Diabetes Knowledge in Youth with T1DM and their Caregivers-A Cross- Sectional Study
Received: 24-Jan-2018 / Accepted Date: 09-Feb-2018 / Published Date: 12-Feb-2018
Abstract
Purpose: The purpose of this study was to evaluate diabetes knowledge in youth with T1DM and their caregivers and its association with clinical outcomes, demographic, and socioeconomic characteristics. Methods: A cross-sectional analysis was conducted. Patients with T1DM aged 2 to 21 were enrolled. A diabetes knowledge questionnaire adapted from a combination of validated studies was completed by adolescents ≥ 14 years and caregivers of children Ãâ¹Ãâ14 years. Diabetes knowledge was considered adequate for ≥ 80% correct answers. Logistic regression was used to associate diabetes knowledge with clinical and demographic data. Results: Overall diabetes knowledge was good, with average scores of 86% and 84% correct responses among adolescents and parents, respectively. Better diabetes knowledge was associated with A1C ≤ 9%, in particular knowledge of nutrition in parents of small children and knowledge of pathophysiology in both groups. Weaker diabetes knowledge was associated with lower socioeconomic status. Overall diabetes knowledge scores were not associated with time since T1DM diagnosis, but knowledge of self-care was better with longer time since diagnosis in adolescence. Conclusions: Proficiency in carbohydrate counting in parents of younger children might have higher clinical impact than in adolescents. Diabetes education curricula should be tailored towards individual patients taking into consideration their socio-economic needs. Diabetes centers should offer re-education on diabetes, in particular, review of pathophysiology, nutrition and carbohydrate counting.
Keywords: T1DM; Pediatric diabetes; Diabetes education
Abbreviations
DSMS: Diabetes Self-Management Skills; DKA: Diabetes Ketoacidosis; ADK: Adequate Diabetes Knowledge; ADA: American Diabetes Association
Introduction
Type 1 diabetes is one of the most prevalent chronic health conditions in youth around the globe [1]. Although treatment of type 1 diabetes has improved dramatically over the past few decades with the implementation of intensive insulin treatments and the advent of insulin pumps and continuous glucose monitors, many pediatric patients are unable to maintain recommended A1C levels and are at increased risk of developing complications [2].
Diabetes treatment often requires complex regimens including calculation of the carbohydrate content of meals as well as frequent self-administration of insulin, therefore it is essential that people living with diabetes are well educated about their condition and make confident decisions regarding their own treatment. In the current standards of care in diabetes treatment, the American Diabetes Association (ADA) places particular emphasis on the importance of diabetes self-management education and diabetes self-management support [3]. Prominent in its outline are specific goals for the Diabetes treatment often requires complex regimens including calculation of the carbohydrate content of meals as well as frequent self-administration of insulin, therefore it is essential that people living with diabetes are well educated about their condition and make confident decisions regarding their own treatment. In the current standards of care in diabetes treatment, the American Diabetes Association (ADA) places particular emphasis on the importance of diabetes self-management education and diabetes self-management support [3]. Prominent in its outline are specific goals for the education of patients with diabetes, which fall into the following categories: Medical nutrition therapy, physical activity, and smoking cessation.
ADA guidelines remain vague with respect to how exactly patients with diabetes should be educated about their disease, and different clinics have developed site-specific curricula for their patients with diabetes. While many studies have demonstrated that better adherence to treatment guidelines is correlated with better control of patient’s A1C [4], and may consequentially mitigate their risk of developing complications associated with chronically elevated blood glucose later in life, the role that education plays in this effect has not been thoroughly investigated.
Several studies have analyzed the logical connection between patients’ knowledge of diabetes and their self-management of the condition (most frequently quantified by A1C values). One study found that patients who knew their recent A1C values also demonstrated better glycemic control [5], but findings in other studies have been inconsistent regarding this association [6,7].
A recent study found that lower A1C values are associated with greater knowledge of diabetes [8], however a previous study did not find a significant correlation between these two variables [7]. Importantly, the most effective way to educate patients in order to improve their outcomes remains unclear. It is also unknown what specific elements of a diabetes education curriculum are essential for better clinical outcomes.
