Diabetes scenario in a backward rural district population of India and need for restructuring of health care delivery services
Received: 19-Feb-2016 / Accepted Date: 25-Feb-2016 / Published Date: 01-Mar-2016 DOI: 10.4172/2161-1165.1000224
Abstract
Background: Poor healthcare infrastructure and utilization complicated Indian diabetic epidemic especially in backward areas where many cases remain uncontrolled or even undiagnosed till complications develop. Dearth of information from eastern India regarding the burden and correlates of such uncontrolled and undiagnosed diabetes and consequent healthcare-seeking thus called for a detailed investigation in a poor-resource setting.
Methods: A community-based cross-sectional study was conducted in Malda, an under-developed district in eastern India. Between October 2013 and July 2014, 18028 consenting adults were randomly recruited, interviewed and tested for capillary blood sugar (fasting/post-prandial/random). Diabetics were defined by previous diagnoses or having fasting capillary blood sugar ≥126mg/dl or post-prandial/random blood sugar ≥200mg/dl. A previously diagnosed case was defined as uncontrolled if his/her measured blood sugar did fall in the diabetic level. On the other hand, previously undiagnosed persons, if found diabetic according to the test results, were termed as undiagnosed diabetic. Descriptive and regression analyses were conducted using SAS-9.3.2.
Results: Six percent adult residents were suffering from diabetes in Malda, India. Unfortunately, more than two-third (approximately sixty-three percent) of these diabetics remained undiagnosed till this study while a little less than half (about forty-seven percent) of the diagnosed cases were uncontrolled. Furthermore, eight percent of the diagnosed diabetics sought treatment from non-qualified practitioners. Among diabetics, odds of remaining undiagnosed were relatively lower among older and richer diabetics of urban area while females were more likely to remain undiagnosed. Secondary-educated subjects had higher and divorced/separated/widowed/widowers had lower odds of having uncontrolled Diabetes. Muslims and backward castes were less and educated, hard-working and richer diabetics were more likely to visit qualified private practitioners.
Conclusions: Burden of uncontrolled and undiagnosed Diabetes were high in Malda. Urgent interventions targeting young, female, married, less-educated and poor diabetics from rural area seemed necessary to ensure early detection and appropriate treatment.
Keywords: Diabetes Mellitus; Undiagnosed diabetes; Uncontrolled diabetes; Healthcare seeking
163767Introduction
The global public health focus is gradually concentrating more on the non-communicable diseases (NCDs), owing to the progressively increasing trend in the burden of NCDs worldwide including the developing countries. Among these NCDs, the silent epidemic of diabetes currently has become one of the most worrisome public health concerns [1-3]. Diabetes mellitus is a heterogeneous metabolic syndrome characterized by variable degrees of insulin resistance and/or impaired insulin secretion resulting in abnormal metabolism of glucose leading to hyperglycemia [4]. Multi-factorial interplay between genetic, behavioral and environmental factors is responsible for abnormal glucose homeostasis in diabetics [4].
Globally an estimated number of 387 million people are currently diagnosed to have diabetes with an adult prevalence of 8.3% [1,2,5- 7]. About 77% of these cases live in low and middle income countries and among them India and China are currently experiencing the most serious epidemic situation. In view of the fact that these two countries are the most populous countries in the world, the scenario seems alarming [1,2,5]. The current national diabetes prevalence is 8.6% in India, with more than 1 million annual diabetes-related deaths in the 20 to 79 age group [1,8].
Diabetes remains undiagnosed in many patients until the development of the symptoms of complications. Globally 46.3% diabetics remain unaware of their diabetic status and in India the estimated number is 35.5 million [1] and may be even higher due to lack of proper access and utilization of healthcare [2,9]. The solitary available evidence revealed that the prevalence of undiagnosed diabetes ranged between 3.1% to 9.4% in 10 states of India [10].
Uncontrolled diabetes among the diagnosed cases is another serious threat owing to its deleterious effects on body organs combined with the huge burden. Evidences suggest that in 70% of the diagnosed cases in India, diabetes remains uncontrolled [11]. To worsen the scenario, 90% of these uncontrolled diabetics consider their disease to be under control [12].
Burden of diabetes has shown a progressively increasing trend in India as evidenced by the upsurge of the diagnosed burden from approximately 62.4 million in 2011[13] to 66.8 million in 2014 [1,8]. Moreover the projected prevalence for the year 2030 was measured to be 79.4 million [4,8]. This increasing trend can well spell a disaster due to the silent destruction of the body organs and functions resulting from diabetes. While one person in every 12 has diagnosed diabetes in India [14]. these estimates are based on some regional observations and may only represent the tip of the iceberg keeping the undiagnosed and uncontrolled burden in mind. Thus, without immediate implementation of efficient intervention for risk reduction, early diagnosis and treatment, controlling the epidemic seems to be impossible. For proper diagnosis and treatment the patterns and predictors of healthcare-seeking are other important issues that need to be addressed appropriately [15].
Regarding risk reduction, in addition to the modifiable genetic factors, the rising burden of diabetes in this country [16] is often correlated with certain modifiable behaviors like lifestyle, eating habits, addictions (smoking and alcoholism), stress, and physical inactivity. Most of these evidences are based on hospital/clinic based purposively sampling from urban areas focusing on estimation of the local burden [12]. Handfuls of studies (mostly in western and southern India) have measured the association of these correlates with diabetes and almost none with uncontrolled and undiagnosed cases among residents of poor-resource settings in eastern India [17].
Dearth of information regarding the correlates of uncontrolled and undiagnosed diabetes among adult Indians living in poorresource settings, thus called for a detailed investigation involving a representative adult population of Malda, one of the poorest districts located in the northern part of West Bengal state in eastern India.
Materials and Methods
Ethics Statement
The study protocol was reviewed and approved by the Ethics Committee of the National Institute of Cholera and Enteric Diseases (NICED), Kolkata. After explaining the study details in local language, written informed consent or left thumb impression (for illiterates, in presence of two impartial literate witnesses) was obtained from each adult resident, in favor of participation and providing sample for the blood sugar test.
Study Design
Between October 2013 and July 2014, a community-based crosssectional study was conducted with the objective of measuring the burden of diagnosed, undiagnosed and uncontrolled diabetes, identifying their socio-demographic correlates and understanding the patterns and predictors of the healthcare-seeking among diabetics in a poor-resource setting.
Study site
The study was conducted involving a representative, consenting, adult (aged ≥18 years) population of Malda, one of the least developed districts in West Bengal state of India, having a population of 3.99 million with population density of 1,069/sq km and average literacy of 61.73% [18,19]. Sharing international border with Bangladesh and interstate borders with Bihar and Jharkhand, rendered this district’s health system exposed to unstable demographic pressure as high as 1,870 persons per available hospital bed [20].
Urban area of the district consists of 2 municipalities: Old Malda and English Bazar, each divided into several administrative units called wards (19 in Old Malda and 25 in English Bazar) while 3701 villages and 27 census towns constitute the rural part [18,21].
Sample size estimation
In the absence of appropriate parameter values for the sample size estimation, to recruit maximum required sample, based on available highest regional estimates for West Bengal till date [22], using 6% as the expected value and an absolute precision of 1%, assuming α=0.05, after finite population correction for 3.99 million, 17294 adults were required to be recruited. To account for an assumed 10% non-response, 19216 adults were invited.
