Review Article Open Access
Development Costs of Inaugurating a Physician Assistant Program
Yealy J and Hooker RS*
Biomedical Campus, Health Policy Northern Arizona University, USA
- *Corresponding Author:
- Roderick S. Hooker
Adjunct Professor, Biomedical Campus, Health Policy Northern Arizona University
Phoenix, AZ 85004, USA
E-mail: rodhooker@msn.com
Received date: July 04, 2016; Accepted date: July 26, 2016; Published date: July 29, 2016
Citation: Yealy J, Hooker RS (2016) Development Costs of Inaugurating a Physician Assistant Program. J Community Med Health Educ 6:454. doi:10.4172/2161-0711.1000454
Copyright: © 2016 Yealy J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
To understand the process of developing a new physician assistant program in the US a 10-year prospective study was undertaken. Critical pathway protocol included a daily log of activity. Expenditures, revenues, and budgets were adjusted to 2015 dollars. The study begins in year one with the Chancellor of the University advocating a program, followed by approvals from the Board of Trustees and Faculty Senate. Next the dean formed a search committee; department chair, program director, key faculty, and staff were hired. The first 10 years of operation was $10.5 M and the break-even point occurred in year 8 based on tuition revenue of $8.4 M. Remodeling classrooms, a laboratory, patient examination simulation spaces were significant expenses. Unanticipated events delayed implementation resulting in cost over runs but in retrospect many could have been avoided. In the end The University of Tennessee’s Physician Assistant program’s opportunity cost for a student was $1200 per month. In summary, the development of a PA program was more complex, lengthy, and costly than predicted by consultants. Critical pathway analysis identified many interconnecting nodes that interfered with the process but with improved modeling could avoid or mitigate them. Comparison of development cost of other types of PA programs is needed research.
Keywords
PA education; Opportunity costs
Introduction
As of 2016 the physician assistant had been a concept for five decades and the profession was in more than a dozen countries. During that first half-century, over 200 PA programs were developed and at least 20 programs closed [1]. In the same year the US Accreditation and Review Commission for Physician Assistant Education (ARC PA) estimated that if new applications to inaugurate a PA program continues the number may exceed 250 by mid-2020 (http://www.arc-pa.org). The characteristics of existing programs spans the diversity of higher education including biomedical universities, community colleges, academic health centers (AHC), and small private colleges [2]. In the UK at least 26 programs are expected to be operational by 2017. PA activity and development is occurring in a dozen countries [3]. However, no template exists about how programs should be developed and modeled.
Globally, within various settings, there exists a diversity of hierarchical and organizational means of administrating a program [4]. In spite of the range of institutional structures and programs, all began with an idea or a dream. From a concept to the commencement of the first class, somehow the idea gets nurtured. During this process advocates are involved, university committees are created, oversight boards informed, money allocated, and personnel hired. The stepwise process seems writ large but to date no details in the public domain inform this process. Furthermore, without documentation the whole process appears highly dependent on personal opinions about who should do it, where it should reside, and how it should happen. Many times a consultant in PA education is contracted to lend their personal opinions and experience. Yet, in spite of this growing activity a blueprint for this process is missing in the literature.
Costs to inaugurate a physician assistant program
What are the costs associated with starting and sustaining a PA program in its formative years? This question is at the heart of education economics and human investment as it can be applied to almost any graduate school. Education institutions are capital ventures — investing today for a financial return tomorrow. Typically in European countries most education expenditure takes the form of government consumption with a small cost borne by individuals. In North America with their state and provincial supported systems, many are considered investments in human capital with a benefit returning to the state/providence in the form of more providers per capita to maintain health in a population - rather than the depletion of resources. In proprietary institutions, they are a significant investment of principal. As financial ventures, the rate of return is largely in tuition dollars and other fees. This return may be contingent on a break-even point with new revenue generated for other projects. For more socialized governments the cost is borne in the return by sustaining or growing a provider cadre to manage the needs of society. Some return is also generated in the production of more graduates with income that is taxed at a higher level of earnings.
