Research Article Open Access
Development and Testing of a Curriculum for Teaching Informed Consent for Spinal Anesthesia to Anesthesiology Residents
Pedro Tanaka1*, Leeanne Park1, Maria Tanaka1, Ankeet D Udani2 and Alex Macario1
1Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine, Stanford, USA
2Department of Anesthesiology, Duke University School of Medicine, Durham, USA
- *Corresponding Author:
- Pedro Tanaka
Department: Department of Anesthesiology, Perioperative and Pain Medicine
Stanford University School of Medicine, Stanford, USA
Tel: 650-724-4066
Fax: 650-724-4066
E-mail: ptanaka@stanford.edu
Received date: August 2, 2016; Accepted date: August 17, 2016; Published date: August 22, 2016
Citation: Tanaka P, Park L, Tanaka M, Udani DA, Macario A (2016) Development and Testing of a Curriculum for Teaching Informed Consent for Spinal Anesthesia to Anesthesiology Residents. J Pain Relief 5:259. doi:10.4172/2167-0846.1000259
Copyright: © 2016 Tanaka P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Abstract
Introduction: Properly obtaining informed consent for spinal anesthesia is a skill expected of anesthesiology residents. The goals of the study were to 1) use a Delphi method to develop a curriculum for teaching informed consent for spinal anesthesia, and a checklist of required elements; 2) determine which elements of the informed consent process were most frequently missed prior to the curriculum; 3) quantify if this curriculum improved performance of correctly obtaining informed consent from a standardized patient; and 4) measure retention of learning as measured by how residents performed on actual patients. Methods: Performance on obtaining informed consent was tested with an 11-item checklist on a standardized patient before and after completing the curriculum. Resident performance on their next three patients scheduled to have spinal anesthesia was evaluated at the bedside using the same checklist. Results: At baseline before completing the curriculum 18 anesthesia residents (39% female) with a mean 6.29 months (SD 3.59, median 6.5, 25th-75th quartile range 4.25-9.75) of residency completed and 11.39 prior spinals (SD 13.1, median 13.14, 25th-75th quartile range 3-14) successfully performed 47% (SD 20%, median 45%, 25th-75th quartile range 36-41%) of the 11 required elements. The 3 most commonly missed elements were: “Teach back: Ask the patient to repeat key items in discussion” (0% correct), “Connect, Introduce, Communicate, Ask permission, Respond, Exit” (6%), and “Have the patient verbally agree with the consent forms (17%).” 7 residents completed the written materials and video curriculum and significantly increased their performance to successfully complete 90% of the required elements on a standardized patient, and 86% on actual patients 1-5 days later (P<0.01). 11 other residents completed the written materials and video curriculum supplemented with a 1:1 session with a faculty and significantly increased the percentage of properly completed elements to 97% on the standardized patient, and to 88% on actual patients (P<0.01). Conclusions: The curriculum developed increased performance on how well informed consent was obtained by junior anesthesia residents on an 11 item checklist and may be used by training programs to teach and evaluate their residents.
Keywords
Informed consent; Spinal anesthesia
Abbreviations
ACGME - Accreditation Council for Graduate Medical Education.
Introduction
Properly obtaining informed consent from a patient prior to an anesthetic is a skill expected of anesthesia residents. Informed consent is specifically listed in the ACGME Anesthesiology Patient Care Competency, as a milestone within Preanesthetic Evaluation, Assessment, and Preparation. For patients and physicians the consent process is a tool for building trust and enhancing decision making [1]. When obtaining informed consent, anesthesiology trainees face ethical challenges (e.g., conflict between patient and family wishes and medical judgment) and patient relationship challenges (e.g., questions about trainee competence) [2]. Other challenges may be categorized as practical and include the amount of information to provide, communication barriers, and time limitations. Although a study of primary care physicians and surgeons showed that consent discussions are often incomplete [3], how well practicing anesthesiologists obtain consent is unknown. Inadequate communication due to incomplete informed consent may increase litigation risk [4].