Recruitment
To recruit a representative sample of required size, maintaining proportional distribution, 16 municipal wards (4 in Old Malda and 12 in English Bazar) from urban and [23] villages/census towns from rural area were selected randomly using stratified random sampling with probability proportional to size (PPS). Exhaustive house-listing was next conducted in each of the selected wards/villages/census towns. Each municipal ward/village/census town was then categorized into several segments, each consisting of 125 households (defined based on sharing of cooking pot in a dwelling). Considering these segments as Primary Sampling Units (PSU), using stratified proportional random multistage sampling with probability proportional to size (PPS), 2 segments were selected randomly in each selected wards/villages/ census towns and all households were surveyed there after collecting written informed consent from the residents. Thus from 4012 urban and 6095 rural households altogether 18028 consenting adults were recruited, interviewed and tested for diabetes.
Interview
Using a structured, pre-tested, bi-lingual (English and local language: Bengali) questionnaire, all the individuals residing in the selected households were interviewed at home by trained interviewers. The instrument collected information on age (18-40/41-60/>60 years), gender (male/female), religion (Hindu/Muslim/Others), caste (backward (SC/ST/OBC)/others), marital status (currently married/never married/divorced, separated, widowed, widower) education (illiterate/primary/secondary/higher secondary/graduate and above), occupational type (sedentary work/moderate work/hard work) and residential area (urban/rural). Information on household assets was also collected and used to calculate an asset index which was logtransformed and categorized into lower/middle/upper tertile to determine lower/middle/upper socio-economic status (SES) based on percentile distribution. Participants were interviewed and their medical records (if available) were checked to identify the diagnosed diabetics and to understand their pattern of healthcare-seeking for diabetes (sought care from: nonqualified practitioners/qualified practitioners from Government sector/qualified practitioners from private sector).
Laboratory testing
The full sequence of the isolated strain was analyzed using the SimPlot ver.4 program to determine the breakpoint of recombination by using window and step sizes of 200bp and 20bp, respectively.
Outcome measures
According to the guidelines of American Diabetes Association, diabetic level of capillary blood sugar was defined as fcg ≥ 126 mg/dL or ppcg/rcg ≥ 200 mg/dL [24,25]. Thus diabetics were defined as those having previously established diagnosis of diabetes or fcg ≥ 126 mg/dL or ppcg/rcg ≥ 200 mg/dL [24-26]. Subjects who were previously diagnosed as diabetic were defined as uncontrolled diabetics if they had fcg ≥ 126 mg/dL or ppcg/rcg ≥ 200 mg/dL [27]. Participants, who were never diagnosed as diabetic before, were termed as undiagnosed cases if they had fcg ≥ 126 mg/dL or ppcg/rcg ≥ 200 mg/dL.
Data analysis
Using SAS version 9.3.2 [28]. overall and stratified distributions (frequency, proportions and corresponding 95% Confidence Intervals (95% CI)) of the study variables were determined followed by simple and multiple (including all socio-demographic factors in to the model) logistic regressions (including multinomial for dependent variables with >2 categories: healthcare-seeking) [29-31], to measure the strengths of associations (unadjusted (OR) from simple and adjusted (each for all other socio-demographic factors) Odds Ratios (OR) from multiple regressions with corresponding 95% CIs) of socio-demographic factors with diabetes (diagnosed, overall, undiagnosed and uncontrolled) and related care-seeking.
Results
Altogether 18028 subjects were included in the analyses. Among participants, majority were aged ≤40 years (n=11191, 62.08%), female (n=11452, 63.52%), had Hindu religion (n=12774, 70.86%), belonged to backward castes (n=10374, 57.54%) and were currently married (n=13972, 77.55%). Higher proportions had secondary level of education (n=6891, 38.22%), were in jobs with moderate workload (n=9428, 52.30%), belonged to lower SES (n=7460, 41.38%) and resided in rural areas (n=10820, 60.02%) (Table 1).
| Variables | Categories | Frequency | Percentages (95% CIb) |
|---|---|---|---|
| Age group | 18-40 years | 11191 | 62.08 (61.37-62.78) |
| 41-60 years | 5210 | 28.90 (28.24-29.56) | |
| >60 years | 1627 | 9.02 (8.61-9.44) | |
| Gender | Male | 6576 | 36.48 (35.77-37.18) |
| Female | 11452 | 63.52 (62.82-64.23) | |
| Religion | Hindu | 12774 | 70.86 (70.19-71.52) |
| Muslim | 5190 | 28.79 (28.13-29.45) | |
| Others | 64 | 0.36 (0.27-0.44) | |
| Caste | Backward castes (SC/ST/OBC) | 10374 | 57.54 (56.82-58.27) |
| General castes | 7654 | 42.46 (41.73-43.18) | |
| Marital status | Currently married | 13972 | 77.55 (76.94-78.16) |
| Never married | 2126 | 11.80 (11.33-12.27) | |
| Divorced/separated/widowed/widower | 1919 | 10.65 (10.20-11.10) | |
| Education | Illiterate | 2558 | 14.19 (13.68-14.70) |
| Primary | 3379 | 18.74 (18.17-19.31) | |
| Secondary | 6891 | 38.22 (37.51-38.93) | |
| Higher secondary | 2269 | 12.59 (12.10-13.07) | |
| Graduate and above | 2931 | 16.26 (15.72-16.80) | |
| Occupational type | Sedentary work | 2788 | 15.46 (14.94-15.99) |
| Moderate work | 9428 | 52.30 (51.57-53.03) | |
| Hard work | 5812 | 32.24 (31.56-32.92) | |
| Socio-economic strata | Upper | 3858 | 21.40 (20.80-22.00) |
| Middle | 6710 | 37.22 (36.51-37.93) | |
| Lower | 7460 | 41.38 (40.66-42.10) | |
| Residential area | Rural | 10820 | 60.02 (59.30-60.73) |
| Urban | 7208 | 39.98 (39.27-40.70) | |
| Previously diagnosed with diabetes | No | 17624 | 97.76 (97.54-97.98) |
| Yes | 404 | 2.24 (2.02-2.46) | |
| Among diabetics: sought healthcare from | Non-qualified practitioners | 34 | 8.42 (5.70-11.13) |
| Qualified practitioners from private sector | 314 | 77.72 (73.65-81.80) | |
| Qualified practitioners from Government sector | 56 | 13.86 (10.48-17.25) | |
| Fasting capillary blood sugar level | Non-diabetic | 1549 | 80.68 (78.91-82.44) |
| Diabetic | 371 | 19.32 (17.56-21.09) | |
| PP/Random capillary blood sugar level | Non-diabetic | 15268 | 96.75 (96.47-97.03) |
| Diabetic | 513 | 3.25 (2.97-3.53) | |
| Diabetes case status | Non-diabetic | 16930 | 93.91 (93.56-94.26) |
| Diabetic | 1098 | 6.09 (5.74-6.44) | |
| Diabetes diagnosis status | Diagnosed case | 404 | 36.79 (33.94-39.65) |
| Undiagnosed case | 694 | 63.21 (60.35-66.06) | |
| Diabetes control status | Controlled | 211 | 52.62 (47.71-57.53) |
| Uncontrolled | 190 | 47.38 (42.47-52.29) |
Table 1: Distribution of Socio-demographics, burden of diabetes (diagnosed/uncontrolled/undiagnosed) and related care-seeking among study subjects (Na=18028).