The cost to start a PA program is a major expense in personnel regardless of institution and shares many characteristics with physical capital. Because the demand for education is investment in the acquisition of skills and knowledge, benefits are stretched out in longer terms. Costs are not easy to calculate because the analysis includes a number of variables, indirect expenses, and in-kind support by the institution, along with a number of unknowns. However, some of the variables that have emerged of importance and should be considered are in the following table (Table 1).
| University/ College Classification |
Medical College Health Science Based Institution Academic Health Center Liberal Arts College |
Administrative support Support from other departments |
|---|---|---|
| Type of Institution |
Public | Private - fewer rules/policies- but hard to fund |
| Private | internally | |
| Proprietary | Public (primary land grant universities) - more | |
| Religious | layers of administration, policies and | |
| accountability, but may be eligible for state or | ||
| provincial funds | ||
| Proprietary - may be a start-up by investors solely | ||
| as an investment | ||
| Religious/Denomination based - may include | ||
| additional protocols and criteria for development | ||
| Infrastructure | Classroom/Office Space | Pre-existing - scheduling issues |
| Cadaver/Learning/ | Pre-existing - pro-rate if shared | |
| Simulation Labs | Renovation vs. new construction | |
| Medical Library | Medical librarian available | |
| Pro-rate cost of medical reference materials | ||
| Labor | Faculty | Availability |
| Staff | Experience | |
| Salary/Benefits | ||
| Tenure/Non-Tenure Positions | ||
| Clinical Education |
Clinical Sites Preceptors |
Student per diem cost for |
| transportation/meals/housing | ||
| Regionally - are clinical sites being reimbursed? | ||
| Other PA Programs |
Density of programs in the region |
Faculty availability |
| Clinical site availability | ||
| Student applicants |
Table 1: Institutional variables affecting the development of a PA program.
Given that PA program growth is underway in many countries, an opportunity presented itself to document what the process was and how long it took – from the beginning. An assessment of the development costs of a PA program from the earliest stages to graduating a class of students is needed if educational efficiency strategies
were undertaken. The intent, from a financial investment viewpoint, was to chronicle the events of activity. Along the way critical pathways were identified and determined whether these were influencers of important developmental events.
The objective of this research project was a case study regarding how a PA program was created from the bottom up and top down as well as the resources used to follow an inaugural class through the full process. The long-term outcome of this endeavor is to use these experiences to construct new educational models more effectively and efficiently. A study of this educational activity sets the stage for more comprehensive analysis of how PA programs can be developed.
Research questions
• What are the costs associated with starting and sustaining a PA program in its formative years?
• What is the succession of events required to inaugurate a PA program and see its first class graduate?
• Can the university recoup its investment in PA program development through tuition?
Method
The approach to this investigation drew on the tools of accounting, financing and economics. A critical pathway analysis served as the timeline of the project. Its utility was to dissect the information involved with the whole project and identify critical junctions or bottlenecks of project flow. An activity log documented events from the beginning of the project through the fifth year (and beyond) and was analyzed for critical events.
Timeline
A timeline of events spanning five years was created. Internal and external documents and records surrounding the concept of a PA program in this university were obtained periodically and archived. A log of institutional and program activity from the time of the employment of the program director, through the ARC PA accreditation process, to the time of the first class graduation was maintained by the authors and shared on a common server. The university offices of the dean, chancellor, and vice president of finance supplied historical documents.
Costs of PA program activity
The timeline was assessed as to event and cost. Costs were both direct and indirect with future operating costs estimated through linear regression techniques. All costs were adjusted to 2015 dollars using the consumer price index for years 2011 through 2015. No interest on the principal or in revenue was incurred but annual inflation was projected through 2020.