Studies of methods to improve residents’ skills in obtaining informed consent exist. For example, 2.5 hr of training with faculty and standardized patients improved surgery residents ability to properly perform on an 8 item checklist from 6.85 to 7.40 items [5]. Direct feedback from standardized patients has also been found to be helpful to teach informed consent [6], as has an online module, a small group discussion with faculty, and standardized patient cases [7]. Training in medicine has relied on acquisition of knowledge and skills via an apprenticeship model utilizing real-world experience with actual patients. Among the limitations of this approach is variability in the types of supervision and feedback that trainees receive [8]. The optimal way to educate or assess anesthesia house staff on obtaining informed consent is unknown.
Simulation on the other hand allows for innovative ways to improve trainee skills in a controlled environment with the opportunity for repetition and accurate feedback [9]. Development of superior performance can be aided by having well-defined learning objectives, a focus on improving particular tasks via repetitive practice, and precise measurements of performance and timely informative feedback [10]. Technical procedures such as central line placement, lumbar puncture, and subarachnoid blocks may benefit from simulation training [11-13]. Less research is published on teaching nontechnical skills such as informed consent.
As a result, this study aimed to study informed consent with spinal anesthesia as the specific topic because it is a common anesthetic type. The goals of the study were to 1) use a Delphi method to develop a curriculum for teaching informed consent for spinal anesthesia, and a checklist of required elements; 2) determine which elements of the informed consent process were most frequently missed prior to the curriculum; 3) quantify if this curriculum improved performance of correctly obtaining informed consent from a standardized patient; and 4) measure retention of learning as measured by how residents performed on actual patients.
Methods
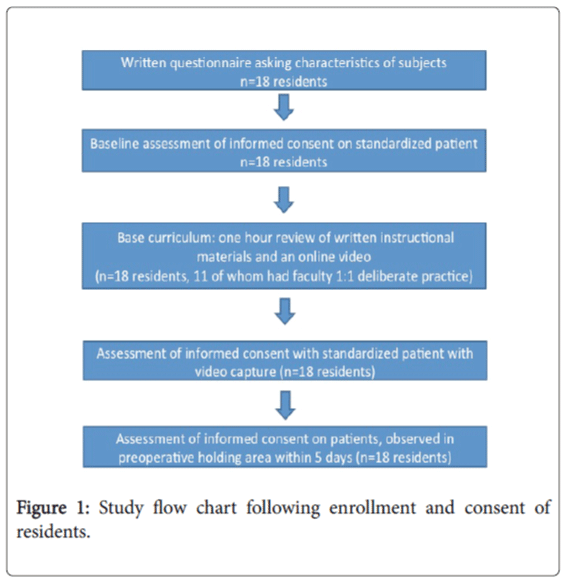
After IRB approval, anesthesiology postgraduate year two residents were recruited to participate in the study. Resident data were kept confidential and residents understood they would not be penalized for not participating in the study (Figure 1). outlines study protocol. Each resident completed a survey to collect demographic data, and answered a question on how comfortable they feel obtaining informed consent for spinal anesthesia (5-point ordinal scale).
Checklist development
A checklist of the necessary elements for obtaining informed consent for spinal anesthesia was derived via a modified Delphi approach [14] among a panel of experts of five board-certified anesthesiologists from four different teaching hospitals to determine the domains and specific items. This was supplemented by analysis of published articles. For example, a systematic review found that physicians rarely discuss alternatives, risks, and benefits when obtaining consent, and tend to overestimate patient’s comprehension of the information [15]. As a result, those items were discussed for inclusion in the checklist. During the Delphi process, suggestions for adding or deleting required elements of informed consent were encouraged, and the checklist assessment tool was reviewed iteratively by the panel until consensus was achieved.
The checklist was also then pilot-tested on a group of 3 attending anesthesiologists, and reviewed again, until consensus was reached to provide face and content validity. For all assessments each checklist element was graded by two trained faculty raters and given equal weight using a dichotomous scoring system (“satisfactory” or “unsatisfactory”) as recommended for performance tests [16].
