Determinants of traditional uvulectomy practice among mothers of Ungogo Local Government, Kano State
Received: 20-May-2024 / Manuscript No. JCPHN-24-136570 / Editor assigned: 22-May-2024 / PreQC No. JCPHN-24-136570 (PQ) / Reviewed: 29-May-2024 / QC No. JCPHN-24-136570 / Revised: 03-Jun-2024 / Manuscript No. JCPHN-24-136570 (R) / Published Date: 11-Jun-2024
Abstract
Traditional uvulectomy is a surgical procedure in which the total or partial part of the uvula is removed by traditional surgeons. Traditional uvulectomy is widely practiced in some African countries such as Nigeria, in northern part of Nigeria particularly the hausa speaking areas, traditional uvulectomy is widely practice especially with the vulnerable children mostly neonates, such practice usually take place at first week of life, which may be associated with life threatening complications. The objectives of the study is to assess the level of knowledge and awareness of traditional uvulectomy, to assess the complications arising from the procedure and where they are managed and to find out possible ways of preventing the traditional uvulectomy practice. a cross sectional study was conducted to assess the determinants of traditional uvulectomy among 150 mothers selected by multi stage sampling from 25 March to 1 April at Ungogo Local Government Kano State. A set of administered questionnaire with translation into hausa by the researcher and assistants was used to collect data on research variables. The data was analysed using frequency and percentages. Most of the respondents were Hausa 60%, Married 70%, Housewife 60% aged range from 26-35 years. Majority of the respondents have idea about uvula 80%, Majority of the respondents believed bleeding is one of the complications of traditional uvulectomy practice 90%, fever 70%, nasal regurgitation 70% they don\'t know and most of the respondents seek their management at health facilities 90%, home 90% and traditional uvulectomist 67% and 70% of the respondents strongly agreed that traditional uvuluvulectomy practice can be prevented through health education 70% agreed can be prevented through Community participation and 70% also through community engagement and involvement and 50% of the respondents agreed that using setting controlling mechanisms for the health care delivery system can be used to prevents traditional uvulectomy practice. This study revealed that there is so many complications arising as a result of traditional uvulectomy practice, and possible ways are found to prevents the procedure mostly through health education and community mobilizations. The government should organizes massive campaigns aimed at discouraging the practice of traditional uvulectomy to the community through media, at home visits and should assist with funding of programs in training and provides the barbers with cleansing agents for disinfecting their equipments.
Keywords
Traditional uvulectomy; Mothers; Ungogo local government; Kano state
Introduction
Background to the study
Uvulectomy is the entire or partial removal of the uvula through surgery, and the procedure can be viewed in two ways. Traditional uvulectomy is a surgical procedure in which the total or partial part of the uvula is removed by traditional surgeons. The uvula is a small pendant fleshy lobe that is located above the throat, hangs from the palate at a lower central border, and between the two lymphoid tissues or tonsils. Uvula helps to prevent choking, during swallowing by moving superiorly and close to the nasopharynx keep swallowed matter like food and liquid get into the nasal cavity. The uvula is a small piece of soft tissue that dangles down centrally from the soft palate. It has an abundance of salivary glands, and plays a large role in moistening the oropharyngeal and pharyngeal mucosa. The Uvula is also important for articulation of speech [1].
The traditional uvulectomy (the partial or complete removal of the uvula traditionally) has for long been a common practice in many African countries especially in north and west African countries [2].
Ajiya A (2019) who conducted a research on pattern of otitis media in children and adolescents with traditional uvulectomy in Kano, Nigeria states that traditional instruments such as a sharp blade (knife) and threads made from horsetail and other inputs are used for the cutting of uvula. First, the baby is held firmly and then the tongue is pulled. The uvula is then strapped by a thread, and cut out with a sharp instrument prepared by a traditional surgeon. The tools used to cut uvula are not clean and the procedure is careless, the individual who is subject to the practice is more likely to be exposed to a variety of health problems including death. As noted by various studies, hemorrhage following the procedure, nasal regurgitation, adjacent body part trauma (soft palate and tongue base abrasion), swallowing difficulty, malnutrition, speech problem, and local infections like abscesses, otitis media were the most prevalent complications.
Traditional uvulectomy is one of the oldest traditional surgical procedures carried out by traditional surgeons and this practice is as old as mankind [3]. Historian speculates on the origins of uvulectomy. At 4th century before the birth of jesus Hippocrates recommended seizing an inflamed uvula with the fingers, pressing it against the palate and cutting off the end. At 2nd century after the birth of jesus Galen suggested not operating upon the uvula until it had assumed assumed the physical characteristics of leather. During the 11th century, Seville and Cordoba in Spain became the headquarters for specialization in surgery. Uvulectomies were performed either with a scalpel or by dipping of the uvula into burning caustics held in a spoon-shaped device. After 11th century, the practice of uvulectomy essentially died out in Europe. There was one brief flourish of popularity, mainly in England and France during the 19th century, when James Yearly introduced and advocated uvulectomy did not diminish in other area.
Fredrico Apffel Marglin who is professor of Anthropology from Morocco speculates that the practice of traditional uvulectomy in northern Morocco may have originated after the ‘reconquista’ with Muslim refugee who may have been a disciple of Spanish physicians. Imperator and Maclean assert that the procedures performed by Hausa barber surgeons are derived from early Arabic medicine. Abdallah on the other hand, feels that while bloodletting came into northern Nigeria with Islam, tribal marks, uvulectomy and hymenectomy are indigenous because there is no reference to uvulectomy in the works on prophetic medicine. He believes that the practice of uvulectomy in Sudan might be a remedy borrowed from Hausa settlers or pilgrims on their way to Mecca.
Apffel, however, has suggested that uvulectomy originated as prophylactic surgery. He found that ‘neonatal uvulectomy is followed by total atrophy or rather non-developmental of the regional lymphoid tissue. He could not see or feel tonsils or adenoids in any of his uvulectomised patients, and found that the incidence of middle ear infection was very low. therefore, a close interdependence between the uvula and the surrounding lymph glands. It’s possible that uvulectomy was at one time thought to be a prophylactic against sleeping sickness. The swelling of the cervical lymph nodes is the most noted symptom of sleeping sickness in areas where the disease is endemic. The lack of swelling associated with uvulectomy might make it appear that the person was immune. It’s interesting to note, in this regard, that ‘enlargement of the neck glands as a sign of sleeping sickness was widely known also among the former slaves who showed this sign. Sickle-cell anemia is another disease which exhibits lymph node and tonsil enlargement. Although this is not widely reported in the American literature on Sickle-cell anemia, a study in Accra, Ghana, described lymph node and tonsil enlargement in 50% of sickle-cell patients. While uvulectomy would neither prevent nor cure Sickle-cell anemia, it could appear to alleviate one of the symptoms and part of the pain.
In Nigeria, traditional uvulectomy is usually performed during neonatal period and the prevalence is higher among the Hausa-Fulani ethnic group. Nevertheless, this can be explain by the fact that, in most Hausa sub group, the practice of traditional uvulectomy is substantially performed around the seventh day after birth during the naming ceremony as the parents believes that, the baby will benefits the the uvulectomy as it is a prophylactically done during the first week by removing the uvula either completely or partially. The procedure of the traditional uvulectomy is usually carried out by barbers on the request of their client, and uses an unsterilized equipments sickle-shapes knife like is used by traditional healers/surgeon without any form of anesthesia [4].
According to Chatora (2015) traditional uvulectomy is the practice of removing uvula for curative customs reason by traditional doctors and is still performed despite numerous hazards associated with it.
The traditional uvulectomy is performed by local Baber's who inherited the skills from their predecessors without any formal medical training, it is often completed without any regard to recommended standard of good surgical practices. In sub-saharan Africa, traditional uvulectomy is largely driven by indigenous beliefs and cultural practice with many local non physicians’ healers believing and preaching that the uvula is the main organ responsible for all throat and chest related health problems and thus should should be removed as early as possible in childhood. However, despite being a common cultural practice, the traditional uvulectomy has been associated with substantial numbers of harmful outcomes with significant morbidity and mortality largely from hemorrhage and sepsis [5].