Economic event analysis
The financial picture used economic event analysis methodology [5]. Event log software assisted in the graphical display of events and the value assigned to each event. The financial assumptions were that operating expenses would be offset by tuition revenue. Operating expenses include the renovation cost of rehabilitating an existing university building to code and make way for classrooms that can accommodate two matriculating classes, 6.5 FTE faculty, and three 3.0 FTE staff. Additionally a laboratory and clinical rooms for patient simulation was part of the renovation. Hardware and software, along with special projections, were part of the encountered costs. No renovation expenses occurred beyond 2014. Substantial unanticipated operating costs occurred as a result of unexpected key faculty turnover. Tuition revenue projections were made based on an initial class size of 36 with an increase to 50 over a five-year time period. However, the ARC-PA released updated guidelines during the development years that required a program to have an accreditation status of continued operation and data accumulation for five consecutive years before requesting an increase in class size. The ARC-PA provisional program application was approved for a class size of 30, down from the requested 36. Therefore, the projected tuition revenues were adversely affected.
Critical pathway model
A critical pathway model (CPM) was constructed from records, interviews, calendars, and project logs throughout the project. This CPM identified critical events at decision point nodes. The CPM calculated the longest path of planned activities to the end of the project, and the earliest and latest that each activity could start and finish. In retrospect certain activities were identified as "critical" (i.e., without which the project cannot go forward)
Study site
The location is the University of Tennessee Health Science Center (UTHSC) in Memphis, an academic health center (AHC) with a medical school, nursing school, health professions school, and teaching hospitals. The PA program is a department in the College of Health Professions and grants a graduate degree in 24 months. The full complement of faculty was 6.5 and 5 were on a tenure track. The medical director was a 0.2 FTE allocation from the Department of Family Medicine. All faculty members held graduate degrees and five were PAs. There were three office staff members: a manager and two administrative personnel. The faculty and the medical director reported to the program director (PD) who had a dual appointment as the department chair. The PD/Chair reported to the Dean of the College of Health Professions.
The class of 2015 was comprised of 25 students (adjusted down from a proposed 36). More than 800 applications were received each year and over 100 applicants were interviewed. Each class started early January and completed the education cycle in December the following year (24 months). Because the projected enrollment for the first 5 years of the PA Program was set for 30 students per class but had to be readjusted for a class of 25 the projected breakeven point in the budget had to be readjusted. The UTHSC Institutional Review Board approved this project in June 2013.
Results
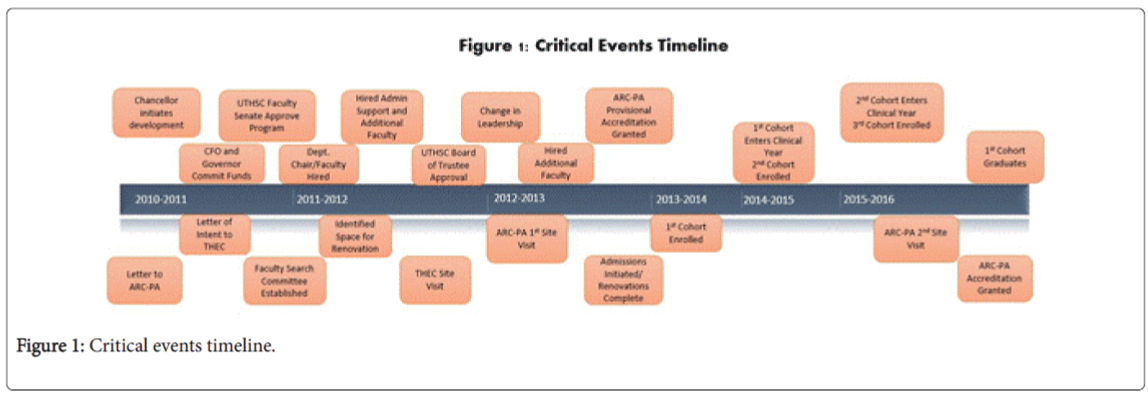
The project spanned five years and the observation period concluded with commencement of the first class in December 2015. The timeline of critical events is summarized in Figure 1.