Among participants, 404 (2.24%) subjects were diagnosed diabetics among whom 77.72% (n=314) sought treatment from qualified physicians in private sector and 8.42% (n=34) visited non-qualified practitioners. Overall burden of diabetes was 6.09% (n=1098), 63.21% (n=694) of which were undiagnosed so far while 47.38% (n=190) of the previously diagnosed cases had uncontrolled diabetes (Table 1).
Prevalence of diabetes across the strata of socio-demographic factors is presented in (Table 2). Age stratified prevalence of diabetes (14.57%, n=237) was highest among subjects aged >60 years. About 7.74% (n=509) males and 5.14% (n=589) females were suffering from diabetes. Divorced/separated/widowed/widower subgroup had higher prevalence of the disease compared to others (10.16%, n=195). Burden was also high among subjects in sedentary work (8.57%, n=239 for diabetes), upper SES (8.63%, n=333 for diabetes) and urban residence (6.67%, n=481 for diabetes) (Table 2).
| Variables | Labels | Diabetic | |
|---|---|---|---|
| Frequency | Percentages (95% CIb) | ||
| Age group | 18-40 years | 353 | 3.15 (2.83-3.48) |
| 41-60 years | 508 | 9.75 (8.94-10.56) | |
| >60 years | 237 | 14.57 (12.85-16.28) | |
| Gender | Male | 509 | 7.74 (7.09-8.39) |
| Female | 589 | 5.14 (4.74-5.55) | |
| Religion | Hindu | 714 | 5.59 (5.19-5.99) |
| Muslim | 381 | 7.34 (6.63-8.05) | |
| Others | 3 | 4.69 (0.00-10.01) | |
| Caste | Backward castes | 563 | 5.43 (4.99-5.86) |
| General castes | 535 | 6.99 (6.42-7.56) | |
| Marital status | Currently married | 861 | 6.16 (5.76-6.56) |
| Never married | 42 | 1.98 (1.38-2.57) | |
| Divorced/separated/widowed/widower | 195 | 10.16 (8.81-11.51) | |
| Education | Illiterate | 112 | 4.38 (3.59-5.17) |
| Primary | 181 | 5.36 (4.60-6.12) | |
| Secondary | 383 | 5.56 (5.02-6.10) | |
| Higher secondary | 175 | 7.71 (6.61-8.81) | |
| Graduate and above | 247 | 8.43 (7.42-9.43) | |
| Occupational type | Sedentary work | 239 | 8.57 (7.53-9.61) |
| Moderate work | 529 | 5.61 (5.15-6.08) | |
| Hard work | 330 | 5.68 (5.08-6.27) | |
| Socio-economic strata | Upper | 333 | 8.63 (7.74-9.52) |
| Middle | 367 | 5.47 (4.93-6.01) | |
| Lower | 398 | 5.34 (4.83-5.85) | |
| Residential area | Rural | 617 | 5.70 (5.27-6.14) |
| Urban | 481 | 6.67 (6.10-7.25) | |
Table 2: Distribution of diabetes across the socio-demographic strata among the study subjects, Malda, India, 2014 (Na=18028).
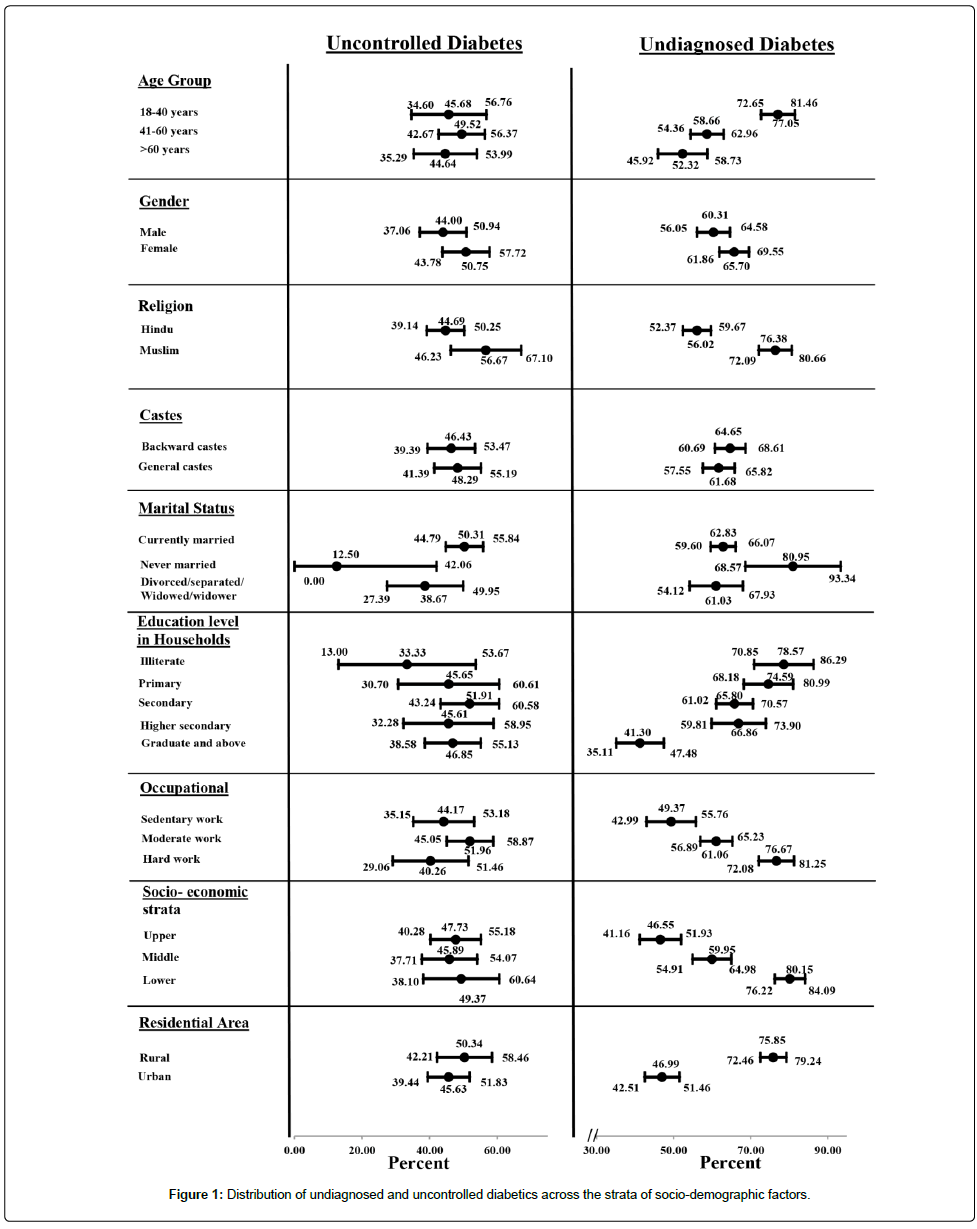
Distribution of the uncontrolled and undiagnosed diabetes is presented in (Figure 1). While the proportion of cases, with uncontrolled diabetes did not vary much (except being much lower (12.5%, n=1) among never married subjects compared to other marital status (50.31%, n=160 among currently married and 38.67%, n=29 among divorced/separated/widowed/widower)) across the strata of different socio-demographic factors, younger subjects (77.05%, n=272 for 18- 40 years age group), Muslims (76.38%, n=291), those who were never married (80.95%, n=34), less educated (78.57%, n=88 for illiterates), hard-workers (76.67%, n=253), subjects with lower SES (80.15%, n=319) and rural residents (75.85%, n=468) had higher proportion of undiagnosed cases (Figure 1).