Statement of the problem
Traditional uvulectomy is a common practice among some tribes especially in northern part of Nigeria and it is usually associated with traditional beliefs and customs and practice and instruments used for the procedure are not sterilized, and there are reports of use of these instruments on several patients in the same session thereby exposing them to complications such as Human Immunodeficiency Virus (HIV) infections, hepatitis and hemorrhage from tonsils [6]. Numerous severe complications have been found in association with the procedure heamorrhage and anemia, oropharyngeal infection, callulitis of the neck, septicemia, tetanus, risk of HIV, peritonsillar and parapheryngeal abscesses, aspiration with consequent upper air-way obstruction and lary diseases, infant and child morbidity and even death [7].
Considering the rate at which complications are arising and still the traditional uvulectomy are undergoing among the newly born babies it is obvious that there is still low level of knowledge and awareness on traditional uvulectomy procedure among their newborn parents. However, ungogo local government area under kano state is a community inhabited predominantly by Hausa-Fulani tribal residents and therefore the practice of traditional uvulectomy has been one of the harmful traditional practice of parents on their newly born babies, as such this stimulated me toward developing an interest and initiative to conduct this very research work to assess the determinants of traditional uvulectomy among mothers in this area.
General Objectives
The general objective is to assess the determinants of traditional uvulectomy practices among mothers in Ungogo Local Government, Kano state.
Specific Objectives
- To assess the knowledge and awareness of traditional uvulectomy practices among mothers in ungogo local government, kano state.
- To determine the complications arising from the traditional procedure and where they are managed among mothers at ungogo local government, kano state.
- To find out the possible ways of preventing the traditional uvulectomy practices among mothers in ungogo local government, kano state.
Research questions
- What is the level of knowledge and awareness of traditional uvulectomy practices among mothers in ungogo local government, kano state.
- What are the complications of traditional uvulectomy practices and where they are managed among mothers in ungogo local government, kano state.
- What are the possible ways of preventing the traditional uvulectomy practices among mothers in ungogo local government, kano state.
Significance of the study
The findings of the research work will specifically benefits the mothers of ungogo local government area, Kano. Community in general as it aimed at assessing and investigation the determinants of the practices of traditional uvulectomy. The research work is very significant to the community, government, organizations and health institutions including health professionals by highlighting the findings of the study, the community will be enlightened on the incidence of the traditional uvulectomy and the hazard associated with it there by discouraging people from the practice. After exploring the government in policy making and also in developing strategies such as community home visit, health education and awareness campaign to combat the problem. It will also help government to introduce programs at health care facilities to prevent dangers associated with traditional uvulectomy. The findings will also educate women, health agencies and community about the dangers associated with the practice of traditional uvulectomy and takes possible precaution before practicing it.
Scope of the study
The research work is limited to the mothers of ungogo local government area under kano state.
Operational definition of terms
Determinants: is a factor or cause that makes something happen or leads directly to a decision.
Traditional: Being part of belief, customs or way of life of a particular group of people that haven’t changed for a long period of time.
Uvulectomy: A surgical procedure in which all or part of the uvula is removed.
Mothers: a woman who has borne a child or a female parent of a child.
Uvula: Is a bell-shaped like organ that hangs from the top of the throat.
Practice: The action rather than the theory of doing something.
Literature review
This chapter will be discussing under the following: conceptual framework, Anatomy of the uvula, functions of the uvula, definition of uvulectomy, indication of uvulectomy, concept of uvulectomy, purpose of the traditional uvulectomy, complication following traditional uvulectomy practice, the preventive measures of traditional uvulectomy, empirical review and theoretical framework
Conceptual review
Anatomy of the uvula
The uvula is sometimes called Palatine uvula and also means “little grape” in Latin. It’s a curved fold of muscle covered with mucous membrane hanging down from the middle of the free border of the soft palate originating from the upper end of the uvula are four folds of mucous membranes, two passing downwards at each side to form membranous arches, the posterior folds, one on each side are palatopharyngeal arches and the two anterior folds are the palatoglossal arches.
Arterial supply is mainly from palatine branch of the ascending pharyngeal artery, the ascending palatine, a branch of the facial artery and supplemented by the lesser palatine branches of the descending palatine (maxillary artery). Venous drainage is to the pterigoid plexus and thence, through the deep facial vein to the anterior facial vein and into the internal jugular vein. The lymphatic drainage is partly by way of retropharyngeal nodes but chiefly direct to the upper deep cervical group of nodes. The mucous membrane is innervated by the lesser palatine and glossopharyngeal nerves while the muscles are supplied by the pharyngeal plexus (a glossopharyngeal/vagal complex).
Functions of uvula
The uvula serves as a pilot for eating and swallowing. It prevents the soft palate from being forced into the nasopharynx or mouth when it is resisting pressure differences between these and the oral part of the pharynx as in coughing or sneezing. It forms part of the soft palate and, together is important in deglutination (maintain the velopharyngeal closure. It acts as as temperature sensor on ingested foods/drinks. The uvula has also its own natural advantages of lubricating oropharyngeal mucosa, serving for language communication, boosting immunological function and in conjunction with the soft palatine closes the nasopharynx, therefore, preventing aspiration and regurgitation of food or water into the nose.
Definition of uvulectomy
Uvulectomy is the entire or partial removal of the uvula through surgery, and the procedure can be viewed in two ways.
Indications of uvulectomy
The removal of the uvula for minor and major pharyngeal lesions is common in the Otorhinolaryngological practice. The Otorhinolaryngological indication for uvulectomy as described by Kristin (2014) includes the following [8]:
- The procedure is indicated alone as a large procedure called Uvulopalatopharyngoplasty (UPPP) to ablate the tissue that may be blocking the air passage.
- It is also indicated for the treatment of Hereditary Angioneurotic Edema (HANE), which is a rare familial disease of C1 esterase inhibitor deficiency that produces recurrent attacks of acute circumscribed non-inflammatory edema, thus causing death by asphyxiation.
- Uvulectomy has also been done for the management of heavy snorers.
- Uvulectomy is also performed for Redundant Uvula, which breaches the laryngeal inlets. In such cases, the patient has a feeling of mass in the voice box (larynx), chocking during sleep and has to clear the throat, in such patients, saliva originating from hyperactive mumcoserous glands from the soft palate is directed right into the supraglottic.
Definition of traditional uvulectomy
The traditional uvulectomy is a procedure in which traditional healer practitioners (usually traditional Barbers) amputate the uvula using unsterilized sickled shaped knife without any form of anesthesia, after which a mixture of herbs is applied to the stump of the soft palate [2]. The practice of traditional uvulectomy has for centuries been a common ritualistic practice in many Sub-saharan African countries and it is much more common in Nigeria, Tanzania Kenya, Sierra Leon and Niger republic. However, in Nigeria the prevalence is higher among Hausa-Fulani ethnic groups (about 66.2%) and the complications for children less than five years of age due to the procedure account for about 7.8% per 1000 [4].
In the Hausa-speaking communities of Nigeria and Niger, traditional uvulectomy is performed as part of a Muslim naming ceremony on the seventh day after birth. This ritual is thought to prevent death from swelling of the uvula, which could burst and kill the neonate. In fact, uvula in Hausa means throat herb in Niger, and it is believed that the uvula should be cut prophylactically, just like weeds in the field. These ritualistic uvulectomy are usually performed by an apprenticed barber-surgeon, who identifies a diseased uvula by looking for a finger imprint after pressing on the child’sforehead or by identifying a swollen, red, white or long uvula. The barber then recites verses from the Koran and an inaudible prayer that is thought to protect the child and to guide the barber. The uvula is completely or partially excised using a sickle-shaped knife. Hemostatis is obtained with herbal providers. The uvula is then placed on the forehead of the child and later hangs on the wall in his or her home. During the ritual, the child’s head is shaved, and circumcision may also be performed [9].