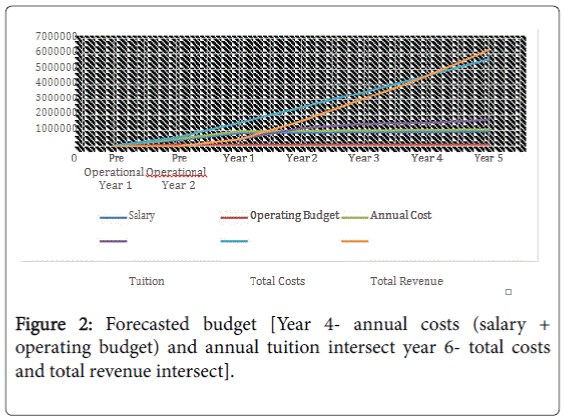
The forecasted budget showing projected revenues and expenses as presented to the university and Board of Regents early in development is included as Figure 2. Initially, the program projected a break-even point for tuition revenue to exceed expenses in year 2 (2013-2014); however, costs related to the remodel of physical space and preparation for faculty as well as accreditation costs were not included in the timeframe. The total opportunity cost break-even point is defined as the period when total allocations would equal total tuition revenue. This break-even point, as presented to the Board of Regents, was at year 5 (2016-2017) with a total investment of 5.67 M and total revenues of 6.29 M.
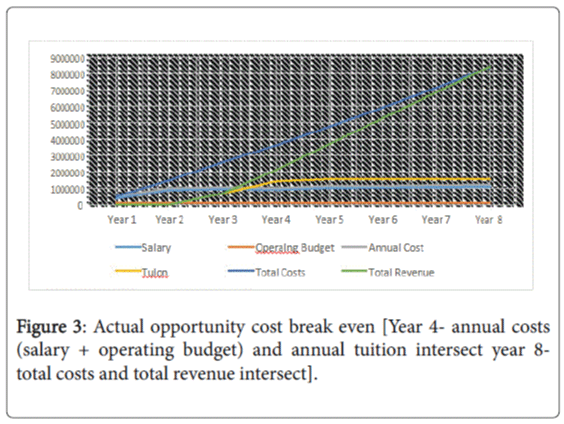
To represent true opportunity costs, the pre-operational years in the actual budget starts with year 1 representing the first year that costs were incurred for program planning and recruitment. In this case, the actual break-even point for annual costs equal to tuition revenue did not occur until year 4 (2015-2016) as seen in Figure 3.
This break-even point was projected to occur at year 5 (2016-2017); however, the amended projections show that it will not occur until year 8 (2019-2020) with a total investment of 8.39 M over the same period. The investment estimates included the funding of the pre-operational year’s faculty and staff, funding an operating budget, and collecting revenue through tuition. No external grants were received. The operating budget (primarily overhead), personnel expenses, along with tuition revenue was created through a regression of expenses for five classes out to 2020. All expenses were held constant in 2015 dollars and those before 2015 were adjusted to 2015 using annual CPI.
The 8 years of operation, beginning with The Chancellor putting forth the idea of a PA program in 2011 to the graduation of 5 classes of PAs by 2020, costs $8.38 M (2015 dollars). In year 8 there is a breakeven of the investment with revenue offsetting operation expenses. The projections show that only by year 8 did revenue exceed operating expenses, ceteris peribus. However, costs related to physical operation of the building space such as electricity, heat, security, parking, etc. were not factored into the financial analysis. These costs were budgeted at $750,000 but exceeded 1.1 M. Costs incurred related to faculty turnover were close to $300,000 but were not included in the analysis.
During the first 5 years of operation, there were approximately 2-3 meetings per week of three or more university personnel that often involved other actors. These meeting were indirect expenses in time, labor, and personnel that are recorded activities necessary for keeping the project on track. The activity log did not account for routine phone calls, emails, or interviews of faculty and applicants. Three sets of consultants were contracted along the way (feasibility study, operational consulting, and mock site visit preparation). The turnover of faculty and staff were unexpected expenses that increased the operating cost of the enterprise.