In this study, we sought to evaluate diabetes knowledge in youth with T1DM and their caregivers and its association with clinical outcomes. We hypothesized that better diabetes knowledge is associated with a lower A1C. We attempted to determine predictors of adequate diabetes knowledge.
Methods
Study design/sample: To study diabetes knowledge in children with T1DM and their caregivers and its association with clinical outcomes, we conducted a cross-sectional descriptive study and approached all patients with T1DM aged 2-21 who had been diagnosed for at least 3 months coming for their routine follow-up appointments in our clinic during 2011-2012 (~750 clinic patients). Patients in state custody were excluded from the study. Our study included two groups of respondents: Adolescent participants aged 14 years and older and caregivers of the younger children.
Setting
This study was performed at a moderately sized outpatient pediatric diabetes program located at an academic tertiary health care center in Springfield, Massachusetts. The program offers comprehensive diabetes education by certified diabetes educators and a registered dietitian that consists of an introductory 3-month course and ongoing individualized review sessions.
The initial in-depth course includes intense 3-4 hour sessions on two consecutive days that cover pathophysiology of diabetes, diabetes self-management skills (DSMS) and diabetes diet. Published [9] and self-developed diabetes education materials are used as a reference and are provided to the families. The initial 2-day course is followed by daily phone nurse/physician interaction with the family for the first week, and clinic visits after 1 week, 1 month, and 2 months.
Patients also meet with a pediatric endocrinologist at all appointments who adjusts insulin doses and guides diabetes education. Beyond the initial 3-month period, patients are followed quarterly, and on-going diabetes education is provided based on their knowledge, needs, and deficiencies in diabetes self-care. These review sessions usually focus on the management of hypo- and hyperglycemia, carbohydrate counting, blood glucose pattern recognition and insulin dose adjustments, blood sugar control around sports activities, and transitioning to use of insulin pump therapy or continuous glucose monitoring.
Data collection
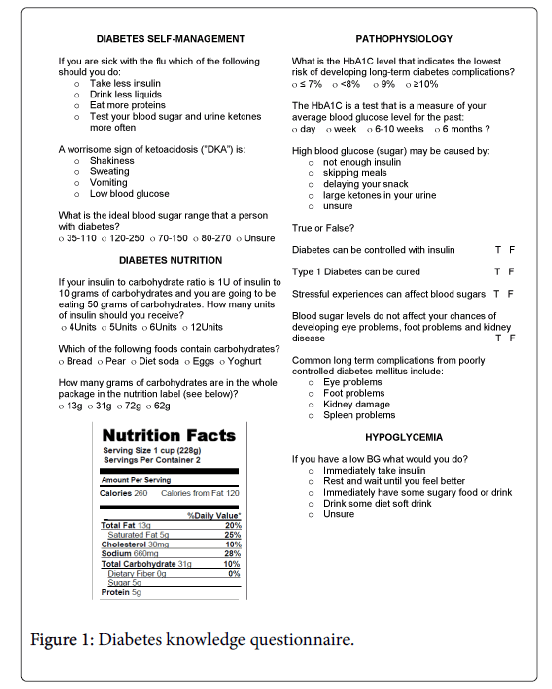
To determine patients’ diabetes knowledge, we developed a questionnaire assessing four different areas: pathophysiology, diabetes self-care, hypoglycemia and nutrition/carbohydrate counting. We utilized questions from several previously validated instruments (Figure 1) [10-13].
Demographic, socioeconomic, and clinical data were collected by self-report through a survey. Clinical data on A1C was retrieved from the electronic medical records: Pediatric Endocrinology Dynamic Record Organizer (PEDRO) (Pedrosoft LLC, Basking Ridge, NJ, USA) or Computer Information System (CIS) (Cerner).
