinical settings [1]. Based on the cytopathological results, a clinician can determine whether to perform surgical biopsy or not and thus avoid unnecessary operation. However, various reporting systems with two or more categories have been adopted at several institutions which has caused confusion among cytopathologists and clinicians [2]. For consensus on the terminology and enhance communication, the National Cancer Institute (NCI) hosted the “NCI Thyroid Fine-Needle Aspiration State of the Science Conference” in Bethesda, MD, in 2007 and proposed a new 6-tiered reporting system, the Bethesda System for Reporting Thyroid Cytopathology (TBSRTC), with each of the 6 categories having a different cancer risk. The categories and their implied risk of malignancy rates were as follows: I. nondiagnostic or unsatisfactory (1%-4%), II. benign (0%-3%), III. atypia of undetermined significance or follicular lesion of undetermined significance (AUS/FLUS) (5%-15%), IV. follicular neoplasm or suspicious for a follicular neoplasm (15%-30%), V. suspicious for malignancy (60%-75%), and VI. malignant (97%-99%) [3].
In the TBSRTC system, the third classification, AUS/FLUS, is used for defining cytologies that are difficult to classify as benign, suspicious, or malignant. Patients with nodules reported as atypia are generally considered a low-risk group, and repeated FNAs were recommended for appropriate initial management. The estimated malignancy of this category is approximately 5%-15%, but higher malignancy rates of 15.7%-45.7% have been reported [4-7]. Undetermined nodules are proposed to be heterogeneous, and at least eight scenarios are listed in TBSRTC to be managed as AUS/FLUS [3].
In this study, we reported the clinical experiences of AUS/FLUS nodules at our medical center in central Taiwan. In addition, we evaluated potentially helpful factors, such as age, sex, number of nodules, and thyroid-stimulating hormone (TSH) level, for identifying high-risk nodules reported with atypia, because these clinical characteristics have been used to predict malignancy in thyroid nodules [8-10].
Material And Methods
We have been using the 6-tiered Bethesda system at our hospital, Taichung Veterans General Hospital, Taiwan R.O.C., since 2010. All cases included in this study were reported by the same cytopathologist. The electronic medical records of patients with thyroid nodules who received FNAs from April 15, 2010 to May 31, 2013 at our hospital were retrospectively searched. Thyroid nodules of a size >1 cm with solid or mixed-solid cystic components and those of the size ultrasonography findings, such as microcalcifications, hypoechoic, increased nodular vascularity, infiltrative margins, or with an observed greater height than width when using a transverse view, were aspirated. Each nodule had one FNA with 3–5 passes of a needle performed by endocrinologists or radiologists and the nodules Papanicolaou stain. Nodules reported with atypical cells, atypia, or AUS were included. Follow-up management was performed based on the recommendations of TBSRTC (e.g., repeating FNA at appropriate intervals or a thyroidectomy if thyroid nodules with AUS were associated with clinical factors with an increased malignancy risk) [3,11] or the physicians’ judgment. Electronic medical records, such as ultrasonography, repeated FNAs, and surgical biopsy conducted on the same nodules until August 19, 2013, were reviewed. The microscopic examination and ultrasonographic reports of each nodule were matched and those in the histopathologic reports were indicated. In addition, demographic data, including age, sex, nodular size, presence of single nodularity on ultrasound, and TSH level, were documented for analysis. Patients with a previous diagnosis of thyroid cancer and those receiving antithyroid drugs or eltroxin were excluded from analysis because these medications may interfere with the TSH level. This study was approved by the Institutional Review Board of the Taichung Veterans General Hospital, Taiwan.
Statistical Analysis
All numerical variables were assessed for normality using the Kolmogorov–Smirnov test. The results were presented as the median (25th quartile, 75th quartile, interquartile range), if they were not normally distributed. The associations between the result of the second AUS, categorical variables, and surgical malignancy rate were assessed using the two-tailed χ2 test or two-tailed Fisher’s exact test, when appropriate. The Mann–Whitney U test was used for determining the statistical significance of continuous variables. All statistical tests were 2-sided and assessed at the significance level of 0.05.