Logistic regressions revealed that previously diagnosed cases were more likely to be relatively aged (aOR41-60years=4.26(3.24-5.60) and aOR>60years=5.88(4.16-8.32); reference=18-40 years), educated (aORSecondary=1.64(1.03-2.60), aORHigher Secondary=1.75(1.05-2.92) and aOR≥Graduate=2.57(1.58-4.19); reference=Illiterates), SES-wise better (aORMiddle=1.45(1.06-1.98) and aORUpper=2.05(1.46-2.88); reference=Upper) and urban residents (aOR=1.68(1.31-2.16); reference=Rural). Female (aOR=0.55(0.43-0.71); reference=Male), never married (aOR=0.23(0.11-0.48); reference=Currently married) and hard-working subjects (aOR=0.59(0.41-0.83); reference=Sedentary work) were less likely to have a prior diagnosis of diabetes. Compared to the respective reference groups, subjects of higher age (aOR41- 60years=2.74(2.36-3.18) and aOR>60 years=3.79(3.06-4.68)), Muslim religion (aOR=1.69(1.43-1.98); reference=Hindu), divorced/separated/ widowed/widower marital status (aOR=1.25(1.03-1.52)), better education (aORPrimary=1.39(1.09-1.78), aORSecondary=1.41(1.13-1.78), aORHigher, secondary=1.90(1.46-2.48) and aOR≥Graduate=1.82(1.40-2.37)) and upper SES (aOR=1.31(1.08-1.59)] had higher odds of diabetes. On the other hand, females (aOR=0.62(0.53-0.72)) and never married participants (aOR=0.39(0.28-0.55)) were comparatively less likely to be diabetic (Table 3).
| Variables | Labels | Type | Previously diagnosed with diabetes | Diabetic (ref=non-diabetic) | Undiagnosed diabetic (ref=diagnosed) | Uncontrolled diabetic (ref=controlled) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| ORc (95% CId) | p value | ORc (95% CId) | p value | ORc (95% CId) | p value | ORc (95% CId) | p value | |||
| Age group (ref=18-40 years) | 41-60 years | Unadjusted | 5.76 (4.45-7.46) | <0.0001 | 3.32 (2.88-3.82) | <0.0001 | 0.42 (0.31-0.57) | <0.0001 | 1.17 (0.70-1.95) | 0.5576 |
| Adjusted | 4.26 (3.24-5.60) | <0.0001 | 2.74 (2.36-3.18) | <0.0001 | 0.51 (0.36-0.71) | <0.0001 | 1.22 (0.70-2.13) | 0.4741 | ||
| >60 years | Unadjusted | 10.24 (7.66-13.69) | <0.0001 | 5.24 (4.40-6.23) | <0.0001 | 0.33 (0.23-0.47) | <0.0001 | 0.96 (0.54-1.70) | 0.8865 | |
| Adjusted | 5.88 (4.16-8.32) | <0.0001 | 3.79 (3.06-4.68) | <0.0001 | 0.44 (0.29-0.69) | 0.0003 | 1.16 (0.59-2.28) | 0.6623 | ||
| Gender (ref=male) | Female | Unadjusted | 0.57 (0.47-0.69) | <0.0001 | 0.65 (0.57-0.73) | <0.0001 | 1.26 (0.99-1.61) | 0.0649 | 1.31 (0.89-1.94) | 0.1765 |
| Adjusted | 0.55 (0.43-0.71) | <0.0001 | 0.62 (0.53-0.72) | <0.0001 | 1.22 (0.87-1.70) | 0.2521 | 1.50 (0.90-2.50) | 0.1214 | ||
| Religion (ref=Hindu) | Muslim | Unadjusted | 0.70 (0.55-0.89) | 0.0032 | 1.34 (1.18-1.52) | <0.0001 | 2.54 (1.92-3.35) | <0.0001 | 1.62 (1.01-2.60) | 0.0462 |
| Adjusted | 1.28 (0.97-1.71) | 0.084 | 1.69 (1.43-1.98) | <0.0001 | 1.26 (0.87-1.83) | 0.231 | 1.72 (0.96-3.09) | 0.068 | ||
| Others | Unadjusted | - | - | 0.83 (0.26-2.65) | 0.7548 | - | - | - | - | |
| Adjusted | - | - | 1.18 (0.36-3.83) | 0.7883 | - | - | - | - | ||
| Caste (ref= General castes) | Backward castes | Unadjusted | 0.71 (0.58-0.87) | 0.0007 | 0.76 (0.68-0.86) | <0.0001 | 1.14 (0.89-1.45) | 0.3076 | 0.93 (0.63-1.37) | 0.7087 |
| Adjusted | 0.88 (0.71-1.10) | 0.2535 | 0.95 (0.83-1.09) | 0.4609 | 1.22 (0.91-1.64) | 0.1926 | 1.00 (0.65-1.53) | 0.9974 | ||
| Marital status (ref=Currently married) | Never married | Unadjusted | 0.16 (0.08-0.33) | <0.0001 | 0.31 (0.22-0.42) | <0.0001 | 2.51 (1.15-5.50) | 0.0209 | 0.14 (0.02-1.16) | 0.0685 |
| Adjusted | 0.23 (0.11-0.48) | <0.0001 | 0.39 (0.28-0.55) | <0.0001 | 1.96 (0.83-4.63) | 0.1273 | 0.14 (0.02-1.25) | 0.0785 | ||
| Divorced/separated/ widowed/widower | Unadjusted | 1.76 (1.36-2.27) | <0.0001 | 1.72 (1.46-2.03) | <0.0001 | 0.93 (0.67-1.28) | 0.6377 | 0.62 (0.37-1.04) | 0.0708 | |
| Adjusted | 1.08 (0.80-1.47) | 0.613 | 1.25 (1.03-1.52) | 0.0255 | 1.20 (0.79-1.82) | 0.4037 | 0.49 (0.26-0.95) | 0.0335 | ||