Outcome measures
Diabetes knowledge surveys were scored as the percentage of correct responses. Subjects were categorized as having adequate diabetes knowledge if scores were ≥80% correct (B or greater in the conventional US grading system). Scores are reported as the percent (%) of respondents who achieved adequate diabetes knowledge. This was done for the overall survey as well as for each of the four subscales. We collected demographic, socioeconomic factors: age, gender, race, type of medical insurance (public vs. private), primary language spoken in the household, and marital status of the parents/caregivers. Clinical data included: time since diagnosis (categorized as ≤ 1 year, 2-5 years or 6+ years), type of insulin therapy (multiple daily injections vs. pump insulin therapy), A1C at visit (dichotomized ≤ 9% and >9% (75 mmol/mol), number of clinic visit in the last year, any occurrence of a diabetes related hospitalizations or emergency department visits in the last year or any admissions for diabetes ketoacidosis since diagnosis.
We have chosen an A1C over 9% (75 mmol/mol) as a cutoff for poor diabetes control based on the average A1C in our clinic (~8.8%). This is in-line with previous studies that reported A1C much higher than 7.5% (recommended by ADA) [3] in the majority of children with T1DM, and A1C over 9.5% in ~ 17% of children with T1DM [2]. This higher A1C cutoff was also driven by our overarching study goal to guide development of a diabetes education program that improves clinical outcomes in the most challenging group.
Data analysis
The secondary exploratory analysis evaluated predictors of diabetes knowledge among adolescents or caregivers. In general, continuous variables are represented as means and standard deviations (SD) while categorical variables are represented as frequencies and percentages. The overall and sub-scale percentage correct scores are reported along with 95% confidence intervals (CI). The prevalence of adequate diabetes knowledge was calculated using logistic regression. Results are presented graphically along with 95% confidence intervals. Exploratory hypothesis testing was conducted assessing the within group (e.g within-adolescent and within-caregiver) differences between demographics, socio-economic and clinical factors. Statistical significance was set at an alpha of 0.05; however, this was used only as a guide to evaluate meaningful clinical differences. Analysis was conducted using Stata v14.0 (StataCorp, LP College Station, TX). This study was approved and overseen by Baystate Medical Center’s institutional review board.
Results
Characteristics of the study group
A total of 215 subjects completed the 22-item diabetes knowledge questionnaire as well as demographic and clinical surveys (Table 1). Over half of them were adolescent respondents.
| Adolescent Respondents | Caregiver Respondents | |
|---|---|---|
| n=124 (57.7%) | n=91 (42.3%) | |
| Demographics | ||
| Age: mean (sd) | 17.1 (2.0) | 10.5 (2.5) |
| Caucasian race: n (%) | 90 (72.6) | 74 (81.3) |
| Male gender: n (%) | 71 (57.3) | 43 (47.3) |
| English as primary language: n (%) | 110 (88.7) | 85 (93.4) |
| Public insurance: n (%) | 31 (25.0) | 23 (25.3) |
| High school education or less: n (%) | 34 (27.4) | 20 (22.0) |
| missing | 3 (2.4) | 2 (2.2) |
| Married parents: n (%) | 77 (62.1) | 69 (75.8) |
| missing | 2 (1.6) | 1 (1.1) |
| Clinical characteristics | ||
| Years since diagnosis: mean (sd) | 7.7 (4.3) | 3.8 (2.8) |
| A1C: mean (sd) | 8.1 (1.6) | 8.0 (1.4) |
| A1C >9: n (%) | 27 (21.8) | 22 (24.2) |
| Insulin pump: n (%) | 79 (63.7) | 70 (76.9) |
| Visits in past year: n (%) 1 to 3 | 40 (32.3) | 13 (14.3) |
| 4 | 51 (41.1) | 39 (42.9) |
| 5 to 6 | 33 (26.6) | 39 (42.9) |
| Hospitalized in past year: n (%) | 7 (5.7) | 7 (7.7) |
| missing | 0 | 1 (1.1) |
| DKA admissions since diagnosis: n (%) | 16 (12.9) | 12 (13.2) |
| missing | 2 (1.6) | 3 (3.3) |
| Diabetes related ED visits in past year: n (%) | 7 (5.7) | 4 (4.4) |
| missing | 1 (0.8) | 1 (1.1) |
Table 1: Characteristics of the study group.