Results
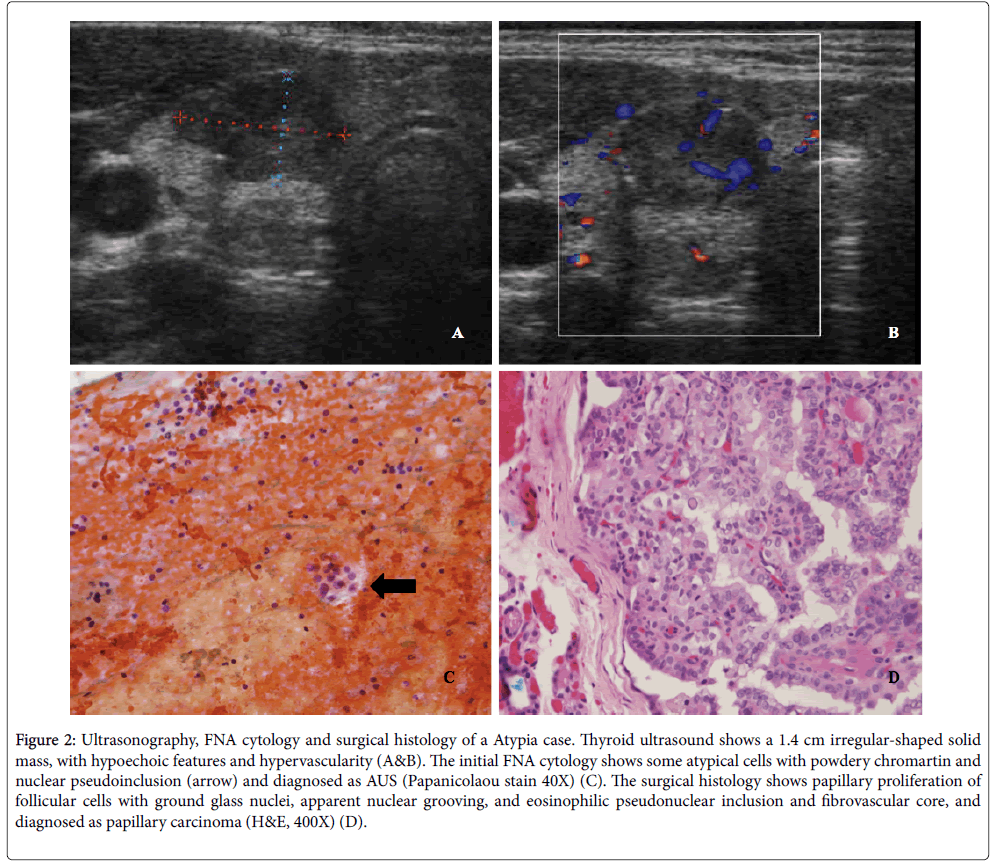
A total of 7382 aspirations were performed during the study period; 5.7% were reported as atypia, 70.3% as benign, 1.5% as follicular neoplasm, 2.7% as suspicious for malignancy or malignant, and 19.8% as nondiagnostic. A total of 388 patients with one nodule reported as AUS initially were eligible for analysis; 19.1% of these were men, and the mean age was 52.7 years. Among these patients, 86 (22.2%) underwent surgical biopsy directly, 127 (32.7%) received repeated FNAs, and 175 (45.1%) received clinical observation. In the 127 patients with follow-up FNAs, 56.7% (n=72) were reclassified into the low-risk category (benign), 7.9% (n=10) into the high-risk category (follicular neoplasm, suspicious for malignancy or malignant), 17.3% (n=22) into AUS, and 18.1% (n=23) into unsatisfactory (Figure 1). The average size of these nodules recorded on thyroid ultrasonography was 2.24 ± 1.11 cm. The thyroid ultrasound, cytology, and surgical histology of one atypia case which was demonstrated in Figure 2.
Figure 1: Diagram showing clinical outcomes of thyroid nodules with AUS. (Abbreviations: AUS=atypia of undetermined significance; FN/Sf FN=follicular neoplasm/suspicious for follicular neoplasm; FNA=fine-needle aspiration; Malig=malignant; Nondiag= Nondiagnostic; OBS=clinical observation; and OP=operation).