Performance assessments
Performance assessment on a standardized patient before curriculum: A baseline assessment of each participant obtaining informed consent was made with a standardized patient before they were exposed to the curriculum. To ensure consistency, the standardized patient first read through the case, and trained and prepared using role-play. Appendix A contains the prompt given to the participant and the instructions for the standardized patient.
The video-recorded performances at baseline were later scored by two authors (AU, PT) using the 11-item checklist developed in the Delphi process.
Curriculum
After the baseline assessment, residents completed the curriculum consisting of one hour to review written instructional materials, including FAQs, as well as an online video a video with a standardized patient (https://m.youtube.com/watch?v=AN8CdzQj6xk) to demonstrate the desired optimal method for obtaining patient informed consent for spinal anesthesia. The curriculum specifically addressed each of the items on the checklist.
Based on an assumed baseline performance of 30% correct of the checklist items and an improvement to 80% correct after completing the curriculum, a power analysis determined that a sample of n=7 would detect this difference with alpha=0.05 and beta=0.8.
7 residents completed the written materials and video and 11 other residents completed the written materials and video curriculum supplemented with a 1:1 session with a faculty. Thereafter all residents underwent re-testing with the standardized patient. The session was video-recorded and scored using the checklist in the same fashion as the baseline assessment.
Performance assessment on actual patients for all residents
To evaluate retention and clinical application, all residents were observed at the bedside by one of the authors (AU, PT) obtaining informed consent for spinal anesthesia on the resident’s next three patients scheduled to have spinal anesthesia.
Their performances were scored live, not video-recorded, using the same 11-item checklist by the two faculty raters (AU, PT).
Statistics
The Wilcoxon signed-rank test paired samples non-parametric test was used to assess before and post curriculum performance scores on the 11 item checklist.
Results
The modified Delphi method resulted in an 11-item checklist of required elements for informed consent (Table 1).
| 1 | Introduce self and the discussion topic |
| 2 | Describe the indications for the procedure |
| 3 | Describe the benefits of the procedure |
| 4 | Describe the procedure itself in clear, simple language |
| 5 | Pause for questions appropriately |
| 6 | Describe the minor risks of the procedure |
| 7 | Describe the risk of serious complications. Emphasize that these are rare. |
| 8 | Describe alternatives to the procedure |
| 9 | Teach back: Ask the patient to repeat key items in discussion |
| 10 | Have the patient verbally agree with the consent form |
| 11 | Utilized Connect, Introduce, Communicate, Ask permission, Respond, Exit |
Table 1: Eleven item checklists for informed consent for spinal anesthesia as developed from them modified Delphi process.
All 18 (39% female) residents recruited consented, and at baseline before completing the curriculum had a mean 6.29 months (SD 3.59, median 6.5, 25th-75th quartile range 4.25-9.75) of residency completed and 11.39 prior spinals (SD 13.1, median 13, 14, 25th-75th quartile range 3-14) (Table 2).
| Mean | SD | Median | low to high range |
25th-75th quartile range |
|
|---|---|---|---|---|---|
| Months of anaesthesia completed | 6.29 | 3.59 | 6.5 | 0.25-12 | 4.25-9.75 |
| Age of resident | 29.39 | 3.03 | 28.5 | 26-37 | 28-30 |
| How many spinal anaesthetics have you done? | 11.39 | 13.1 | 13.14 | 0-50 | 3-14 |
| How comfortable do you feel completing a preoperative assessment & obtaining informed consent for spinal anaesthesia? (1=not comfortable; 3=somewhat comfortable; 5=very comfortable) |
3.44 | 0.92 | 3 | 2-5 | 3-4 |
Table 2: Characteristics of residents (n=18).