| Education (ref=Illiterate) | Primary | Unadjusted | 1.46 (0.89-2.39) | 0.137 | 1.24 (0.97-1.57) | 0.0854 | 0.80 (0.46-1.40) | 0.4373 | 1.68 (0.60-4.70) | 0.3227 |
| Adjusted | 1.52 (0.92-2.51) | 0.1031 | 1.39 (1.09-1.78) | 0.0083 | 0.89 (0.49-1.60) | 0.6956 | 2.06 (0.69-6.14) | 0.1932 | ||
| Secondary | Unadjusted | 2.05 (1.32-3.17) | 0.0013 | 1.29 (1.04-1.60) | 0.0225 | 0.53 (0.32-0.86) | 0.0112 | 2.16 (0.86-5.39) | 0.0994 | |
| Adjusted | 1.64 (1.03-2.60) | 0.0355 | 1.41 (1.13-1.78) | 0.0029 | 0.89 (0.52-1.53) | 0.6717 | 3.18 (1.14-8.89) | 0.0275 | ||
| Higher secondary | Unadjusted | 2.77 (1.72-4.47) | <0.0001 | 1.83 (1.43-2.33) | <0.0001 | 0.55 (0.32-0.95) | 0.0333 | 1.68 (0.62-4.54) | 0.3088 | |
| Adjusted | 1.75 (1.05-2.92) | 0.0326 | 1.90 (1.46-2.48) | <0.0001 | 1.05 (0.57-1.94) | 0.8804 | 2.37 (0.77-7.31) | 0.1336 | ||
| Graduate and above | Unadjusted | 5.50 (3.56-8.49) | <0.0001 | 2.01 (1.60-2.53) | <0.0001 | 0.19 (0.11-0.32) | <0.0001 | 1.76 (0.71-4.38) | 0.222 | |
| Adjusted | 2.57 (1.58-4.19) | 0.0001 | 1.82 (1.40-2.37) | <0.0001 | 0.55 (0.30-1.01) | 0.0546 | 2.35 (0.80-6.89) | 0.1186 | ||
| Occupational type (ref=Sedentary work) | Moderate work | Unadjusted | 0.49 (0.39-0.62) | <0.0001 | 0.63 (0.54-0.74) | <0.0001 | 1.61 (1.18-2.19) | 0.0025 | 1.37 (0.87-2.15) | 0.1759 |
| Adjusted | 0.87 (0.66-1.16) | 0.3567 | 0.96 (0.79-1.17) | 0.6678 | 1.18 (0.78-1.78) | 0.4261 | 1.01 (0.57-1.80) | 0.9686 | ||
| Hard work | Unadjusted | 0.30 (0.22-0.40) | <0.0001 | 0.64 (0.54-0.76) | <0.0001 | 3.37 (2.35-4.83) | <0.0001 | 0.85 (0.48-1.52) | 0.5886 | |
| Adjusted | 0.59 (0.41-0.83) | 0.0025 | 0.83 (0.67-1.03) | 0.0905 | 1.57 (0.99-2.47) | 0.0555 | 0.61 (0.30-1.24) | 0.1744 | ||
| Socio-economic strata (ref=Lower) | Upper | Unadjusted | 4.52 (3.46-5.91) | <0.0001 | 1.68 (1.44-1.95) | <0.0001 | 0.22 (0.16-0.30) | <0.0001 | 0.94 (0.55-1.59) | 0.8082 |
| Adjusted | 2.05 (1.46-2.88) | <0.0001 | 1.31 (1.08-1.59) | 0.0068 | 0.50 (0.33-0.77) | 0.0016 | 0.80 (0.38-1.65) | 0.5383 | ||
| Middle | Unadjusted | 2.09 (1.59-2.76) | <0.0001 | 1.03 (0.89-1.19) | 0.7239 | 0.37 (0.27-0.51) | <0.0001 | 0.87 (0.50-1.51) | 0.6181 | |
| Adjusted | 1.45 (1.06-1.98) | 0.0207 | 1.00 (0.84-1.18) | 0.9729 | 0.62 (0.42-0.92) | 0.0161 | 0.68 (0.34-1.34) | 0.2589 | ||
| Residential area (ref=rural) | Urban | Unadjusted | 2.63 (2.14-3.22) | <0.0001 | 1.18 (1.05-1.34) | 0.0076 | 0.28 (0.22-0.37) | <0.0001 | 0.83 (0.55-1.24) | 0.3625 |
| Adjusted | 1.68 (1.31-2.16) | <0.0001 | 1.12 (0.96-1.31) | 0.1534 | 0.49 (0.36-0.68) | <0.0001 | 0.94 (0.56-1.55) | 0.7955 | ||
Table 3: Associations of socio-behavioral correlates with diagnosed, undiagnosed and uncontrolled diabetes among study subjects (Nb=18028).
Subjects having higher age (aOR41-60 years=0.51(0.36-0.71) and aOR>60 years=0.44(0.29-0.69)), better SES (aORMiddle=0.62(0.42-0.92) and aORUpper=0.50(0.33-0.77)) and urban residence (aOR=0.49(0.36-0.68)) were less likely to have undiagnosed diabetes. Although the multiple regressions lacked sufficient power for the adjusted estimates, as per the unadjusted ORs it seemed that: among diabetics, educated subjects (ORSecondary=0.53(0.32-0.86), ORHigher secondary=0.55(0.32-0.95) and OR≥Graduate=0.19(0.11-0.32)) were less likely and Muslims (OR=2.54(1.92- 3.35)), never married (OR=2.51(1.15-5.50)) and moderate/hardworkers (ORModerate-worker=1.61(1.18-2.19), ORHard-worker=3.37(2.35-4.83)) were more likely to remain undiagnosed (Table 3).
Among those who were previously diagnosed as a case of diabetes, divorced/separated/ widowed/widowers had lower (aOR=0.49(0.26- 0.95)) and subjects with secondary level of familial education had higher (aOR=3.18(1.14-8.89)) odds of having uncontrolled diabetes. According to the unadjusted model, likelihood of having uncontrolled diabetes seemed to be higher among Muslims also (OR=1.62(1.01- 2.60)) (Table 4).