Traditional instruments such as a sharp blade (knife) and threads made from horsetail and other inputs are used for the cutting of uvula. First, the baby is held firmly and then the tongue is pulled. The uvula is then strapped by a thread, and cut out with a sharp instrument prepared by a traditional surgeon. The tools used to cut uvula are not clean and the procedure is careless, the individual who is subject to the practice is more likely to be exposed to a variety of health problems including death.
Purpose of traditional uvulectomy
The most common purpose behind the mind of community members that practices the procedure of traditional uvulectomy is to prevent death due to swelling of the uvula. This is because, it is a ritual to them that the uvula is growing as an individual is growing by age to the extent that the uvula will one day become so big enough and block the food and air passages. While some belief that uvula is the resultant root cause of all throat related health problems. Reasons for performing ritual uvulectomy is it facilitates breast-feeding and speech, it ensures better health throughout life, that it decreases thirst, it prevents infants from choking; and prevents infant diarrhea [6].
Complications following traditional uvulectomy
Some of the complications of traditional uvulectomy are as follows:
- Nasal regurgitation of fluid: the uvula and soft palate creates a barrier between the throat and the esophageal tract during swallowing, therefore, taking it off removes the barrier and can allow food or fluid to enter the upper respiratory tract.
- Speech change: Speech and voice are good with uvula especially in some languages because it enhances and provides good pitch when pronunciation, a person who undergoes uvulectomy experience change in voice which tends to be more resonance and occurs when the uvula is removed because the soft palate alone may not be able to completely prevent the air flow from the throat to the nose during speech.
- Infection: Infection may be confined to the uvula stump or can extend to the surrounding tissues, hence, epiglottis, acute otitis media, tonsillitis, or may be disseminated as in tetanus, HIV/AIDs and septicemia. Sometimes infections can lead to disseminated intravascular coagulation or endotoxic shock [10].
- Velopharyngeal insufficiency: Damage to the soft palate of varying degrees in cases of bifid palate and complete amputation results in velopharyngeal insufficiency. Other complications include aspiration of the amputated tissues of the uvula and blood.
- Neurogenic shock: this occur as a result of the procedure that is carried out without any form of analgesics or an anesthesia, as such the pain put the victims in to shock.
- Stenosis of the pharynx: It was observed that people who have had traditional uvulectomy or uvulopalatopharyngoplasty develops complications which include pharyngeal stenosis, tubal disorders and regurgitation of food through the nose. Other complications encountered include obstructive feeling in the throat, disorder of sense of taste and difficulties in disgorging fish bones while eating fish. Sometimes post uvulectomy patients burns their throat even after sensing food and/or soup was not so hot in the oral cavity.
Preventive measures of traditional uvulectomy
According to Isah (2016) the following are strategic of preventing traditional uvulectomy practice [9]:
- Organizing workshops involving the traditional barber, parents and community leaders to sensitize them on the functions of palatine uvula and the negative effects following traditional uvulectomy practice.
- Educating mothers on the commonest throat disorders and their signs and symptoms and advise them on prompt presentation of children to the nearest health facilities when they are sick.
- Educate mothers to avoid such things or practices that injure the uvula or lead to throat problems especially poor personal hygiene.
- At health facility setting, a health worker (especially midwife) should advices the mother including the family members on not to allow the practice of traditional uvulectomy on the offsprings as it has a recognized negative effect on the baby's health and well-being.
- Mobilize the community-based barber in particular to understand the effects of and refrain from the practice of traditional uvulectomy by probing them that the uvula was found to be useful to human life as in voice tone and immunological functions and so on.
- Advocate the community leaders to have an insight about the practice of traditional uvulectomy and its possible effects to the health and to put their efforts on measures to be carried out for the people to stop it in their respective communities.
Empirical review
Knowledge and awareness of traditional uvulectomy practices
In a study conducted by Dr Samuel Kariuki Ngugi (2005) on determinants of traditional uvulectomy among under five children at Thika District Hospital shows out of 311 children who had uvulectomy done, 67.2% of their parents/guardians were of primary school standard. On indications most parents took their children for uvulectomy to prevent vomiting after feeds (43%). Recurrent cough accounted to 36%. It is worth noting that most of these indications can be grouped together as upper respiratory tract infections. On Belief in uvulectomy out of the 311 respondents, 217(69.8%) indicated they still believe in uvulectomy. The main reason for this is because there was improvement on the index child. Only 17% would have uvulectomy because of cultural believes. There were 93 (30.2%) of parents who would not take another child for uvulectomy again. This is either due to lack of improvement (34.4%), or are well informed (15%) or just don’t believe in this practice.
The age at which traditional uvulectomy is performed vary from community to community, reports shows that the procedure of traditional uvulectomy is normally done at birth to 1 year or 5 years of age, the incidence of the procedure decreases as the age of the children increases [11].
In Ajibade et al study (2013) most (68.8%) of the children that had traditional uvulectomy were aged 0-12 months, 21.1% aged 2-3years and 4-5 years accounts for 10%.
In the study conducted by Adamu Asma'u et al (2021) on perception of traditional uvulectomy and associated factors among mothers of under five years children in Sokoto State, Nigeria shows that 320 mothers were selected and majority 136(42.5%) of the respondents were between 25-34 years with a mean age of 29.9± 8.3 years. Most 304 (95.0) were Hausa’s and Muslims 315 (98.4). Fulltime house wives constituted 234(73.1%) of the respondents, while those with children between one to five years were 244(76.2%). Almost two-third (65.0%) of the respondents had inappropriate perception on traditional uvulectomy (TU). Two hundred and fifteen (67.2%) of the respondents believed traditional uvulectomy should be done for under five years’ children. Most (57.2%) of them perceived it is not necessary for government to come up with a law to abolish the practice of TU in the society. Majority (59.9%) of the respondents believed TU should be done for under fiveyear children as a tradition.
Complications arising from the traditional procedure and where they are managed
Elyajouri et al reported a case of Grisel’s Syndrome in an eight month eight baby following TU. The outcome of this procedure varies, in Niger, where by the age of five years 19.6% of the population has had TU, complications of traditional uvulectomy account for 7.8 per 1000 cases of hospital admission for children below 15 years of age, notable complications from their study were infections(including Tetanus),haemorrhage and passage of cut pieces of uvula down the respiratory tract [12].
In the study of Abdullahi M et al (2016) on traditional uvulectomy among the neonates experienced in a Nigerian [6]. Tertiary Health Institution shows out of 27 medical case folders of neonates hospitalized for traditional uvulectomy, only 21 case folders were available for review. There were 12(57.1%) males and 9(42.9%) females, with a male to female ratio of 1.3:1. the age range between 1 to 21 days with the mean age of 8.8 days. All the patients had traditional uvulectomy within the 21 days of life but majority 11(52.4%) were performed in the first week of life. The mean duration of complications before hospitalization was 8.4 hours: only 1(4.8%) patient presented in an hour to the hospital. Post-uvulectomy haemorrhage 18(85.7%) was the most common complication occurring from complete amputation of the uvula 8(38.1%) and partial uvular amputation 4(19%), other collateral bleeding sites secondary to trauma were: soft palatal abrasion 5(23.8%) and tongue base abrasion 1(4.8%) as shown in table 1 However, only 12(57.1%) patients presented with active post-uvulectomy haemorrhage. Three (14.3%) patients had septicaemia from the infected site of uvulectomy [13]. All the patients were anaemic (PCV 15-24%). Prevention of sore throat 12(57.1%) was the main reason for traditional uvulectomy. Other reasons include: family tradition 5(23.8%), cough 2(9.5%) and to prevent delay speech 2(9.5%). Traditional medications were administered by the traditional healers in 7(33.3%) patients to control bleeding.
In the study of Abdullahi M et al (2016) in management and outcome, all the patients had blood transfusions, anti-tetanus toxoid, intravenous antibiotics was administered [6], and 12(57.1%) patients had bleeding site coagulated with bipolar diathermy under general anaesthesia. Two (9.5%) patients with severe septicaemia died within 24 hours of admission, while the rest were discharged after full recovery. Only five (23.8%) patients came for follow-up after a week of discharge (no complication was observed).