At baseline, they successfully performed 47% (SD 20%, median 45%, 25th-75th quartile range 36-41%) of the 11 required elements (Table 3). The most commonly correctly performed element was “Describe the procedure itself in clear, simple language” (100%), followed by “Describe the minor risks of the procedure” (89%)(Table 4).
| Checklist element | % of residents completing successfully |
|---|---|
| Introduce self and the discussion topic | 78% |
| Describe the indications for the procedure | 39% |
| Describe the benefits of the procedure | 50% |
| Describe the procedure itself in clear, simple language | 100% |
| Pause for questions appropriately | 56% |
| Describe the minor risks of the procedure | 89% |
| Describe the risk of serious complications. Emphasize that these are rare. | 56% |
| Describe alternatives to the procedure | 33% |
| Teach back: Ask the patient to repeat key items in discussion | 0% |
| Have the patient verbally agree with the consent form | 17% |
| Utilized CI-CARE* | 6% |
Table 3: Prior to completing curriculum the percentage of required elements on checklist Performed properly for obtaining informed consent for spinal anesthesia as assessed on a standardized patient.
| Performance assessed on | Performance assessed on actual patients | |||
|---|---|---|---|---|
| standardized patient | ||||
| Written & | Written, video | Written & | Written, video | |
| video | curriculum & | video | curriculum & | |
| curriculum | deliberate | curriculum | deliberate | |
| practice | practice | |||
| Introduce self and the | 100% | 100% | 100% | 100% |
| discussion topic | ||||
| Describe the indications | 100% | 91% | 93% | 93% |
| for the procedure | ||||
| Describe the benefits of | 100% | 100% | 93% | 90% |
| the procedure | ||||
| Describe the procedure | 100% | 100% | 100% | 100% |
| itself in clear, simple | ||||
| language | ||||
| Pause for questions | 86% | 100% | 100% | 90% |
| Appropriately | ||||
| Describe the minor risks of | 100% | 100% | 100% | 93% |
| the procedure | ||||
| Describe the risk of serious | 100% | 100% | 93% | 93% |
| Complications. Emphasize that these are rare. | ||||
| Describe alternatives to | 71% | 100% | 86% | 83% |
| the procedure | ||||
| Teach back: Ask the | 57% | 100% | 36% | 63% |
| patient to repeat key items | ||||
| in discussion | ||||
| Have the patient verbally | 86% | 100% | 79% | 97% |
| agree with the consent | ||||
| form | ||||
| Utilized CI-CARE* | 86% | 73% | 71% | 70% |
Table 4: Percentage of required elements performed properly after completing the curriculum.
The 3 most commonly missed elements were: “Teach back: Ask the patient to repeat key items in discussion” (0% correct), “Connect, Introduce, Communicate, Ask permission, Respond, Exit” (6%), and “Have the patient verbally agree with the consent forms (17%).”
The 7 residents completing the written materials and video curriculum significantly increased their performance to successfully complete 90% (SD 13%, median 91%, 25th-75th quartile range 86-100%) of the required elements on a standardized patient. They had an average of 2.0 (SD 1.4) patients for which informed consent was assessed in the preoperative holding area, and correctly performed 86% of the total of 154 (14 patients 11 elements per patient) required elements.
We were unable to study a full set of 3 patients for each of the 18 residents for logistical reasons mainly that residents moved on to other non-operating room rotations or other hospitals before completing 3 new spinals. Assessments on actual patients were performed an average of 3.22 (SD 1.2, median 3, and range 2–5 days) days after finishing the curriculum.
The 11 other residents completed the written materials and video curriculum supplemented with a 1:1 session with faculty significantly increased the percentage of properly completed elements to 97% (SD 4%, median 100%, 25th-75th quartile range 95-100%) on the standardized patient (P<0.01). These residents had a total of 30 patients for which informed consent was assessed in the preoperative holding area, and correctly performed 88% of the total of 330 (30 patients x 11 elements per patient) required elements.