| Variables | Categories | Type of analyses | Among diabetics: sought healthcare from (ref=Qualified physician from Governmental sector) | |||
|---|---|---|---|---|---|---|
| Non-qualified practitioner | Qualified practitioner from private sector | |||||
| ORc (95% CId) | p value | ORc (95% CId) | p value | |||
| Age group (ref=18-40 years) | 41-60 years | Unadjusted | 0.47 (0.16-1.36) | 0.1626 | 0.95 (0.44-2.08) | 0.9055 |
| Adjusted | 0.40 (0.13-1.29) | 0.1247 | 0.69 (0.30-1.62) | 0.3969 | ||
| >60 years | Unadjusted | 0.43 (0.13-1.42) | 0.1654 | 0.86 (0.37-2.01) | 0.7327 | |
| Adjusted | 0.27 (0.06-1.16) | 0.0775 | 0.56 (0.20-1.56) | 0.2679 | ||
| Gender (ref=male) | Female | Unadjusted | 1.21 (0.52-2.84) | 0.6638 | 1.07 (0.61-1.90) | 0.8055 |
| Adjusted | 1.51 (0.49-4.65) | 0.4713 | 1.48 (0.68-3.19) | 0.3221 | ||
| Religion (ref=Hindu) | Muslim | Unadjusted | 1.10 (0.44-2.75) | 0.8428 | 0.56 (0.30-1.06) | 0.0769 |
| Adjusted | 0.50 (0.15-1.66) | 0.2585 | 0.41 (0.17-0.95) | 0.0381 | ||
| Caste (ref= General castes) | Backward castes | Unadjusted | 0.84 (0.36-1.99) | 0.6975 | 0.68 (0.38-1.20) | 0.1831 |
| Adjusted | 0.64 (0.24-1.70) | 0.3706 | 0.50 (0.26-0.98) | 0.0434 | ||
| Marital status (ref=Currently married) | Never married | Unadjusted | - | - | - | - |
| Adjusted | - | - | - | - | ||
| Divorced/separated/widowed/widower | Unadjusted | 2.35 (0.80-6.87) | 0.1194 | 1.42 (0.64-3.17) | 0.389 | |
| Adjusted | 2.73 (0.65-11.39) | 0.1693 | 1.71 (0.60-4.83) | 0.3126 | ||
| Education (ref=Illiterate) | Primary | Unadjusted | 2.23 (0.36-13.96) | 0.3924 | 1.19 (0.38-3.70) | 0.7664 |
| Adjusted | 3.93 (0.54-28.42) | 0.1757 | 1.47 (0.42-5.12) | 0.5434 | ||
| Secondary | Unadjusted | 2.33 (0.41-13.20) | 0.3379 | 2.62 (0.94-7.32) | 0.0664 | |
| Adjusted | 5.83 (0.85-40.21) | 0.0736 | 3.80 (1.14-12.66) | 0.0298 | ||
| Higher secondary | Unadjusted | 2.72 (0.43-17.42) | 0.2903 | 2.18 (0.69-6.88) | 0.1848 | |
| Adjusted | 8.05 (0.98-66.35) | 0.0528 | 3.19 (0.82-12.47) | 0.0955 | ||
| Graduate and above | Unadjusted | 1.91 (0.30-12.26) | 0.4955 | 5.43 (1.83-16.12) | 0.0023 | |
| Adjusted | 7.45 (0.84-66.46) | 0.0722 | 8.42 (2.17-32.74) | 0.0021 | ||
| Occupational type (ref=Sedentary work) | Moderate work | Unadjusted | 0.63 (0.23-1.70) | 0.3594 | 0.92 (0.48-1.75) | 0.798 |
| Adjusted | 0.48 (0.13-1.83) | 0.284 | 0.97 (0.41-2.33) | 0.9499 | ||
| Hard work | Unadjusted | 2.21 (0.65-7.54) | 0.2062 | 1.57 (0.61-4.00) | 0.3482 | |
| Adjusted | 1.90 (0.41-8.73) | 0.4093 | 3.09 (1.01-9.52) | 0.0491 | ||
| Socio-economic strata (ref=Lower) | Upper | Unadjusted | 0.69 (0.23-2.06) | 0.5013 | 2.35 (1.08-5.09) | 0.0307 |
| Adjusted | 0.91 (0.21-4.04) | 0.9035 | 1.46 (0.51-4.17) | 0.4834 | ||
| Middle | Unadjusted | 0.56 (0.20-1.57) | 0.2715 | 1.16 (0.56-2.42) | 0.6871 | |
| Adjusted | 0.68 (0.19-2.49) | 0.5628 | 0.88 (0.35-2.24) | 0.7952 | ||
| Residential area (ref=rural=1) | Urban | Unadjusted | 0.41 (0.17-0.97) | 0.043 | 0.94 (0.52-1.71) | 0.8373 |
| Adjusted | 0.28 (0.09-0.87)) | 0.0271 | 0.51 (0.22-1.15) | 0.1045 | ||
Table 4: Associations of socio-behavioral correlates with health-seeking pattern among diabetics (Nb=18028).
Regarding healthcare-seeking, the odds of seeking healthcare from nonqualified practitioners were less for urban diabetics (aOR=0.28(0.09-0.87)) compared to their rural counterparts. Diabetics of Muslim religion (aOR=0.41(0.17-0.95)) and backward caste (aOR=0.50(0.26-0.98)) were less likely while educated patients (aORSecondary=3.80(1.14-12.66) and aOR≥Graduate=8.42(2.17-32.74)) and those in hard-working jobs (aOR=3.09(1.01-9.52)) were more likely to visit qualified practitioner from private sector. Likelihood of visiting qualified physicians from private sector also seemed to be higher among cases belonging to upper SES (OR=2.35(1.08-5.09)).
Discussion
In this current study involving 18028 representative subjects from one of the poorest districts (Malda) of the West Bengal state of eastern India, the prevalence of diabetes was estimated to be 6.09% which was a bit lower than the adult prevalence of diabetes observed in other parts of India (10.4% in Tamil Nadu, 8.4% in Maharashtra and 13.6% in Chandigarh in 2010) but slightly higher than the value reported from the neighboring state of Jharkhand (5.3%) and urban part of West Bengal (4.8%) [13] The observed value was also lower than the global prevalence of diabetes among adults (9%) in 2014 [6], the prevalence reported from similar settings in Afghanistan (8.5%), Bangladesh (8.6%), China (8.0%), Indonesia (8.0%), Malaysia (10.2%), Thailand (8.9%), Nepal (8.8%), Pakistan (9.9%), Japan (7.3%), South Africa (11.8%) and Sri Lanka (8.3%), in 2010 [7].
Although this lower percentage could be interpreted as an improvement in the situation regarding diabetes epidemic in this poor-resource area, the actual picture might be quite reverse. Only 2.24% residents were previously diagnosed as diabetic, 47.38% of whom remained uncontrolled as they were found to be diabetic in our investigation also and 63.21% of the diabetics in the study area were undiagnosed so far. This burden of undiagnosed diabetes among adults seemed to be alarmingly high compared to the reported corresponding values from elsewhere (4.5% in Malaysia in 2006) [32] as well as other parts of India (10.5% in central and urban Kerala, 9.1% in Chennai, 40% in southern India as a whole and 4.25% in Kashmir) [33-36]. Compared to the global (46.3% in 2013) [2] and Indian (53.1%, 35.5 million undiagnosed among 66.8 million diabetics) [1] estimates for undiagnosed diabetes by IDF this value was also very high. But the results were not surprising keeping the respective observations of Ramachandran et al. and Graber et al. in mind who previously found that >70% diabetics in rural India [35] and 71% of diabetic patients admitted in a hospital in US [37] remained undiagnosed. The detected burden of uncontrolled cases also corroborated with previously observed level of poor glycemic control among Indian diabetics which ranged between 42-70% [3,11,34,38,39].
This high prevalence of uncontrolled and undiagnosed diabetics in Malda might have emphasized upon poor healthcare-seeking behavior of the study population as evident from the observation that among the diagnosed diabetics, 8.42% sought care from non-qualified practitioners. It was very likely that diagnosis of only those diabetics were possible who sought some healthcare services either for some symptoms related to diabetes or due to some other reasons (e.g. routine checkup). Residents who got tested for diabetes could also be the more health-aware fraction of the population, having a relatively better healthcare-seeking and utilization. Owing to the largely asymptomatic nature of diabetes, especially in the early stages, it was also possible that only complicated cases were being diagnosed while being symptomatic and thus controlling the disease course among those late-diagnosed cases probably were more difficult. Cumulatively it seemed that infrastructural development and behavioral modification programs were the need of the hour to ensure early diagnosis and appropriate treatment for minimizing the burden of diagnosed, undiagnosed and uncontrolled diabetes in this poor-resource setting.