The majority of subjects were white (73% of adolescents, and 81% of caregivers), spoke English as their primary language (89% of adolescents, and 93% of caregivers), had married parents with at least a college education (73% of adolescents, and 78% of caregivers), and had private health insurance (75% for both adolescents and caregivers) (Table 1).
As expected, adolescents had a twice longer mean time since diagnosis (7.7 years) than children in the younger group (3.8 years). The mean A1C for adolescents was 8.1% (65 mmol/mol), and 8.0% (64 mmol/mol) for children under 14. About a quarter of patients from both groups had an A1C above 9% (75 mmol/mol). About two thirds of adolescents and nearly three quarters of caregivers of younger children reported using insulin pumps. Families with small children were more likely to adhere to ADA recommendation [3] of quarterly clinic visits. Only 13% of them reported less than 4 visits in the last year compared with 40% in the adolescent group.
Diabetes knowledge was generally good, with average scores of 86% and 84% correct responses among adolescents and caregivers, respectively. In the hypoglycemia category, adolescents scored an average of 98%, and caregivers scored an average of 96%. For questions related to nutrition/carbohydrate counting, both groups answered 83% of questions correctly. For pathophysiology the averages scores were 86% and 84% for adolescents and caregivers; and for self-care related questions the average scores were 87% and 84% for adolescents and caregivers. For the purpose of our analysis, a score of 80% or higher on our diabetes knowledge questionnaire (overall and for each specific knowledge category) was considered an acceptable level of knowledge. Scores are reported in (Figures 1-3) as the percent (%) of respondents who achieved adequate diabetes knowledge. No significant differences in diabetes knowledge were observed based on gender or patient age.
Diabetes knowledge and glycemic control
Overall, better glycemic control, defined as A1C below 9% (75 mmol/mol), was associated with higher total percent of adequate knowledge on our questionnaire (Figure 2). Adolescents with an A1C below 9% (75 mmol/mol) had adequate diabetes knowledge that was19 percentage points higher than those with an A1C above 9% (75 mmol/ mol) (p=0.030). Parents’ whose children had an A1C below 9% (75 mmol/mol) had adequate diabetes knowledge that was 28 percentage points higher on the diabetes knowledge questionnaire (p=0.017).
A similar trend was observed among caregivers, but not adolescents, with regards to the nutrition/carb counting questions, where only higher probability of adequate nutrition for parents (caregivers) were associated with lower A1C. For questions related to pathophysiology, higher probability of adequate knowledge for both parents and adolescents were associated with lower A1C. No significant differences were observed for the hypoglycemia and self-care subscales with respect to patients’ most recent A1C.
Children in both groups had low rates of hospitalization and diabetes related ED visits for acute complications of diabetes: hypo/ hyperglycemia within the past year and ketoacidosis (DKA) since diagnosis (Table 1). Only 13% of all subjects were ever admitted for a DKA (including admission on T1DM diagnosis). Due to the rarity of these events, associations and confidence intervals were very unstable, making it difficult to draw any conclusions, and therefore these values are not reported.
Diabetes knowledge and socioeconomic factors
Lower levels of parent education, and public health insurance were associated with lower probability of adequate diabetes knowledge. The rate of adequate knowledge was 29% lower in adolescents (whose caregivers had a high-school education or less) and 17% lower in caregivers with a high-school education or less, compared to those with at least a college education (p=0.001 and p=0.141, respectively) (Figure 3). Publicly insured adolescents and caregivers had a 44% and 20% lower rate of adequate scores respectively compared those who were privately insured (p<0.001 and p=0.072, respectively) (Figure 3).
Additionally, for both adolescent and caregiver respondents, strong differences in DK were observed between white and non-white subjects (p<0.001 for both groups). Patients’ race was associated with a 35% difference in overall adequate diabetes knowledge score for adolescent group, and a 44% difference in adequate diabetes knowledge score for caregivers (Non-whites had lower scores).
