Determination of the Location of Acute Gastric Leakage after Bariatric Surgery - A Novel and Simple Tool
Received: 14-May-2022 / Manuscript No. JOWT-22-63870 / Editor assigned: 16-May-2022 / PreQC No. JOWT-22-63870(PQ) / Reviewed: 30-May-2022 / QC No. JOWT-22-63870 / Revised: 04-Jun-2022 / Manuscript No. JOWT-22-63870(R) / Published Date: 10-Jun-2022 DOI: 10.4172/2165-7904.1000496
Keywords
LSG; Gastric leakage
Description
Bariatric surgery is now widely accepted as the only longterm effective treatment for morbid obesity metabolic syndrome. Laparoscopic sleeve gastrectomy (LSG) is one of the most frequently performed surgical procedures in weight loss surgery. According to the statistics of American Society for metabolic and bariatric surgery (ASMBS) in 2018, LSG ranked first in all weight loss operations, accounting for about 61.4% [1]. LSG has relatively simple operation process, significant bariatric and hypoglycemic effect, and low incidence of postoperative complications, so patients can generally accept it [2]. However, the low incidence of complications does not mean that complications can be avoided. Gastric leakage is the most serious complication of LSG. The incidence of gastric leakage after LSG in surgical centers of different hospitals varies greatly, usually 0.7% ~ 7.0% [3,4]. Gastric leakage occurred within 7 days after operation is generally called acute gastric leakage [5].
At present, for the gastric leakage in the acute stage of operation, that is, the gastric leakage within 7 days after operation, according to existing views, it is mostly advocated to focus on emergency operation + flushing + drainage + repairing the leakage, and implement all or part of it according to the situation, but repairing the leakage is indeed necessary, especially when the patient has hemodynamic instability or diffuse peritonitis. However, it is not easy to find the location of the leak during the operation. Generally speaking, due to edema, exudation and pus, it is difficult to find the specific location of the gastric leak around the gastric leak. Here, we propose a new method to use endotracheal intubation to help the operator quickly find the location of leakage in the residual stomach.
For the selection of endotracheal tube, adults generally choose 7.0- 7.5mm endotracheal tube. After selecting the tube, prepare two more tubes that are greater than and less than 0.5mm of the inner diameter of the endotracheal tube according to the actual needs, so as to adjust the model of the endotracheal tube in time during the intubation process. Before operation, check whether the catheter cuff leaks, lubricate the front section of the catheter with medical lubricant or normal saline, and place the guide wire in the endotracheal tube cavity. The intubation should be operated by an experienced anesthesiologist and carried out after the patient's anesthesia. In order to save time, it can be started simultaneously with the operation or after the operation. The best time for esophageal intubation is after laparoscopic cleaning of the abdominal cavity and before searching for the location of gastric leakage. Since there is intubation in the trachea, the difficulty of esophageal intubation is reduced, but it can also be carried out with the assistance of Macintosh laryngoscope or visual laryngoscope. One thing to emphasize is that the catheter intubation should enter the esophagus rather than the trachea. In general, the patient has entered the state of anesthesia during esophageal intubation, and the original endotracheal intubation occupies the tracheal channel. In order to avoid the compression of trachea after air bag inflation, it is generally recommended to insert all endotracheal intubation into esophagus.
After confirming the successful insertion of the endotracheal tube, inject about 10ml of gas into the guide tube cuff. However, due to the strong ductility of the esophagus, the best standard for injecting gas into the airbag is to make the pressure in the airbag reach the minimum pressure without obvious leakage around the airbag during manual inflation. After the surgeon is ready, the methylene blue test and gastric inflation test are carried out through the tracheal tube inserted into the esophagus to find the site of gastric leakage. After repair, conduct methylene blue or inflation test again to confirm that the leak has been repaired.
Gastric leakage can be divided into proximal gastric leakage, central gastric leakage, distal gastric leakage, gastric leakage in the posterior wall of the stomach and gastric leakage that cannot be located. Proximal gastric leakage is more common, especially near his angle [5,6]. The causes of gastric leakage after LGS are relatively complex. It is generally believed that it is related to the operation proficiency of doctors during operation and whether the incision is sutured and reinforced [5]. It seems to be a necessary condition to ensure the blood supply near the incision, because the perfusion of CT scanning gastric wall is significantly reduced near the his angle where gastric leakage most often occurs [7]. However, acute gastric leakage may occur even when the blood supply is sufficient.
When looking for the leak in the conventional process, the position of the leak is generally verified by methylene blue test or inflation test after inserting the gastric tube. However, there are obvious shortcomings in this way. The gastric tube is relatively slender. During the verification of the leak position, the gas or methylene blue solution may flow back along the esophageal space of patients under anesthesia. This means you can't fill the patient's stomach with enough reagent or gas. In this case, the lighter outcome is the failure of the test, and the more serious one may cause gastroesophageal reflux, esophageal ulcer and other more serious consequences. The use of nasogastric balloon tube seems to be a better choice, but patients after weight loss surgery have narrow intragastric space, especially at the gastroesophageal junction. Blind use of nasogastric tube balloon may cause incision tear,that is, the formation of new or aggravate the original gastric leakage [8].
After clinical verification, we propose a novel test method. In some patients we observed, using our method to find the site of gastric leakage in surgery is simple and easy, and achieved particularly good results. Even if there are patients with heavy abdominal adhesion, multiple operations and other complex reasons, the site of gastric leakage can still be determined. All patients recovered well after operation. Long term follow-up and observation showed that the weight loss effect of patients was not affected by the complications of postoperative gastric leakage.