Majority of the patients (76.2%) in this study never came for follow up after discharged. Probably because of parenteral perception of no need for follow up, low socioeconomic status and or poor educational status. Emphasis on follow up should be made for early recognition and prompt treatment of speech problems and nasal regurgitation from velopharyngeal incompetence.
In the study by Adoga AA, et al (2011): 165 patients who had uvulectomy, 8% had septicaemia as a complication [7].
Possible ways of preventing the traditional uvulectomy practices
In a study conducted by Dr Samuel Kariuki Ngugi (2005) on determinants of traditional uvulectomy among under five children at Thika District Hospital shows only 88(28.3%) of the respondents sort advise from the health provider on indications for uvulectomy before making a decision to have their children undergo uvulectomy. For those that no longer believe in uvulectomy 93(28.9%), they gave reason as no improvement on previous operation 32(34.4%), well informed 14(15.1%) or just don’t believe in the practice 27(29.0%).
Women (mothers) are the most important in making decisions when it comes to traditional uvulectomy.
In the Study done By Sadiya (2023) the result of the study indicated that it can be prevented through health education (40%),it can be prevented through community mobilization (42%),it can be prevented through community participation (18%).
Theoretical framework
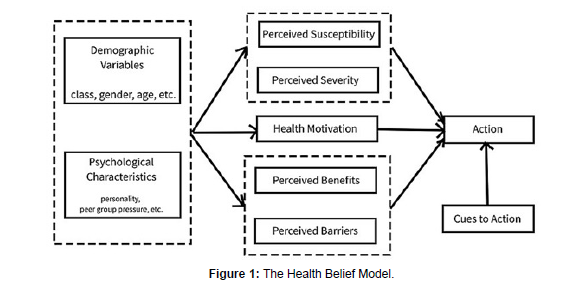
The health belief model (HBM) is a social psychological health behavior change model developed to explain and predict health-related behaviors, particularly in regard to the uptake of health services. The HBM suggests that people's beliefs about health problems, perceived benefits of action and barriers to actionand self-efficacy explain engagement(or lack ofengagement) in health-promoting behavior. A stimulus, or cue to action, must also be present in order to trigger the health-promoting behavior [14].
The practice of health promotion and diseases prevention is supported by numerous theories and concepts. In order to understand and explain health behavior and to guide the selection, development, and implementation of preventions, program planners employ theories and models.One of the first theories of health behavior, the HBM was developed in 1950s by social psychologists Irwin. Rosenstock, Godfrey. Hochbaum. Stephen Kegeles, and Howard Leventhal at the U.S. Public Health Service. At that time, researchers and health practitioners were worried because few people were getting screened for Tuberculosis (TB), even if mobile X-ray cars went to neighborhoods. The HBM has been applied to predict a wide variety of health-related behaviors such as being screened for the early detection of asymptomatic diseases and receiving immunizations. More recently, the model has been applied to understand intentions to vaccinate (e.g. COVID-19), responses to symptoms of disease, compliance with medical regimens, lifestyle behaviors (e.g., sexual risk behaviors), and behaviors related to chronic illnesses, which may require long-term behavior maintenance in addition to initial behavior change. Amendments to the model were made as late as 1988 to incorporate emerging evidence within the field of psychology about the role of self-efficacy in decision-making and behavior. According to this model, your individual beliefs about health and health conditions play a role in determining your health-related behaviors. Key factors that affect approach to health include:
- Any barriers that might be standing in someone way
- Exposure to information that prompts a person to take action
- How much of a benefit that someone think can get from engaging in healthy behaviors
- How susceptible a person think is to illness
- What a person think the consequences will be of becoming sick
- Confidence in ability to succeed.
- This article discusses how the Health Belief Model works, the different components of the model, and how this approach can be used to address health-related behaviors.
- What Are the Components of the Health Belief Model?
- There are six main components of the Health Belief Model. Four of these constructs were main tenets of the theory when it was first developed. Two were added in response to research on the model related to addiction.
Perceived severity
The probability that a person will change their health behaviors to avoid a consequence depends on how serious they believe the consequences will be. For example: If a person is young and grow seeing certain traditional procedure is undergoing in a community, it is unlikely to avoid practicing that procedure just because certain problem may likely to arise.
Perceived susceptibility
People will not change their health behaviors unless they believe that they are at risk. For example:
- Individuals who do not think they will get the flu are less likely to get a yearly flu shot.
- People who think they are unlikely to get certain infection are less likely to protect themselves.
Perceived benefits
It's difficult for someone to convince people to change a behavior if there isn't something in it for them. People do not want to give up something they enjoy if they don't also get something in return. For example:
- A person probably would not stop some harmful traditional practices if they don't think that doing so will improve their life in some way.
- A couple might not choose to practice safe sex if they don't see how it could make their sex life better.
Perceived barriers
One of the major reasons people do not change their health behaviors is that they think doing so is going to be hard. Changing health behaviors can require effort, money, and time. Commonly perceived barriers include:
- Amount of effort needed
- Danger
- Discomfort
- Social consequences
- Cues to Action
One of the best things about the Health Belief Model is how realistically it frames people's behaviors. It recognizes the fact that sometimes wanting to change a health behavior isn't enough to actually make someone do it. Because of this, it includes two more elements that are necessary to get an individual to make the leap. These two elements are cues to action and self-efficacy [15].
Cues to action are external events that prompt a desire to make a health change. They can be anything from a blood pressure van being present at a health fair, to seeing a condom poster on a train, to having a relative die of cancer. A cue to action is something that helps move someone from wanting to make a health change to actually making the change.
Self-efficacy
Self- Efficacy was not added to the model until 1988. Self-efficacy looks at a person's belief in their ability to make a health-related change. It may seem trivial, but faith in your ability to do something has anenormous impact on your actual ability to do it. Finding ways to improve individual self-efficacy can have a positive impact on health-related behaviors. For example, one study found that women who had a greater sense of self-efficacy toward breastfeeding were more likely to nurse their infants longer. The researchers concluded that teaching mothers to be more confident about breastfeeding would improve infant nutrition [16].
In this study as well, teaching mothers and parents the possible ways of preventing the traditional uvulectomy and the reason of preventing the procedure will improve the quality of life in the most especially in children (Figure 1).
The Health Belief Model proposes that people most likely to take preventative action if they perceive the threat of a health risk to be serious, if they feel they are personally susceptible and if there are fewer costs than benefits to engaging in it. For an individual to adopt a specific behavior, the perception of the threat of awareness and acceptance of the health behavior must outweigh the perceived barriers.
Material and Methods
This chapter described the various research methodologies and procedures used in carrying out the study. These are: research design, research setting, target population, sample and sampling technique, Instrument for data collection, validity and reliability of instrument, method of data collection, method of data analysis, and Ethical consideration.
Research design
A descriptive cross-sectional research design was used for this study. This Method allows people's views, opinions on a particular issue that concerns them, it also allows people to show their feelings or reaction to estimate the general view of the entire population about the topic being investigated [17].
Research setting
This study was carried out in Ungogo LGA which is situated in Kano state, North-west region of Nigeria. It is located at latitude 12.0906°N and longitude 8.4967°E. (Post offices, 2009). It is one of the 44 LGAs in the state and is situated in the northern part of the country. The majority of the people in the area are Hausa-Fulani, who are predominantly Muslims. However, there are also significant populations of other ethnic groups, including Kanuri, Igbo, Yoruba, and others. The headquarters of Ungogo LGA is in the town of Ungogo. Ungogo LGA, like other LGAs in Nigeria, is governed by a chairman who is elected by the people. The LGA administration is responsible for providing basic amenities and services to the residents, such as healthcare, education, infrastructure, and basic social amenities. Ungogo LGA is known for its cultural heritage and traditional festivals. Ungogo LGA shares borders with several other LGAs within Kano State, Nigeria. Its neighboring LGAs include: Kano Municipal LGA: Located to the south of Ungogo, Tarauni LGA: Situated to the west of Ungogo, Dawakin Kudu LGA: Located to the north of Ungogo, Kumbotso LGA: Situated to the east of Ungogo [18]. The lifestyle in Ungogo LGA is primarily influenced by the agrarian economy, Islamic culture, and traditional values.