Figure 2: Ultrasonography, FNA cytology and surgical histology of a Atypia case. Thyroid ultrasound shows a 1.4 cm irregular-shaped solid mass, with hypoechoic features and hypervascularity (A&B). The initial FNA cytology shows some atypical cells with powdery chromartin and nuclear pseudoinclusion (arrow) and diagnosed as AUS (Papanicolaou stain 40X) (C). The surgical histology shows papillary proliferation of follicular cells with ground glass nuclei, apparent nuclear grooving, and eosinophilic pseudonuclear inclusion and fibrovascular core, and diagnosed as papillary carcinoma (H&E, 400X) (D).
The overall surgical malignancy rate in the 119 patients who underwent surgical biopsy was 19.3%. The malignancy rate in the 86 patients who underwent operation directly after their first AUS report was 17.4%. The overall malignancy rate in the 33 patients out of 127 who underwent surgical biopsy after repeated FNAs was 24.2%. Among the patients, 7 were categorized as nondiagnostic, 11 as benign, 8 as atypia, 6 as suspicious for neoplasm, and 1 as suspicious for malignancy according to the cytology categories. Notably, the malignancy rates in the 8 patients with repeated AUS results and 11 patients with benign results in the secondary FNA were 50% and 9.1%, respectively (Figure 1).
The results of Fisher’s exact test revealed that the malignancy rate in the 8 patients with consecutive AUS results (4 benign and 4 malignant) was marginally significantly (p=0.05) higher than that in 86 patients with initial AUS cases but without repeated FNAs (71 benign and 15 malignant).
To examine whether clinical characteristics, nodular size, and number of nodules were helpful in preoperative evaluation of AUS cases by using Chi-Square test, our study revealed no significant difference in sex, age, nodular size, single nodularity, and preoperative TSH levels between the benign and malignant groups (Table 1).
| Benign | Malignant | P value | |
|---|---|---|---|
| N | 96 | 23 | |
| Male | 15.60% | 13.00% | 1.000 |
| Female | 84.40% | 87.00% | 1.000 |
| Age | 52.4 (40.33, 61.15) | 51.0 (38.3, 56.8) | 0.677 |
| Single nodule | 18.90% | 30.40% | 0.226 |
| Size | 2.09 (1.60,2.84) | 2.39 (1.85, 2.88) | 0.29 |
| TSH mIU/L (N=78 vs. 20)* |
1.25 (0.77, 2.28) | 1.40 (0.90, 2.14) | 0.979 |
Categorical variables (sex and single nodule) were assessed using the χ2 test.Continuous variables (age, size, and TSH level) were assessed using the Mann–Whitney U test.*98 of 119 patients who underwent operation had TSH levels for analysis.
Table 1: Demographic characteristics associated with benign or malignant nodules.
Among all malignant results of histopathology, nearly 70% (16 out of 23 cases) were reported as papillary carcinoma or papillary microcarcinoma and 26% (6 out of 23) were reported as follicular carcinoma (one case with concomitant papillary carcinoma and follicular carcinoma). In addition, 11 patients had an uncertain diagnosis, including 4 with follicular neoplasm with uncertain malignant potential and 7 with well-differentiated tumors of uncertain malignant potential (Table 2).
| Histopathologic results | No. of cases (%) |
|---|---|
| Benign (N=85, 71.4%) | |
| Nodular hyperplasia | 68 (57.1%) |
| Follicular adenoma | 7 (5.9%) |
| Oncocytic adenoma | 1 (0.8%) |
| Chronic lymphocytic thyroiditis | 9 (7.6%) |
| Undifferentiated (N=11, 9.3%) | |
| Follicular neoplasm of uncertain malignant potential | 4 (3.4%) |
| Well-differentiated tumor of uncertain malignant potential | 7 (5.9%) |
| Malignant (N=23, 19.3%) | |
| Papillary microcarcinoma | 5 (4.2%) |
| Papillary carcinoma | 11 (9.2%) |
| Follicular carcinoma1 | 6 (5.0%) |
| Anaplastic carcinoma | 1 (0.8%) |
| Carcinoma, poorly differentiated | 1 (0.8%) |
1One with concomitant papillary carcinoma and follicular carcinoma.
Table 2: Distribution of histopathologic results of patients undergoing operation.