Regarding the distribution of diabetes we observed that prevalence increased with age, being highest among subjects aged >60 years (14.57%) which corroborated with the global scenario [2,9,14,32]. Similar findings were also reported from studies conducted in Kashmir [36], urban slums of northern India [40] and the National Urban Survey in six major Indian cities [41]. Prevalence was higher among males (7.74 vs 5.14) compared to females alike other studies in India [35,40,42] and abroad [14]. Muslims (7.34%), general caste (6.99%), divorced/ separated/widowed/widower (10.16%), more educated (8.43%), sedentary workers (8.57%) and those who were economically better-off (8.63) had higher diabetic prevalence among respective categories. The likelihood of being diabetic was more among urban residents (6.67%) than their rural counterparts, which also corroborated with previous observations from different parts of India [36,43].
Consistent with other studies in this country (both at the national level and in the southern parts), we found that odds of having diabetes increased among adults with advancing age [13,33,35,41] and females were less likely to be diabetic compared to males [13]. Muslims and general castes had higher odds of being diabetic compared to Hindus and backward castes respectively. Compared to currently married subjects, those who were never married had lower likelihood of being diabetic while those who were divorced/separated/widowed had higher odds of diabetes. With increase in educational level among adults in the households, odds of suffering from diabetes increased in the present study. Higher education was also found to be a significant correlate of diabetes among adults aged ≥20 years in Southern India [36]. Participants in hard-working jobs were less likely to have diabetes compared to those habituated to sedentary work, which corroborated with the National Urban Diabetic Survey and the Non-communicable Diseases Risk Factor Surveillance in India [41,44].
Similar to prior studies [13,41,43], subjects belonging to upper SES had higher risk of diabetes compared to poorer subjects in Malda district. With reference to rural, urban residents were more likely to be diabetic in our study. Similar findings were reported in other population-based studies among individuals aged 15 years or more in India [13,41,44].
In a previous study in Indonesia, age was found to be an important predictor for undiagnosed diabetes [45]. In the current study it was observed that compared to younger, older subjects were less likely to have undiagnosed diabetes. Higher scope and requirement for testing of sugar levels (routinely or due to other co-morbidities) probability increased the chance of diagnosis of diabetes with advancing age.
Female diabetics were more likely to remain undiagnosed compared to their male counterparts in Malda. Keeping the social position of women in a poor-resource Indian setting it seemed that comparatively higher self-neglect, poorer awareness and inappropriate perception of own health might be among the potential explanations.
Subjects belonging to relatively higher SES had lower odds of having undiagnosed diabetes compared to poorer subjects. Similar observation was reported from Bangladesh by Islam et al. [46]. Better awareness, affordability and healthcare-seeking among diabetics in higher SES probably resulted in increased probability of being tested and thus being diagnosed.
Being consistent with the prior findings from another Indian study, we also found that urban subjects were less likely to have undiagnosed diabetes with reference to the rural residents [47]. Potential explanations might include relatively better awareness, availability of testing facilities, healthcare access and utilization in urban areas compared to rural.
In the current study it was observed that subjects with secondary level (compared to illiterate) of education were more likely while divorced/ separated/widowed/widowers (compared to currently married) were less likely to have uncontrolled diabetes. For most of the other variables we did not have sufficient power to infer. Higher education seemed to instill improved awareness and thus better glycemic control among diabetics, as was observed previously [3]. Muslim diabetics also seemed more likely to have poorer control on their disease status probably due to different food habits and lifestyle. Awareness and healthcare-seeking could also be considered as other issues.
Data on healthcare-seeking behavior among patients diagnosed with diabetes is limited, more so in developing countries. With increase in educational level, chances of seeking healthcare from qualified private practitioner increased among diabetics of Malda. An evaluation of healthcare-seeking among diabetics in Malaysia revealed an independent association of higher education with treatment-seeking [48]. Education was also associated with healthcare-seeking behavior and compliance among diabetic patients in rural areas of South India [49]. Probably higher education resulted in better knowledge, attitude and practice regarding healthcare-seeking among diabetics in general. Urban diabetics had lower odds of seeking care from non-qualified practitioners while Muslims and backward castes were less likely to seek care from qualified private practitioners. On the other hand diabetics who were hard working had higher odds of seeking care from qualified private practitioner.
This study had certain limitations. Like any other cross-sectional study, causal interpretation of the observed associations is not recommended. Results of our study should also be extrapolated beyond the study sample with caution. Due to the potential vulnerability to temporal ambiguity by design, some of our observations might have suffered from reverse causation. Residual confounding due to variables not included in our analyses could also be an issue. Information bias due to misclassification of self-reported information should always be kept in mind, especially due to the potential for differential recall. Relatively higher participation of the female members during the household survey could also be considered as a limitation.
Despite the aforementioned limitation, it seemed that by virtue of a large, representative population-based sampling and robust analyses our study could generate important insight regarding the burden and correlates of uncontrolled and undiagnosed diabetics in a poor resource setting of our country. Policy makers are likely to be able to design appropriately targeted intervention based on the findings of our result.
Burden of undiagnosed and uncontrolled diabetes was alarmingly high in Malda. Urgent intervention to improve detection, control and prevention of diabetes, targeting young adults, females, rural residents, Muslims, married subjects and those having lower SES seemed to be the need of the hour. Effective utilization of services for early detection of diabetes & initiation of treatment could be achieved through successful awareness generation followed by community participation. Nonqualified practitioners should be adequately trained to motivate and mobilize the individuals and the community to ensure early diagnosis of diabetics, their appropriate treatment and referral. Qualified physicians should also be trained suitably and provided with necessary logistics to motivate individuals regarding healthy lifestyle, appropriate testing, compliance to treatment and regular follow up to ensure prevention of the disease, early diagnosis and appropriate treatment. Extensive community awareness involving community leaders would help in minimizing the burden of Diabetes in these poorresource settings.
Acknowledgments
The study was funded (Grant No. 65/56/2012-13ECD-II) by Indian Council of Medical Research (https://icmr.nic.in/Grants/Grants.html).
Authors are hereby acknowledging their gratitude to Professor Dr. V. I. Mathan (Former Chair, National Institute of Epidemiology, Chennai and Chairman of the Scientific Advisory Committee, NICED, Kolkata) and Dr. Sekhar Chakrabarti (Scientist G and Director in Charge, National Institute of Cholera and Enteric Diseases, Kolkata) for critically reviewing the proposal and the result. The authors also acknowledge the support of Dr. V. M Katoch (Director General, Indian Council of medical Research, Government of India) and Dr. Rashmi Arora, (Scientist G , Indian Council of Medical Research), for providing necessary logistic and administrative support. The Office of the Chief Medical Officer of Malda provided necessary permission and logistic support for the study. The authors are indebted to Prof (Dr.) Rama Prasad Ray, Dept of Community Medicine, Malda Medical College and Hospital for providing critical inputs and operational help in conducting the study. In addition authors also acknowledge the cooperation of the participants and the project staff.
Conflict of interests
None to declare.
References
- (2014)Regional Factsheets, IDF Diabetic Atlas. International Diabetes Federation. sixth Edition: 2014 Update.
- (2013)6th edn, International DiabetiFederation,IDF Diabetes Atlas. Intenational Diabetes Federation.
- Nagpal J, Bhartia A (2006) Quality of diabetes care in the middle- and high-income group populace: the Delhi Diabetes Community (DEDICOM) survey.Diabetes Care 29: 2341-2348.
- Scheen AJ (2003) Pathophysiology of type 2 diabetes. ActaClinBelg 58: 335-341.