Ungogo is a local government with the estimated population of 369,567 and it has an, area of 204km2. (Census2006)
There are 11 wards in Ungogo Local Government Area which are Bachirawa, Gayawa, Kadawa, Rangaza, Zango, Karo, Panisau, Tudun Fulani, Rijiyar Zaki, Ungogo and Yadakunya. ( INEC, 2023)
The National Population Commission of Nigeria and National Bureau of Statistics from protection 2022 estimated that Ungogo Local Government has a total population of 6015000
Target population
The ungogo has a female projected population of 173,365 from census 2006 and the target population for this study were the mothers of Ungogo Local Government. The mothers of Ungogo local government are women that are from low socio economic status, mostly having the age of 17 to above with low level of education. Some of them have single families in which their husbands dead and leave them with their children. While some are divorcee while others are married. Most of the mothers are unemployed and some participate in sewing and weaving as occupations. Due to their adherence to traditional practices and unaware of some harmful traditional practices that is what make the researcher to assess the determinants of traditional uvulectomy practice in Ungogo LGA [19].
Sample size
The minimum sample size for this study is calculated using Cochrans formulae
This formula has been used because the exact number of population is not known.
Sample Size = [z2 × p (1-p)] / e^2
z = z-score = 1.652
e = margin of error = 0.07
p = standard of deviation = 0.5
Sample Size = [z2 × p (1-p)] / e^2
= [1.652 × 0.5(1-0.5)] / 0.07^2
= [2.7225 × 0.25] / 0.0049
= 0.6806 / 0.0049
= 138.89 plus 10% attrition
10/100 = 0.1
=0.1×138.89
=13.889 + 138.89
= 152.77
= 153 approximately
Sampling techniques
A multistage sampling technique was used in conducting this research. simple random and systematic sampling was used. The simple random sampling is a type of probability sampling in which the researcher randomly selects a subset of participants from a population, and systematic sampling is a probability sampling method where researchers select participant members of a population at a regular interval. This gives every individual an equal chance of being selected. Two of the 11 wards of Ungogo LGA was randomly selected by using die draws method, this resulted in the selection of Bachirawa and Ungogo and 500 houses were chosen at random using their address numbers. Finally, the houses were selected by systematic sampling using a sampling interval of 3 obtained by dividing the number of houses (500) by the required sample (153). From each selected house, an eligible mother was identified and administered the tool after her informed consent. Where there were more than one eligible respondent in a house, one was selected using a simple random sampling by die draws. This was continued until the desired sample size was attained.
Instruments for data collection
A self-structured questionnaire was the instrument for data collection which comprises of four sections Section A: Assess respondent personal data, Section B: Assess the knowledge and awareness of traditional uvulectomy practice of the respondents, Section C: Determine the complications arising from the traditional procedure and where they are managed from the respondents and Section D: To find out the possible ways of preventing the traditional uvulectomy practices
Validity of instrument
Validity refers to how accurately a method measures what is intended to measure. The validity of a measurement can be estimated based on three main types of evidence;
- Construct validity is about how well a test measures the concept it was designed to evaluate.
- Face validity refers to the degree to which an assessment or test subjectively appears to measure the variable or construct that it is supposed to measure.
- Criterion validity evaluates how accurately a test measures the outcome it was designed to measure.
- The instrument was prepared by the researcher after reviewed of relevant literatures and was presented to the research supervisor and two (2) other lecturers from the department of nursing sciences BUK for face and content validity.
- To establish face validity, the instrument was given to the supervisor who reviewed the instrument and made necessary suggestions.
For content validity, in addition to linking the research objectives for establishing face and content validity, two experts from department of nursing science BUK was solicited to review the instrument's items follow, easiness and correctness of the items of the questionnaire. The suggestions made by these experts were affected. The instrument was taken back to them after affecting their suggestions. Corrections were made before the final draft of the instrument and was produced and administered to the respondent [20].
Reliability of instrument
The reliability of instrument was obtained by test and retest method by giving the same test to the same test respondents on different occasions. where (15) of the questionnaires were distributed in different communities. thirteen (13) response obtained from respondents were analyzed which necessitate the continuation of the study.
Method of data collection
After obtaining an ethical clearance and permission from the Kano state ministry of health and Wards Head, an informed consent, from the respondents after a full introduction by the researcher prior to the conduct of the study. The researcher explained the purpose and nature of the study to the participants. The researcher together with two other colleagues who were willingly volunteers to participate in the study, the data were collected by reading and translating the questionnaire in Hausa for five days period, after explaining in details and making emphasis on confidentiality before the data were collected and names of the respondents would not be captured in the questionnaire. The participants gave their answers base on what they experienced [21].
Method of data analysis
The collected data was analyzed by the researcher using statistical package of social sciences (SPSS) where the subjects responses was categorized, coded, and label. Descriptive statistics of frequency and percentage where applied to present the data.
Ethical considerations
Ethical clearance was sought from Kano State ministry of health. The permission to conduct the study was obtained from the ministry and wards head. Inform consent was obtained from each study participant through explanation of the study as well as the importance of their participation and they will inform of their right to withdraw at any time, all information that will be obtained from the study will keep confidential. Questionnaires was administered by the researcher to respondents after their inform consent was obtained to participate in the study.
Results and Analysis
This chapter present the findings of the study conducted on Assessment of Determinants of Traditional Uvulectomy Practice Among Mothers of Ungogo Local Government Area, Kano State. A quantitative (descriptive cross-sectional design) was utilized in this study. Participants of the study were drawn from two wards. A total of one hundred and fifty respondents participated in the descriptive cross-sectional design, questionnaires were successfully administered. The results of the study are divided into parts according to research objectives;
Socio-Demographic characteristics data of the respondent
This section presents the socio-demographic characteristics of the respondents. Variable covered include age in years, occupation, tribe, marital status and their higher formal educations
The table 4.2.1 above presents the characteristics of the respondents that participated in the study. The table shows that the age of the respondent from 15-25 years of age with 31 (26.6%), 26-35 with 77 (51.3%), 36-45 with 31 (20.6%) and 45 and above (7.3%), this shows that the majority of the respondent were 26-35years with (51.3%), occupation of the respondent, civil servant 15 (10%), student 45 (30%), housewife 90 (60%), this shows that the majority of the respondent were housewife with (60%), tribe of the respondent, hausa 90 (60%), fulani 45(30%), kanuri 13 (8.67%) and others 2 (1.33%), this shows that the majority of the respondent were hausa, marital status of the respondent, married 105 (70%), single 5 (3.3%) and widower 30 (20%) and others 10 (6.7%), this shows that the majority of the respondent were married with 70%, and educational status of the respondent, primary 15 (10%), secondary 45 (30%), tertiary 30(20%), no formal education 60 (40%), this shows that the majority of respondents have no formal education with 40% (Table 1).
| Variables | Categories | Frequency (N) | Percentage (%) |
|---|---|---|---|
| Age | 15-25 | 31 | 20.7 |
| 26-35 | 77 | 51.3 | |
| 36-45 | 31 | 20.7 | |
| 46 and above | 11 | 7.3 | |
| Mean ±SD | 32.4±4.04 | ||
| Range | 70-15 | ||
| Tribe | Hausa | 90 | 60.0 |
| Fulani | 45 | 30.0 | |
| Kanuri | 13 | 8.7 | |
| Others | 2 | 1.3 | |
| Higher Education Status | Primary | 15 | 10.0 |
| Secondary | 45 | 30.0 | |
| Tertiary | 30 | 20.0 | |
| No formal education | 60 | 40.0 | |
| Occupation | Civil Servant | 15 | 10.0 |
| Student | 45 | 30.0 | |
| House Wife | 90 | 60.0 | |
| Marital | Single | 5 | 6.7 |
| Married | 105 | 70.0 | |
| Widower | 30 | 20.0 | |
| Others | 2 | 3.3 |
Table 1: Distribution of Respondents According to the Socio-Demographic Characteristics. n=150.
The level of knowledge and awareness on traditional uvulectomy practice
This sections presents the finding of the study on the level of awareness of traditional uvulectomy.