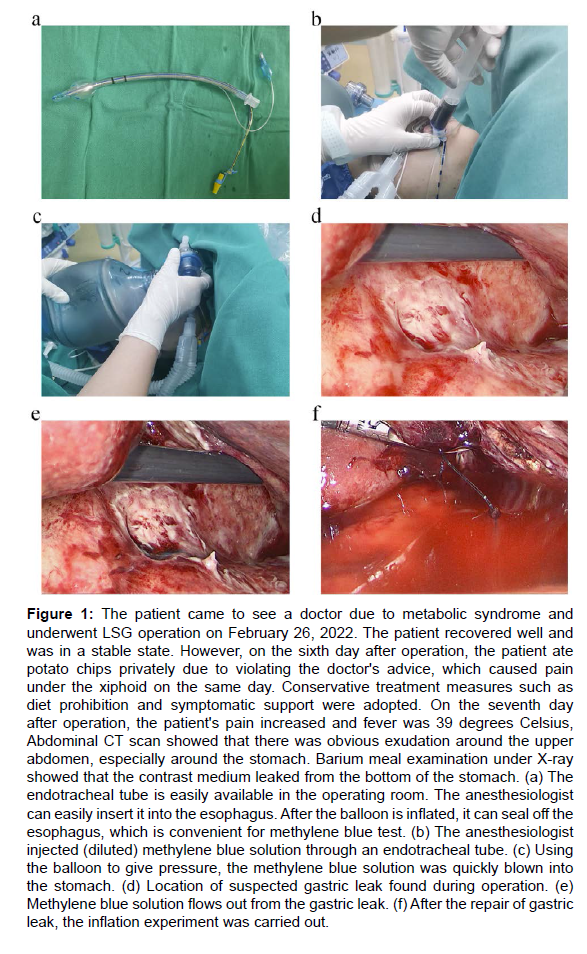
Endotracheal tube is one of the most commonly used tools in the operating room. We use it to put it into the esophagus, but it can play a unique role in detecting and verifying gastric leakage. Indeed, tracheal tube insertion into the esophagus can also lead to complications. However, according to our single center observation data, there is almost no iatrogenic injury through the operation of skilled anesthesiologists. The new acute gastric leakage detection device proposed in this paper not only greatly improves the accuracy of gastric leakage detection, but also has low cost and high safety, which helps the operator to quickly solve the problem and shorten the operation time. Moreover, in the standard process of routine laparoscopic sleeve gastrectomy, using this simple device to find gastric leakage before the end of the operation may have considerable potential to ensure the quality of the operation, and further clinical research is needed (Figure 1).
Figure 1: The patient came to see a doctor due to metabolic syndrome and underwent LSG operation on February 26, 2022. The patient recovered well and was in a stable state. However, on the sixth day after operation, the patient ate potato chips privately due to violating the doctor's advice, which caused pain under the xiphoid on the same day. Conservative treatment measures such as diet prohibition and symptomatic support were adopted. On the seventh day after operation, the patient's pain increased and fever was 39 degrees Celsius, Abdominal CT scan showed that there was obvious exudation around the upper abdomen, especially around the stomach. Barium meal examination under X-ray showed that the contrast medium leaked from the bottom of the stomach. (a) The endotracheal tube is easily available in the operating room. The anesthesiologist can easily insert it into the esophagus. After the balloon is inflated, it can seal off the esophagus, which is convenient for methylene blue test. (b) The anesthesiologist injected (diluted) methylene blue solution through an endotracheal tube. (c) Using the balloon to give pressure, the methylene blue solution was quickly blown into the stomach. (d) Location of suspected gastric leak found during operation. (e) Methylene blue solution flows out from the gastric leak. (f) After the repair of gastric leak, the inflation experiment was carried out.
Funding Sources
None.
Conflict of Interest
The authors have declared that no competing interests exist.
References
- English WJ, DeMaria EJ, Hutter MM, Kothari SN, Mattar SG, et al. (2020) American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis 16(4): 457-63.
- Young MT, Gebhart A, Phelan MJ, Nguyen NT (2015) Use and Outcomes of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Gastric Bypass: Analysis of the American College of Surgeons NSQIP. J Am Coll Surg 220(5): 880-5.
- Aurora AR, Khaitan L, Saber AA (2012) Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc 26(6): 1509-15.
- Rosenthal RJ, Diaz AA, Arvidsson D, Baker RS, Basso N, et al. (2012) International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis 8(1): 8-19.
- Cesana G, Cioffi S, Giorgi R, Villa R, Uccelli M, et al. (2018) Proximal Leakage After Laparoscopic Sleeve Gastrectomy: an Analysis of Preoperative and Operative Predictors on 1738 Consecutive Procedures. Obes Surg 28(3): 627-35.
- Csendes A, Braghetto I, Leon P, Burgos AM (2010) Management of leaks after laparoscopic sleeve gastrectomy in patients with obesity. J Gastrointest Surg 14(9): 1343-8.
- Saber AA, Azar N, Dekal M, Abdelbaki TN (2015) Computed tomographic scan mapping of gastric wall perfusion and clinical implications. Am J Surg 209(6): 999-1006.
- Roewer N (1995) Can pulmonary aspiration of gastric contents be prevented by balloon occlusion of the cardia? A study with a new nasogastric tube. Anesth Analg 80(2): 378-83.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Yin M, Ding R, Zhang C, Pan S, Gong C (2022) Determination of the Location of Acute Gastric Leakage after Bariatric Surgery - A Novel and Simple Tool. J Obes Weight Loss Ther 12: 496. DOI: 10.4172/2165-7904.1000496
Copyright: © 2022 Yin M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2875
- [From(publication date): 0-2022 - Nov 16, 2025]
- Breakdown by view type
- HTML page views: 2272
- PDF downloads: 603