Discussion
This hospital-based study found that 5.7% of thyroid FNAs reported AUS. The overall malignancy rate of atypia nodules, which received thyroid surgery, was 19.3% and higher in those with repeated FNAs than those without repeated FNAs (24.2% vs. 17.4%). A similar finding was previously reported on malignancy rates in AUS cases with and without repeated FNAs, which were 29% and 14%, respectively [12]. Patients with consecutive AUS exhibited a higher malignancy rate than those with single AUS (50% vs. 17.4%). Although our sample size was small and the p value was marginally significant, repeated FNAs may help exclude some clotting artifacts and select high-risk nodules. Thyroid nodules with a subsequent benign result after initial AUS on FNA exhibited a lower malignancy rate. However, these nodules possess a malignancy rate higher than nodules with benign cytological diagnosis alone must be noticed [13].
TBSRTC recommends repeat FNAs in AUS nodules with uncertain but assumed to be low malignancy rates (5%-15%) [3]. A previous study reported a lower risk of malignancy in indeterminate thyroid nodules in post-TBSRTC than pre-TBSRTC (13% vs. 35%), despite similar thyroidectomy rates (47% vs. 35%) [14]. Our cohort exhibited a similar thyroidectomy rate (30.7%), but up to 175 of 388 (45.1%) atypia cases received clinical observation only and 86 (22.2%) cases underwent operation directly without follow-up FNA. The clinicians at our institution might not be familiar with TBSRTC and therefore have been led to different clinical decisions. In our cohort, patients who were referred to repeated FNAs might have suspicious clinical presentations that resulted in higher malignancy rates of histopathology. Besides, unnecessary surgery should be avoided in this low malignancy risk group because thyroid operation may be complicated owing to postoperative thyroid hormone imbalance, hypoparathyroidism, recurrent laryngeal nerve injury, bleeding, and infection [1,15]. Patients with thyroid FNAs yielding AUS may undergo thyroid surgery only in the presence of associated clinical factors that increase malignancy risk. All other AUS cases are best managed with repeated FNAs [3].
In the present study, more than 20% (5 out of 23) surgical malignancy cases were papillary microcarcinoma; this incidence was marginally higher than the incidence of ipsilateral incidental papillary microcarcinoma from nodules with undetermined result FNAs [16]. TBSRTC proposes that some subtypes of AUS have features suggestive of papillary carcinoma such as nuclear grooves, enlarged nuclei with pale chromatin, and alterations in nuclear contour and shape [3]. Previous studies have reported that nodules with such AUS features may carry a higher risk of malignancy than other subtypes of AUS [17-19]. Papillary microcarcinoma also remained significantly associated with the AUS group [20]. Several studies have reported that papillary microcarcinoma, particularly nonincidental microcarcinoma, can have aggressive behaviors similar to those demonstrated by local metastasis and recurrent disease [21,22], and careful cytological evaluation of these atypia nodules may help in identification of these nonincidental microcarcinomas and perform timely surgical biopsy [23].
Demographic data revealed no clinical significance between benign and malignant nodules; this observation was consistent with the results of a previous more extensively reviewed study [24]. Thus, a more effective diagnostic approach with fewer complications rather than clinical follow-up should be adopted for these patients to prevent a delayed diagnosis of malignant nodules. Recently, core-needle biopsy (CNB) has been proposed as a complementary test to FNA for evaluating thyroid nodules [25-27]. One study reported better sensitivity to malignancy and a lower inconclusive diagnosis rate of CNBs than repeated FNAs because of the greater numbers of cells obtained from CNBs [28]. However, CNBs have several limitations in clinical practice, such as not being feasible in some small nodules and requiring a prolonged training period, specific skills, and experiences in image-guided thyroid intervention. In addition, several immunocytochemical markers, including cytokeratin-19, galectin-13, Hector Battifora mesothelial-1, and genetic-expression classifiers have been used to improve cytological diagnostic accuracy, although meta-analytical results have revealed that preoperative applications of these molecular markers have not proved to have adequate sensitivity and specificity [29-32]. In this study, we did not perform CNBs or use immunohistochemistry preoperatively. Therefore, whether these technologies may help us manage thyroid nodules appropriately and avoid unnecessary operation and complication further investigation.
Our study was limited by the retrospective design and only 33% of the patients had histopathologic confirmation. The statistical significance of comparing the malignancy risk between repeated AUS and nonrepeated, single AUS cases was marginal. Further study should recruit a larger group of patients. In addition, these patients were reviewed at a single medical center. Therefore, whether our study results can be applied to the management of undetermined nodules in a clinical setting requires further investigation.