The Table 2 shows the response of the respondents on the level of awareness of traditional uvulectomy practice. In the above table, the respondents were asked do they have idea about what uvula is, the majority (80%) responded positively indicating they have idea about what uvula is, while the smaller percentage (20%) expressed they do not have idea about what uvula is.. The respondents were also asked do they know the importance of uvula to life and health, majority (80%) responded positively, indicating they know the importance of uvula to life and health while the remaining (20%) said no. The respondents were asked that are they aware that the traditional uvulectomy is dangerous to health, majority (70%) responded with yes while (30%) with no. The respondents were asked do they believe that traditional uvulectomy helps to treat sore throat, majority of the respondents (80%) believed that the traditional uvulectomy helps to treat sore throat while (20%) of them the do not believed. The respondents were also asked that do they believe that it prevents chronic cough, majority (80%) responded that they believed it prevents chronic cough while (20%) they do not believed (Table 2).
| Items | Yes(n) | % | No(n) | % |
|---|---|---|---|---|
| Idea about uvula | 120 | 80.0 | 30 | 20.0 |
| Importance of uvula to life and health | 120 | 80.0 | 30 | 20.0 |
| Dangerous of traditional uvulectomy to health | 105 | 70.0 | 45 | 30.0 |
| Traditional uvulectomy practice helps to treat sore throat | 120 | 80.0 | 30 | 20.0 |
| Traditional uvulectomy prevents chronic cough | 120 | 80.0 | 30 | 20.0 |
Table 2: Distribution of Respondents According to level of knowledge and awareness on traditional uvulectomy practice. n=150.
Complications arising from the traditional Uvulectomy procedure and where they are managed
This section presents the findings of the study on complications arising from traditional uvulectomy practice.
The table 4.4.1 shows that the (90%) of the respondents agreed the bleeding is one of the complications while (10%) of the respondents they don't know, (70%) of the respondents agreed that fever is also one of the complications of traditional uvulectomy, (10%) they do not agreed while (20%) they don't know. (50%) of the respondents they don't know whether nasal regurgitation of food is one of the complications of traditional uvulectomy, then (40%) were not agreed that is one complications and (10%) were agreed. (80%) of the respondents were agreed that weight loss is one of the complications of traditional uvulectomy, (10%) were not agreed and (10%) they don't know. (50%) they don't know whether infections or septicaemia is one of the complications of traditional uvulectomy, (30%) were not agreed and (20%) were agreed. (50%) of the respondents agreed stenosis of the pharynx is one of the complications of traditional uvulectomy, (40%) they don't know and (10%) were not agreed. (35.3%) were not agreed that neonatal tetanus is one of the complications of traditional uvulectomy, (34.7%) were agreed and (30%) they don't know. (48%) were not agreed that speech problems is one of the complications of traditional uvulectomy, (26.7%) they don't know and (25.3%) were agreed (Table 3).
| Items | Yes(n) | % | No(n) | % | I don't know (n) | % |
|---|---|---|---|---|---|---|
| Speech problems | 38 | 25.3 | 70 | 48.0 | 42 | 26.7 |
| Fever | 105 | 70.0 | 15 | 10.0 | 30 | 20.0 |
| Weight loss | 120 | 80.0 | 15 | 10.0 | 15 | 10.0 |
| Nasal regurgitation of food | 15 | 10.0 | 60 | 40.0 | 75 | 50.0 |
| Infections/septicaemia | 30 | 20.0 | 45 | 30.0 | 75 | 50.0 |
| Stenosis of the pharynx | 75 | 50.0 | 15 | 10.0 | 60 | 40.0 |
| Neonatal tetanus | 52 | 34.7 | 53 | 35.3 | 45 | 30.0 |
| Bleeding | 135 | 90.0 | 0 | 0.0 | 15 | 10.0 |
Table 3: Distribution of Respondents on complications arising from the traditional Uvulectomy procedure. (n=150).
This section presents the findings of the study on where they respondents seek their management of the complications. It shows that most of them seek their management at home (Table 4).
Variables |
Yes N | % | No N | % |
|---|---|---|---|---|
| Home treatment | 135 | 90.0 | 15 | 10.0 |
| Health facilities | 135 | 90.0 | 15 | 10.0 |
| Traditional uvulectomist | 100 | 67.0 | 50 | 33.0 |
Table 4: Where they are managed.
The Table 5 shows that (90%) managed their complications at home, (10%) were not managed at home. (90%) managed their complications at home and (10%) were not managed at health facilities. (67%) managed their complications by visiting traditional uvulectomist while (33%) were not managed by visiting traditional uvulectomist (Table 5).
VARIABLES |
RESPONSE (n =308) | MEAN | SD | REMARK | ||||
|---|---|---|---|---|---|---|---|---|
| Strongly Agree | Agree | Neutral | Disagree | Strongly disagree | ||||
| Traditional uvulectomy can be prevented through health education | 105 | 41 | 4 | 0 | 0 | 4.67 | 0.98 | Strongly Agree |
| 70.0% | 27.3% | 2.7% | 0.0% | 0.0% | ||||
| Traditional uvulectomy can be prevented through community participation | 45 | 105 | 0 | 0 | 0 | 4.3 | 0.99 | Strongly Agree |
| 30.0% | 70.0% | 0.0% | 0.0% | 0.0% | ||||
| Traditional uvulectomy can be prevented through community mobilization | 45 | 75 | 15 | 0 | 0 | 3.9 | 0.98 | Agree |
| 30.0% | 50.0% | 10.0% | 0.0% | 0.0% | ||||
| Traditional uvulectomy can be prevented through community engagement and involvement | 30 | 105 | 15 | 0 | 0 | 4.1 | 0.96 | Strongly Agree |
| 20.0% | 70.0% | 10.0% | 0.0% | 0.0% | ||||
| Traditional uvulectomy can be prevented through community advocacy | 30 | 105 | 15 | 0 | 0 | 4.1 | 0.96 | Strongly Agree |
| 20.0% | 70.0% | 10.0% | 0.0% | 0.0% | ||||
| Using setting controlling mechanisms for the health care delivery system | 60 | 75 | 15 | 0 | 0 | 4.3 | 0.99 | Strongly Agree |
| 40.0% | 50.0% | 10.0% | 0.0% | 0.0% | ||||
| Through awareness creation to social help like traditional healers to draw clients enhancing the capacity of service provision | 45 | 90 | 15 | 0 | 0 | 4.2 | 0.98 | Agree |
| 30.0% | 60.0% | 10.0% | 0.0% | 0.0% | ||||
Table 5: Distribution of respondents on possible ways of preventing traditional uvulectomy practice (n=150).
Awareness on the Prevention or possible ways of traditional uvulectomy practice
The table 4.5 shows that 105 (70%) of the respondents strongly agreed, i can be prevented through health education, 41(27.3%) agreed, 4 (2.7%) Neutral, 0 (0%) disagreed, 0 (0%) strongly disagreed with a mean score of 4.67. It can be prevented through community participation 45 (30%) strongly agreed, 105 (70%) agreed, 0 (0%) Neutral, 0 (0%) disagreed, 0 (0%) strongly disagreed with a mean score of 4.3. It can be prevented through community mobilization, 45 (30%) strongly agreed, 75 (50%) agreed,15 (10%) Neutral, 0 (0%) disagreed, 15 (10%) strongly disagreed with a mean score of 3.9. It can be prevented through community engagement and involvement 30 (20%) strongly agreed, 105 (70%) agreed, 15 (10%) Neutral, 0 (0%) disagreed, 0 (0%) strongly disagreed, It can be prevented through community advocacy 30 (20%)) strongly agreed, 105 (70%) agreed, 15 (10%) neutral, 0 (0%) disagreed, 0 (0%) strongly disagreed. It can be prevented by using setting controlling mechanisms for the health care delivery system 60 (40%) strongly agreed, 75 (50%) agreed, 15 (10%) neutral, 0 (0%) disagreed, 0 (0%) strongly disagreed. It can be prevented through awareness creation to social help like traditional healers to draw clients enhancing the capacity of service provision 45 (30%) strongly agreed, 90 (60%) agreed, 15 (10%) neutral, 0 (0%) disagreed, 0 (0%) strongly disagreed with a mean score of 4.2. six out of the seven possible ways are strongly agreed.