- (2014)Statistics about diabetes, Data from the National Diabetes Statisitcs Report . American Diabetes Association
- Whiting DR, Guariguata L, Weil C, Shaw J (2011) IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030.Diabetes Res ClinPract94: 311-321.
- Hjelm K, Atwine F (2011) Health-care seeking behaviour among persons with diabetes in Uganda: an interview study.BMC Int Health Hum Rights 11: 11.
- Joshi SR, Saboo B, Vadivale M, Dani SI, Mithal A, et al. (2012) Prevalence of diagnosed and undiagnosed diabetes and hypertension in India-results from the Screening India's Twin Epidemic (SITE) study.Diabetes TechnolTher 14: 8-15.
- Kaku K (2010) Pathophysiology of Type 2 Diabetes anditstreatment policy.JMAJ 53: 41–46.
- Anjana RM, Pradeepa R, Deepa M (2011) Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdiaDIABetes (ICMR-INDIAB) study. Diabetologia 54: 3022-3027.
- Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030.Diabetes Care 27: 1047-1053.
- Kanungo S, Bhowmik K, Mahapatra T, Mahapatra S, Bhadra UK, et al. (2015) Perceived morbidity, healthcare-seeking behavior and their determinants in a poor-resource setting: observation from India.PLoS One 10: e0125865.
- Mohan V, Sandeep S, Deepa R, Shah B, Varghese C (2007) Epidemiology of type 2 diabetes: Indian scenario.Indian J Med Res 125: 217-230.
- Chow CK, Raju PK, Raju R, Reddy KS, Cardona M, et al. (2006) The prevalence and management of diabetes in rural India.Diabetes Care 29: 1717-1718.
- (2010) Health on the march 2010-2011, State Bureau of Health Intelligence, Govt. of West Bengal.
- Das S, Maji D, Majumder PP (2005) Prevalence of diabetes in various habitats of West Bengal, India.J Indian Med Assoc 103: 580-584.
- (2013) User Instruction Guide, SD CodeFreeâ„¢ Blood Glucose Monitoring System. SD Biocensor INC. Korea.
- (2012) Diagnosis of Diabetes and Prediabetes, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Nationl Institute of Health (NIH).
- (2012) Standards of Medical Care in Diabetes, American Diabetes Association. Diabetes Care 35: S11-S63
- (2006) WHO Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia, Report of a World Health Organization (WHO)/International Diabetes Federation (IDF) consultation.
- Bharati DR, Pal R, Rekha R, Yamuna TV (2011) Evaluation of the burden of type 2 diabetes mellitus in population of Puducherry, South India.Diabetes MetabSyndr 5: 12-16.
- Hosmer JDW, Lemeshow S, Sturdivant RX (2013). 3rd edn. Applied logistic regression: Wiley.
- Kwak C, Clayton-Matthews A (2002) Multinomial logistic regression.Nurs Res 51: 404-410.
- Letchuman GR, Nazaimoon WM, Mohamad WB, Chandran LR, Tee GH, et al. (2010) Prevalence of diabetes in the Malaysian National Health Morbidity Survey III 2006.Med J Malaysia 65: 180-186.
- Menon VU, Kumar KV, Gilchrist A, Sugathan TN, Sundaram KR, et al. (2006) Prevalence of known and undetected diabetes and associated risk factors in central Kerala--ADEPS.Diabetes Res ClinPract 74: 289-294.
- Ramachandran A, Mary S,Sathish CK, Selvam S, Seeli AC, et al. (2008) Population based study of quality of diabetes care in southern India.J Assoc Physicians India 56: 513-516.
- Ramachandran A, Mary S, Yamuna A, Murugesan N, Snehalatha C (2008) High prevalence of diabetes and cardiovascular risk factors associated with urbanization in India.Diabetes Care 31: 893-898.
- Zargar AH, Khan AK, Masoodi SR, Laway BA, Wani AI, et al. (2000) Prevalence of type 2 diabetes mellitus and impaired glucose tolerance in the Kashmir Valley of the Indian subcontinent.Diabetes Res ClinPract 47: 135-146.
- Graber AL, McDaniel H, Sussman C, Wooldridge K (1986) Clinical characteristics of hospitalized diabetic patients.South Med J 79: 281-284.
- Raheja BS, Kapur A, Bhoraskar A, Sathe SR, Jorgensen LN, et al. (2001) DiabCare Asia--India Study: diabetes care in India--current status.J Assoc Physicians India 49: 717-722.
- Ramachandran A, Das A, Joshi S, Yajnik C, Shah S, et al.(2010) Current status of diabetes in India and need for novel therapeutic agents. J Assoc Physicians India 58: 7-9.
- Misra A, Pandey RM, Devi JR, Sharma R, Vikram NK, et al. (2001) High prevalence of diabetes, obesity and dyslipidaemia in urban slum population in northern India.Int J ObesRelatMetabDisord 25: 1722-1729.
- Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, et al. (2001) High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey.Diabetologia 44: 1094-1101.
- Gupta A, Gupta R, Sarna M, Rastogi S, Gupta VP, et al. (2003) Prevalence of diabetes, impaired fasting glucose and insulin resistance syndrome in an urban Indian population.Diabetes Res ClinPract 61: 69-76.
- Raghupathy P, Antonisamy B, Fall CH, Geethanjali FS, Leary SD, et al. (2007) High prevalence of glucose intolerance even among young adults in south India.Diabetes Res ClinPract 77: 269-279.
- Mohan V, Mathur P, Deepa R, Deepa M, Shukla DK, et al. (2008) Urban rural differences in prevalence of self-reported diabetes in India--the WHO-ICMR Indian NCD risk factor surveillance.Diabetes Res ClinPract 80: 159-168.
- Pramono LA, Setiati S, Soewondo P, Subekti I, Adisasmita A, et al. (2010) Prevalence and predictors of undiagnosed diabetes mellitus in Indonesia.Acta Med Indones 42: 216-223.
- Islam FM, Chakrabarti R, Islam MT (2016)Prediabetes, diagnosed and undiagnosed diabetes, their risk factors and association with knowledge of diabetes in rural Bangladesh: The Bangladesh Population-based Diabetes and Eye Study. J Diabetes 8: 260-268.
- Anjana RM, Ali MK, Pradeepa R, Deepa M, Datta M, et al. (2011) The need for obtaining accurate nationwide estimates of diabetes prevalence in India - rationale for a national study on diabetes.Indian J Med Res 133: 369-380.
- Hasan SS, Ahmed SI, Bukhari NI, Loon WC (2009) Use of complementary and alternative medicine among patients with chronic diseases at outpatient clinics. Complement TherClinPract 15: 152-7.
- Srinivas G, Suresh E, Jagadeesan M, Amalraj E, Datta M (2002) Treatment-seeking behavior and compliance of diabetic patients in a rural area of south India.Ann N Y AcadSci 958: 420-424.
Citation: Kanungo S, Mahapatra T, Bhowmik K, Mahapatra S, Saha J, et al. (2016) Diabetes Scenario in a Backward Rural District Population of India and Need for Restructuring of Health Care Delivery Services. Epidemiol 6:224. DOI: 10.4172/2161-1165.1000224
Copyright: © 2016 Kanungo S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 13780
- [From(publication date): 4-2016 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 12701
- PDF downloads: 1079