The cost of educating one student for 12 months was calculated by dividing the total budget annually by the number of matriculates using all resources in 2015. This results in an estimated $1,197 per student per month. Operating expenses were offset by tuition revenue of $1,709 revenue per student per month (2015 dollars). Budget expenses were projected to grow 3% per annum along with tuition increases.
Discussion
A 10 year commitment to starting and seeing through a PA education program is not a trivial undertaking in this century, at least in a public institution in America. In this case study there were many participants involved, unexpected setbacks, and unexpected expenses. In general, based on this analysis of a land grant school in the eastern part of America, it costs about $8.38 M to see it through for 8 years with offsetting revenue delays throughout most of the timeline. Only in the eighth year is there adequate revenue to obtain a return on the initial expenses and balance the outgoing expenditures to date. Had renovation and faculty turnover costs been included in the analysis, the break-even would have been at year 10 with a 10 M investment. This opportunity cost break even point for this particular institution could have been shifted if the planned class size (50 students) had been realized, the length of program extended (30-36 months) and/or the original faculty retained.
Critical event analysis suggests the main spark that set the process in motion was when the new chancellor arrived from Duke University in 2010 and championed the project in 2011. This advocacy appears to have set up a series of events that involved earmarking start-up funds, Board of Trustees meetings that eventually met approval, followed by faculty senate approval – all critical events that each could have curtailed the process. While this series of events seems inevitable, once advocacy by the chancellor was in place, there were some unexpected barriers to overcome. Initial resistance from the College of Nursing was intense and resulted in the resignation of the Dean of the College of Nursing.
Another critical factor was the Dean of the College of Health Professions. While she facilitated meetings, appointments, and some clinical sites within and outside the university, she was inexperienced working with PA education and leadership and was the principal involved in hiring and dismissing faculty and staff. The inaugural PA department chair/program director was replaced before the initial ARC-PA site visit and another one in place for the final site visit. This pattern repeated itself with an ultimate employment of 3 department chairs within the first three years of development. While the nature of personnel changes that occurred in 2014 and 2015 is beyond the scope of this study, they serve as important reminders that additional and unexpected expenses should be factored in any predictive model. One recommendation is to include a realistic sensitivity analysis in the budget that could accommodate cost overruns.
Multiple decisions during the development made by committees, rather than experienced PA directors, significantly altered the development costs. Anticipated dates of starting had to be altered due to circumstances. The program had an initial site visit in March 2012 that resulted in an ARC-PA accreditation decision in September; therefore, the earliest start date was the following spring. As a consequence six months of faculty and staff salary revenue was spent before a class was inducted. Tuition was set at a relatively low level when compared to peer organizations and the class size of 30 was small comparative to other AHC programs. The 24-month length of the program was a critical decision but could easily have been 36 months (a strategy that tends to increase tuition revenue without appreciable differences in certification rates).
The average operating budget reported by 182 established PA programs was $2,221,751 (2014 dollars) [2]. That number is subject to many variables because 80% of the reporting programs received direct support from their sponsoring institutions. However, the operating budget reported in this study suggests the UTHSC budget is well within the margins of a modern PA program.
The opportunity cost modeled in this scenario involves a PA program in an AHC, an institution consisting of a medical school, health profession schools or programs, and a teaching hospital or health system. While only a fourth of PA programs in the US are in AHCs, in other countries almost all are AHCs (realizing that non- American academic institutions may differ from American ones; on the other hand, the critical pathway and use of resources to develop a PA program may be similar). In theory PA programs are probably more similar than different in the way they invest in human capital.
Most of the new US PA programs will be in private (for profit) institutions [6]. Because this is an analysis that identified all of the resources used in the development project, each institution will need to assign their own costs to each of the required operating expenses. Profit margins will differ but outcomes are likely to be similar.