Discussion, Summary and Conclusion
This chapter comprises of discussion of the major findings of the study, summary, conclusion and recommendations.
Discussion OF Finding
Socio-demographic characteristics
The finding of this study revealed that majority of the respondents were aged 26-35 years while those between 15-25 and 36-45 years accounting less than half, Best on occupation more than one third of the respondents were Housewife while the remaining ones are civil servants and students accounting for less than half respectively. On tribe more than half of the respondents were Hausa while fulani accounting for one third of the respondents [22]. For marital status more than two third of the respondents were married, while single accounting less than half and widower accounting for less than half of the responses. On educational status, majority of the respondents have no formal education, those with secondary level accounting for one third and those with tertiary accounting for less than half and those with primary accounting for less than half of the responses [23].
The socio-demographic finding is consistent with that of Adamu Asma'u et al (2021) on perception of traditional uvulectomy and associated factors among mothers of under five years children in Sokoto State, Nigeria shows that 320 mothers were selected and majority of the respondents were between 25-34 years with a mean age of 29.9± 8.3 years. Most of the respondents were Hausa’s and Muslims. Fulltime house wives constituted more than half of the respondents.
Best on this findings there is agreement between this research and research done by Adamu Asma`u et al (2021) were many of the respondents were Hausa by tribe and best on occupation more than half of the respondents were Housewives. Traditional believes make it to be one of the determinants of traditional uvulectomy.
Additionally, the overwhelming majority of the respondents identified as married and adhered to the Islamic faith and reflecting the socio-cultural context of the study location. Addressing the socio-cultural factors will be a key in reducing the traditional uvulectomy practice [24].
Research Question 1
What is the level of knowledge and awareness on traditional uvulectomy practice?
This study give an insight on the level of awareness on traditional uvulectomy practice of the respondents it is also revealed that those that have idea about uvula is, more than half of the respondents have idea about uvula. Those that know the importance of uvula to life and health, more than half responded positively, indicating they know the importance of uvula to life and health while less than half said no. Those that aware that the traditional uvulectomy is dangerous to health, more than half are aware that is dangerous to health. Those that believe that traditional uvulectomy practice helps to prevent sore were accounting two third of the responses while that do not believed accounting for less than half of the responses. majorityresponded that they believed it prevents chronic cough [25].
The finding has some similar finding with that of Abdullahi M et al (2016) on traditional uvulectomy among the neonates experienced in a Nigerian Tertiary Health Institution [6]. Prevention of sore throat was account more than half as the main reason for traditional uvulectomy. Other reasons include: family tradition less than half, cough less than half and to prevent delay speech less than half also. When compare with this research there is similar finding with that of Abdullahi M et al (2016) in the level of knowledge and awareness where all believe there is prevention of sore throat as one of the main reason of traditional uvulectomy practice, additionally, both researches find that the respondents believe traditional uvulectomy helps to prevents chronic cough [6].
Research Question 2
What are the complications arising from the traditional Uvulectomy procedure and where they are managed?
The finding of this study revealed that that the majority of the respondents agreed the bleeding is one of the complications while less than of the respondents they don't know, more than half of the respondents agreed that fever is also one of the complications of traditional uvulectomy, while than half they do not agreed and they don't know. Half of the respondents they don't know whether nasal regurgitation of food is one of the complications of traditional uvulectomy,. More than of the respondents were agreed that weight loss is one of the complications of traditional uvulectomy, less than half were not agreed and less than half they don't know. Half of the respondents they don't know whether infections or septicaemia is one of the complications of traditional uvulectomy, one third of the respondents were not agreed and less than half were agreed [26]. Half of the respondents agreed stenosis of the pharynx is one of the complications of traditional uvulectomy, more than one third they don't know and less than half were not agreed. One third of the respondents were not agreed that neonatal tetanus is one of the complications of traditional uvulectomy, one third were agreed and less than half they don't know. Less than half of the respondents were not agreed that speech problems is one of the complications of traditional uvulectomy, less than one third they don't know and were agreed respectively. Based on where the complications are managed that majority of the respondents managed their complications at home, less than one third were not managed at home. More than two third of the respondents managed their complications at health facilities and less than half were not managed at health facilities. More than half of the respondents managed their complications by visiting traditional uvulectomist while less than half were not managed by visiting traditional uvulectomist.
The finding further validates that of Abdullahi M et al (2016) on traditional uvulectomy among the neonates experienced in a Nigerian Tertiary Health Institution. in management and outcome, Two less than half patients with severe septicaemia died within 24 hours of admission, while the rest were discharged after full recovery. Only five less than half patients came for follow-up after a week of discharge (no complication was observed). Traditional medications were administered by the traditional healers in less than half patients to control bleeding.
Majority of the patients in the study never came for follow up after discharged. Probably because of parenteral perception of no need for follow up, low socioeconomic status and or poor educational status. Emphasis on follow up should be made for early recognition and prompt treatment of speech problems and nasal regurgitation from velopharyngeal incompetence.
This finding is also consistent with previous research study done by Adoga AA, et al (2011): 165 patients who had uvulectomy, less than half had septicaemia as a complication. And the research emphasizes that there is septicaemia as one of the complications [7].
Research Question 3
What are the possible ways of preventing traditional uvulectomy practice
The findings of this study revealed that majority of the respondents strongly agreed that it can be prevented through health education, while less than half of the respondents were agreed, less than half Neutral,. It can be prevented through community participation majority of the responses were agreed while less than half strongly agreed, It can be prevented through community mobilization, half of the respondents were agreed agreed while less than half were strongly agreed, less than Neutral, less than half strongly disagreed. It can be prevented through community engagement and involvement less than half of the respondents strongly agreed, while majority of the responses were agreed, less than half Neutral, , It can be prevented through community advocacy, More than half of the responses were agreed less than half strongly agreed, less than half neutral,. It can be prevented by using setting controlling mechanisms for the health care delivery system less than half strongly agreed, half of the respondents agreed, less than half neutral,. It can be prevented through awareness creation to social help like traditional healers to draw clients enhancing the capacity of service provision more than half of the responses were agreed while the remaining less than half strongly agreed, less than half neutral.
The finding is also correspondent with that of the Study done By Sadiya (2023) the result of the study indicated that less than half can be prevented through health education , more than one third it can be prevented through community mobilization, it can be prevented through community participation one third of the respondents.
The finding is a way similar to the study conducted by Dr Samuel Kariuki Ngugi (2005) on determinants of traditional uvulectomy among under five children at Thika District Hospital shows only less than half of the respondents sort advise from the health provider on indications for uvulectomy before making a decision to have their children undergo uvulectomy. For those that no longer believe in uvulectomy accounted for less than half. they gave reason as no improvement on previous operation accounted for one third, well informed less than half or just don’t believe in the practice. Women (mothers) are the most important in making decisions when it comes to traditional uvulectomy. This finding also shows when there is sufficient information or health education towards the traditional uvulectomy practice, the procedure will continue to reduced. Therefore through health education and community mobilization, the traditional uvulectomy practice can be prevented as people are now reducing the practice because of health education given to them.
Summary
Uvulectomy is the entire or partial removal of the uvula through surgery, and the procedure can be viewed in two ways.Traditional uvulectomy is a surgical procedure in which the total or partial part of the uvula is removed by traditional surgeons. This study was used to Assess the Determinants of Traditional Uvulectomy Practice Among Mothers of Ungogo Local Government, Kano. The objectives of the study was to assess the level of awareness of traditional uvulectomy practice, complications arising from the traditional uvulectomy procedure and where it is managed and ways of preventing traditional uvulectomy practice among Mothers of Ungogo Local Government, Kano State. A multistage sampling technique was used in conducting the research . simple random and systematic sampling was used. the data were collected by reading and translating the questionnaire in Hausa for five days period, after explaining in details and making emphasis on confidentiality before the data were collected and analyzed. Most of the respondents were Hausa, more than half were Married, more than half were Housewife aged range from 26-35 years. Majority of the respondents have idea about uvula, more than half of the respondents believed bleeding is one of the complications of traditional uvulectomy practice, fever accounted for more than half, nasal regurgitation accounted for more than two third, less than half they don't know and most of the respondents seek their management at health facilities , homeand traditional uvulectomist accounted for more than half also and more than of the respondents strongly agreed that traditional uvulectomy practice can be prevented through health education two third agreed can be prevented through Community participation and more than half also through community engagement and involvement and half of the respondents agreed that using setting controlling mechanisms for the health care delivery system can be used to prevents traditional uvulectomy practice.