Conclusion
Repeated FNA can identify high-risk nodules in patients with AUS. The malignancy rate was higher in patients with repeated AUS than in those with AUS plus benign or in those with nonrepeated, single AUS. However, we could not determine particular clinical parameters for preoperatively differentiating between benign and malignant nodules among atypia cases. Multidisciplinary management along with advanced techniques, such as CNB and molecular markers, may be required for a more accurate preoperative diagnosis of these cytologically undetermined nodules.
References
- Yassa L, Cibas ES, Benson CB, Frates MC, Doubilet PM, et al. (2007) Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer 111: 508-516.
- Wang HH (2006) Reporting thyroid fine-needle aspiration: literature review and a proposal. Diagn Cytopathol 34: 67-76.
- Cibas ES, Ali SZ; NCI Thyroid FNA State of the Science Conference (2009) The Bethesda System For Reporting Thyroid Cytopathology. Am J Clin Pathol 132: 658-665.
- VanderLaan PA, Marqusee E, Krane JF (2011) Clinical outcome for atypia of undetermined significance in thyroid fine-needle aspirations: should repeated fna be the preferred initial approach? Am J Clin Pathol 135: 770-775.
- Nagarkatti SS, Faquin WC, Lubitz CC, Garcia DM, Barbesino G, et al. (2013) Management of thyroid nodules with atypical cytology on fine-needle aspiration biopsy. Ann SurgOncol 20: 60-65.
- Broome JT, Solorzano CC (2011) The impact of atypia/follicular lesion of undetermined significance on the rate of malignancy in thyroid fine-needle aspiration: evaluation of the Bethesda System for Reporting Thyroid Cytopathology. Surgery 150: 1234-1241.
- Dincer N, Balci S, Yazgan A, Guney G, Ersoy R, et al. (2013) Follow-up of atypia and follicular lesions of undetermined significance in thyroid fine needle aspiration cytology. Cytopathology 24: 385-390.
- Rago T, Fiore E, Scutari M, Santini F, Di CG, et al. (2010) Male sex, single nodularity, and young age are associated with the risk of finding a papillary thyroid cancer on fine-needle aspiration cytology in a large series of patients with nodular thyroid disease. Eur J Endocrinol 162: 763-770.
- Brito JP, Yarur AJ, Prokop LJ, McIver B, Murad MH, et al. (2013) Prevalence of thyroid cancer in multinodulargoiter versus single nodule: a systematic review and meta-analysis. Thyroid 23: 449-455.
- Haymart MR, Repplinger DJ, Leverson GE, Elson DF, Sippel RS, et al. (2008) Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab 93: 809-814.
- Chen JC, Pace SC, Chen BA, Khiyami A, McHenry CR (2012) Yield of repeat fine-needle aspiration biopsy and rate of malignancy in patients with atypia or follicular lesion of undetermined significance: the impact of the Bethesda System for Reporting Thyroid Cytopathology. Surgery 152: 1037-1044.
- Ustün H, Astarcı HM, Altunkaya C, Yılmaz S, Barın A, et al. (2012) Fine-needle aspiration of follicular patterned lesions of the thyroid: diagnosis, management, and follow-up according to thyroid Bethesda system. Acta Cytol 56: 361-369.
- Renshaw AA (2010) Does a repeated benign aspirate change the risk of malignancy after an initial atypical thyroid fine-needle aspiration? Am J ClinPathol 134: 788-792.
- Rabaglia JL, Kabbani W, Wallace L, Holt S, Watumull L, et al. (2010) Effect of the Bethesda system for reporting thyroid cytopathology on thyroidectomy rates and malignancy risk in cytologically indeterminate lesions. Surgery 148: 1267-1272.
- Christou N, Mathonnet M (2013) Complications after total thyroidectomy. J Visc Surg 150: 249-256.
- Teixeira GV, Chikota H, Teixeira T, Manfro G, Pai SI, et al. (2012) Incidence of malignancy in thyroid nodules determined to be follicular lesions of undetermined significance on fine-needle aspiration. World J Surg 36: 69-74.
- Olson MT, Clark DP, Erozan YS, Ali SZ (2011) Spectrum of risk of malignancy in subcategories of 'atypia of undetermined significance'. Acta Cytol 55: 518-525.
- Renshaw AA (2011) Subclassification of atypical cells of undetermined significance in direct smears of fine-needle aspirations of the thyroid: distinct patterns and associated risk of malignancy. Cancer Cytopathol 119: 322-327.