Diabetes knowledge and duration since diagnosis
Overall adequate diabetes knowledge was not significantly associated with the time since diagnosis in either adolescents or caregivers. Only self-care probability of adequate knowledge in the adolescent group was higher with the longer duration since diagnosis (p=0.004) (Figure 4). Although we did not find any other significant associations, we observed several suggestive trends. Among caregivers, self-care probability of adequate knowledge rose with greater time since diagnosis (similar to adolescents) (p=0.21). While adolescent probability of adequate nutrition knowledge showed a tendency to decline in relation to the duration since diagnosis (p=0.24), caregivers’ probability of adequate knowledge rose the longer their child had been diagnosed (p=0.33). Pathophysiology probability of adequate knowledge trended up for adolescents the longer they had been diagnosed (p=0.26) and although no clear trend was observed, caregivers adequate pathophysiology knowledge worsened over time.
Discussion
Using a combination of questions compiled and adapted from previously validated questionnaires, this study sought to evaluate diabetes knowledge in youth with T1DM and their caregivers. In this study we examined associations between diabetes knowledge and patients’ clinical outcomes, demographic and socioeconomic characteristics. Our results provide detailed estimates of various aspects of diabetes knowledge and skill areas. While it was generally reassuring that, on average, the patients in our study scored 83% or better on all sub-categories of our questionnaire, the breakdown of our results into specific associations with patients’ recent A1C, and demographic and socioeconomic status can help to inform diabetes educators as they continue to develop diabetes program curricula to better serve patients with T1DM.
Our study found a significant relationship between diabetes knowledge in adolescents and caregivers of younger children, and patients’ most recent A1C. This finding is in agreement with the findings of Beck et al. [8], but differs from the findings of Santos et al. [7], who saw no such relationship. More specifically, our results show that knowledge of pathophysiology in both groups and nutrition/ carbohydrate counting in parents if younger children individually associated with current glycemic control. The reason our results differ from those of Santos et al. [7] is most likely because we considered an A1C < 9% (75 mmol/mol) as our criterion dividing line, whereas they chose A1Cs < 7.5% (58 mmol/mol) as their cutoff. Our sample was also larger resulting in additional power.
Though knowledge of hypoglycemia was not significantly associated with patents’ most recent A1C, not surprisingly, both adolescents and caregivers performed better on hypoglycemia than any of the other question categories. On the one hand, hypoglycemia is a scary acute complication of diabetes and early appreciation and management of this serious problem could be lifesaving. On the other hand, excessive fear of hypoglycemia could lead to decreasing insulin doses and higher glucose levels and A1C. A notable limitation was that this knowledge area was covered by only one question. Diabetes knowledge scores in the other three categories that we analyzed, nutrition/carb counting, pathophysiology, and self-care, were all similar for both adolescents and caregivers.
A strong association was observed between adequate knowledge of the pathophysiology of type 1 diabetes and recent A1C values for both adolescent patients and caregivers. It is logical that patients who are able to understand the physiological basis for T1DM are also more likely to better treat themselves and achieve better glycemic control. On the other hand this may seem odd given indirectness of the link between the knowledge of pathophysiology of type 1 diabetes and A1C compared to more specific topics, such as, treatment of hypoglycemia, nutrition, or diabetes self-care. This contradiction may point to a number of confounding factors, such as, socioeconomics, or education that impact both ability to understand complex pathophysiological concepts and diabetes control.
Considering the differences between groups, it was surprising that we did not find any relationship between patient or caregiver knowledge of pathophysiology and the duration since diagnosis (Figure 3). Four out of five questions in the pathophysiology area were devoted to long-term diabetes complications. Adolescents in our study had been diagnosed with T1DM on average twice as long as children whose caregivers responded to our questionnaire, and therefore were likely more exposed to education on the consequences of uncontrolled diabetes.