This PA education study is grounded in human capital theory - an aggregate economic view of people acting within economies. Human capital theory is an attempt to capture some aspect of the social, biological, cultural, and psychological complexity as they interact in explicit economic transactions. Many theories connect investment in human capital development to education. The role of human capital in economic development, productivity growth, and innovation has frequently been cited as a justification for government subsidies for education and job skills training. That this project was undertaken with public funds speaks to the belief that Tennessee is experiencing significant shortages in health professionals [7]. This was a study in human capital theory and how investment in producing functional graduates for the needs of a state was put forth.
Limitations
All studies have attributes and limitations. The attributes of this research are as the first study of its kind in the public literature that attempted to detail all aspects of development of a PA program and are prospective in nature. It is a case study, a form of qualitative and qualitative descriptive research that is used to look at individuals, a small group of participants or objects, or a group as a whole. From a case study of how a PA program is developed and its total costs, the next step is to gather additional observations of other sites to see how representative this surveillance was. The work was prospective, was five years in observation, and had full cooperation from the Chancellor, the VP for finance, the IRB, the Dean, the 2015 Department Chair, Program Director, and administrative staff.
The limitations are that one American university that is publically funded is not representative of the full collection of PA programs nationally, much less internationally. UTHSC is an AHC, which differs from the majority of American PA programs operationally or in development (although AHCs are largely the standard in Canadian, and European PA programs). Distilling all the details, complexities, data, and nuances of this project were beyond the limits of a research manuscript of this type but the fundamentals are laid out as a case study and available for replication. As in epidemiology, case studies serve as foundations for additional comparative work even when not considered representative of the full nature of other institutions. Another limitation is that projections have their own inherent problems that cannot account for all of the unexpected issues that may impact operations and revenue. Forecasting is based on simulations (e.g., trend analysis and best guess scenarios). Look-back analyses serve as determinants of predictive modeling and should be scored for accuracy by 2021.
The third limitation is that some clinical training sites at the opposite end of the state were subsidized and budgeted. Subsidizing for clinical sites was a fixed cost for this activity. However, for the most part physicians, nurses, and other health personnel employed in UTHSC clinics where the program was located typically work with health professional students. Other clinical training sites where students rotated were federal and state-supported community health centers, a pediatric teaching hospital, a regional burn center, and the Department of Veterans Affairs medical center and clinics. Normally these public institutions do not charge for mentoring health professions students. Competition for future sites may require more remuneration for student rotations and should be built into financial projections.
Conclusion
The result of the first prospective study how a PA program was inaugurated in a publically funded university over a 5 year period gives a representative picture of predicted and unpredicted resources used, costs incurred, and entangling events. The outcomes included timelines and a model that could be utilized by institutions as they plan for the future development of PA programs. Realistic budgets, costs, and personnel needs were documented in an unprecedented way and serve to guide administrations in critical event decision-making and how pitfalls can impact projections. Like all case studies, needed research lies in comparative analyses of other start-up programs and how they can manage expenses better.
References
- Cawley JF, Hooker RS (2013) Physician assistants in american medicine: At the half-century mark. Am J Manag Care 19: e333-e341.
- Physician Assistant Education Association (2015) Thirtieth annual report on physician assistant educational programs in the united states, 2013-2014. PAEA 30: 1-54.
- Hooker RS, Ballweg RM (2016) Celebrating 20 Years of the PA Profession in India. PA.
- Wright KA, Cawley JF, Hooker RS, Ahuja M (2009) Organizational infrastructure of american physician assistant education programs. J Physician Assist Educ 20: 15-21.
- MacKinlay AC (1997) Event studies in economics and finance.J Economic Literature 35: 13-39.
- Cawley JF, Jones PE (2013) Institutional sponsorship, student debt, and specialty choice in physician assistant education. J Physician Assist Educ 24: 4-8.
- DesRoches CM, Buerhaus P, Dittus RS, Donelan K (2015) Primary care workforce shortages and career recommendations from practicing clinicians Academic Medicine. J Assoc Am Med Colleges 90: 671-677.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 13300
- [From(publication date):
August-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 12462
- PDF downloads : 838