- Bonzanini M, Amadori P, Morelli L, Fasanella S, Pertile R, et al. (2011) Subclassification of the "grey zone" of thyroid cytology; a retrospective descriptive study with clinical, cytological, and histological correlation. J Thyroid Res 2011: 251680.
- Song JY, Chu YC, Kim L, Park IS, Han JY, et al. (2012) Reclassifying formerly indeterminate thyroid FNAs using the Bethesda system reduces the number of inconclusive cases. ActaCytol 56: 122-129.
- Roti E, Rossi R, Trasforini G, Bertelli F, Ambrosio MR, et al. (2006) Clinical and histological characteristics of papillary thyroid microcarcinoma: results of a retrospective study in 243 patients. J Clin Endocrinol Metab 91: 2171-2178.
- Mehanna H, Al-Maqbili T, Carter B, Martin E, Campain N, et al. (2014) Differences in the recurrence and mortality outcomes rates of incidental and nonincidental papillary thyroid microcarcinoma: a systematic review and meta-analysis of 21 329 person-years of follow-up. J Clin Endocrinol Metab 99: 2834-2843.
- Yang GC, LiVolsi VA, Baloch ZW (2002) Thyroid microcarcinoma: fine-needle aspiration diagnosis and histologic follow-up. Int J SurgPathol 10: 133-139.
- Castro MR, Espiritu RP, Bahn RS, Henry MR, Gharib H, et al. (2011) Predictors of malignancy in patients with cytologically suspicious thyroid nodules. Thyroid 21: 1191-1198.
- Zhang S, Ivanovic M, Nemcek AA Jr, Defrias DV, Lucas E, et al. (2008) Thin core needle biopsy crush preparations in conjunction with fine-needle aspiration for the evaluation of thyroid nodules: a complementary approach. Cancer 114: 512-518.
- Sung JY, Na DG, Kim KS, Yoo H, Lee H, et al. (2012) Diagnostic accuracy of fine-needle aspiration versus core-needle biopsy for the diagnosis of thyroid malignancy in a clinical cohort. Eur Radiol 22: 1564-1572.
- Hahn SY, Shin JH, Han BK, Ko EY, Ko ES (2013) Ultrasonography-guided core needle biopsy for the thyroid nodule: does the procedure hold any benefit for the diagnosis when fine-needle aspiration cytology analysis shows inconclusive results? Br J Radiol 86: 20130007.
- Na DG, Kim JH, Sung JY, Baek JH, Jung KC, et al. (2012) Core-needle biopsy is more useful than repeat fine-needle aspiration in thyroid n odules read as nondiagnostic or atypia of undetermined significance by the Bethesda system for reporting thyroid cytopathology. Thyroid 22: 468-475.
- Ferraz C, Eszlinger M, Paschke R (2011) Current state and future perspective of molecular diagnosis of fine-needle aspiration biopsy of thyroid nodules. J Clin Endocrinol Metab 96: 2016-2026.
- Alexander EK, Kennedy GC, Baloch ZW, Cibas ES, Chudova D, et al. (2012) Preoperative diagnosis of benign thyroid nodules with indeterminate cytology. N Engl J Med 367: 705-715.
- de Matos LL, Del Giglio AB, Matsubayashi CO, de Lima Farah M, Del Giglio A, et al. (2012) Expression of CK-19, galectin-3 and HBME-1 in the differentiation of thyroid lesions: systematic review and diagnostic meta-analysis. Diagn Pathol 7: 97.
- Jeong SH, Hong HS, Lee EH, Cha JG, Park JS, et al. (2013) Outcome of thyroid nodules characterized as atypia of undetermined significance or follicular lesion of undetermined significance and correlation with Ultrasound features and BRAF(V600E) mutation analysis. AJR Am J Roentgenol 201: W854-860.
Citation: Kuo YT, Chang MC, Song YM, Lee CL, Fu CP, et al. (2016) Diagnosis and Management of Thyroid Nodules with Atypia: A Three-year Study at an Institution in Taiwan. Diagn Pathol Open 1: 105. DOI: 10.4172/2476-2024.1000105
Copyright: ©2016 Kuo YT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 13912
- [From(publication date): 3-2016 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 12968
- PDF downloads: 944