The nutrition and carbohydrate counting section of our questionnaire dealt with assessment of the carbohydrate content of foods: reading nutritional value labels, and simple math skills. In our practice “number concepts” are the hardest in diabetes education, but are essential to patients’ ability to manage their diabetes. In light of this, it was not surprising to see that adolescents’ knowledge of nutrition and carbohydrate counting was not associated with A1C in the adolescent group (Figure 2). In our practice, adolescents are much more likely to “guesstimate” the amount of bolus insulin based on their experience. On the other hand, caregivers’ knowledge of nutrition and carbohydrate counting was strongly associated with patient A1C (Figure 2). As parents of younger children are usually responsible for care including carbohydrate counting and insulin administration, it seems logical that their knowledge of this area directly impacts glycemic control. These results emphasize the importance of educating parents and caregivers about appropriate dietary considerations in any effort to improve patients’ glycemic control. This is not to say that less attention should be given to educating adolescents about healthy nutrition, but our results suggest that, for adolescents, other factors than knowledge of nutrition may play a stronger role in diabetes control. Alternative and more concrete recommendations on insulin meal coverage might be beneficial. For example, in our practice, when carbohydrate counting failure is recognized, we occasionally propose fixed insulin doses for meals depending on its size (small, medium, large).
Our results regarding the associations between adequate diabetes knowledge and demographic markers such as race, public versus private insurance, and parents’ highest level of education are all in accordance with well established relationships between socioeconomic factors and patient health [14]. Lower socioeconomic status, as indicated by public health insurance, level of education, and primary language was significantly associated across the board with lower adequate diabetes knowledge for adolescents. It was also observed that non-white patients’ demonstrated lower adequate diabetes knowledge than their white counterparts. Importantly, adolescent patients’ adequate diabetes knowledge appears to be more severely affected by socioeconomic factors than parents’ and caregivers’. Many other studies have also found that poor glycemic control is associated with lower socioeconomic status [14-16]. Our results suggest that diabetes knowledge may play a role in impacting this disparity. Particular attention then should be given to helping teach adolescents from disadvantaged backgrounds about proper dietary and self-care practices; and education programs should be developed with special emphasis on using a curriculum that serves these patients.
Moreover, our results regarding the relationships between race and socioeconomic status and adequate diabetes knowledge serve to reemphasize the significance of considering the treatment of chronic health conditions like T1DM not merely as medical problems, but also as larger social issues. It is important that health care providers realize the inherent inadequacy of their treatment of patients, and that healthcare outcomes are influenced significantly by factors beyond their immediate control. In light of this, our research serves not only to stress the importance of improving diabetes education curricula in an effort to improve the health of patients, it also serves as a stark reminder that social and economic disparities deserve equal, if not greater attention from the public and medical communities if patients’ lives are going to be significantly improved.
Although our knowledge survey was based on prior validated surveys, this version was not validated among adolescents or caregivers. However, we feel that the questions represent real life experiences that patients and caregivers should be able to understand and answer. Regardless, it is possible that some subjects were misclassified in regards to adequate knowledge. This may be especially true in regards to the sub-scales (particularly hypoglycemia which is only one question). However, we would not expect this to differ by any other characteristics suggesting that this misclassification would be non-differential and therefore would only bias the results towards a null finding. Given this, true differences may be larger than those observed.
One of the largest issues with this study is the temporality of associations. In particular, our assessment of time since diagnosis and adequate knowledge gives the impression that change in knowledge was observed over time when in fact these are just snapshots at a given point in time. To better assess this association, we would need to follow patients and caregivers over time starting at their diagnosis. The associations we observed, although intuitive, may be influenced by other confounding factors as well as sample size at each interval. In addition, our observation that A1C’s >9% are associated with lower diabetes knowledge implies that the less a patient knows about their disease, the higher their A1C. However, it may be that the converse is true: the higher the patient’s A1C the lower their score on the test. This could be due to either anxiety over high A1C’s (especially caregivers worried about children) or decreased cognitive functioning [17].
Conclusion
Finally, our patient population was largely Caucasian with private insurance and a college education; therefore, generalizing our findings to patient populations with largely different demographic characteristics may be limited.
Recommendations
Given positive association between the diabetes knowledge and diabetes control, and no overall increase in knowledge scores with time since diagnosis we recommend strengthening of diabetes review programs in particular addressing pathophysiology, nutrition and carbohydrate counting. The latter skill might have a bigger clinical impact in families with pre-adolescent children. Diabetes education curricula should be individualized with emphasis on individual patient’s socioeconomic challenges and knowledge gaps.