Conclusion
In conclusion, the traditional uvulectomy practice is still being practiced in our society. It should be out rightly discouraged and laws promulgated to stop it or programs for training and re-training of the practitioners instituted to improve their practice and safeguard people in our society. Most of the respondents have good idea about what uvula is and where it is situated and the respondents believed the bleeding, fever and weight loss are some of the complications arising as a result of traditional uvulectomy practice and most of the respondents seek their care at home health facilities and traditional uvulectomist. And most of the respondents believed the procedure is now reducing due to provision of health education programs and increased in community mobilization and participation, Community mobilization and using setting controlling mechanisms for the health care delivery system will help in preventing the traditional uvulectomy practice (Table 6).
Recommendations
The present research work finding results made the following recommendations
There is a saying that "prevention is better than cure" and since the problem were identified it can be considered as saved.
- Health education of the committees through mass media on the danger of traditional uvulectomy and also designing strategies to improve community. Orthodox health seeking behavior whenever there is parental suspicion of childhood illness attribute to the uvula is another way of preventing traditional uvulectomy.
- Educate mothers to avoid such things or practices that injure the uvula or lead to throat problems especially poor personal hygiene.
- The health facility setting, a health worker (especially midwife) should advices the mother including the family members on not to allow the practice of traditional uvulectomy on the offsprings as it has a recognized negative effects on the baby's health and well-being.
- Collaborate with local healthcare workers and traditional healers to gather insight into the prevalence and perception of traditional uvulectomy.
- The government should organizes massive campaigns aimed at discouraging the practice of traditional uvulectomy to the community through media, at home visits and should assist with funding of programs in training and provides the barbers with cleansing agents for disinfecting their equipments.The case is reported to highlights these neurological threatening complications following traditional uvulectomy.
- Organizing workshops involving the traditional barber, parents and community leaders to sensitize them on the functions of palatine uvula and the negative effects following traditional uvulectomy practice.
- Organising collaborative ways with local health authorities and traditional healers to establish reporting mechanisms for complications associated with traditional uvulectomy.
- Implementation of community based educational programs aimed at raising awareness about the risks and potential complications of traditional uvulectomy.
- promote dialogue and collaboration between traditional healers and health care providers to develop culturally appropriate guidelines and practices for managing childhood illnesses without resolving to traditional uvulectomy.
Dear respondent,
The researcher is a 500-level student of the above-named institution, I am conducting a research titled “Assessment of Determinants of Traditional Uvulectomy Practices among Mothers of Ungogo LGA, Kano state”. Your participation is voluntary, your full cooperation and participation and will be greatly appreciated, hence you are expected to respond to every question sincerely. No name is required and all information given will be kept strictly confidential and will be used for research purpose only.
…………………….
Respondent’s signature
References
- Hoehn EN (2016) Human Anatomy & Physiology. Tenth edition.
- Adebola S, Ogunkeyede S, Obebe F, Olaniyan O, Fawole O et al. (2016) Profile of paediatric traditional uvulectomy in North -Western Nigeria:The need for caution and education. Intt J Pediatr Otorhinolaryngol 88: 194-9.
- Ogah SA, Ocheni SE (2014) Traditional uvulectomy in Lokoja, Nigeria and its associated complications. Asian J Pharm Nursing and Medical sciences 2: 47-9.
- Chukwezi (2015) A good shepherd, but with obstructive sleep apnea syndrome: traditional uvulectomy case series and literature review. The Journal of Laryngology & Otology 125: 982-986.
- Gan et al (2019) Beliefs about traditional Uvulectomy and Teething: Awareness and perception Among mothers in Tanzanian Rural setting. Ann Int Med Den Res 4: 20-25.
- Abdullahi M, Amuta SB (2016) Traditional uvulectomy among the neonate : Experience in a Nigerian Tertiary Health Institution. Borno Medical Journal 13: 16-20.
- Adoga AA, Nimkur LT (2011) The traditionally amputated uvular amongst Nigerians: still an ongoing practice. ISRN Otolaryngology.
- Kristin (2014) Otorhinolaryngological indication for uvulectomy.
- Isa A, Omotara BA, Sandabe MB, Garandawa HI (2011) PARENTAL REASONS AND PERCEPTION OF TRADITIONAL UVULECTOMY IN CHILDREN. Sahel Medical Journal 14: 210-216.
- Alene G, Edris M (2002) Knowledge Attitude and practices involved in Harmful Health Behaviour in Demba District,NorthWest Ethiopia. Ethiop J Health 16: 199-207.
- Kambale RM, Balibuno Y, Francisca NI, Kasengi JB, Mayele GF et al. (2018) Traditional uvulectomy, a common practice in South Kivu in the Democratic Republic of Congo. Medecine et sante tropicales 28: 176–81.
- Anatomy Oxford Medical Publications, 15th edition 3: 144-145.
- Araoye M (2004) Research methodology with statistics for health and social sciences. Ilorin Nathadex publishers 115-121.
- Cohen BJ (2016) Memmler’s Structure and Function of the Human Body, 11th edition.
- Harrington L, Tannock IF, Hill R, Cescon D (2021) Basic sciences of Oncology. 6th edition Butterworth and Co Publishers 10: 15-17.
- Eregie CO (1994) Uvulectomy as an epidermiological factor in neonatal tetanus mortality: observations from a cluster survey. West African Journal of Medicine 13: 56-58.
- Johnston NL, Riordan PJ (2005) Tooth follicle extirpation and uvulectomy. Australian Dental Journal 50: 267-272.
- Gebrekirstos K, Abebe M, Fantahun A (2014) A cross sectional study on factors associated with harmful traditional practices among children less than 5 years in Axum town north Ethiopia, 2013. Reprod Health 11: 46-47.
- Hunter L (1995) Uvulectomy--the making of a ritual. S Afr Med J 85: 901-2.
- Ijaduola GT (1982) Hazards of traditional Uvulec-tomy in Nigeria. East Afr Med J.
- Ladan ZF, Mohammed A, Ibrahim M, Obiagwu PN, Abba SU (2015) Neonatal tetanus in Kano: A ten year review. Niger J Basic ClinSci 12: 30-3.
- Eregie CO (1994) Uvulectomy as an epidemiological factor in neonatal tetanus mortality:-observations from a cluster survey. West African Journal of Medicine 13: 56-58.
- Miles SH, Ololo H (2003) Traditional surgeons in sub-Saharan Africa images from south Sudan. International Journal of STD AIDS 14: 505- 508.
- Murray A, Gardiner DS, McGuiness RJ (1998) Primary mycobacteria infection of the uvula. J Laryngol Otol 112: 11183-5.
- Olaosun A, Ojemakinde K, Raji A, Adedeji T, Adebola S (2006) Death of a child with Leukaemia subjected to Traditional Uvulectomy. The internet Journal of Third World Medicine 4: 1-4.
- Owbingire SS, Kamya ER, Sohal KS (2018) Beliefs about traditional Uvulectomy and Teething: Awareness and perception Among Adults in Tanzanian Rural setting. Ann Int Med Den Res 4: 25-30.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Abubakar SS (2024) Determinants of traditional uvulectomy practice among mothers of Ungogo Local Government, Kano State. J Comm Pub Health Nursing, 10: 539.
Copyright: © 2024 Abubakar SS. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 93
- [From(publication date): 0-2024 - Nov 18, 2024]
- Breakdown by view type
- HTML page views: 63
- PDF downloads: 30