Discussion
The modified Delphi method resulted in an 11-item checklist of required elements for obtaining consent for spinal anesthesia which can be further tested for use by residency programs in assessment of this skill. We used this procedural checklist to create a base written curriculum and an online video for teaching proper informed consent for spinal anesthesia. Prior to residents completing the base curriculum, the most commonly missed of the 11 required elements was “Teach back: Ask the patient to repeat key items in discussion” which aims to make sure patients understand what is being presented as this has been found in other studies to be a common deficiency.
The curriculum that was developed significantly increased correct performance for obtaining informed consent for spinal anesthesia as measured using standardized patients from slightly less than half to more than 90% of items as measured via an 11 item checklist. These benefits for proper performance of obtaining informed consent persisted for several days later on actual patients, revealing translation to clinical benefit. Additional research is required to determine what the minimum performance would have to be to have a “passing” score.
The main goal of the study was to develop the curriculum and to test it. We choose to have some of the residents also receive additional one-on-one faculty coaching but the study was not powered to detect if that had an independent incremental benefit and further studies may be warranted to assess this. The use of deliberate practice has been found to be an effective method for training for some skills including crisis management situations, cardiopulmonary bypass weaning, EEG interpretation, laryngoscopy, intubation and more [17]. However, this educational method is resource intensive primarily due to the cost of the expert’s time. For a large program with dozens of residents the 1:1 coaching may not be feasible.
Another potential limitation of deliberate practice may be that it is not well-known or understood among anesthesiology faculty educators and programs so ongoing dissemination nationally may be helpful [18]. Innate ability and learner differences may also confound the study of deliberate practice [19].
In addition to a small number of participants, this study has several other limitations. All participants were active anesthesiology residents less than 12 months into training, with varying case numbers which is common in anesthesia training [20]. Not enough residents were enrolled and there was not sufficient variability in prior spinal anesthesia experience to assess statistically whether prior experience affected baseline performance. We chose first year clinical anesthesia residents as study participants as they were most likely to have little prior exposure to obtaining consent for spinal anesthesia. Other limitations include that this study was conducted at a single institution so it is unknown if the results would have been different if participants were members of other residency programs, the study did not test for decay of skill improvement past 5 days, and completeness of documentation of informed consent in the medical record was not measured.
Although written signed consent for anesthesia may be often bundled into the patient’s surgical consent or part of a generic hospital consent form, informed consent in anesthesia is meant to be a two-way communication between the physician and the patient prior to initiation of an anesthetic. Aside from the ethical and legal responsibility, the informed consent process also may prompt active discussion of the anesthesia plan of care, associated risks, and patient concerns and expectations [21-23]. It is a key component of patientphysician communication and functions to uphold patient autonomy and promote shared decision making [24], which is associated with improved patient satisfaction and favorable outcomes [25,26]. In 2006, and again in 2011, the American Society of Anesthesiologists recommended that an anesthesia-specific informed consent to ensure that the necessary level of information has been provided to patients. Anesthesia residencies will need to have specific training and assessment for informed consent.
Anesthesiology trainees must acquire a large range of knowledge and skills. It is important to identify the most efficient way to educate anesthesiology trainees given that the formal training time is limited to 4 years. The curriculum that was developed significantly increased correct performance of properly obtaining informed consent for spinal anesthesia, and persisted at least for several day later when consenting real patients. The 11 item checklist could be further tested and used by residency programs to assess this nontechnical skill.
References
- McKneally MF, Ignagni E, Martin DK, D’Cruz J (2004) The leap to trust: perspective of cholecystectomy patients on informed decision making and consent. J Am Coll Surg 199: 51-57.
- Waisel DB, Lamiani G, Sandrock NJ, Pascucci R, Truog RD, et al. (2009) Anesthesiology trainees face ethical, practical, and relational challenges in obtaining informed consent. Anesthesiology 110: 480-486.
- Braddock CH, Edwards KA, Hasenberg NM, Laidley TL, Levinson W (1999) Informed decision making in outpatient practice: time to get back to basics. JAMA 282: 2313-2320.
- Bhattacharyya T, Yeon H, Harris MB (2005) The medical-legal aspects of informed consent in orthopaedic surgery. J Bone Joint Surg Am 87: 2395-2400.