Acknowledgement
We would like to thank the diabetes educators of the Baystate Pediatric Diabetes Program: Kathy Dunn, RN, CDE, Lynn Henry, RD, CDE, and Lori Nowak RN for providing diabetes education and caring for study patients.
References
- Stanescu DE, Lord K, Lipman TH (2012) The epidemiology of type 1 diabetes in children. Endocrinol Metab Clin North Am 41: 679-694.
- Petitti DB, Klingensmith GJ, Bell RA, Andrews JS, Dabelea D, et al. (2009) Glycemic control in youth with diabetes: The Search for diabetes in Youth Study. J pediatr 155: 668-672.
- Diabetes care (2016) Standards of medical care in diabetes-2016. J Clin Appl Res Edu 1: S4-5.
- Hood KK, Peterson CM, Rohan JM, Drotar D (2009) Association between adherence and glycemic control in pediatric type 1 diabetes: A meta-analysis. Pediatrics 124: e1171-1179.
- Heisler M, Piette JD, Spencer M, Kieffer E, Vijan S (2005) The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care 28: 816-822.
- Stark Casagrande S, Rios Burrows N, Geiss LS, Bainbridge KE, Fradkin JE, et al. (2012) Diabetes knowledge and its relationship with achieving treatment recommendations in a national sample of people with type 2 diabetes. Diabetes Care 35: 1556-1565.
- Santos FR, Bernardo V, Gabbay MA, Dib SA, Sigulem D (2013) The impact of knowledge about diabetes, resilience and depression on glycemic control: A cross-sectional study among adolescents and young adults with type 1 diabetes. Diabetol Metab Syndr 5: 55.
- Beck JK, Zhang Y, Shay CM, Muhamedagic CA, Sternlof SA, et al. (2015) Diabetes knowledge in young adults: Associations with hemoglobin A1C. Fam Syst Health 33: 28-35.
- Chase HP (2006) Understanding diabetes (11th edn). Barbara Davis Center for Childhood Diabetes.
- Speight J, Bradley C (2001) The ADKnowl: Identifying knowledge deficits in diabetes care. Diabet Med 18: 626-633.
- Koontz MB, Cuttler L, Palmert MR, O'Riordan M, Borawski EA, et al. (2010) Development and validation of a questionnaire to assess carbohydrate and insulin-dosing knowledge in youth with type 1 diabetes. Diabetes Care 33: 457-462.
- Fitzgerald JT, Funnell MM, Hess GE, Barr PA, Anderson RM, et al. (1998) The reliability and validity of a brief diabetes knowledge test. Diabetes Care 21: 706-710.
- Eigenmann CST, Colagiuri R (2011) Development and validation of a diabetes knowledge questionnaire. Practical Diabetes Int 28: 166-170.
- Macias ARG, Macias SR, Kaufman E, Skipper B, Kalishman N (2003) Relationship between glycemic control, ethnicity and socioeconomic status in Hispanic and white non-Hispanic youths with type 1 diabetes mellitus. Pediatr Diabetes 4: 19-23.
- Coulon SJ, Velasco-Gonzalez C, Scribner R, Park CL, Gomez R, et al. (2016) Racial differences in neighborhood disadvantage, inflammation and metabolic control in black and white pediatric type 1 diabetes patients. Pediatr Diabetes 18: 120-127.
- Hassan K, Loar R, Anderson BJ, Heptulla RA (2006) The role of socioeconomic status, depression, quality of life, and glycemic control in type 1 diabetes mellitus. J Pediatr 149: 526-531.
- Cox DJ, Kovatchev BP, Gonder-Frederick LA, Summers KH, McCall A, et al. (2005) Relationships between hyperglycemia and cognitive performance among adults with type 1 and type 2 diabetes. Diabetes Care 28: 71-77.
Citation: Moskovitz A, Alex Knee MS, Frydman E, Allen H, Tonyushkina K (2018) Diabetes Knowledge in Youth with T1DM and their Caregivers-A Cross-Sectional Study. J Diabetes Clin Prac 1: 101.
Copyright: © 2018 Moskovitz A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3588
- [From(publication date): 0-2018 - Dec 22, 2024]
- Breakdown by view type
- HTML page views: 2869
- PDF downloads: 719