- Thompson BM, Sparks RA, Seavey J, Wallace MD, Irvan J, et al. (2015) Informed consent training improves surgery resident performance in simulated encounters with standardized patients. Am J Surg 210: 578-584.
- Leeper-Majors K, Veale JR, Westbrook TS, Reed K (2003) The effect of standardized patient feedback in teaching surgical residents informed consent: results of a pilot study. Curr Surg 60: 615-622.
- Joyce BL, Scher E, Steenbergh T, Voutt-Goos MJ (2011) Development of an institutional resident curriculum in communication skills. J Grad Med Educ 3: 524-528.
- Ericsson KA (2015) Acquisition and Maintenance of Medical Expertise: A Perspective from the Expert-Performance Approach with Deliberate Practice. Acad Med 90: 1471-1486.
- Macario, A (2014) Can physician performance be assessed via simulation? Anesthesiology 120: 18-21.
- Ericsson KA (2008) Deliberate practice and acquisition of expert performance: a general overview. AcadEmerg Med 15: 988-994.
- Barsuk, JH, McGaghie WC, Cohen ER, O’Leary KJ, Wayne DB (2009) Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. J Crit Care Med 37: 2697-2701.
- Barsuk, JH, Cohen ER, Caprio T, McGaghie WC, Simuni T, et al. (2012) Simulation-based education with mastery learning improves residents’ lumbar puncture skills. Neurology 79: 132-137.
- Udani AD, Macario A, Kiruthiga N, Tanaka MA, Tanaka PP (2014) Simulation-based mastery learning with deliberate practice improves clinical performance in spinal anesthesia. Anesthesiol Res Pract1-10.
- Graham B, Regehr G, Wright JG (2003) Delphi as a method to establish consensus for diagnostic criteria. J ClinEpidemiol 56: 1150-1156.
- Hall DE, Prochazka AV, Fink AS (2012) Informed consent for clinical treatment. CMAJ 184: 533-540.
- Yudkowsky R (2009) Performance tests. In: Downing SM, Yudkowsk R, editors. Assessment in Health Professions Education. Routledge Taylor and Francis Group, New York 217-243.
- Hastings RH, Rickhard TC (2015) Deliberate Practice for Achieving and Maintaining Expertise in Anesthesiology. AnesthAnalg 120: 449-459.
- Udani AD, Harrison TK, Mariano ER, Derby R, Kan J et al. (2016) Comparative-Effectiveness of Simulation-Based Deliberate Practice Versus Self-Guided Practice on Resident Anesthesiologists' Acquisition of Ultrasound-Guided Regional Anesthesia Skills.RegAnesth Pain Med 41: 151-157.
- Kulasegaram KM, Grierson LE, Norman GR (2013) The roles of deliberate practice and innate ability in developing expertise: evidence and implications. Med Educ 47: 979-989.
- Yamamoto S, Tanaka P, Madsen MV, Macario A (2016) Analysis of Resident Case Logs in an Anesthesiology Residency Program.AA Case Rep 6: 257-262.
- Heine MF, Lake CL (2004) Nature and prevention of errors in anesthesiology. J Surg Oncol 88: 143-152.
- Smith, AF, Greaves JD (2010) Beyond competence: defining and promoting excellence in anaesthesia. Anaesthesia 65: 184-191.
- Lindfors PM, Meretoja OA, Töyry SM, Luukkonen RA, Elovainio MJ, et al. (2007) Job satisfaction, work ability, and life satisfaction among Finnish anaesthesiologists. ActaAnaesthesiolScand 51: 815-822
- Krumholz HM (2010) Informed consent to promote patient-centered care. JAMA 303: 1190-1191.
- Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA (2002) The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med 17: 243-252.
- Klafta JM, Roizen MR (1996) Current understanding of patients’ attitudes toward and preparation for anesthesia: a review. AnesthAnalg 83: 1314-1321.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 12155
- [From(publication date):
September-2016 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 11190
- PDF downloads : 965